Abstract
Background
The role of rotavirus as main etiologic agent of diarrhea has been well documented worldwide, including in Venezuela. However, information about the prevalence of gastrointestinal viruses such as calicivirus, adenovirus and astrovirus is limited and the contribution of other agents as Aichi virus and klassevirus is largely unknown. To explore the etiological spectrum of diarrhea associated with agents other than rotaviruses, 227 stool samples from children under 5 years old with acute gastroenteritis, collected in Valencia (Venezuela) from 2001 to 2005, and previously tested as rotavirus-negative, were analyzed for caliciviruses, adenoviruses, astroviruses, Aichi viruses, klasseviruses, picobirnaviruses and enteroviruses by specific RT-PCRs.
Results
At least one viral agent was detected in 134 (59%) of the samples analyzed, mainly from children under 24 months of age and most of them belonging to the lowest socioeconomic status. Overall, enterovirus was identified as the most common viral agent (37.9%), followed by calicivirus (23.3%), adenovirus (11.5%), astrovirus (3.5%), klassevirus (1.3%) and Aichi virus (0.4%), while no picobirnavirus was detected. Klasseviruses were found during 2004 and 2005 and Aichi viruses only in 2005, indicating their circulation in Venezuela; meanwhile, the rest of the viruses were detected during the whole study period. Coinfections with two or more viruses were found in 39 (29.1%) of the infected children, most under 24 months of age. Adenovirus was involved as the coinfecting agent in at least 46.9% of the cases, but no differences concerning socio-demographic variables were observed between the coinfected and the single infected children.
Conclusions
The results show that various enteric viruses, including enteroviruses, caliciviruses and adenoviruses, accounted for a significant proportion of infantile diarrhea cases in Venezuela before rotavirus vaccine implementation. In addition, emerging viruses as Aichi virus and klassevirus were found, indicating the need to continue monitoring their spreading into the communities. Efforts are needed to develop more accurate methods to identify the major causes of diarrhea and to provide tools for more effective preventive measures.
Keywords: Acute gastroenteritis, Children, Enteric viruses, Prevalence, Venezuela
Background
Acute gastroenteritis (AGE) in children is one of the most significant diseases, causing morbidity and mortality worldwide [1, 2]. Although the improvement in sanitation and prevention strategies has determined a substantial reduction in the mortality rate for diarrhea from 15% in 2008, to about 9% in 2015, equivalent to 500,000 deaths among children less than 5 years old, infectious diarrheas are still an important public health concern, both in resource-poor settings and industrialized countries [2, 3].
Viruses are recognized as a major cause of severe AGE, particularly in children. Rotaviruses (RV) are the main cause of mortality due to diarrhea in those under 5 years old, preventable with the vaccination [4, 5]. Yet, despite a significant reduction after RV vaccine introduction in 2006, hospitalizations for infantile AGE of viral etiology continued to be reported [6–9]. The increasing use of more powerful diagnostic systems in the last few years, as the conventional polymerase chain reaction (PCR) or high-throughput technologies, for the amplification and identification of virus genomes in stool samples, has resized the study of the agents involved in childhood AGE [7, 10, 11], and changed significantly the pathogen spectrum of community-acquired gastroenteritis [6, 7, 12, 13].
Other viruses considered of clinical importance and frequently associated with diarrhea mortality are the human caliciviruses (HuCVs), members of the family Caliciviridae, which have acquired importance, especially after RV vaccine implementation [6, 10, 14]. Human adenoviruses (HAdVs), members of the family Adenoviridae, are often reported as the second or third cause of infantile diarrhea, both sporadic or outbreak associated, and cause a wide range of disease symptoms [14, 15]. Finally, human astroviruses (HAstVs), of the family Astroviridae, which affect predominantly children under 2 years of age, have been involved in 0.5–15% of diarrheal outbreaks associated to severe pediatric cases [16–18].
On the other hand, the clinical importance of viruses belonging to the wide family Picornaviridae, such as enterovirus (EV), Aichi virus (AiV) and klassevirus/salivirus (KV), is up-to-date unclear, with those viruses presumably playing a rather minor epidemiological role in diarrhea [14, 19–22]. Some subgroups of EVs have been involved as causative of at least 3.4% of AGE of unknown etiology [23]. Similarly, AiV, of the genus Kobuvirus, was initially described as cause of oyster-associated non-bacterial gastroenteritis in human [22], and later associated with AGE, reaching detection rates between 0.5 and 0.9% in Europe, and up to 4% in Asia and Africa [20, 24]. AiVs were recovered during a study from a major river polluted with sewage discharges in Caracas (Venezuela) during 2007–2008 [25], but its impact on the burden of AGE in Venezuela is unknown. Finally, KVs, discovered in human stool and sewage [22], have been significantly associated with pediatric diarrhea in different countries, especially in children less than 3 years old, with a frequency ranging from 0.1 to 8.7% [26–28].
Because the information about viruses different from RV associated with diarrhea in Venezuela is limited, the present study was aimed to determine the incidence of infections caused by other conventional gastroenteritis viruses before RV vaccine implementation, and to investigate the contribution of AiV and KV to diarrheal diseases, until now unknown in Venezuela. For this purpose, children less than 5 years old with diarrhea attended at a large public hospital in Valencia City, over a 5-year period (2001–2005), were studied using molecular detection assays.
Methods
Study design
The study included stool samples collected from children with AGE under 5 years old, attended during the years 2001–2005 in the city of Valencia, Carabobo State (Venezuela), as part of a RV diarrhea surveillance program conducted at the Hospital de Niños ‘‘Dr. Jorge Lizarraga’’ of the Ciudad Hospitalaria ‘‘Dr. Enrique Tejera’’ (CHET) described previously [29].
AGE was defined as three or more liquid stools over a 24-h period and for not over 14 days. To determine the epidemiologic and clinical characteristics of the AGE, information from the clinical history and the physical examination were collected: age, gender, nutritional status and type of treatment (outpatient or inpatient hospital based) were recorded for each case and used as measurement instrument for the severity of the community-acquired AGE, together with the estimation of dehydration, assessed according to WHO criteria [30]. Inpatient treatment was defined as the admission to either the emergency room for a short stay to receive oral rehydration therapy (< 24 h) or to the regular pediatric wards of the hospital for longer time [31]. The socioeconomic status was determined by a modified Graffar methodology [32].
Sample collection
From a total of 13,026 fecal diarrhea specimens obtained from the enrolled children within 48 h following admission, 227 were randomly selected from RV negative-tested samples. All the samples had been systematically examined for the presence of RV antigen, bacteria and parasites as previously described [29, 33] and resulted negative for all of them. All samples were stored at − 80 °C until processed.
Nucleic acid extraction
Fecal suspensions (10% w/v in phosphate buffer saline) were prepared from each stool sample, vortexed, and clarified by centrifugation at 10,000g for 10 min. Viral RNA/DNA was extracted simultaneously from 200 µl of supernatant, using the QIAamp MinElute Virus Spin Kit (QIAGEN, Hilden, Germany), based in a spin-column procedure, and following the manufacturer’s instructions. Briefly, samples were lysed in the presence of QIAGEN Protease and Buffer AL containing RNA carrier provided by the kit. Ethanol absolute (Merck, KGaA, Darmstadt, Germany) was added to the sample that was then transferred onto a QIAamp MinElute column, where the viral nucleic acids were adsorbed onto the silica-gel membrane. Wash buffers were used to remove impurities by centrifugation, and finally, the viral nucleic acids were eluted in 50 µl of Buffer AVE (provided), for use in amplification reactions or storage at − 70 °C.
Reverse transcription (RT)
Screening for the presence of RNA viruses, such as HuCV, HAstV, AiV, KV, EV and human picobirnavirus (HPBV), was conducted firstly by RT reaction, as follows: the extracted RNA was denatured and then reverse transcribed with random primers (0.02 µg) using M-MLV reverse transcriptase (200 U) and deoxynucleoside triphosphate mix (0.2 mM), RNasin (40 U) (Invitrogen, Carlsbad, California, USA) in reverse transcription buffer to a final volume of 50 µl. The mixture was incubated at 37 °C for 1 h followed by incubation at 70 °C for 15 min, to obtain cDNA.
Polymerase chain reaction (PCR)
Single PCR reactions were performed from 5 µl of extracted DNA (for HAdV detection), or cDNA (for RNA viruses), using a selected combination of oligonucleotide primers specific for each virus previously described [22, 34–40] at a final concentration of 0.2 µM each one. Two additional degenerated primers were designed for this study by multiple alignments, leading to broad target specificity for HuCV (290YM) and HAstV (MON394d) (Table 1). Cycling conditions used were adapted as shown in Table 1. All PCR reactions were done in a final volume of 50 µl and the PCR products were analyzed by agarose gel electrophoresis and ethidium bromide staining.
Table 1.
Oligonucleotide primers and amplification conditions used in this study for the molecular detection of gastroenteritis viruses
| Virus | Target region | Rounds of PCR | Sense | Primer name | Sequence 5′–3′ | Cycling protocol1 | Nucleotide position | Amplicon size (bp) | Reference |
|---|---|---|---|---|---|---|---|---|---|
| Calicivirus | RNA-dependent RNA polymerase |
1st | − | 289H | TGACGATTTCATCATCACCATA | 4865–4886a | 34 | ||
| − | 289I | TGACGATTTCATCATCCCCGTA | A | 4865–4886a | 319 | ||||
| + | 290YM | GATTACTCCAGGTGGGAYTCMAC | 4568–4590a | In this study | |||||
| Adenovirus | Hexon | 1st | + | hexAA1885 | GCCGCAGTGGTCTTACATGCACATC | B | 18,858–18,883b | 301 | 35 |
| − | hexAA1913 | CAGCACGCCGCGGATGTCAAAGT | 19,136–19,158 | ||||||
| Astrovirus | ORF-1 | 1st | + | MON340 | CGTCATTATTTGTTGTCATACT | C | 1182–1203 | 289 | 36 |
| − | MON348 | ACATGTGCTGCTGTTACTATG | 1450–1470 | ||||||
| 2nd | + | MON394d | GARATCCGTGATGCTAATGG | D | 1250–1269 | 220 | In this study | ||
| − | MON348 | ACATGTGCTGCTGTTACTATG | 1450–1470 | 37 | |||||
| Aichi virus | 3C-3D | 1st | + | 6261 | ACACTCCCACCTCCCGCCAGTA | E | 6261–6282c | 519 | 38 |
| − | 6779 | GGAAGAGCTGGGTGTCAAGA | 6760–6779 | ||||||
| Klassevirus | 2C | 1st | + | LG0098 | CGTCAGGGTGTTCGTGATTA | F | 4463–4482 | 345 | 27 |
| − | LG0093 | AGAGAGAGCTGTGGAGTAATTAGTA | 4783–4807 | ||||||
| Enterovirus | 5′NTR2 | 1st | + | EV1 | CGGCCCCTGAATGCGGC | G | 454–470 | 194 | 39 |
| − | EV2 | CACCGGATGGCCAATCCA | 630–647 | ||||||
| Picobirnavirus | + | PicoB25 | TGGTGTGGATGTTTC | 665–679d | 201 | ||||
| RNA-dependent RNA polymerase |
Multiplex PCR |
− | PicoB43 | ARTGYT GGTCGAACTT | H | 850–865d | 40 | ||
| + | PicoB23 | CGGTATGGATGTTTC | 685–699e | 369 | |||||
| − | PicoB24 | AAGCGAGCCCATGTA | 1039–1053e |
1Cycling conditions for the PCRs were as follows: A = 94 °C for 2 min, 40 cycles of 94 °C for 30 s, 50 °C for 30 s, 72 °C for 1 min, and a final elongation at 72 °C for 10 min; B = 94 °C for 4 min, 40 cycles of 92 °C for 1.5 min, 55 °C for 1.5 min, 72 °C for 2 min, and final elongation at 72 °C for 10 min; C = 94 °C for 5 min, 40 cycles of 94 °C for 30 s, 50 °C for 30 s, 72 °C for 30 s; and final elongation at 72 °C for 10 min; D = 94 °C for 2 min, 30 cycles of 94 °C for 30 s, 50 °C for 30 s, 72 °C for 30 s, and final elongation at 72 °C for 10 min; E = 95 °C for 1 min, 40 cycles of 95 °C for 30 s, 55 °C for 30 s, 72 °C for 1 min and a final elongation at 72 °C for 10 min; F = 94 °C for 2 min, 40 cycles of 94 °C for 30 s, 56◦C for 30 s, 72 °C for 1 min, and final elongation at 72 °C for 10 min; G = 94 °C for 2 min, 40 cycles of 94 °C for 30 s, 60 °C for 30 s, 72 °C for 1 min, and a final elongation at 72 °C for 7 min. H = 94 °C for 3 min, 40 cycles of 94 °C for 1 min, 42 °C for 1 min, 72 °C for 1 min, and a final elongation at 72 °C for 10 min
25′nontranslated region
aNumbering given according to positions in Norovirus GI, complete genome (NC_001959.2)
bSequence position refers to the Ad2 hexon region. The primers used allow detecting the 47 human adenovirus serotypes
cSequence position refers to Aichi virus genomic RNA, Ac. N. AB010145.1
dSequence position refers to the 1-CHN-97 strain (Genogroup I)
eSequence position refers to the 4-GA-91 strain (Genogroup II)
Statistical analysis
Data were analysed for the comparisons of variables using 2 × 2 tables with χ2 test, or Fisher’s exact test (two-tailed, 95% confidence intervals) (Epi Info™ 7.1.4.0, CDC Atlanta, GA, USA). Student’s test was applied for comparisons of variable values. Tests were considered significant when p < 0.05.
Results
Prevalence of the viral infections
Overall, the analysis by RT-PCR for HuCV, HAdV, HAstV, AiV, KV, EV and HPBV of the 227 selected stool samples negative for RV, enteropathogenic bacteria and parasitic infections, revealed the presence of at least one viral agent in 134 (59%) of them. The annual prevalence of viral infection fluctuated around an average of 65%, with comparable values between 2001 and 2004 (range 62.5–69.2%) and a significant drop (37.5%) in 2005 (p < 0.015) (Fig. 1).
Fig. 1.
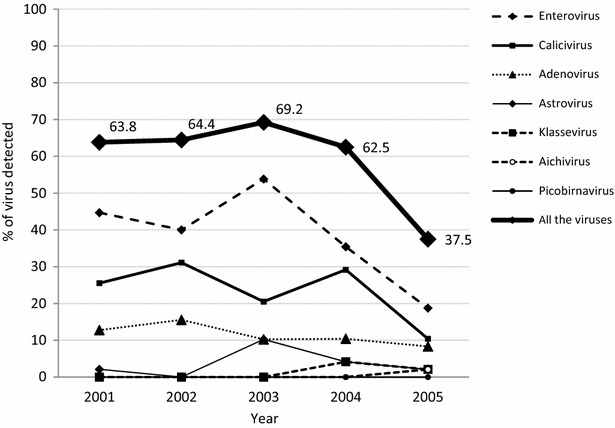
Temporal variation of the positivity rate for gastroenteritis viruses in children with diarrhea from Valencia, 2001–2005. The prevalence of viral infection among the 227 RV-negative children studied is indicated with the line marked with diamonds. A significant drop (p < 0.015) in the overall percentage of children infected was observed in 2005. The others drawn lines show the temporal detection rates for each single viral infection
Detection rate and temporal variation of gastrointestinal viral agents
Figure 2 shows the detection rate for each single virus found in the stools of the 227 children studied from Valencia. EV was the most common etiological agent detected, present in 86 (37.9%) of the 227 samples, followed by HuCV in 53 (23.3%), HAdV in 26 (11.5%), HAstV in 8 (3.5%), KV in two (1.3%) and AiV in one (0.4%) (Fig. 2). No HPBV was detected.
Fig. 2.
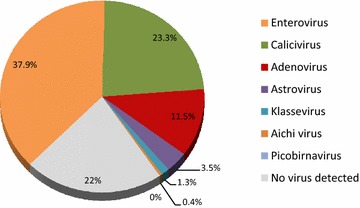
Distribution (%) of gastrointestinal viruses among 227 children with non-RV associated diarrhea from Valencia, 2001–2005
As shown in Fig. 1, EV, HuCV, and HAdV were detected throughout the study period, while the finding of HAstV, KV and AiV was intermittent (particularly KV and AiV that emerged at the last years). A significant decrease (from 53.8 to 18.8%, p = 0.0006) in the detection rate for EV was observed between 2003 and 2005; a reduction was also observed for HuCV (from 29.2 to 10.4%, p = 0.021) from 2004 to 2005. No trend was observed for the other viruses (Fig. 1).
Socio-demographic variables of all the children studied
Age
The median age of the 227 children studied was of 11 months (range 1–58). No significant difference was observed in the median age of the 134 virus infected children when compared with the 93 children who resulted negative for all viral agents studied (diarrhea of unknown etiology) (13 vs. 10 months, p = 0.218). For the children under 24 months of age, the proportion of positive samples for viruses was significantly higher than that of negative samples (85.8% vs. 75.3%) (p = 0.044) (Fig. 3a).
Fig. 3.
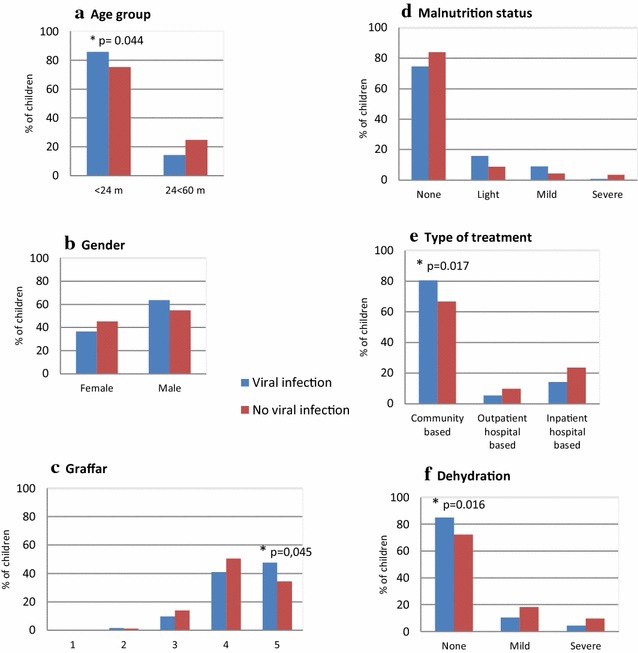
Distribution (%) of virus positive and negative children in according to demographic and clinical characteristics. A comparison between the proportion of children with viral infection (n = 134, histogram bars in blue color) and those without any virus detectable with the specific primers used in this study (n = 93, in red color) is shown. The variables shown are: a age group, b gender, c Graffar, d malnutrition status, e type of treatment, and f dehydration. Significant differences among groups are indicated with asterisk (*), including “p” value
Gender
A predominance of male over female was observed among the children positive, as well as among those negative children for viral infection (Fig. 3b), and the differences within genders were not significant (p > 0.05).
Socioeconomic level (Graffar)
The proportion of children from the lowest socioeconomic level (Graffar 5) was significantly higher among the positive for viral detection than among those negative (47.8% vs. 34.4%, p = 0.045) (Fig. 3c).
Malnutrition status
Well-nourished children prevailed over those with some condition of malnourishment; nevertheless, no statistical significant differences (p > 0.05) were observed for infected or non-infected children in any status (Fig. 3d).
Type of treatment
The diarrhea caused by viruses was significantly more associated with outpatient episodes that did not require hospitalization than diarrhea episodes of unknown etiology, not caused by any of the viruses studied (80.6% vs. 66.7%, p = 0.017) (Fig. 3e).
Dehydration
The proportion of children who suffered a mild or severe form of dehydration was significantly lower among virus infected children than among children with no detectable virus (14.9% vs 28%, p = 0.016) (Fig. 3f).
Incidence of single or mixed infection
Of the 134 children with diarrhea caused for any of the viruses studied, 95 (70.9%) resulted positive at a single enteric viral pathogen, and 39 (29%) suffered a mixed infection or coinfection (simultaneous detection of two or more viruses) (Table 2). The analysis of the socio-demographic variables and clinical parameters in relation with the severity of the AGE between single and mixed infected children did not reveal any significant difference (p > 0.05). Thus, age, gender, Graffar, nutritional status, dehydration and type of treatment of the children infected with a single virus were similar to those observed in children with coinfections (Table 2).
Table 2.
Comparison of the demographic and clinical characteristics of children suffering single or mixed viral infections
| Single infection | Mixed infection | |
|---|---|---|
| N. of children infected | 95 (70.9) | 39 (29.1) |
| Median age, months | 13 | 11 |
| Age group, months | ||
| < 24 | 78 (82.1) | 37 (94.9) |
| 24–60 | 17 (17.9) | 2 (5.1) |
| Gender | ||
| Female | 31 (32.6) | 18 (46.2) |
| Male | 64 (67.4) | 21 (53.8) |
| Graffar socioeconomic level, n. (%) | ||
| 1 | – | – |
| 2 | 1 (1.1) | 1 (2.6) |
| 3 | 9 (9.5) | 4 (10.3) |
| 4 | 39 (41.1) | 16 (41) |
| 5 | 46 (48.4) | 18 (46.2) |
| Malnutrition status | ||
| None | 73 (76.8) | 28 (71.8) |
| Light | 13 (13.7) | 7 (17.9) |
| Mild | 9 (9.5) | 3 (7.7) |
| Severe | – | 1 (2.6) |
| Dehydration | ||
| None | 82 (86.3) | 31 (79.5) |
| Mild | 10 (10.5) | 5 (12.8) |
| Severe | 3 (3.2) | 3 (7.7) |
| Type of treatment | ||
| Outpatient | 78 (82.1) | 30 (76.9) |
| Inpatient | 17 (17.9) | 9 (23.1) |
Data are n (%) of children studied. No significant difference (p > 0.05) related with these variables was observed. Data were analysed using χ2 or Fisher’s exact test (two-tailed, 95% confidence intervals) when the size sample was less than 5 (Epi Info™ 7.1.4.0, CDC Atlanta, GA, USA). The significance of the difference for the ages was calculated by Student’s test. The scale used for the Graffar socioeconomic level was based in a modified methodology described by Méndez Castellano et al. [32]
Figure 4 shows the proportion of gastrointestinal viruses involved in single or in coinfection during the AGE episodes. EVs were more frequently associated with single infection (58/86 strains detected, 67.4%, p = 0.003) than the other viruses. In contrast, HAdVs were significantly more involved in coinfections (18/26, 69.2%, p = 0.011) than in single infections. Finally, for HuCV and HAstV more than half of the infections were coinfections (54.7 and 62.5%, respectively) (Fig. 4).
Fig. 4.
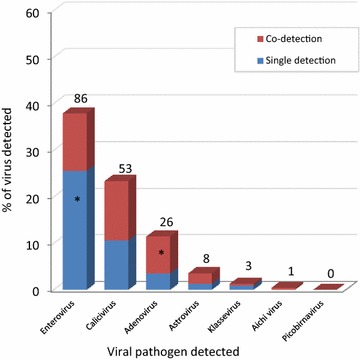
Proportion of gastrointestinal viruses involved in single or in coinfection in children with diarrhea from Valencia, 2001–2005. The figure shows the frequency of detection of each virus involved in single infection (only one virus detected, in blue color) or in co-infection (virus simultaneously detected together with one or more viruses, in red color). Numbers above the histogram bars indicate the total number of viruses detected (n = 177) among the 227 children studied. Significant differences (p < 0.05) compared to the rest of the groups are indicated with asterisk (*) inside the histograms
The most frequent combination of coinfecting agents was given by HuCV/EV, which affected 15 of 39 children (38.5%) (Table 3). HAdV coinfected especially with EV (17.9%), HuCV (15.4%), both together (10.3%), or with HAstV (2.6%) (Table 3), which represent altogether 46.2% of the 39 mixed infections evaluated in this study. The only AiV strain found in this study was detected in mixed infection with a strain of HuCV (Table 2) in a severely dehydrated and malnourished child of 1 month old, living in poor conditions (Graffar 5), who required to be hospitalized.
Table 3.
Viral agents involved in the 39 coinfections in children suffering diarrhea in Valencia, 2001–2005
| Coinfection pattern | Number (%) |
|---|---|
| Calicivirus + Enterovirus | 15 (38.5) |
| Enterovirus + Adenovirus | 7 (17.9) |
| Calicivirus + Adenovirus | 6 (15.4) |
| Calicivirus + Adenovirus + Enterovirus | 4 (10.3) |
| Calicivirus + Astrovirus | 2 (5.1) |
| Calicivirus + Klassevirus | 1 (2.6) |
| Calicivirus + Aichi virus | 1 (2.6) |
| Adenovirus + Astrovirus | 1 (2.6) |
| Astrovirus + Enterovirus | 2 (5.1) |
Socio-demographic and clinical features of the children according to the gastrointestinal virus detected.
Table 4 shows the comparison of the socio-demographic and clinical parameters for the 95 children presenting only single virus infection. The analysis excluded HAstV and KV because of the low number of samples positive.
Table 4.
Demographic and clinical characteristics of the children with single infection
| Enterovirus | Calicivirus | Adenovirus | Astrovirus | Klassevirus | Aichi virus | Picobirnavirus | |
|---|---|---|---|---|---|---|---|
| N. of children infected | 58 | 24 | 8 | 3 | 2 | 0 | 0 |
| Median age, months | 14 | 11 | 8 | 13 | 0.6 | – | – |
| Age group, months | |||||||
| < 24 | 45 (77.6) | 21 (87.5) | 7 (87.5) | 3 (100) | 2 (100) | – | – |
| 24–60 | 13 (22.4) | 3 (12.5) | 1 (12.5) | – | – | – | – |
| Gender | |||||||
| Female | 16 (27.6) | 9 (37.5) | 3 (37.5) | 2 (66.7) | 1 (50) | – | – |
| Male | 42 (72.4) | 15 (62.5) | 5 (62.5) | 1 (33.3) | 1 (50) | – | – |
| Graffar socioeconomic level | |||||||
| 1 | – | – | – | – | – | – | – |
| 2 | – | 1 (4.2) | – | – | – | – | – |
| 3 | 6 (10.3) | 2 (8.3) | 1 (12.5) | – | – | – | – |
| 4 | 21 (36.2) | 11 (45.8) | 4 (50) | 1 (33.3) | 2 (100) | – | – |
| 5 | 31 (53.4) | 10 (41.7) | 3 (37.5) | 2 (66.7) | – | – | – |
| Malnutrition status | |||||||
| None | 43 (74.1) | 18 (75.0) | 8 (100) | 2 (66.7) | 2 (100) | – | – |
| Light | 7 (12.1) | 5 (20.8) | – | 1 (33.3) | – | – | – |
| Mild | 8 (13.8) | 1 (4.2) | – | – | – | – | – |
| Severe | – | – | – | – | – | – | – |
| Dehydration | |||||||
| None | 51 (87.9) | 22 (91.7) | 5 (62.5) | 3 (100) | 1 (50) | – | – |
| Mild | 6 (10.3) | 1 (4.2) | 3 (37.5) | – | – | – | – |
| Severe | 1 (1.7) | 1 (4.2) | – | – | 1 (50) | – | – |
| Type of treatment | |||||||
| Outpatient | 49 (84.5) | 20 (83.3) | 5 (62.5) | 3 (100) | 1 (100) | – | – |
| Inpatient | 9 (15.5) | 4 (16.7) | 3 (37.5) | – | – | – | – |
Data are n (%) of children studied. No significant difference (p > 0.05) related with these variables was observed. Data were analysed using χ2 or Fisher’s exact test (two-tailed, 95% confidence intervals) when the size sample was less than 5 (Epi Info™ 7.1.4.0, CDC Atlanta, GA, USA). The significance of the difference for the ages was calculated by Student’s test. The scale used for the Graffar socioeconomic level was based in a modified methodology described by Méndez Castellano et al. [32]
No significant difference was shown in the median age, gender, Graffar and nutritional status of the children affected, regardless of the infecting virus. Children less than 24 months prevailed over the oldest, and although the EV infected subjects were slightly in a higher percentage (22.4%) when compared with those infected with HuCV and HAdV, the differences were not significant (p > 0.05).
Regarding the variables related with the severity of the AGE, no virus was significantly associated with more severe dehydration or a greater number of inpatient episodes (p > 0.05).
Discussion
The present study shows the epidemiology of viruses that caused pediatric AGE in Valencia (Venezuela) between 2001 and 2005 before the RV vaccine implementation. Although the population studied does not represent the entire epidemiological data of the viral diarrheal disease of this country, the results should provide a good estimation of the real impact of the viral AGE during the years 2001–2005 by causes other than RV.
The high prevalence of enteric virus found in this study is similar to that reported previously by others authors [12, 41, 42], and showed that EV, HuCV, HAdV, HAstV, AiV and KV accounted for a significant proportion of RV-negative AGE in this locality. The rate was lower than that shown by a Japanese study where multiplex assays including a larger number of target pathogens were applied [8], but it was higher than that described in European, Asian and African studies [17, 43–45], as well as that reported in a previous study performed during the year 2003 in Valencia City [46]. Of note, a fraction (41%) of the diarrhea cases here studied remained without a precise etiology, probably due to a low viral load, the presence of inhibitors in the samples or viruses not included in the assays. However, the relatively higher detection rate of viral agents reflects an increase of the diagnostic capabilities of the PCR-based assays used, although it could also depend on the population group studied, which included mostly children under 24 months of age, belonging to the lowest socioeconomic stratum (Graffar 5), living in the most precarious sanitary and dietary conditions, where the fecal–oral transmission of a wide range of pathogens was favored.
The significant higher frequency of viral infections, as well coinfections, shown here in children less than 24 months of age contrasts with previous data from Valencia where no age differences were observed in viral enteric infections [46]. It is instead in agreement with data obtained by others authors elsewhere [44, 47], and shows the highest susceptibility of the children to the viral infection during the early childhood, perhaps due to unsatisfactory protective immunity.
Previous data have reported that viral infections other than RV are clinically milder than the RV infection [44, 46, 48]. In this study, only RV-negative stool samples were included; therefore a comparison of the clinical conditions with children infected with RV could not be done. However, the data suggest that the infections by viruses such as EV, HuCV, HAdV, HAstV, AiV and KV would be mainly associated with less severe diarrheic episodes, not necessarily demanding medical intervention or hospitalizations.
This study demonstrates the contribution of EV and HuCV as important etiologic agents of viral AGE in the setting studied, both viruses found together in mixed infections in almost a quarter of the cases studied. The detection rate obtained for EV as single infecting agent was similar to that reported in a study carried out in Maracaibo (Venezuela) during 2008–2009 [49], and it was higher than that described in Thailand [23]. On the other hand, this rate was similar to the RV rate detection (24.5%) reported in another study carried out in Valencia City, during the same period [33]. Some serotypes of echovirus and coxsackievirus B have been described to be cause of diarrhea [50, 51]. It is noteworthy that the presence of Sabin vaccine-related strains in stool samples of diarrheic children could have caused an overestimation in the EV detection rate with the PCR assay used. In addition, EVs could be occasionally shed with the feces of patients suffering a broad spectrum of other non-enteric diseases, sometimes in prolonged way [20, 23, 50]. This would explain in part the relatively higher rate of EV found in this study in infected children older than 24 months than that of other viruses. Thus, case–control studies and further genotyping of the strains detected will be desirable, to better define the burden of EV as a cause of diarrheal disease.
The overall prevalence of HuCV observed in this study, the second most common causative agent of viral AGE, was comparable to that described by others among RV-negative samples from children with diarrhea in four distinct Thai regions under sentinel surveillance between 2006 and 2008 [52], and higher than that reported previously in Valencia City during the 2003 [46]. This prevalence indicates a greater ability of the primers used in the PCR assay to detect a broad diversity of strains. It ratifies also the need of monitoring the contribution of the HuCVs to the burden of the AGE after implementation of RV vaccination.
A significant observation in this study was also the relatively higher detection rate of HAdV infection, as compared to a previous study based on serologic assays from Valencia [46], and to reports from other continents [53–55] that suggest the existence of a geographic variability of the virus prevalence, as well as the important contribution of the HAdVs to the mixed infections. A similar rate of HAdV detection was reported from Korea during the years 2012–2013 [6], but it is noteworthy that the relative high prevalence for HAdV observed in this study could have also been determined by the presence in the stools of non-enteric types that could occasionally be excreted from respiratory source, and detected by the assay used, directed to amplify a conserved portion of the hexon-coding gene, common for all the HAdV. Thus, the molecular characterization is a crucial step to define the species of HAdV mainly involved in diarrhea and to understand the true contribution to the AGE. No information about the types of HAdV that have been circulating in Venezuela is available, but preliminary results indicate that most of the HAdV strains found in Valencia City during the same period were enteric types (Blanco R., personal communication).
HAstV were involved in a modest number of episodes, mainly in mixed infections with HuCV, HAdV and EV, which evolved as a mild form of AGE, similar to that reported by other studies [17, 41]. The HAstV detection rate found here was comparable with the data from a previous local study [46], and those from Lebanon, France and Germany [41, 44, 56].
Although AiV and KV have been associated with AGE in several continents [17, 24, 27, 28, 57–59], to our knowledge, there have not been reports of AiV and KV causing infections in Venezuelan human population. Unfortunately, the low rate of detection in this study did not allow to evaluate their relationship with socio-demographic and clinic variables, but their presence confirms the participation as agent of childhood diarrhea and the relatively recent introduction in Venezuela.
In this study were used primers directed to the most commonly described HPBVs of genogroup I and II [40], but no virus was found. Possibly, their high genomic diversity could have limited the detection with the RT-PCR assay available. Thus, additional efforts are required to optimize assays able to identify these and other uncommon viruses associated with AGE, as well the use of new technologies as virus microarray, sequence-independent amplification and sequencing of viral nucleic acids [7, 11, 22], to clarify their epidemiology and possible pathogenicity.
Conclusions
This study demonstrated a high prevalence of enteropathogenic viruses other than RV in Venezuelan children suffering acute diarrhea, confirming the contribution of conventional enteric viruses in the pediatric AGE in this country. In addition, the presence of emergent viruses more recently described, such as AiV and KV is also described. Because the study included only diarrheic pediatric patients who received medical attention in Valencia City, the prevalence of virus infection reported here could represent an underestimation of the true rates of gastroenteritis associated viruses circulation in the population. Future studies should consider asymptomatic and self-limiting diarrhea cases. However, these results, obtained from five consecutive years, expand the knowledge about the spectrum of viral agents involved in acute community-acquired disease, and provide a baseline data for the molecular epidemiology study of these pathogens, which will be helpful for comparison with regional data obtained in post-RV vaccination era. Finally, they ratify the need for a long-term surveillance for such enteropathogenic viruses, following the implementation of RV vaccination, to better understand the participation of these agents in children AGE.
Authors’ contributions
EV and ACA conceived the study, participated in the design/adaptation of experimental protocols, analysis results and wrote the initial draft of the manuscript. RG, ACA and RB were engaged in sample processing and data collection. EV supervised the laboratory procedures and PCR quality control, performed the statistical analysis, data interpretation, graphic representations of the results, and drafted the final manuscript. ACA, KP and RB performed the molecular analysis. ACA, RB, RG, JEL and FL helped reviewing the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors are in debt with the infants and their families who participated in this study. We would like to thank the staff members and physicians of the CHET involved in this study, whom were engaged to sample and data collection, and Francesca Pagano for the HPBV testing at the Laboratorio de Biología de Virus (IVIC).
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
Data of the study can be available upon request from the corresponding author (EV).
Ethics approval and consent to participate
The study was approved by the ethical review committee of the IVIC. Informed written consent was obtained from the parents/guardians of the subjects before collecting the stool samples.
Funding
This study was partially supported by Grant LOCTI (Total Venezuela, C.A.) n. 2011000904 and by regular funds from the Instituto Venezolano de Investigaciones Científicas (IVIC), Venezuela.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- RT-PCR
reverse transcriptase polymerase chain reaction
- AGE
acute gastroenteritis
- RV
rotavirus
- HuCV
human calicivirus
- HAdV
human adenovirus
- HAstV
human astrovirus
- HPBV
human picobirnavirus
- HBoV
human bocavirus
- KV
klassevirus/salivirus
- AiV
Aichi virus
- EV
enteroviruses
- CHET
Ciudad Hospitalaria ‘‘Dr. Enrique Tejera”
- IVIC
Instituto Venezolano de Investigaciones Científicas
- MMLV
Moloney Murine Leukemia Virus
- cDNA
complementary DNA
- WHO
World Health Organization
References
- 1.Liu L, Oza S, Hogan D, Chu Y, Perin J, Zhu J, Lawn JE, Cousens S, Mathers C, Black RE. Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the sustainable development goals. Lancet. 2016;388:3027–3035. doi: 10.1016/S0140-6736(16)31593-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD Diarrhoeal Diseases Collaborators Estimates of global, regional, and national morbidity, mortality, and aetiologies of diarrhoeal diseases: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Infect Dis. 2017;17:909–948. doi: 10.1016/S1473-3099(17)30276-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, Jha P, Campbell H, Walker CF, Cibulskis R, Eisele T, Liu L, Mathers C, Child Health Epidemiology Reference Group of WHO and UNICEF Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375:1969–1987. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 4.Tate JE, Burton AH, Boschi-Pinto C, Steele AD, Duque J, Parashar UD, WHO coordinated Global Rotavirus Surveillance Network 2008 estimate of worldwide rotavirus-associated mortality in children younger than 5 years before the introduction of universal rotavirus vaccination programmes: a systematic review and meta-analysis. Lancet Infect Dis. 2012;2012(12):136–141. doi: 10.1016/S1473-3099(11)70253-5. [DOI] [PubMed] [Google Scholar]
- 5.Lanata CF, Fischer-Walker CL, Olascoaga AC, Torres CX, Aryee MJ, Black RE, Child Health Epidemiology Reference Group of the World Health Organization and UNICEF Global causes of diarrheal disease mortality in children < 5 years of age: a systematic review. PLoS ONE. 2013;8(9):e72788. doi: 10.1371/journal.pone.0072788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim A, Chang JY, Shin S, Yi H, Moon JS, Ko JS, Oh S. Epidemiology and factors related to clinical severity of acute gastroenteritis in hospitalized children after the introduction of rotavirus vaccination. J Korean Med Sci. 2017;32:465–474. doi: 10.3346/jkms.2017.32.3.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spina A, Kerr KG, Cormican M, Barbut F, Eigentler A, Zerva L, Tassios P, Popescu GA, Rafila A, Eerola E, Batista J, Maass M, Aschbacher R, Olsen KE, Allerberger F. Spectrum of enteropathogens detected by the FilmArray GI Panel in a multicentre study of community-acquired gastroenteritis. Clin Microbiol Infect. 2015;21:719–728. doi: 10.1016/j.cmi.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 8.Thongprachum A, Khamrin P, Pham NT, Takanashi S, Okitsu S, Shimizu H, Maneekarn N, Hayakawa S, Ushijima H. Multiplex RT-PCR for rapid detection of viruses commonly causing diarrhea in pediatric patients. J Med Virol. 2017;89:818–824. doi: 10.1002/jmv.24711. [DOI] [PubMed] [Google Scholar]
- 9.Vizzi E, Piñeros OA, Oropeza MD, Naranjo L, Suárez JA, Fernández R, Zambrano JL, Celis A, Liprandi F. Human rotavirus strains circulating in Venezuela after vaccine introduction: predominance of G2P[4] and reemergence of G1P[8] Virol J. 2017;14:58. doi: 10.1186/s12985-017-0721-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Simpson R, Aliyu S, Iturriza-Gómara M, Desselberger U, Gray J. Infantile viral gastroenteritis: on the way to closing the diagnostic gap. J Med Virol. 2003;70:258–262. doi: 10.1002/jmv.10386. [DOI] [PubMed] [Google Scholar]
- 11.Liu Y, Xu ZQ, Zhang Q, Jin M, Yu JM, Li JS, Liu N, Cui SX, Kong XY, Wang H, Li HY, Cheng WX, Duan ZJ. Simultaneous detection of seven enteric viruses associated with acute gastroenteritis by a multiplexed luminex-based assay. J Clin Microbiol. 2012;50:2384–2389. doi: 10.1128/JCM.06790-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Valentini D, Vittucci AC, Grandin A, Tozzi AE, Russo C, Onori M, Menichella D, Bartuli A, Villani A. Coinfection in acute gastroenteritis predicts a more severe clinical course in children. Eur J Clin Microbiol Infect Dis. 2013;32:909–915. doi: 10.1007/s10096-013-1825-9. [DOI] [PubMed] [Google Scholar]
- 13.Koh H, Baek SY, Shin JI, Chung KS, Jee YM. Coinfection of viral agents in Korean children with acute watery diarrhea. J Korean Med Sci. 2008;23:937–940. doi: 10.3346/jkms.2008.23.6.937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glass RI, Bresee J, Jiang B, Gentsch J, Ando T, Fankhauser R, Noel J, Parashar U, Rosen B, Monroe SS. Gastroenteritis viruses: an overview. vol. 38. In: Novartis Found Symposium 238; New York: Wiley; 2001. p. 5–19. (discussion 19–25). [DOI] [PubMed]
- 15.Wilhelmi I, Roman E, Sánchez-Fauquier A. Viruses causing gastroenteritis. Clin Microbiol Infect. 2003;9:247–262. doi: 10.1046/j.1469-0691.2003.00560.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.De Benedictis P, Schultz-Cherry S, Burnham A, Cattoli G. Astrovirus infections in humans and animals—molecular biology, genetic diversity, and interspecies transmissions. Infect Genet Evol. 2011;11:1529–1544. doi: 10.1016/j.meegid.2011.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sdiri-Loulizi K, Gharbi-Khélifi H, de Rougemont A, Chouchane S, Sakly N, Ambert-Balay K, Hassine M, Guédiche MN, Aouni M, Pothier P. Acute infantile gastroenteritis associated with human enteric viruses in Tunisia. J Clin Microbiol. 2008;46:1349–1355. doi: 10.1128/JCM.02438-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jiang H, Holtz LR, Bauer I, Franz CJ, Zhao G, Bodhidatta L, Shrestha SK, Kang G, Wang D. Comparison of novel MLB-clade, VA-clade and classic human astroviruses highlights constrained evolution of the classic human astrovirus nonstructural genes. Virology. 2013;436:8–14. doi: 10.1016/j.virol.2012.09.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ouédraogo N, Kaplon J, Bonkoungou IJ, Traoré AS, Pothier P, Barro N, Ambert-Balay K. Prevalence and genetic diversity of enteric viruses in children with diarrhea in Ouagadougou, Burkina Faso. PLoS ONE. 2016;19(11):e0153652. doi: 10.1371/journal.pone.0153652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pham NT, Trinh QD, Chan-It W, Khamrin P, Shimizu H, Okitsu S, Mizuguchi M, Ushijima H. A novel RT-multiplex PCR for detection of Aichi virus, human parechovirus, enteroviruses, and human bocavirus among infants and children with acute gastroenteritis. J Virol Methods. 2010;169:193–197. doi: 10.1016/j.jviromet.2010.07.038. [DOI] [PubMed] [Google Scholar]
- 21.Yamashita T, Kobayashi S, Sakae K, Nakata S, Chiba S, Ishihara Y, Isomura S. Isolation of cytopathic small round viruses with BS-C-1 cells from patients with gastroenteritis. J Infect Dis. 1991;164:954–957. doi: 10.1093/infdis/164.5.954. [DOI] [PubMed] [Google Scholar]
- 22.Holtz L, Finkbeiner S, Zhao G, Kirkwood C, Girones R, Pipas J, Wang D. Klassevirus 1, a previously undescribed member of the family Picornaviridae, is globally widespread. Virol J. 2009;6:86. doi: 10.1186/1743-422X-6-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chansaenroj J, Tuanthap S, Thanusuwannasak T, Duang-In A, Klinfueng S, Thaneskongtong N, Vutithanachot V, Vongpunsawad S, Poovorawan Y. Human enteroviruses associated with and without diarrhea in Thailand between 2010 and 2016. PLoS ONE. 2017;27(12):e0182078. doi: 10.1371/journal.pone.0182078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ambert-Balay K, Lorrot M, Bon F, Giraudon H, Kaplon J, Wolfer M, Lebon P, Gendrel D, Pothier P. Prevalence and genetic distribution of Aichi virus strains in stool samples from community and hospitalized patients. J Clin Microbiol. 2008;46:1252–1258. doi: 10.1128/JCM.02140-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alcalá A, Vizzi E, Rodríguez-Díaz J, Zambrano JL, Betancourt W, Liprandi F. Molecular detection and characterization of Aichi viruses in sewage-polluted waters of Venezuela. Appl Environ Microbiol. 2010;76:4113–4115. doi: 10.1128/AEM.00501-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li L, Victoria J, Kapoor A, Blinkova O, Wang C, Babrzadeh F, Mason CJ, Pandey P, Triki H, Bahri O, Oderinde BS, Baba MM, Bukbuk DN, Besser JM, Bartkus JM, Delwart EL. A novel picornavirus associated with gastroenteritis. J Virol. 2009;83:12002–12006. doi: 10.1128/JVI.01241-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Han TH, Kim CH, Chung JY, Park SH, Hwang ES. Klassevirus infection in children, South Korea. Emerg Infect Dis. 2010;16:1623–1625. doi: 10.3201/eid1610.100539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Itta KC, Patil T, Kalal S, Ghargi KV, Roy S. Salivirus in children with diarrhoea, western India. Int J Infect Dis. 2016;52:14–15. doi: 10.1016/j.ijid.2016.09.015. [DOI] [PubMed] [Google Scholar]
- 29.Salinas B, González G, González R, Escalona M, Materán M, Pérez-Schael I. Epidemiologic and clinical characteristics of rotavirus disease during five years of surveillance in Venezuela. Pediatr Infect Dis J. 2004;23:S161–S167. doi: 10.1097/01.inf.0000142465.25992.c3. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization (WHO) A manual for the treatment of diarrhea: for use by physicians and other senior health workers. Geneva: World Health Organization; 2005. [Google Scholar]
- 31.O’Ryan ML, et al. Rotavirus-associated medical visits and hospitalizations in South America: a prospective study at three large sentinel hospitals. Pediatr Infect Dis J. 2001;20:685–693. doi: 10.1097/00006454-200107000-00009. [DOI] [PubMed] [Google Scholar]
- 32.Méndez-Castellano H, De Méndez MC. Estratificación social y biología humana: método Graffar modificado. Arch Venez Pueric Pediatr. 1986;49:93–104. [Google Scholar]
- 33.González R, Rivero L. Genetic diversity of rotavirus group a: correlation between G3 type and severity of the infection, Valencia, Venezuela. Invest Clin. 2013;54:34–46. [PubMed] [Google Scholar]
- 34.Farkas T, Zhong WM, Jing Y, Huang PW, Espinosa SM, Martinez N, Morrow AL, Ruiz-Palacios GM, Pickering LK, Jiang X. Genetic diversity among sapoviruses. Arch Virol. 2004;149:1309–1323. doi: 10.1007/s00705-004-0296-9. [DOI] [PubMed] [Google Scholar]
- 35.Allard A, Girones R, Juto P, Wadell G. Polymerase chain reaction for detection of adenoviruses in stool samples. J Clin Microbiol. 1990;28:2659–2667. doi: 10.1128/jcm.28.12.2659-2667.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Belliot G, Laveran H, Monroe SS. Detection and genetic differentiation of human astroviruses: phylogenetic grouping varies by coding region. Arch Virol. 1997;142:1323–1334. doi: 10.1007/s007050050163. [DOI] [PubMed] [Google Scholar]
- 37.Belliot GM, Fankhauser RL, Monroe SS. Characterization of “Norwalk-like viruses” and astroviruses by liquid hybridization assay. J Virol Methods. 2001;91:119–130. doi: 10.1016/S0166-0934(00)00254-8. [DOI] [PubMed] [Google Scholar]
- 38.Yamashita T, Sugiyama M, Tsuzuki H, Sakae K, Suzuki Y, Miyazaki Y. Application of a reverse transcription-PCR for identification and differentiation of Aichi virus, a new member of the Picornavirus family associated with gastroenteritis in humans. J Clin Microbiol. 2000;38:2955–2961. doi: 10.1128/jcm.38.8.2955-2961.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shen S, Desselberger U, McKee TA. The development of an antigen capture polymerase chain reaction assay to detect and type human enteroviruses. J Virol Methods. 1997;65:139–144. doi: 10.1016/S0166-0934(97)02181-2. [DOI] [PubMed] [Google Scholar]
- 40.Rosen BI, Fang ZY, Glass RI, Monroe SS. Cloning of human picobirnavirus genomic segments and development of an RT-PCR detection assay. Virology. 2000;25(277):316–329. doi: 10.1006/viro.2000.0594. [DOI] [PubMed] [Google Scholar]
- 41.Oh DY, Gaedicke G, Schreier E. Viral agents of acute gastroenteritis in German children: prevalence and molecular diversity. J Med Virol. 2003;71:82–93. doi: 10.1002/jmv.10449. [DOI] [PubMed] [Google Scholar]
- 42.Lekana-Douki SE, Kombila-Koumavor C, Nkoghe D, Drosten C, Drexler JF, Leroy EM. Molecular epidemiology of enteric viruses and genotyping of rotavirus A, adenovirus and astrovirus among children under 5 years old in Gabon. Int J Infect Dis. 2015;34:90–95. doi: 10.1016/j.ijid.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 43.Colomba C, De Grazia S, Giammanco GM, Saporito L, Scarlata F, Titone L, Arista S. Viral gastroenteritis in children hospitalised in Sicily, Italy. Eur J Clin Microbiol Infect Dis. 2006;25:570–575. doi: 10.1007/s10096-006-0188-x. [DOI] [PubMed] [Google Scholar]
- 44.Marie-Cardin A, Gourlain K, Mouterde O, Castignolles N, Hellot MF, Mallet E, Buffet-Janvresse C. Epidemiology of acute viral gastroenteritis in children hospitalized in Rouen, France. Clin Infect Dis. 2002;34:1170–1178. doi: 10.1086/339807. [DOI] [PubMed] [Google Scholar]
- 45.Ouyang Y, Ma H, Jin M, Wang X, Wang J, Xu L, Lin S, Shen Z, Chen Z, Qiu Z, Gao Z, Peng L, Li J. Etiology and epidemiology of viral diarrhea in children under the age of five hospitalized in Tianjin, China. Arch Virol. 2012;157:881–887. doi: 10.1007/s00705-012-1235-9. [DOI] [PubMed] [Google Scholar]
- 46.González GG, Liprandi F, Ludert JE. Molecular epidemiology of enteric viruses in children with sporadic gastroenteritis in Valencia, Venezuela. J Med Virol. 2011;83:1972–1982. doi: 10.1002/jmv.22185. [DOI] [PubMed] [Google Scholar]
- 47.Thongprachum A, Takanashi S, Kalesaran AF, Okitsu S, Mizuguchi M, Hayakawa S, Ushijima H. Four-year study of viruses that cause diarrhea in Japanese pediatric outpatients. J Med Virol. 2015;87:1141–1148. doi: 10.1002/jmv.24155. [DOI] [PubMed] [Google Scholar]
- 48.Pang XL, Honma S, Nakata S, Vesikari T. Human caliciviruses in acute gastroenteritis of young children in the community. J Infect Dis. 2000;181(Suppl 2):S288–S294. doi: 10.1086/315590. [DOI] [PubMed] [Google Scholar]
- 49.Wildermann N, Porto-Espinoza L, Moronta R, Bracho M, Costa L, Callejas D. Detección molecular mediante RT PCR de calicivirus y enterovirus en niños menores de 6 años con síndrome diarreico. Rev Soc Ven Microbiol. 2010;2010(30):1–8. [Google Scholar]
- 50.Zhou HT, Yi HS, Guo YH, Pan YX, Tao SH, Wang B, Chen MJ, Yang M, Yu N. Enterovirus-related diarrhoea in Guangdong, China: clinical features and implications in hand, foot and mouth disease and herpangina. BMC Infect Dis. 2016;16:128. doi: 10.1186/s12879-016-1463-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Holtz LR, Cao S, Zhao G, Bauer IK, Denno DM, Klein EJ, Antonio M, Stine OC, Snelling TL, Kirkwood CD, Wang D. Geographic variation in the eukaryotic virome of human diarrhea. Virology. 2014;468–470:556–564. doi: 10.1016/j.virol.2014.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pongsuwanna Y, Tacharoenmuang R, Prapanpoj M, Sakon N, Komoto S, Guntapong R, Taniguchi K. Monthly distribution of norovirus and sapovirus causing viral gastroenteritis in Thailand. Jpn J Infect Dis. 2017;24(70):84–86. doi: 10.7883/yoken.JJID.2015.440. [DOI] [PubMed] [Google Scholar]
- 53.Chhabra P, Payne DC, Szilagyi PG, Edwards KM, Staat MA, Shirley SH, Wikswo M, Nix WA, Lu X, Parashar UD, Vinjé J. Etiology of viral gastroenteritis in children < 5 years of age in the United States, 2008–2009. J Infect Dis. 2013;208:790–800. doi: 10.1093/infdis/jit254. [DOI] [PubMed] [Google Scholar]
- 54.Rovida F, Campanini G, Piralla A, Adzasehoun KM, Sarasini A, Baldanti F. Molecular detection of gastrointestinal viral infections in hospitalized patients. Diagn Microbiol Infect Dis. 2013;77:231–235. doi: 10.1016/j.diagmicrobio.2013.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dey SK, Shimizu H, Phan TG, Hayakawa Y, Islam A, Salim AF, Khan AR, Mizuguchi M, Okitsu S, Ushijima H. Molecular epidemiology of adenovirus infection among infants and children with acute gastroenteritis in Dhaka City, Bangladesh. Infect Genet Evol. 2009;9:518–522. doi: 10.1016/j.meegid.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 56.Zaraket H, Abou-El-Hassan H, Kreidieh K, Soudani N, Ali Z, Hammadi M, Reslan L, Ghanem S, Hajar F, Inati A, Rajab M, Fakhouri H, Ghanem B, Baasiri G, Melhem NM, Dbaibo G. Characterization of astrovirus-associated gastroenteritis in hospitalized children under five years of age. Infect Genet Evol. 2017;53:94–99. doi: 10.1016/j.meegid.2017.05.016. [DOI] [PubMed] [Google Scholar]
- 57.Pham NT, Khamrin P, Nguyen TA, Kanti DS, Phan TG, Okitsu S, Ushijima H. Isolation and molecular characterization of Aichi viruses from fecal specimens collected in Japan, Bangladesh, Thailand, and Vietnam. J Clin Microbiol. 2007;45:2287–2288. doi: 10.1128/JCM.00525-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Oh DY, Oh DY, Silva PA, Hauroeder B, Diedrich S, Cardoso DD, Schreier E. Molecular characterization of the first Aichi viruses isolated in Europe and in South America. Adv Virol. 2006;151:1199–1206. doi: 10.1007/s00705-005-0706-7. [DOI] [PubMed] [Google Scholar]
- 59.Chuchaona W, Khamrin P, Yodmeeklin A, Kumthip K, Saikruang W, Thongprachum A, Okitsu S, Ushijima H, Maneekarn N. Detection and characterization of Aichi virus 1 in pediatric patients with diarrhea in Thailand. J Med Virol. 2017;89:234–238. doi: 10.1002/jmv.24630. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data of the study can be available upon request from the corresponding author (EV).


