Abstract
BACKGROUND
The National Breast and Cervical Cancer Early Detection Program (NBCCEDP) is the largest cancer screening program for low-income women in the United States. This study updates previous estimates of the costs of delivering preventive cancer screening services in the NBCCEDP.
METHODS
We developed a standardized web-based cost-assessment tool to collect annual activity-based cost data on screening for breast and cervical cancer in the NBCCEDP. Data were collected from 63 of the 66 programs that received funding from the Centers for Disease Control and Prevention during the 2006/2007 fiscal year. We used these data to calculate costs of delivering preventive public health services in the program.
RESULTS
We estimated the total cost of all NBCCEDP services to be $296 (standard deviation [SD], $123) per woman served (including the estimated value of in-kind donations, which constituted approximately 15% of this total estimated cost). The estimated cost of screening and diagnostic services was $145 (SD, $38) per women served, which represented 57.7% of the total cost excluding the value of in-kind donations. Including the value of in-kind donations, the weighted mean cost of screening a woman for breast cancer was $110 with an office visit and $88 without, the weighted mean cost of a diagnostic procedure was $401, and the weighted mean cost per breast cancer detected was $35,480. For cervical cancer, the corresponding cost estimates were $61, $21, $415, and $18,995, respectively.
CONCLUSIONS
These NBCCEDP cost estimates may help policy makers in planning and implementing future costs for various potential changes to the program.
Keywords: economic cost, cost analysis, NBCCEDP, breast cancer screening, cervical cancer screening, program evaluation
INTRODUCTION
In the United States, screening for breast and cervical cancer is recommended by the U.S. Preventive Services Task Force.1 Screening for these cancers has been reported to be effective in reducingmorbidity and mortality associated with these cancers through early detection and treatment.2,3
Despite evidence showing a modest decrease in incidence and mortality rates associated with breast and cervical cancers,4 little progress has been achieved in increasing screening rates for these cancers over the last decade.5 In addition, screening rates have been substantially lower than the national average among low-income women who are uninsured or underinsured,6,7 and these women have been found to be more likely to present with advanced-stage cancer than privately insured women.7,8 To reduce disparities in cancer mortality rates and provide low-income uninsured women with greater access to cancer screening and diagnostic services, in 1990 the US Congress passed the Breast and Cervical Cancer Mortality Prevention Act (Public Law 101–354). Detailed descriptions of this law and of the National Breast and Cervical Cancer Early Detection Program (NBCCEDP), which was formed as a result of it, have been presented previously9 and are also provided elsewhere in this Supplement.10 Since 2000, with the implementation of the Breast and Cervical Cancer Prevention and Treatment Act, women diagnosed with cancer through the NBCCEDP are enrolled in state Medicaid programs to receive treatment.
As the largest organized cancer screening program in the United States, the NBCCEDP is a complex system of 68 individual screening programs, each with its own service delivery model. Because of this diversity of service delivery models, the operating efficiency of each screening program within the NBCCEDP needs to be assessed separately. In 2005, we began to systematically collect cost data to comprehensively address economic issues related to the NBCCEDP. The NBCCEDP cost estimates presented in this article update and extend previously published estimates of the costs of delivering cancer screening services through the NBCCEDP during the 2003/2004 fiscal year.9
MATERIALS AND METHODS
Study Population and Definitions
The previous study of NBCCEDP service costs was based on data collected from only 9 program grant recipients.9 This study is based on data collected from 63 of the 66 grantees that received Centers for Disease Control and Prevention (CDC) funding during the 2006/2007 fiscal year. On the basis of these data, we calculated the following 8 outcomes: 1) the mean and median number of women served and the associated total program costs, 2) the cost per woman served with and without in-kind donations, 3) the cost per woman served for clinical services, 4) the cost per woman screened for breast and cervical cancer with and without office visits, 5) the cost per case of cancer detected, 6) the cost of diagnostic procedures performed during an office visit, 7) the cost and percent distribution per woman served by each program component, and 8) the relationship between the average cost per woman served and the number of women served by the various grant recipients.
In our analyses, “women served” referred to women who received a screening test in the program plus women who received a screening test outside the program but were referred to the program for a diagnostic procedure; “cost per woman served” referred to the cost of screening a woman in the program plus the cost of diagnostic procedure for a woman who was screened outside the program but was referred to the program at a diagnostic stage; “women screened” referred only to those who received a screening test through the NBCCEDP; “screening services” referred to either mammography and clinical breast examination for breast cancer screening or a Papanicolaou (Pap) test for cervical cancer screening; and “in-kind donations” referred to our estimates of the value of the time of volunteers and the value of donated materials for which an NBCCEDP grantee did not have to pay. We included the estimated value of these “free” resources in some of our cost estimates so that the estimates would reflect the full economic cost of providing cancer screening services in the NBCCEDP.
CAT Development and Data Collection
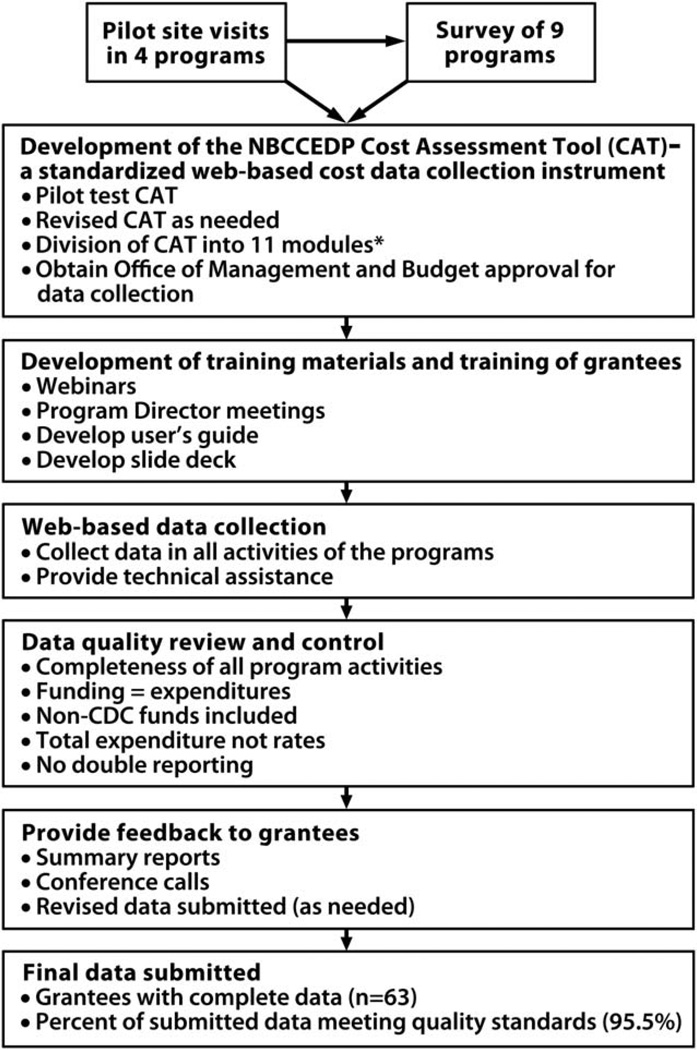
To adequately collect economic costs related to NBCCEDP, we developed a cost assessment tool (CAT). The CAT is a standardized web-based instrument designed to collect activity-based cost data from the NBCCEDP (or other cancer screening programs). Details of the development of this tool and an overview of its 11 modules have been presented previously.11 Figure 1 summarizes the process used to obtain primary data for this study, which included developing the CAT, developing training materials to train grantees on how to use the CAT to collect cost data in their respective programs.
Figure 1.
Summary of CAT Development and Activity-Based Cost Data Collection Process.
*The 11 modules in CAT are: 1) Grantee details; (2) Total funding; (3) In-kind contribution, (4) Personnel expenditure: (5) Consultant expenditure; (6) Screening expenditure; (7) Expenditure for non-screening activities performed by health departments/centers or providers; (8) Expenditures associated with contracts, materials, travel and services; (9) Administrative expenditures; (10) Resource allocation to breast versus cervical cancer screening for selected activities; and (11) Screening and diagnostic activities supported through the use of non-federal funds.
We used the CAT to collect cost data for the 2006/2007 fiscal year. Program activities and costs related to all funding sources, including the CDC and state and other organizations, were collected in the CAT and reported in this study. Data were collected for clinical and health promotion activities from each NBCCEDP grantee. “Clinical activities” referred to screening, diagnostic follow-up for abnormal results and referral for treatment. “Health promotion activities” referred to activities related to program management, patient support/case management, data management, quality assurance and improvement, partnerships, professional development, recruitment, public education, program evaluation, and administration. We also collected data on the number of women screened and served by NBCCEDP grantees with the use of non-CDC funds as well as with the use of CDC funds.
Data Quality Review and Control
We performed the following steps to ensure the accuracy of data collected with the CAT: 1) checked to ensure that all CAT modules were fully and accurately completed; 2) reviewed records to ensure that data submitted with the CAT agreed with information grantees provided to CDC in their financial status report; 3) requested that grantees report all funds used in the program, including non-CDC funds received from various sources; 4) reviewed the submitted data to determine whether grantees reported their actual total expenditures for clinical (screening and diagnostic) procedures rather than their rates per procedure; and 5) checked to ensure that grantees did not double-report cost data. For grantees with incomplete or inaccurate data, we conducted several rounds of follow-up telephone calls to clarify inconsistencies, and in some cases we required grantees to resubmit their data. We excluded data from 3 grantees that did not meet our data quality criteria, leaving us with data from 63 grantees for our analysis.
Program Outcome Measures
We obtained the following program outcome measures from the NBCCEDP surveillance database and the CDC CAT for non-CDC funded screens: 1) the number of women screened for breast cancer and the number screened for cervical cancer with and without CDC funds, 2) the number of women served in the program with and without CDC funds, and 3) the number of breast and cervical cancer cases and precancerous tumors detected. Breast cancer cases include invasive cancer and carcinoma in situ (CIS), whereas cervical cancer cases include invasive tumors, high-grade cervical intraepithelial neoplasia (CIN; ie, CIN2, CIN3, or CIS), and adenocarcinoma in situ.
Data Analysis
The data collected in the CAT and the NBCCEDP surveillance database were analyzed using Stata v10 (Stata, College Station, TX). The analysis was conducted from a program perspective; therefore, the article only examines direct costs of providing preventive cancer screening services and diagnostic procedures to the women participating in the program. Because the study was conducted during a 1-year period, we did not discount costs and outcome measures.
Calculating Program Costs
Costs were calculated with and without in-kind donations. For all cost calculations, we present the arithmetic mean, the weighted mean, and the median. Using the arithmetic mean and median, we first calculated the total number of women served per program, the cumulative number of women screened with and without CDC funds, the number of women who received diagnostic follow-up procedures for abnormal results, and the number of cancer cases detected by stage. To express variation across programs, we calculated the standard deviation (SD) for reported means and interquartile ranges surrounding the medians. These calculations were performed separately for breast and for cervical cancer, respectively. Second, we calculated mean and median values for program costs in a similar manner. Third, we calculated the weighted mean cost of providing preventive health services weighted by the number of women served or screened in each program. We also used weighted mean values to estimate cost per woman served by program component as well as the corresponding percent distribution by program component. Further, we explored the relationship between the calculated average cost per woman served and the number of women served.
RESULTS
During the 1-year period, the NBCCEDP as a whole served 1.02 million women at a total cost of $255.53 million, not counting the estimated value of in-kind donations (Table 1). Individual NBCCEDP grantees served an average of 16,135 women (SD, 30,165) at an average cost of $4.06 million (SD, $6.41 million). The weighted mean cost per woman served excluding the value of in-kind donations was $251.38 (SD, $76.90), of which $144.53 (SD, $38.12) was for clinical services. The total weighted mean cost per woman served including the $45.05 (SD, $73.89) estimated value of in-kind donations was $296.44 (SD, $122.55).
TABLE 1.
Estimated Outcomes and Costs Among 63a Recipients of CDC Funds for NBCCEDP Activities During 2006/2007 Fiscal Year
| Program Outcomes | ||
| Total number of women served | 1,016,492 | |
| Mean number served (SD) | 16,135 (30,165) | |
| Median number served (25th, 75th percentiles) | 10,963 (4043, 17,504) | |
| Program Costs | With In-Kind Donations | Without In-Kind Donations |
| Total program costs, in millions of $ | 301.33 | 255.53 |
| Mean cost per program (SD), in millions of $ | 4.78 (6.90) | 4.06 (6.41) |
| Median cost per program (25th, 75th percentiles), in millions of $ | 3.21 (1.50, 5.05) | 2.46 (1.23, 4.60) |
| Weighted mean cost per woman served (SD), $ | 296.44 (122.55) | 251. 38 (76.90) |
| Weighted Mean cost of clinical services per woman servedb (SD), $ | — | 144.53 (38.12) |
| Mean value of in-kind donations per woman servedc (SD), $ | 45.05 (73.89) | — |
Abbreviations: CDC, Centers for Disease Control and Prevention; NBCCEDP, National Breast and Cervical Cancer Early Detection Program; SD, standard deviation.
Three recipients of CDC funds did not meet data quality criteria for this analysis.
Clinical services include screening and diagnostic services.
In-kind donations are defined as those contributions that strictly represent opportunity cost.
Table 2 presents the weighted mean outcomes and costs for breast and cervical cancer screening in the program. For breast cancer, the calculated average number of women screened by these programs with only CDC funds was 4509 (SD, 4186) and with CDC and non-CDC funds was 7850 (SD, 21,520). For cervical cancer, these estimates were 4858 (SD, 5778) with CDC funds and 6056 (SD, 8220) with and without CDC funds.
TABLE 2.
Weighted Mean Outcomes and Costs for Breast and Cervical Cancer Screening in the Program During 2006/2007 Fiscal Year
| Breast Cancer Screening, Weighted Mean (SD) |
Cervical Cancer Screening, Weighted Mean (SD) |
|
|---|---|---|
| Program outcome | ||
| Women screened with NBCCEDP funds | 4,509 (4,186) | 4,858 (5,778) |
| Women screened with all funds (ie, CDC + 1 non-CDC funds) | 7,850 (21,520) | 6,056 (8,220) |
| Women receiving diagnostic follow-up visits for abnormal results | 1,969 (2,998) | 491 (619) |
| Program cost ($)a | ||
| Cost of screening with an office visit | 109.77 (43.80) | 61.38 (24.82) |
| Cost of a diagnostic procedure | 400.68 (128.39) | 415.16 (347.13) |
| Cost of screening mammography without an office visitb | 88.44 (31.23) | — |
| Cost of Pap smear without an office visitc | — | 20.62 (18.86) |
Two programs were dropped from these calculations because of insufficient screening data.
No data on the number of mammograms that were performed using non-CDC funds were available, so this calculation includes only the 28 programs with complete data that did not perform any mammograms using non-CDC funds.
No data on the number of Pap tests that were performed using non-CDC funds was available, so this calculation includes only the 33 programs with complete data that did not perform any Pap tests using non-CDC funds.
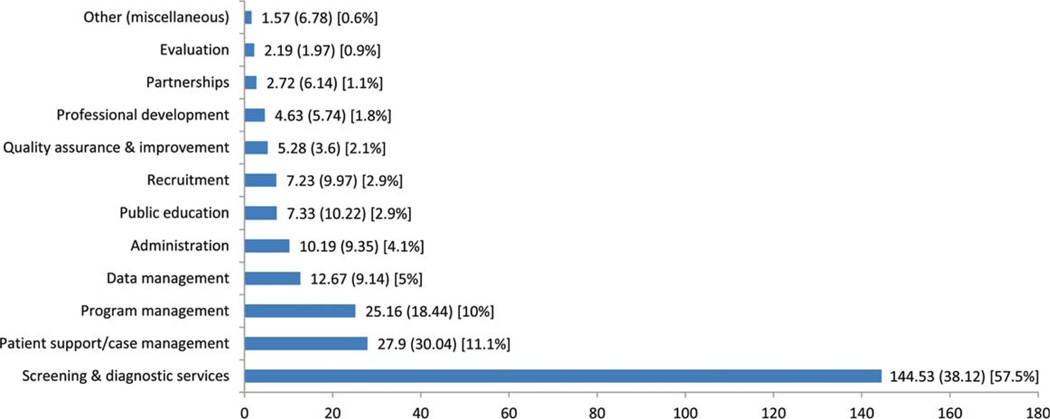
Using the weighted mean approach, the cost of screening with an office visit was $109.77 (SD, $43.80) for breast cancer and $61.38 (SD, $24.82) for cervical cancer (Table 2). Without an office visit, the weighted mean cost was $88.44 (SD, $31.23) for breast cancer and $20.62 (SD, $18.86) for cervical cancer. The weighted mean cost of a diagnostic procedure was $400.68 (SD, $128.39) for breast cancer and $415.16 (SD, $347.13) for cervical cancer. The estimated distribution of weighted mean cost and percent distribution per woman served by a program component is presented in Figure 2. Screening and diagnostic services accounted for the highest cost, of $144.53 (SD, $38.12), which represented 57.5% of total program costs per woman served (Fig. 2). Patient support/case management was the second highest, with an estimated weighted average cost of $27.90 (SD, $30.04) per woman served (11.1% of the total costs). Program management was the third highest, with an estimated weighted average cost of $25.16 (SD, $18.44) per woman served (10.0% of the total costs).
Figure 2.
Estimated Distribution of Weighted Mean Costs and Percent Distribution per Woman Served, by Program Component. Estimates exclude the value of in-kind contributions, the numbers in parentheses are standard deviation, and the numbers in brackets are % distribution of cost per woman served by program component.
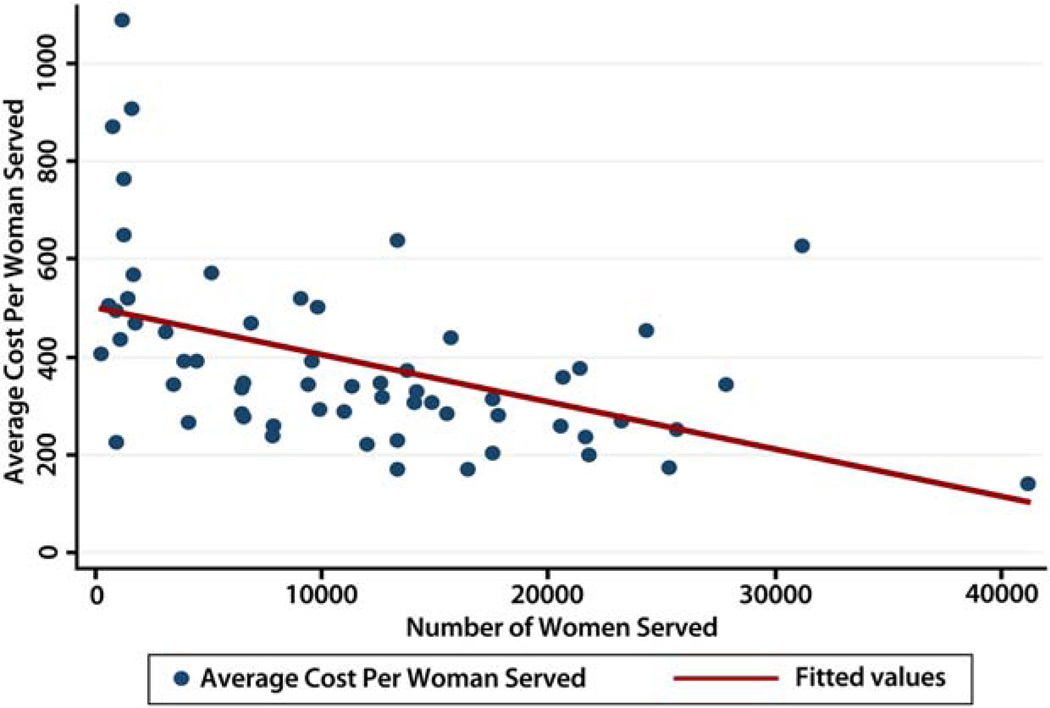
As shown in Table 3, we estimated that 5687 cases of breast cancer were detected during the study period by the 63 NBCCEDP grantees whose data we analyzed, an average of 90.3 cases (SD, 117.2) per grantee, and that the weighted mean cost per cancer case detected was $35,480. We estimated that grantees detected an average of 83.2 cases of cervical cancer (SD, 111.9) and that the weighted mean cost per cancer case detected was $18,995. As shown in Figure 3, data suggest that grantees’ average cost of detecting a case of cancer appears to decline as the total number of women they served increases.
TABLE 3.
Number o f Cancer Cases Detected and Cost per Cancer Detected by the NBCCEDP During 2006/2007 Fiscal Year
| Breast Cancers Detected | Number of Cancers Detected | Mean Cancers Detected (SD) |
| All breast cancer | 5687 | 90.3 (117.2) |
| Carcinoma in situ | 1467 | 23.3 (34.0) |
| Invasive cancer | 4220 | 67.0 (89.3) |
| Cost per Breast Cancer Detected | Median by Program (IQR), $ | Weighted Mean, $a |
| All breast cancer | 39,769 (31,538–52,693) | 35,480 |
| Carcinoma in situ | 174,398 (104,991–248,704) | 137,543 |
| Invasive cancer | 54,896 (42,081–84,549) | 47,814 |
| Cervical Cancers Detected | Number of Cancers Detected | Mean Cancers Detected (SD) |
| All cervical cancer | 5241 | 83.2 (111.9) |
| High-grade cervical intraepithelial neoplasiab | 4981 | 79.1 (108.3) |
| Invasive cancer | 260 | 4.1 (4.5) |
| Cost per cervical cancer detected | Median by Program (IQR), $ | Weighted Mean, $a |
| All cervical cancer | 27,230 (12,377–54,346) | 18,995 |
| High-grade cervical intraepithelial neoplasiab | 31,131 (13,040–64,039) | 19,986 |
| Invasive cancer | 465,425 (206,028–972,478) | 382,892 |
Mean calculated by dividing costs for all programs divided by cancers detected for all programs. Standard deviation not included because some programs did not detect any cancers.
High-grade cervical intraepithelial neoplasia (CIN) includes CIN2, CIN3, carcinoma in situ, and adenocarcinoma in situ.
Figure 3.
Average Cost per Woman Served by Number of Women Served in NBCCEDP during 2006/2007 Fiscal Year.
DISCUSSION
Excluding the value of in-kind donations, we estimated that the weighted average cost of the NBCCEDP per woman served was $251 and that the weighted average cost of clinical services per woman served was $145. Including the value of in-kind donations, we estimated that the weighted average cost was $296 per woman served. We also estimated that the weighted average cost of screening for breast cancer was $110 with an office visit and $88 without, that the average cost of the breast cancer diagnostic procedure was $401, and that the cost per case of breast cancer detected was $35,480. For cervical cancer, we estimated that corresponding costs were $61, $21, $415, and $18,995, respectively. In an era of constrained resources for public health programs, these cost estimates calculated directly from NBCCEDP can provide useful information for program planning and budget allocation. Lack of cost information directly obtained from a program is often a limiting factor in using such data to make realistic policy decisions in public health programs. These cost estimates provide a baseline against which future NBCCEDP cost estimates can be assessed.
As mentioned earlier, these cost estimates update our previous estimates of NBCCEDP costs that were based on data from 9 grantees.9 In general, these updated cost estimates were slightly higher than those we reported previously. Other previous estimates of the cost of mammography screening during an office visit have ranged from $73 to $170 when adjusted to 2007 dollars,12–15 and other previous estimates for a Pap test during an office visit have ranged from $48 to $118 (in 2007 dollars).16–20 Although cost estimates from different studies are difficult to compare because of differences in cost estimation methods, study objectives, viewpoint of the analysis, and study settings,21 our estimates of per-person cost of services provided by the NBCCEDP are within the range of previous estimates. For example, previous estimates of the cost of a diagnostic procedure for breast cancer have ranged from $351 to $374,12,14 whereas we estimated that the cost of a procedure in the NBCCEDP ranged from $368 to $433. Although numerous studies have assessed the costs of breast and cervical cancer screening and diagnosis in the last decade,22,23 few studies have assessed the cost of such preventive health services provided through public health programs designed for low-income underserved populations.
The NBCCEDP is mandated by law to allocate about 60% of its resources to clinical services. In this study, we found that 57.5% of the program resources (excluding the value of in-kind donations) are allocated to clinical services, indicating that program administrators are, on balance, adhering to this mandate. The law mandates that the remaining 40% of the program’s resources be used to support health promotion activities or other nonclinical activities essential to the success of clinical services. The provision of resources for health promotional activities in this program by policy makers is perhaps in recognition that there are other factors that affect the ability of uninsured low-income women to receive cancer screening services in addition to financial barriers. Studies have identified these factors to include both patient and provider behavior.24–27 For instance, studies have shown that the degree to which patients seek cancer screening services is associated with their usual source of care, public education, outreach/recruitment, physician recommendation, and implementation of interventions to increase professional development of preventive health among health providers.28–30 We estimated that the NBCCEDP spends 2.9% of its resources on public education, 2.9% on outreach/recruitment activities, and 1.8% on professional development. These health promotional activities are used to educate and improve the knowledge, skills, and attitudes of the general public about the importance of cancer prevention.
The NBCCEDP attempts to ensure that women who have abnormal screening results receive timely diagnosis, affordable care, and treatment. We estimated that for every woman served, the program spends $28 (11.1% of its resources) in patient support/case management services. These services are considered essential to helping women with limited access to health care overcome barriers to receiving services, adhere to screening recommendations, receive timely diagnostic recommendations, and make effective use of recommended treatment therapies.31–34 Quantifying the amount of program resources that the NBCCEDP allocates to different health promotion activities is essential to ensuring that the program is accountable for how it uses its resources to encourage women to be screened and to help them obtain other recommended preventive health services.
The 2010 Affordable Care Act (ACA) is expected to reduce financial barriers to preventive health services such as cancer screening by expanding insurance coverage for these services and eliminating copayments and deductibles for millions of low-income Americans. Because many of these newly insured people may have limited knowledge of the health care system and thus may have difficulty accessing available services,35,36 health care workers trained in health promotion activities can play an important role in helping them obtain services. In the past 20 years, the NBCCEDP has built a strong infrastructure and gained experience in using health promotion activities to help to deliver cancer screening and diagnostic services to women with limited access to the health care system. As the nation implements the ACA, this infrastructure and experience may be useful in helping newly insured people obtain recommended preventive health services. In addition, our estimates of the cost of various NBCCEDP health promotion activities (presented in Fig. 2) could be used as benchmarks against which current and future expenditures for similar services could be compared or as a guide for estimating the financial resources required to provide such services for the increased number of women who may have insurance coverage as the result of the ACA.
However, extrapolations of our NBCCEDP cost estimates to the much larger population of women expected to become eligible to receive preventive health care services under the ACA may overestimate the actual cost of such services because the average cost of these services may decline as the number of women served increases (as suggested by data presented in Fig. 3). However, quantifying the extent to which the per-person cost of service provision may decrease as the number of women served increases would require more years of program cost data than we had available for this article.
In the past 20 years, NBCCEDP partners have invested a substantial amount of their resources to this program. We estimated that the value of in-kind donations to the NBCCEDP by its partners amounted to $45 per woman served, or 15% of the estimated $296 weighted average cost per woman served in the program. These in-kind donations are a clear indication of the strong commitment that NBCCEDP’s various partners have to the program and have been instrumental in advancing the program’s ultimate goal of providing all US women with access to breast and cervical cancer screening, diagnosis, and treatment services. On the other hand, we estimated that NBCCEDP administrators spend approximately 1.1% of its resources in developing, maintaining, and sustaining relationships with its partners, which indicates that NBCCEDP administrators understand the importance of partner involvement to the success of this program.
Despite our concerted effort to ascertain the true cost of delivering cancer screening services in publicly funded cancer screening programs, there are 6 notable limitations to our study. First, the cost data presented in this article did not include cost of resources incurred by women participating in this program. These resources include transportation cost, child and dependent care costs, value of time spent in traveling and receiving preventive cancer screening services, and psychosocial costs such as anxiety from false-positive test results. As a result, our estimates do not reflect the total societal cost of delivering cancer screening and related follow-up services through a publicly funded program. However, this total cost could be estimated easily by adding our estimates of program costs to previously published estimates of personal costs incurred by program participants, such as the estimate that women screened for breast cancer through the NBCCEDP incurred average personal costs of $17 (range, $11–$23).37 Such estimates of the total societal cost of specified health care services can be used by policy makers for program planning and by researchers attempting to estimate societal cost-effectiveness of the NBCCEDP. Second, because we did not have another source of information against which to check grantees’ reports of non-CDC funding, we were unable to verify the accuracy of these reports; any inaccuracies in these reports would obviously have affected the accuracy of our estimates of the total cost of delivering cancer screening services in the program. Third, because we analyzed only 1 year of data, our estimates do not reflect variations in federal funding levels or in the availability of other program resources. To produce multiyear cost estimates that do reflect such variations, we are currently collecting multiple years of program cost data. Fourth, our assumption that the average costs of office visits for breast and cervical screening were identical may have led us to under- or overestimate the costs of screening for these cancers. However, the results of previous studies suggest that the impact of this assumption on our cost estimates may have been minimal.12–20 Fifth, we did not allocate the estimated value of in-kind donations to specific program activities. Finally, because of the short duration of our study period, we had to use an intermediate outcome measures (eg, cases of cancer detected)21 rather than a long-term outcome measure such as life-years gained. However, we are currently conducting study designed to estimate life-years gained through the NBCCEDP and have recently published some findings from that study.38
These limitations notwithstanding, we believe that the data presented in this article are important because they provide primary information on the overall allocation of NBCCEDP resources into various activities. This information will be very useful for policy makers in determining the amount of resources that may be needed in implementing potential policy, systems, and environmental changes in the program. For example, the results reported in this article could be used to estimate the amount of resources required to implement a population-based organized breast and cervical cancer screening programin the United States.
Acknowledgments
FUNDING SUPPORT
This Supplement edition of Cancer has been sponsored by the U.S. Centers for Disease Control and Prevention (CDC), an Agency of the Department of Health and Human Services, under the Contract #200-2012-M-52408 00002.
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
This article has been contributed to by US Government employees and their work is in the public domain in the USA.
CONFLICT OF INTEREST DISCLOSURES
The authors made no disclosures.
REFERENCES
- 1.U.S. Preventive Services Task Force. Prevention and care management. Available at http://www.ahrq.gov/clinic/prevenix.htm.
- 2.Nelson HD, Tyne K, Naik A, Bougatsos C, Chan BK, Humphrey L. Screening for breast cancer: an update for the U.S. Preventive Services Task Force. Ann Intern Med. 2009;151:727–737. doi: 10.1059/0003-4819-151-10-200911170-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.U.S. Preventive Services Task Force. Prevention and care management. [Accessed on September 25, 2013]; Available at http://www.uspreventiveservicestaskforce.org/uspstf/uspscerv.htm. [Google Scholar]
- 4.Kohler BA, Ward E, McCarthy BJ, et al. Annual report to the nation on the status of cancer, 1975–2007, featuring tumors of the brain and other nervous system. Natl Cancer Inst. 2011;103:714–736. doi: 10.1093/jnci/djr077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Healthy People 2010 Final Review. [Accessed on September 25, 2013]; Available from URL: www.cdc.gov/nchs/healthy_people/hp2010/hp2010_final_review.htm.
- 6.Sabatino SA, Coates RJ, Uhler RJ, Breen N, Tangka F, Shaw KM. Disparities in mammography use among US women aged 40–64 years, by race, ethnicity, income, and health insurance status, 1993 and 2005. Med Care. 2008;46(7):692–700. doi: 10.1097/MLR.0b013e31817893b1. [DOI] [PubMed] [Google Scholar]
- 7.Ward E, Halpern M, Schrag N, et al. Association of insurance with cancer care utilization and outcomes. CA Cancer J Clin. 2008;58:9–31. doi: 10.3322/CA.2007.0011. [DOI] [PubMed] [Google Scholar]
- 8.Halpern MT, Ward EM, Pavluck AL, Schrag NM, Bian J, Chen AY. Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: a retrospective analysis. Lancet Oncol. 2008;9:222–231. doi: 10.1016/S1470-2045(08)70032-9. [DOI] [PubMed] [Google Scholar]
- 9.Ekwueme DU, Gardner JG, Subramanian S, Tangka FK, Bapat B, Richardson LC. Cost analysis of the National Breast and Cervical Cancer Early Detection Program: selected states, 2003 to 2004. Cancer. 2008;112:626–635. doi: 10.1002/cncr.23207. [DOI] [PubMed] [Google Scholar]
- 10.Lee NC, Wong FL, Jamison PM, et al. Implementation of the National Breast and Cervical Cancer Early Detection Program: The beginning. Cancer. 2014;120(16 Suppl.):2540–2548. doi: 10.1002/cncr.28820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Subramanian S, Ekwueme DU, Gardner JG, Trogdon J. Developing and testing a cost-assessment tool for cancer screening programs. Am J Prev Med. 2009;37:242–247. doi: 10.1016/j.amepre.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 12.Schousboe JT, Kerlikowske K, Loh A, Cummings SR. Personalizing mammography by breast density and other risk factors for breast cancer: analysis of health benefits and cost-effectiveness. Ann Intern Med. 2011;155:10–20. doi: 10.7326/0003-4819-155-1-201107050-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mandelblatt JS, Schechter CB, Yabroff KR, et al. Toward optimal screening strategies for older women: costs, benefits, and harms of breast cancer screening by age, biology, and health status. J Gen Intern Med. 2005;20:487–496. doi: 10.1111/j.1525-1497.2005.0116.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Poplack SP, Carney PA, Weiss JE, Titus-Ernstoff L, Goodrich ME, Tosteson AN. Screening mammography: costs and use of screening-related services. Radiology. 2005;234:79–85. doi: 10.1148/radiol.2341040125. [DOI] [PubMed] [Google Scholar]
- 15.O’Malley AS, Lawrence W, Liang W, et al. Feasibility of mobile cancer screening and prevention. J Health Care Poor Underserved. 2002;13:298–319. [PubMed] [Google Scholar]
- 16.McCrory DC, Matchar DB, Bastian L, et al. Evaluation of cervical cytology. Evid Rep Technol Assess (Summ) 1999;5:1–6. [PMC free article] [PubMed] [Google Scholar]
- 17.Kulasingam SL, Myers ER. Potential health and economic impact of adding a human papillomavirus vaccine to screening programs. JAMA. 2003;290:781–789. doi: 10.1001/jama.290.6.781. [DOI] [PubMed] [Google Scholar]
- 18.Schabert VF, Ye X, Insinga RP, Singhal PK, Riedel AA. Five-year routine cervical cancer screening rates and intervals in a US health plan. Curr Med Res Opin. 2008;24:2429–2435. doi: 10.1185/03007990802281671. [DOI] [PubMed] [Google Scholar]
- 19.Melnikow J, Kulasingam S, Slee C, et al. Surveillance after treatment for cervical intraepithelial neoplasia: outcomes, costs, and cost-effectiveness. Obstet Gynecol. 2010;116:1158–1170. doi: 10.1097/AOG.0b013e3181f88e72. [DOI] [PubMed] [Google Scholar]
- 20.Goldie SJ, Kim JJ, Wright TC. Cost-effectiveness of human papillomavirus DNA testing for cervical cancer screening in women aged 30 years or more. Obstet Gynecol. 2004;103:619–631. doi: 10.1097/01.AOG.0000120143.50098.c7. [DOI] [PubMed] [Google Scholar]
- 21.Gold MR, Siegel JE, Russell LB, Weinstein MC. Cost-Effectiveness in Health and Medicine. New York, NY: Oxford University Press; 1996. [Google Scholar]
- 22.Yabroff RK, Warren JL, Brown ML. Costs of cancer care in the USA: a descriptive review. Nat Clin Pract Oncol. 2007;4:643–656. doi: 10.1038/ncponc0978. [DOI] [PubMed] [Google Scholar]
- 23.Greenberg D, Earle C, Fang CH, Eldar-Lissai A, Neumann PJ. When is cancer care cost-effective? A systematic overview of costutility analyses in oncology. J Natl Cancer Inst. 2010;102:82–88. doi: 10.1093/jnci/djp472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Legler J, Meissner HI, Coyne C, Breen N, Chollette V, Rimer BK. The effectiveness of interventions to promote mammography among women with historically lower rates of screening. Cancer Epidemiol Biomarkers Prev. 2002;11:59–71. [PubMed] [Google Scholar]
- 25.Marcus AC, Crane LA. A review of cervical cancer screening intervention research: implications for public health programs and future research. Prev Med. 1998;27:13–31. doi: 10.1006/pmed.1997.0251. [DOI] [PubMed] [Google Scholar]
- 26.Meissner HI, Breen N, Coyne C, Legler JM, Green D, Edwards BK. Breast and cervical cancer screening interventions: an assessment of the literature. Cancer Epidemiol Biomarkers Prev. 1998;7:951–961. [PubMed] [Google Scholar]
- 27.Stone EG, Morton SC, Hulscher ME, et al. Interventions that increase use of adult immunization and cancer screening services: a meta-analysis. Ann Intern Med. 2002;136:641–651. doi: 10.7326/0003-4819-136-9-200205070-00006. [DOI] [PubMed] [Google Scholar]
- 28.Breen N, Wagener DK, Brown ML, Davis WW, Ballard-Barbash R. Progress in cancer screening over a decade: results of cancer screening from the 1987, 1992, and 1998 National Health Interview Surveys. J Natl Cancer Inst. 2001;93:1704–1713. doi: 10.1093/jnci/93.22.1704. [DOI] [PubMed] [Google Scholar]
- 29.Mandelblatt JS, Gold K, O’Malley AS, et al. Breast and cervix cancer screening among multiethnic women: role of age, health, and source of care. Prev Med. 1998;28:418–425. doi: 10.1006/pmed.1998.0446. [DOI] [PubMed] [Google Scholar]
- 30.Baron RC, Melillo S, Rimer BK, Coates RJ, Kerner J, Habarta N. Task Force on Community Preventive Services. Intervention to increase recommendation and delivery of screening for breast, cervical, and colorectal cancers by healthcare providers: a systematic review of provider reminders. Am J Prev Med. 2010;38:110–117. doi: 10.1016/j.amepre.2009.09.031. [DOI] [PubMed] [Google Scholar]
- 31.Bickell NA, Wang JJ, Oluwole S, et al. Missed opportunities: racial disparities in adjuvant breast cancer treatment. J Clin Oncol. 2006;24:1357–1362. doi: 10.1200/JCO.2005.04.5799. [DOI] [PubMed] [Google Scholar]
- 32.Psooy BJ, Schreuer D, Borgaonkar J, Caines JS. Patient navigation: improving timeliness in the diagnosis of breast abnormalities. Can Assoc Radiol J. 2004;55:145–150. [PubMed] [Google Scholar]
- 33.Battaglia TA, Roloff K, Posner MA, Freund KM. Improving follow-up to abnormal breast cancer screening in an urban population. A patient navigation intervention. Cancer. 2007;109(2 Suppl):359–367. doi: 10.1002/cncr.22354. [DOI] [PubMed] [Google Scholar]
- 34.Ramsey SD, Whitley E, Mears VW, et al. Evaluating the cost-effectiveness of cancer patient navigation programs: conceptual and practical issues. Cancer. 2009;115:5394–5403. doi: 10.1002/cncr.24603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Peipins LA, Graham S, Young R, et al. Time and distance barriers to mammography facilities in the Atlanta metropolitan area. J Community Health. 2011;36:675–683. doi: 10.1007/s10900-011-9359-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gwyn K, Bondy ML, Cohen DS, et al. Racial differences in diagnosis, treatment, and clinical delays in a population-based study of patients with newly diagnosed breast carcinoma. Cancer. 2004;100:1595–1604. doi: 10.1002/cncr.20169. [DOI] [PubMed] [Google Scholar]
- 37.Ekwueme DU, Hall IJ, Richardson LC, Gardner JG, Royalty J, Thompson TD. Estimating personal costs incurred by a woman participating in mammography screening in the National Breast and Cervical Cancer Early Detection Program. Cancer. 2008;113:592–601. doi: 10.1002/cncr.23613. [DOI] [PubMed] [Google Scholar]
- 38.Hoerger TJ, Ekwueme DU, Miller JW, et al. Estimated effects of the National Breast and Cervical Cancer Early Detection Program on breast cancer mortality. Am J Prev Med. 2011;40:397–3404. doi: 10.1016/j.amepre.2010.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]