Abstract
Background
Breastfeeding of children, which needs to continue until two years and beyond, is one of the essential requirements for child survival. However, in Ethiopia there is scarcity of literatures on the duration of breastfeeding. Therefore, the aim of this study was to assess the rate of cessation of breastfeeding among mothers with index children aged 2 to 3 years, northwest Ethiopia.
Methods
A retrospective follow-up study was conducted at Debre Markos town from March 1, 2014 to March 30, 2016. A total of 500 mother-child pairs were selected using the systematic random sampling method by moving from house to house with an interval of three eligible houses. A structured questionnaire was used to collect data. The Cox regression model was employed to identify the predictors of breastfeeding cessation.
Results
The proportion of women breastfeeding until 2 years was 13.70 per 1000 person- months. HIV-positive mothers decreased the time of breastfeeding by 3.4 times compared to HIV-negative mothers (AHR = 3.41, 95% CI: 1.96, 5.94). Government employee mothers decreased the time of breastfeeding by 2.8 times compared to housewives (AHR = 2.8, 95% CI: 1.80, 4.40).Better education increased the time of breastfeeding (AHR = 0.45, 95% CI: 0.24, 0.58). Number of children, family income, and place of delivery were the other significant predictors of time to cessation of breastfeeding (p < 0.05).
Conclusion
In this study, the rate of cessation of breastfeeding was good. HIV negative mothers, government employment, number of children, place of delivery, and family monthly income were significant predictors to the time of breastfeeding cessation. Therefore, family planning and breastfeeding education in health institutions are essential to increase breastfeeding duration.
Keywords: Ethiopia, Cessation of breastfeeding, Factors
Background
Breast milk, the first natural food for children, has nutritional, immunological, developmental, and psychological advantages [1]. The World Health Organization (WHO) recommends that children should be breastfed until 2 years of age or beyond [2].The promotion of children breastfeeding until 2 years is one of the indicators of appropriate child feeding practices [3].
Although breastfeeding practice is universal in Africa, where more than 90% of the mothers breastfeed, some mothers initiate the practice late; others do not do it exclusively, and still others cut the duration to less than two years [4]. In the continent, late cessation of breastfeeding (CBF) has greater effects on child morbidity and mortality [5].The problem of malnutrition begins early in life during the first two years due to suboptimal breastfeeding [6]. A meta- analysis study showed that late CBF was associated with elevated risk of pneumonia [7].
The time to breastfeeding cessation varies from country to country. For instance, in America, Iran, and Italy, 60%, 57%, and 12% [8–10] of the mothers ceased breastfeeding before the children were two years of age, respectively. In China, the median breastfeeding duration was 6.0 months in urban groups and 8.0 months in rural groups [11], and it was 8.6 months in the United Arab Emirates [12]. In Pakistan more than half of the mothers (54%) ceased breastfeeding before the children were 6 months of age [13]. In Tanzania, 94.0% of the infants were breastfed till 12–15 months, but the proportion of breastfeeding decreased to 51.1% at 20–23 months of age [14].
Studies done in Lithuania and Norway showed that the time to CBF was associated with maternal factors, such as age, ethnicity, religion, and marital status [15, 16]. Studies done in Brazil, Nigeria, and Kuwait showed that the time to CBF was associated with child sex, place of delivery, maternal education, maternal employment, and family monthly income [17–19]. In addition, health and health service related factors, maternal and child illness [15], multiple births, breastfeeding experience [5], HIV status of the mother [5, 20], mode of delivery [21], place and attendant of delivery, birth interval, and antenatal care [22] were also factors influencing the time to CBF. Similarly, the time to CBF was related to support from father [23], postpartum employment [17], mother’s attitude and knowledge about breastfeeding [18].
The Federal Ministry of Health of Ethiopia has developed a guideline on infant and young child feeding practices [6]. However, the duration of breastfeeding has decreased from time to time [24]. Therefore, this study aimed to assess the rate and predictors of the time to CBF, using survival analysis among mothers who had index children aged two to three years at Debre Markos, northwest Ethiopia.
Methods
Study design and period
A quantitative community-based retrospective follow-up study was conducted between March 2014 and March 2016 to assess the rate of CBF before two years and associated factors among mothers who had index children aged two to three years.
Study setting
Debre Markos town is located at 300 km northwest of Addis Ababa, the capital of Ethiopia. In Debre Markos, there are seven kebeles (the lowest local administrative units). The total population of the town is 101,582, (52,833 female and 48,749 are male). In the town, there are 23,956 women in the reproductive age group (15–49 years) and 2310 children two to three years of age [24]. In the town one referral hospital, three health centers, and two nongovernmental organization clinics provide health care services to the residents.
Sample size, sampling technique, and procedures
For determining the sample size, a single population formula was used with an assumption of 95% confidence interval, marginal error of 5%,and 18% as the proportion of CBF before two years of age [24]. Adding 10% to account for a non-response rate and a design effect of 2 gave us the final sample of 500mother-childpairs.By taking the ratio of the total mother-child pairs of 1632 in five selected kebeles a total sample size of 500 was attained with a sample interval of three.
In the five selected kebeles, a total of 1632 (273,597,300,229 and 233 in each kebele) eligible mother-child pairs were found, out of which 500(84, 183, 92, 70 and 71) eligible participants were selected for each kebele, using the population proportion formula. Mother-child pairs were selected using the systematic random sampling technique with a sample interval of three eligible households. To get eligible mother-child pairs, we moved from block to block of each selected kebele and every household was visited until the required sample size was secured.
Data collection
Data were collected using an interviewer-administered structured questionnaire. The questions were drawn from the literature in the Ethiopian Demographic Health Survey, and we also used some literature on breastfeeding written in the Ethiopian context. The questionnaire comprised socio-demographic, health service, and obstetric related components.
The survival data were collected from mothers with index children aged two to three years. The mothers were asked the date on which they ceased breastfeeding, which was the event of interest. The date of birth of the index child was taken as the starting point of the retrospective follow-up study. The length of time was measured in months (from birth to 3 years of age) and was taken to be the survival time for those who had experienced the event of interest. A mother who ceased breastfeeding before two years was an event of interest, and those who were breastfed during data collection were considered as right censored.
Possible predictors of time to CBF, such as socio-demographic variables, like number of children, birth interval, mode of delivery, breastfeeding experience and place of delivery were studied. In addition to these, ANC follow up, attendant of delivery, breastfeeding counseling before and after delivery, HIV status of the mother, knowledge and attitude about breastfeeding were the other potential factors evaluated in terms of their association with the time to CBF.
Data quality control
In order to maintain the quality of data, the principal investigator trained the five data collectors and one supervisor for one day. A pretest was conducted on 20 mothers from a non-selected kebele. On-site supervision was performed and each copy of the questionnaire was checked for completeness and accuracy before data entry, and incomplete questions were excluded.
Definitions
Early cessation of breastfeeding
Mothers stoppages of breastfeeding before their children are two years of age.
Knowledge
Mothers’ awareness about the advantages and duration of breastfeeding.
Adequate knowledge
If a mother answered at least nine of the twelve knowledge assessment questions correctly.
Favorable attitude
If a mother responded positively to at least nine of the twelve attitude assessment questions.
Statistical analysis
Data were entered, coded and cleaned using Epi-info version7.0statistical software and were then exported to SPSS version 20 for further analysis. The Kaplan-Meier curve was used to measure the probability of surviving the breastfeeding duration.
Incidence rate was calculated as the number of events over the person-months of follow- up. Both bivariate and multivariate Cox proportional regression models were used to identify factors that affected the CBF before two years. Variables with P-value < 0.2 in the bivariate Cox regression model were entered spontaneously into the multivariate Cox regression model to measure the effect of each variable on the hazard function after adjusting the effects of other variables using the Backward LR method. Variables with P-value< 0.05 in the multivariate Cox regression analysis were considered as statistically significant for the CBF before two years.
Results
Socio-demographic, health, and health service-related characteristics
In the study, a total of 500 mother-child pairs were included. Of these, 483 (96.6%) were followed retrospectively. The mean age of the mothers was 28.59 (± 4.95) years, while that of the children was 30.11 (±4.15) months. In this study, the majority of the mothers were married; they were Amhara by ethnicity. Almost half of the mothers were housewives, and one-third completed secondary school [Table 1].
Table 1.
Socio-demographic characteristics of mothers who have index children aged two to three years, northwest Ethiopia 2016 (n = 483)
| Variables | Number | Percent |
|---|---|---|
| Age of mother | ||
| 15–19 | 4 | 0.8 |
| 20–24 | 86 | 17.8 |
| 25–29 | 199 | 41.2 |
| 30–34 | 130 | 26.9 |
| ≥ 35 | 64 | 13.3 |
| Marital status | ||
| Married | 426 | 88.2 |
| Divorced | 13 | 2.7 |
| Widowed | 44 | 9.1 |
| Sex of index child | ||
| Male | 263 | 54.5 |
| Female | 220 | 45.5 |
| Family size | ||
| ≤ 4 | 266 | 55.1 |
| > 4 | 217 | 44.9 |
| Number of children | ||
| ≤ 3 | 419 | 86.7 |
| > 3 | 64 | 13.3 |
| Maternal education | ||
| non educated or Informal education | 91 | 18.8 |
| Primary education | 93 | 19.3 |
| Secondary education | 141 | 29.2 |
| Certificate, and above | 158 | 32.7 |
| Educational status of father | ||
| Not educated or Informal education | 88 | 18.2 |
| Primary education | 70 | 14.5 |
| Secondary education | 119 | 24.6 |
| Certificate and above | 206 | 42.7 |
| Maternal employment | ||
| House wife | 252 | 52.2 |
| Government | 107 | 22.2 |
| Private | 113 | 23.4 |
| Private organization | 11 | 2.3 |
| Family monthly income | ||
| ≤ 29.5$ | 76 | 15.7 |
| 29.6–63.6$ | 89 | 18.4 |
| 63.7–106.8$ | 105 | 21.7 |
| 106.9–161.4$ | 81 | 16.8 |
| ≥ 161.41$ | 132 | 27.3 |
More than half of the mothers (62%) had adequate knowledge, whereas half of them had favorable attitude towards breastfeeding in general, and the majority preferred breastfeeding to formula feeding [Table 2].
Table 2.
Health and health service related characteristics of mothers who have index children aged two to three years at Debre Markos, northwest Ethiopia, 2016 (n = 483)
| Characteristics | Number | Percent |
|---|---|---|
| Antenatal care | ||
| Yes | 455 | 94.2 |
| No | 28 | 5.8 |
| BF counseling during ANC | ||
| Yes | 336 | 69.6 |
| No | 147 | 30.4 |
| Place of delivery | ||
| At home | 53 | 11.0 |
| Government hospital | 326 | 67.5 |
| Government health center | 95 | 19.7 |
| Non government health facility | 9 | 1.8 |
| Mode of delivery | ||
| Vaginal | 441 | 91.3 |
| Cesarean section | 42 | 8.7 |
| Attendant of the delivery | ||
| Health profession | 435 | 90.1 |
| Relative/Friends | 48 | 9.9 |
| Breastfeeding counseling after delivery | ||
| Yes | 370 | 76.6 |
| No | 113 | 23.4 |
| Breastfeeding experience | ||
| Yes | 274 | 57.7 |
| No | 209 | 43.3 |
| Maternal HIV status | ||
| Positive | 28 | 5.8 |
| Negative | 455 | 94.2 |
| Knowledge about breastfeeding | ||
| Adequate | 297 | 61.5 |
| Inadequate | 186 | 38.5 |
| Attitude about breastfeeding | ||
| Favorable | 252 | 52.2 |
| Unfavorable | 231 | 47.8 |
Survival analysis for breastfeeding cessation
The overall person-time of CBF was 11,181 person months. The overall incidence rate of CBF before 2 years of age was 13.70 per 1000 person-months (95% CI: 27.3–35.8). The cumulative survival probability in life table indicated that the percentage of children who remained on breastfeeding for the first two years was 68.5% [Fig. 1].
Fig. 1.
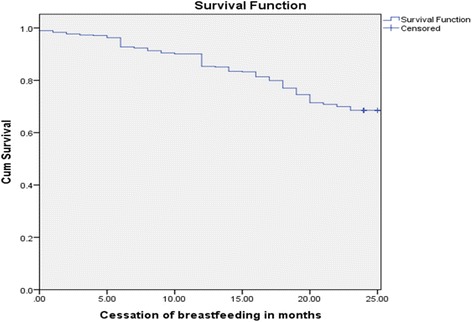
Survival of breastfeeding among mothers who have index children aged two to three years at Debre Markos, northwest Ethiopia, 2016
Multivariate survival analysis
In the bivariate Cox regression model, age, marital status, educational status, occupation of mother, place of delivery, HIV status of the mother, family monthly income, and number of children were independent predictors of CBF before two years of age(p < 0.2). In the multivariate Cox regression model, maternal education, maternal occupation, place of delivery, HIV status of the mother, family monthly income, and number of children were significantly associated with time to cessation of breastfeeding at 95% confidence level (p < 0.05).
In this study, mothers who were government employees decreased the time of breastfeeding by 2.8 times compared to housewife mothers (AHR = 2.81, 95% CI: 1.80–4.38). HIV positive mothers deceased the time of breastfeeding almost by 3.4 times compared to HIV-negative mothers (AHR = 3.42, 95% CI: 1.96–5.94). Mothers with less than three children increased the time of breastfeeding by 57% compared to mothers who had more than three children (AHR = 0.43, 95% CI: 0.28–0.65). Mothers who had certificate and above educational qualification increased the time of breastfeeding almost by 55% compared to less educated mothers (AHR = 0.45, 95% CI: 0.24, 0.85) [Table 3].
Table 3.
Bivariate and multivariate cox regression of CBF among mothers who have index children aged two to three years Debre Markos, northwest Ethiopia 2016 (n = 483)
| Variables | Cessation of breastfeeding | |||
|---|---|---|---|---|
| Yes (%) | No (%) | CHR (95% CI) | AHR (95% CI) | |
| Age of mother (in years) | ||||
| < =24 | 18 (20.0) | 72 (80.0) | 1 | 1 |
| 25–29 | 61 (30.6) | 138 (69.4) | 1.59 (0.94,2.69) | 1.27 (0.73,2.20) |
| 30–34 ≥ 35 |
48 (36.9) | 82 (63.1) | 2.05 (1.19,3.53) | 1.33 (0.72,2.43) |
| 26 (40.6) | 38 (59.4) | 2.48(1.36,4.53) | 1.34 (0.67,2.65) | |
| Marital status | ||||
| Married | 127 (29.8) | 299 (70.2) | 0.61 (0.38,1.00) | 0.77 (0.43,1.37) |
| Divorced | 7 (53.8) | 6 (46.20) | 1.20 (0.51, 2.87) | 0.44 (0.32,2.22) |
| Widowed | 19 (43.2) | 25 (56.8) | 1 | 1 |
| Maternal education | ||||
| Non educated and Informal Education | 32 (35.2) | 59 (64.8) | 1 | 1 |
| Primary education | 24 (25.8) | 69 (74.2) | 0.66 (0.39,1.13) | 0.72 (0.42,1.26) |
| Secondary education | 38 (26.95) | 103 (73.1) | 0.69 (0.44,1.12) | 0.59 (0.34,1.03) |
| Certificate and above | 59 (37.3) | 99 (62.7) | 1.00 (0.65,1.54) | 0.45 (0.24, 0.85)* |
| Educational status of father | ||||
| Non educated or Informal Education | 30 (34.1) | 58 (65.9) | 1 | 1 |
| Primary education | 16 (22.9) | 54 (77.1) | 0.65 (0.36,1.17) | 1.04 (0.52, 2.07) |
| Secondary education | 30 (25.2) | 89 (74.8) | 0.65(0.39,1.08) | 0.93 (0.49,1.77) |
| Certificate and above | 153 (54.3) | 129 (45.7) | 1.06 (0.69,1.61) | 1.04 (0.53, 2.05) |
| Maternal employment | ||||
| House wife | 64 (25.4) | 188 (74.6) | 1 | 1 |
| Government | 58 (54.2) | 49 (45.8) | 2.46 (1.72,3.51) | 2.81(1.80, 4.38)* |
| Private organization | 2 (18.2) | 9 (81.2) | 0.62 (0.15,2.53) | 0.76 0.18, 3.13) |
| Private(self) work | 29 (25.7) | 84 (74.3) | 1.01 (0.65,1.57) | 0.95 (0.61, 1.49) |
| Monthly family income | ||||
| ≤ 29.5$ | 33(43.4) | 43 (56.6) | 1 | 1 |
| 29.6–63.6$ | 17 (19.1) | 72 (80.9) | 0.36 (0.20, 0.64) | 0.29(0.16, 0.54)* |
| 63.7–106.8$ | 27 (25.7) | 78 (74.3) | 0.50 (0.30, 0.83) | 0.40 (0.24, 0.68)* |
| 106.9–161.4$ | 17 (21.0) | 64 (79.0) | 0.38 (0.22, 0.69) | 0.29 (0.16, 0.55)* |
| ≥ 161.41$ | 59 (44.7) | 73 (55.3) | 0.97 (0.63,1.48) | 0.48 (0.29, 0.81)* |
| Antenatal care (ANC) | ||||
| Yes | 144 (31.6) | 311 (68.4) | 1 | 1 |
| No | 9 (32.1) | 19 (67.9) | 1.08 (0.55, 2.11) | 1.13 (0.53,2.38) |
| Family size | ||||
| ≤ 4 | 78 (29.3) | 188 (70.7) | 0.8 (0.58,1.10) | 0.88 (0.58,1.34) |
| > 4 | 75 (34.6) | 142 (65.4) | 1 | 1 |
| Place of delivery | ||||
| At home | 10 (18.9) | 43 (81.1) | 1 | 1 |
| Government hospital | 110 (33.7) | 216 (66.3) | 1.93 (1.01,3.68) | 2.30 (1.15, 4.62)* |
| Health center, post | 33 (31.7) | 71 (68.3) | 1.75 (0.86,3.55) | 2.04 (0.96, 4.32) |
| Attendant of delivery | ||||
| Health professional | 144 (33.1) | 291 (66.9) | 1 | 1 |
| Relative/friend | 9 (18.75) | 39 (81.25) | 0.53 (0.27, 1.04) | 1.08 (0.26, 4.38) |
| Mode of delivery | ||||
| Cesarean section | 18 (42.8) | 24 (57.2) | 1.523 (0.931, 2.49) | 1.3 (0.75, 2.24) |
| Vaginal | 135 (30.6) | 306 (69.4) | 1 | 1 |
| BF counseling on ANC | ||||
| Yes | 128 (34.6) | 242 (65.4) | 1.30 (0.90, 1.87) | 1.29 (0.89, 1.87) |
| No | 25 (22.3) | 87 (77.7) | 1 | 1 |
| Number of Children | ||||
| ≤ 3 | 124 (29.6) | 295(70.4) | 0.57(0.38, 0.86) | 0.43 (0.28, 0.65)* |
| > 3 | 29 (45.3) | 35(54.7) | 1 | 1 |
| Maternal HIV status | ||||
| Positive | 17 (60.7) | 11 (39.3) | 2.66 (1.61, 4.42) | 3.42 (1.96, 5.94)* |
| Negative | 136 (29.9) | 319 (70.1) | 1 | 1 |
| BF Experience | ||||
| Yes | 83 (30.3) | 191 (69.7) | 1 | 1 |
| No | 70 (33.5) | 139 (66.5) | 1.12 (0.82, 1.54) | 1.31 (0.93, 1.85) |
| Attitude of mother | ||||
| Favorable | 74 (29.4) | 178 (70.6) | 1 | 1 |
| Unfavorable | 79 (34.2) | 152 (65.8) | 0.81 (0.59, 1.11) | 0.81 (0.88, 1.71) |
*Statistically significant at P value < 0.05, 1 BF Breastfeeding
CHR Crude hazard ratio, AHR Adjusted hazard ratio
"1" indicates statistically significant variables
Discussion
In this study, 483 mother-child pairs were followed retrospectively for a total of 11,181 person-months. The incidence rate of breastfeeding cessation before two years of age was 13.70 person-months. One-third of the mothers (32%) ceased breastfeeding before two years of age. This prevalence is higher than the national average [24], but lower than that of a study done in Iran (57%) [9].The variation may be due to the fact that the present study considered only urban residents, while the national study considered both urban and rural residents. But the difference between this and the Iranian study may be due to the socio-demographic variations between the two countries.
This study showed that HIV-positive mothers reduced the time of breastfeeding by 3.4 times compared to HIV-negative mothers. This result corresponds to that of a study done in South Africa [5]. The low breastfeeding duration of HIV-positive mothers might be due to the fear of HIV transmission to their children and mothers’ illness due to HIV/AIDS.
In this study, mothers who were better educated increased the time of breastfeeding compared to less educated mothers. This is in line with other findings in South Africa and Kuwait [5, 19] which showed that educational level of mothers influenced breastfeeding duration. The possible explanation might be when mothers are educated, the knowledge of breastfeeding duration and willingness to continue breastfeeding increases compared to non-educated mothers. But a study conducted in India showed that better-educated mothers reduced the time of breastfeeding than less educated ones [25]; this difference might be due to early introduction of supplementary feeding among more educated mothers leading to reduce the time of breastfeeding.
Mothers who had family monthly income of $29.6–63.6 increased the time of breastfeeding by 51% compared to mothers with lower family monthly income. However, a study done in Pakistan [22] showed that mothers who had lower family monthly income increased the time of breastfeeding more than owners of higher family monthly income. The possible reason for the direct relationship between income and breastfeeding duration might be that mothers who had higher family monthly income could have good knowledge about the advantages of breastfeeding.
In this study, mothers with less than four children increased the time of breastfeeding by 57% compared to mothers who had more than four children. This finding is similar with that of a study done in Bangladesh [21].The possible reason for this is that mothers a lower number of children have enough time to continue breastfeeding.
In our study, government employee mothers were more likely to reduce the time of breastfeeding compared to housewife mothers. This finding is in line with those of studies done in Greece and Australia [16, 26]. The explanation for this finding might be that in Ethiopia government employee mothers return to work within a short time (three months) after delivery. In addition to these reasons, in Ethiopia there are no breastfeeding rooms in working areas. This might be the cause of early termination of breastfeeding for government employee mothers.
In Ethiopia, 15% of the births are delivered at health facilities [24]. This study showed that about 89% of the births at Debre Markos town were delivered at health facilities. Mothers who delivered at health institutions decreased the time of breastfeeding compared to mothers who delivered at home, but a study done in India showed that those mothers who delivered at health facility increased the time of breastfeeding [25].The reason might be in India mothers can get better breastfeeding counseling in the health facilities.
Strengths and limitations
The strength of this study was that it assessed breastfeeding duration up to two years (most studies assessed for 1 year); this adds significant variables to the CBF and helps determine the rate of breastfeeding proportion (person months).
This study has potential limitations, like recall bias which may possibly result in under or over estimation of the actual breastfeeding durations. This bias was not fully controlled although interviewers were trained to minimize it by encouraging mothers to remember when they had their index children by relating their deliveries with the calendar for local events. Another limitation of this study was that the authors did not account for mothers who had breast pumps. In fact, as breast pumps are not common in Ethiopia.
Conclusion
The incidence rate of time to CBF before children were two years of age was 13.70 per 1000 person- months (95%CI 27.3–35.8). The mean duration of breastfeeding was longer than in most countries. Family monthly income, educational status of the mother, HIV status of the mother, place of delivery, number of children, and employment of mothers were significantly associated with the time to CBF before two years of age. Therefore, interventions such as family planning and educating HIV positive mothers about the options of breastfeeding are essential to increase breastfeeding duration.
Acknowledgements
We would like to acknowledge the University of Gondar for the ethical clearance. The authors would like to thank the study participants, data collectors, and the supervisor.
Funding
The authors have declared that there was no funding.
Availability of data and materials
The data that support the findings of this study are available from https://github.com/melkamut/breastfeeding-one. Full data set and materials pertaining to this study can be obtained from corresponding author on reasonable request.
Abbreviations
- AHR
Adjusted Hazard Ratio
- ANC
Antenatal Care
- BF
Breast Feeding
- CBF
Cessation of Breast Feeding
- CHR
Crude Hazard Ratio
- EDHS
Ethiopian Demographic and Health Survey
- IYCF
Infant and Young Child Feeding
- NGO
None Governmental Organizations
- WHO
World Health Organization
Authors’ contributions
MT made the draft proposal and acquisition and analysis of data, KA worked on the interpretation and discussion of results. BM involved in drafting and revising the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Ethical clearance was obtained from the Ethical Review Committee of the Institute of Public Health the University of Gondar (Ref: 2284/06/08). An official permission letter was obtained from Debre Markos town Health Office. Informed consent was obtained from study participants in their local language after explaining the purpose of the study, potential risks and benefits of partaking in the study, and the right to withdraw from the study at any time. The participants were also assured that the data was confidential. In this study we included only mothers having their children age 2 and above years, in this case there were no mothers having age less than 18 years in this study, therefore we took informed written parental consent.
Consent for publication
Not applicable.
Competing interest
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Melkamu Tamir Hunegnaw, Phone: +251-910-30-59-24, Email: melkamutamir@gmail.com.
Kassahun Alemu Gelaye, Phone: + 251-911-75-24-66, Email: alemukass@yahoo.comg.
Bekri Mohammed Ali, Phone: +251-920-25-57-14, Email: bekrim12@gmail.com.
References
- 1.Riskin A, Breast BD. Is best--human milk for premature infants. Harefuah. 2003;142(3):217–222. [PubMed] [Google Scholar]
- 2.World Health Organization,Global Strategy for Infant and Young Child Feeding, world health Organization, Editor 2003: http://www.breastfeedingcanada.ca/documents/Global_Strategy_for_Infant_And_Young_Child_Feeding.pdf
- 3.World Health Organization, Indicators for assessing infant and young child feeding practices, 2008, World Health Organization: Geneva. http://apps.who.int/iris/bitstream/10665/43895/1/9789241596664_eng.pdf
- 4.Trends NF. In infant feeding in developing countries. Pediatrics. 1984;74(4):648–666. [PubMed] [Google Scholar]
- 5.Doherty T, Sanders D, Jackson D, Swanevelder S, Lombard C, Zembe W, Chopra M, Goga A, Colvin M, Fadnes TL, Engebretsen IM. Early cessation of breastfeeding amongst women in South Africa: an area needing urgent attention to improve child health. BMC Pediatr. 2012;12(1):105. doi: 10.1186/1471-2431-12-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ethiopian National Strategy on Infant and Young Child Feeding, 2004, Ministry of Health: Ethiopia. https://extranet.who.int/nutrition/gina/sites/default/files/ETH%202004%20National%20Strategy%20for%20Infant%20and%20Young%20Child%20Feeding.pdf
- 7.Lamberti LM, Zakarija-Grković I, Walker CL, Theodoratou E, Nair H, Campbell H, Black RE. Breastfeeding for reducing the risk of pneumonia morbidity and mortality in children under two: a systematic literature review and meta-analysis. BMC Public Health. 2013;13(3):S18. doi: 10.1186/1471-2458-13-S3-S18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Odom EC, Li R, Scanlon KS, Perine CG. Grummer_Strawn L. Reasons for earlier than desired cessation of breastfeeding. Pediatrics. 2013;131(3):e726–32. doi: 10.1542/peds.2012-1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olang B, Heidarzadeh A, Strandvik B, Yngve A. Reasons given by mothers for discontinuing breastfeeding in Iran. Int Breastfeed J. 2012;7(1):7. doi: 10.1186/1746-4358-7-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carletti C, Pani P, Knowles A, Monasta L, Montico M, Cattaneo A. Breastfeeding to 24 months of age in the northeast of Italy: a cohort study. Breastfeed Med. 2011;6(4):177–182. doi: 10.1089/bfm.2011.0019. [DOI] [PubMed] [Google Scholar]
- 11.Huang L, Zeng G, Li M, Ran L, Chen K, Pang X, Yu L. Duration of breastfeeding and its relevant influencing factors in urban and rural areas of Chengdu. Wei sheng yan jiu=Journal of hygiene research. 2012;41(5):760–764. [PubMed] [Google Scholar]
- 12.Radwan H. Patterns and Determinants of breastfeeding and complementary feeding practices of emirates mothers in the United Arab Emirates. BMC Public Health. 2013;13(1):171. doi: 10.1186/1471-2458-13-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saeed MA, Badar S, Yasmeen S, Hussain W. Discontinuation of breast feeding in infants. J Rawalpindi Medical College (JRMC) 2013;17(2):281–283. [Google Scholar]
- 14.Victor R, Baines SK, Agho KE, Dibley MJ. Determinants of breastfeeding indicators among children less than 24 months of age in Tanzania: a secondary analysis of the 2010 Tanzania demographic and health survey. BMJ Open. 2013;3(1):e001529. doi: 10.1136/bmjopen-2012-001529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Afrose L, Banua B, Ahmeda KR, Khanoma K. Factors associated with knowledge about breastfeeding among female garment workers in Dhaka city. WHO South-East Asia Journal of Public Health. 2012;1(3):249–255. doi: 10.4103/2224-3151.207021. [DOI] [PubMed] [Google Scholar]
- 16.Bakoula C, Veltsista A, Prezerakou A, Moustaki M, Fretzayas A, Nicolaidou P. Working mothers breastfeed babies more than housewives. Acta Paediatr. 2007;96(4):510–515. doi: 10.1111/j.1651-2227.2006.00185.x. [DOI] [PubMed] [Google Scholar]
- 17.Bai DL, Fong DY, Tarrant M. Factors associated with breastfeeding duration and exclusivity in mothers returning to paid employment postpartum. Matern Child Health J. 2015;19(5):990–999. doi: 10.1007/s10995-014-1596-7. [DOI] [PubMed] [Google Scholar]
- 18.Mbada CE, Olowookere AE, Faronbi JO, Oyinlola-Aromolaran FC, Faremi FA, Ogundele AO, Awotidebe TO. Ojo AA, Augustine OA. Knowledge, attitude and techniques of breastfeeding among Nigerian mothers from a semi-urban community. BMC research notes. 2013;6(1):552. doi: 10.1186/1756-0500-6-552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dashti M, Scott JA, Edwards CA, Al-Sughayer M. Predictors of breastfeeding duration among women in Kuwait: results of a prospective cohort study. Nutrients. 2014;6(2):711–728. doi: 10.3390/nu6020711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haile D, Belachew T, Birhanu G, Setegn T, Biadgilign S. Predictors of breastfeeding cessation among HIV infected mothers in southern Ethiopia: a survival analysis. PLoS One. 2014;9(3):e90067. doi: 10.1371/journal.pone.0090067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Akter S, Rahman MM. Duration of breastfeeding and its correlates in Bangladesh. J Health Popul Nutr. 2010;28(6):595–601. doi: 10.3329/jhpn.v28i6.6608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hazir T, Akram DS, Nisar YB, Kazmi N, Agho KE, Abbasi S, Khan AM, Dibley MJ. Determinants of suboptimal breast-feeding practices in Pakistan. Public Health Nutr. 2013;16(4):659–672. doi: 10.1017/S1368980012002935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Olayemi O, Aimakhu CO, Bello FA, Motayo VO, Ogunleye AA, Odunukan OW, Ojengbede OA. The influence of social support on the duration of breast-feeding among antenatal patients in Ibadan. J Obstet Gynaecol. 2007;27(8):802–805. doi: 10.1080/01443610701666876. [DOI] [PubMed] [Google Scholar]
- 24.Ethiopia Demographic and Health Survey, 2011, Central Statistical Agency: Addis Ababa. https://www.unicef.org/ethiopia/ET_2011_EDHS.pdf
- 25.Malhotra R, Noheria A, Amir O, Ackerson LK, Subramanian SV. Determinants of termination of breastfeeding within the first 2 years of life in India: evidence from the National Family Health Survey-2. Maternal & child nutrition. 2008;4(3):181–193. doi: 10.1111/j.1740-8709.2007.00130.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Scott JA, Binns CW, Oddy WH, Graham KI. Predictors of breastfeeding duration: evidence from a cohort study. Pediatrics. 2006;117(4):e646–e655. doi: 10.1542/peds.2005-1991. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from https://github.com/melkamut/breastfeeding-one. Full data set and materials pertaining to this study can be obtained from corresponding author on reasonable request.


