Abstract
This study tested the hypothesis that side-to-side differences in knee gait mechanics 2 years after anterior cruciate ligament (ACL) reconstruction are associated with long-term (~8 years post-reconstruction) changes in patient-reported outcome scores. Sixteen subjects (5 males; age: 29.1 ± 7.1 years) with primary unilateral ACL reconstruction were gait tested at baseline (2.2 ± 0.3 years post-ACL reconstruction) and filled out KOOS and Lysholm surveys. At long-term follow-up (7.7 ± 0.7 years post-ACL reconstruction), the same subjects completed KOOS and Lysholm surveys. Pearson correlation coefficients assessed relationships between side-to-side differences in kinematics and kinetics at baseline and changes in Lysholm and KOOS Pain/QOL scores from 2 to 8 years post-ACL reconstruction. Significant associations were seen between greater average varus rotation (Lysholm: R =−0.654, p =0.006) and less anterior femoral displacement (Lysholm: R =0.578, p =0.019) during stance of the ACL reconstructed knee versus the contralateral knee at baseline and worse follow-up outcome scores. Significant associations were seen between greater peak knee flexion moment (KOOS Pain: R =−0.572, p =0.026; KOOS QOL: R =−0.636, p =0.011), peak knee adduction moment (Lysholm: R =−0.582, p =0.018; KOOS Pain: R =−0.742, p =0.002; KOOS QOL: R =−0.551, p =0.033), and peak internal rotation moment (Lysholm: R =0.525, p =0.037; KOOS Pain: R =0.815, p <0.001; KOOS QOL: R =0.777, p =0.001) in the ACL reconstructed knee at baseline with worse follow-up outcomes. The results of this study support the hypotheses that early changes in gait mechanics following ACL reconstruction are associated with longer-term clinical changes in patient-reported outcomes, suggesting that biomechanical markers obtained as early as 2 years after ACL reconstruction may be useful to understand clinical outcomes in this population.
Keywords: ACL, reconstruction, patient-reported outcome, gait analysis, knee
Injuries to the anterior cruciate ligament (ACL) are common, with an estimated annual injury rate of nearly 200,000 ACL tears in the United States.1 Although ACL reconstruction surgery is successful in restoring knee strength and stability, it has not been shown to prevent premature development of post-traumatic knee osteoarthritis (OA). Approximately 50% of ACL reconstructed (ACLR) patients develop rapidly progressive premature OA within 10–15 years following injury,2–5 and markers of early disease are needed for development of new strategies to prevent or delay OA onset.
There is increasing awareness that the ACL reconstruction procedure generally does not restore normal knee mechanics and that altered mechanics may then initiate degenerative processes leading to deterioration of clinical outcomes over time.6–8 Following ACL reconstruction, altered knee mechanics have been reported years before clinical signs of degenerative changes. One of the most common functional deficits observed after ACL reconstruction is loss of knee extension.8,9 Post-operative deficits in knee extension have been shown to be predictive of an increased risk for OA in the ACLR knee.8 Motion analysis studies have found kinematic changes to the ACLR knee in all three planes, including an increase in knee flexion,10–14 a shift towards external tibial rotation,15–17 and a shift toward varus rotation.16,18 Furthermore, studies of quasi-static weight-bearing function after ACL reconstruction have observed a consistent anterior shift in the relative tibial position, even in knees judged to be clinically stable.19,20 These changes in knee kinematics following ACL injury and reconstruction could have important implications for the deterioration of clinical outcomes over time because shifting the contact locations in articular cartilage during weight bearing activities could initiate degenerative changes.21,22
In addition to kinematic changes following ACL reconstruction, changes in knee kinetics have also been observed. Reductions in the external knee flexion moment23–26 and internal rotation moment26 have been reported in the ACLR knee when compared to either healthy control knees or to the contralateral uninjured knee. Knee adduction moment in ACLR knees also differs from the uninjured contralateral limb or from that of uninjured controls with some studies reporting lower adduction moments26–28 and other work29 finding increased adduction moments. As prior work in an OA population has found significant associations between higher joint moments and disease progression,30–32 it is likely that changes to the external knee moments also contribute to knee degeneration after ACL reconstruction and thus impact longer-term clinical outcomes after reconstruction.
The purpose of this study was to determine whether side-to-side differences in knee kinematics and kinetics during walking 2 years after ACL reconstruction are associated with longer-term (~8 years post-reconstruction) changes in patient-reported outcome scores. Specifically, we tested the hypotheses that (i) greater external tibial rotation, varus rotation, knee flexion, and posterior femoral displacement of the ACLR knee versus the contralateral knee; and (ii) increased peak knee flexion moment, first peak knee adduction moment, and peak internal rotation moment of the ACLR knee versus the contralateral knee 2 years after ACLR would be associated with worse patient-reported outcomes at 8 years follow-up.
METHODS
Study Design and Level of Evidence. Prognostic Study, Level II
Human Subjects
Sixteen human subjects with primary unilateral transtibial ACL reconstruction and no subsequent injuries or operations to either knee were tested at approximately 2 years post-ACL reconstruction (2.2 ± 0.3 years), and returned for follow-up testing at approximately 8 years post-ACL reconstruction (7.7 ± 0.7 years). Subjects who returned for follow-up testing were part of a larger cohort of 42 subjects who underwent gait analysis, MRI, and completion of patient-reported outcomes approximately 2 years post ACL reconstruction and agreed to further contact by researchers. We received IRB approval to re-contact subjects from the 2 year study for additional follow-up. Of the 26 subjects who did not return for follow-up testing, 10 did not respond, 5 were unable to participate due to time constraints, 3 had moved away from the area, 3 had additional arthroscopic surgery on their affected limb, 2 had re-torn their ACL, 2 were not interested, and 1 had injured their contralateral limb.
All subjects participated in this study after providing IRB-approved informed consent. Inclusion criteria included: (i) successful single-bundle unilateral ACL reconstruction based on clinical exam (KT-1000 side-to-side difference <5 mm); (ii) no other history of serious lower limb injury; (iii) self-reported history of knee stability; and (iv) knee MRI to confirm intact graft. Exclusion criteria included: (i) removal of more than 25% of the meniscus; (ii) a history of other serious ligamentous injury to either lower limb; (iii) clinical instability of the reconstructed knee; (iv) BMI >30 kg/m2; (v) significant observable chondral defects by MRI; or (vi) a history of surgical procedures performed on either lower limb or revision operation of the ACL. The surgical procedures were performed by seven surgeons between 2006 and 2009.
Gait Analysis
At the baseline test, subjects performed walking trials at self-selected normal walking speed along a level 10-m walkway, with three successful trials collected per subject. Kinematic data were collected using a multi-camera motion capture system (Qualisys Medical, Gothenburg, SE) and the point cluster technique, which uses a redundant set of 21 reflective markers,33 while a multicomponent force plate embedded in the ground (Bertec Corporation, Columbus, OH) was used to capture ground reaction forces. The systems were synchronized and recorded data at 120 Hz. A trial was considered successful when the foot of the test leg fully stepped on the force plate. Lower-limb kinematics were calculated using the software application BioMove (Stanford University, CA) following previously described methods.33–36 Briefly, the position and orientation of the foot, shank, and thigh segments were calculated using clusters of reflective markers fixed to the participant.33,34 The segments’ anatomical frames were determined following a previously described procedure34 during a standing reference pose collected before the walking trials. Knee angles, including the knee flexion angle, external rotation of the tibia relative to the femur, and varus rotation of the tibia relative to the femur, were calculated according to the joint coordinate system.36 The anterior-posterior displacement of the femur relative to the tibia was defined as the position of the center of the femoral trans-epicondylar axis along the anterior-posterior axis of the tibial anatomical frame.34 Stance phase was defined as the time during which the foot is in contact with the floor, determined by a >10-N force plate measurement in the vertical direction. The average knee flexion angle, external tibial rotation angle, varus rotation angle, and anterior-posterior displacement of the femur relative to the tibia were extracted over stance phase for analyses.
Knee moments were calculated using an inverse dynamics approach,37 with the foot, lower leg, and thigh segments idealized as rigid bodies and their scaled inertial properties taken from the literature.38 The knee moments were expressed as external moments relative to the tibial anatomical frame based upon the position of anatomical landmarks identified by palpation.34 Moments were normalized to bodyweight and height (%Bw*Ht) to allow for comparison between subjects. The first peak knee adduction moment and peak knee flexion moment, defined as the maximum moments during the first half of stance, and the peak internal rotation moment, defined as the minimum peak during the second half of stance, were extracted for each trial. The amplitudes of each peak for the three successful walking trials were averaged for each knee.
Patient-Reported Outcomes
At baseline and follow-up, subjects completed self-administered Lysholm39 and Knee Injury and Osteoarthritis Outcome Score (KOOS)40 questionnaires. A single score is given for the Lysholm questionnaire, with a maximum score of 100 points, indicating no symptoms. The KOOS Pain and knee related quality of life (QOL) subscales were selected as outcomes for this study, with higher scores (maximum score of 100 points) indicating better outcomes.
Data Analysis
Relationships between differences in kinematics and kinetics between the ACLR and contralateral leg at baseline as predictors of the change in Lysholm and KOOS Pain and QOL scores from 2 to 8 years post-ACL reconstruction were assessed by the calculation of Pearson correlation coefficients. Side-to-side differences in kinematic and kinetic variables between the two knees were calculated by subtracting the value for the intact contralateral limb from the value for the ACLR limb. For this exploratory analysis, a p-value <0.05 was considered significant. All statistical calculations were performed with SPSS version 20.0 (SPSS Inc., Chicago, IL).
RESULTS
Participant Characteristics
The participants included 5 males and 11 females. Fifteen subjects had reconstructions with Achilles allografts, and one subject had a reconstruction with bone-patellar tendon-bone autograft. Demographic data of the study population are presented in Table 1.
Table 1.
Demographics of the 16 Study Participants
| Number | 16 |
|---|---|
| Gender | 5 males/11 females |
| Injured limb | 8 left/8 right |
| Mean age at baseline (years; SD, range) | 29.1 (7.1, 21 to 41) |
| Mean height at baseline (m; SD, range) | 1.70 (0.07, 1.57 to 1.83) |
| Mean weight at baseline (kg; SD, range) | 68.4 (10.6, 53.6 to 91.8) |
| Mean time from injury to operation (days; SD, range) | 61.6 (55.4, 14 to 238) |
| Mean time to baseline testing postoperatively (years; SD, range) | 2.2 (0.3, 1.9 to 2.9) |
| Mean time to follow-up testing postoperatively (years; SD, range) | 7.7 (0.7, 6.5 to 8.7) |
| Mean baseline Lysholm score (SD, range) | 93.6 (5.6, 80 to 100) |
| Mean baseline KOOS Pain score (SD, range) | 95.3 (6.6, 78 to 100) |
| Mean baseline KOOS QOL score (SD, range) | 78.9 (22.1, 19 to 100) |
| Mean follow-up Lysholm score (SD, range) | 92.1 (9.3, 74 to 100) |
| Mean follow-up KOOS Pain score (SD, range) | 94.4 (5.8, 81 to 100) |
| Mean follow-up KOOS QOL score (SD, range) | 80.0 (16.7, 44 to 100) |
| Mean baseline KT-1000 side-to-side difference 30 lb manual force (mm; SD, range) | 0.7 (1.9, −3 to 3) |
SD, standard deviation; ADL, activities of daily living; QOL, quality of life.
Gait Analysis and Patient-Reported Outcomes
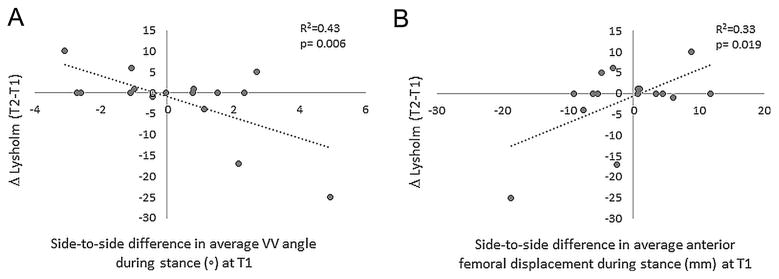
Statistical analyses demonstrated significant associations between side-to-side differences in kinematics (Table 2) and kinetics (Table 3) 2 years post-ACL reconstruction with longer-term changes in patient-reported outcomes. Specifically, significant associations were seen between greater average varus rotation during the stance phase of walking (Lysholm: R =−0.654, p =0.006) of the ACLR knee as compared to the contralateral knee at baseline and worse patient-reported outcome scores at 8-year follow-up (Fig. 1 and Table 2). The data also showed that less anterior femoral displacement on average during stance (greater anterior tibial displacement) of the ACLR knee versus the contralateral knee at baseline was associated with worse patient outcome at 8 years post-ACL reconstruction as assessed by the Lysholm survey (R =0.578, p =0.019) (Fig. 1 and Table 2). No associations were found between either knee flexion angle or external tibial rotation angle at baseline and changes in patient-reported outcomes.
Table 2.
Associations Between Side-to-Side Differences (ACLR—Contralateral) in Kinematic Variables During Walking at Baseline Testing 2 Years Post-ACL Reconstruction and Changes in Lysholm and KOOS Pain and QOL Subscales From 2 to 8 Years Post-ACL Reconstruction
| Side-to-Side Difference (ACLR—Contralateral) in Kinematic Variable | ||||
|---|---|---|---|---|
|
|
||||
| Change in Patient-Reported Outcome Scale | Average KFA in Stance | Average VV Angle in Stance | Average IE Rotation Angle in Stance | Average Anterior FD in Stance |
| Lysholm | −0.30 (0.258) | −0.65 (0.006) | −0.37 (0.157) | 0.58 (0.019) |
| KOOS pain | −0.20 (0.486) | −0.38 (0.165) | −0.15 (0.588) | 0.31 (0.266) |
| KOOS QOL | −0.08 (0.768) | −0.15 (0.586) | −0.08 (0.795) | 0.10 (0.731) |
Pearson correlation coefficients (p-values) are presented. Bold indicates significance at the α =0.05 level. For kinematic variables, positive indicates flexion, varus rotation, external rotation, and anterior femoral displacement. KFA, knee flexion angle; VV, varus-valgus; IE, internal-external; FD, femoral displacement.
Table 3.
Associations Between Side-to-Side Differences (ACLR—Contralateral) in Kinetic Variables During Walking at Baseline Testing 2 Years Post-ACL Reconstruction and Changes in Lysholm and KOOS Pain and QOL Subscales From 2 to 8 Years post-ACL Reconstruction
| Side-to-Side Difference (ACLR—Contralateral) in Kinetic Variable | |||
|---|---|---|---|
|
|
|||
| Change in Patient-Reported Outcome Scale | Peak Knee Flexion Moment | First Peak Knee Adduction Moment | Peak Internal Rotation Moment |
| Lysholm | −0.36 (0.174) | −0.58 (0.018) | 0.53 (0.037) |
| KOOS pain | −0.57 (0.026) | −0.74 (0.002) | 0.82 (<0.001) |
| KOOS QOL | −0.64 (0.011) | −0.55 (0.033) | 0.78 (0.001) |
Pearson correlation coefficients (p-values) are presented. Bold indicates significance at the α =0.05 level. For kinetic variables, positive indicates flexion, adduction, and external rotation.
Figure 1.
Representative correlations between side-to-side differences in (A) varus angle and (B) anterior femoral displacement at 2-year post-ACL reconstruction (T1) and changes in patient-reported outcomes from 2 years (T1) to 8 years (T2) post-ACL reconstruction. Less varus rotation of the ACLR knee, less anterior femoral displacement of the ACLR knee, and worse outcomes in patient-reported scores at 8 years are shown as negative values.
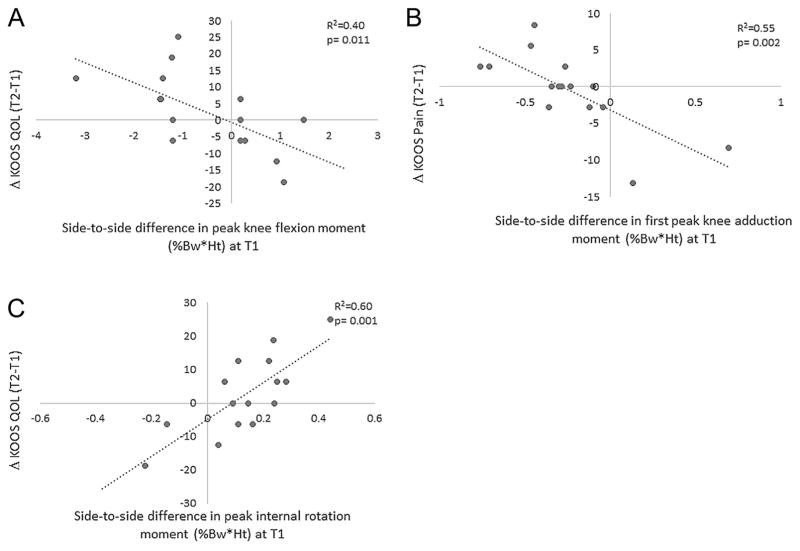
For kinetic variables, significant associations were seen between greater peak knee flexion moment in the ACLR knee at baseline versus the contralateral knee and worse KOOS Pain (R =−0.572, p =0.026) and KOOS QOL (R =−0.636, p =0.011) outcomes at 8 years post-ACL reconstruction (Fig. 2 and Table 3). Similarly, greater peak knee adduction moment at baseline in the ACLR knee was associated with worse outcome in Lysholm (R =−0.582, p =0.018), KOOS Pain (R =−0.742, p =0.002), and KOOS QOL (R =−0.551, p =0.033) scores at follow-up (Fig. 2 and Table 3). Finally, greater peak internal rotation moment in the ACLR knee at baseline was correlated with worse outcomes in Lysholm (R =0.525, p =0.037), KOOS Pain (R =0.815, p <0.001), and KOOS QOL (R =0.777, p =0.001) surveys at 8-year follow-up (Fig. 2 and Table 3).
Figure 2.
Representative correlations between side-to-side differences in (A) peak knee flexion moment, (B) first peak knee adduction moment, and (C) peak internal rotation moment at 2-year post-ACL reconstruction (T1) and changes in patient-reported outcomes from 2 years (T1) to 8 years (T2) post-ACL reconstruction. Greater peak knee flexion moment and knee adduction moment of the ACLR knee are shown as positive values, and greater peak internal rotation moment of the ACLR knee and worse outcomes in patient-reported scores at 8 years are shown as negative values.
DISCUSSION
The results of this study indicate that abnormal gait mechanics measured just 2 years after ACL reconstruction are associated with deteriorating patient-reported clinical outcomes in human subjects with clinically stable knees at 2 years and no subsequent injuries or operations to either knee at 8-year follow-up. Greater side-to-side differences between the ACLR knee and the contralateral knee in knee kinematic variables of varus rotation angle and anterior femoral displacement as well as in kinetic measures of knee flexion moment, adduction moment, and internal rotation moment 2 years after ACL reconstruction showed significant associations with changes in patient-reported outcomes at 8-year follow-up. Specifically, greater average varus rotation, less anterior femoral displacement (greater anterior tibial displacement), and greater peak knee flexion, adduction, and internal rotation moments in the ACLR knee were associated with worsening in patient-reported outcomes at follow-up. These results support the hypothesis that altered gait mechanics after ACL injury and reconstruction impact long-term clinical outcome.
This longitudinal study inclusive of 8-year patient-reported outcomes highlights the adverse impact of aberrant knee mechanics on long-term outcomes after ACL reconstruction. Few studies have investigated associations between aberrant kinematics and kinetics following ACL reconstruction with clinical outcomes even in cross-sectional studies. Zampeli et al.41 looked at the association between rotational knee kinematics between the ACLR and contralateral knee during dynamic pivoting activities and patient-reported outcome scores at the same time point, and found that greater side-to-side differences in rotational range of motion was associated with worse clinical scores. In another cross-sectional study, Kalawadia et al.42 looked at the relationship between patient-reported outcomes and knee kinematics 6 months following ACL reconstruction during downhill treadmill running, and found that greater symmetries in restoration of knee flexion and axial rotation in comparison to the contralateral knee were associated with better scores. The longitudinal work presented here provides a longer-term perspective on the implications of several previously reported kinematic changes following ACL reconstruction, including a shift toward varus rotation16,18 and an anterior shift in the relative tibial position.19,20 These same parameters were found in this work to be significantly associated with worsening subjective knee symptoms and function at follow-up.
In addition to kinematic changes following ACL reconstruction, altered external knee moments, which are surrogate measures of changes in knee joint loading,43,44 have been reported. These kinetic changes include a reduction in the external knee flexion moment,23–26 a reduction in the internal rotation moment,26 and reports of both increased29 and reduced26,28 knee adduction moments in the ACLR knee. The data presented in this study suggests that ACLR knees with greater relative loading as compared to the contralateral knee, including greater peak knee adduction moment, peak flexion moment, and peak internal rotation moment, have worsening patient-reported outcomes at 8-year follow-up. It is possible that some individuals may adapt their gait mechanics following ACL reconstruction to lower stresses on the joint and potentially serve as a protective mechanism against joint degeneration. These results could give insight into possible methods to identify patients at greater risk for developing OA.
The results of this study should be interpreted in the context of its limitations. While the sample size is small, the fact that consistent associations were observed between several mechanics measures and multiple subjective outcome scales, in a select group of subjects who have done well after ACL reconstruction, supports the assertion that the results describe real phenomena. Moreover, the data align with the changes in kinematics and kinetics that have been previously reported after ACL reconstruction. While a state-of-the-art technique to analyze ground walking was used,33,34 the use of skin-based marker systems could introduce errors caused by movement of the skin markers relative to the underlying bone during gait. However, these errors should not affect the conclusions of this study as both the reconstructed and contralateral knees were equally exposed to any skin artifact. Finally, our study investigated changes in subjective patient-reported outcomes over time and did not evaluate changes to joint structure which should be incorporated in future studies. By focusing on a small group of subjects with minimal knee changes beyond the primary ACL reconstruction that was judged to be clinically stable at entry and without subsequent additional injury or operation to either knee, this initial work suggests that gait metrics may provide early warning in otherwise well-functioning subjects for relatively poorer outcomes after ACL reconstruction, and supports future work in larger studies.
While there are many factors that could be responsible for poor long-term results after ACL reconstruction, altered kinematics and kinetics could be significant contributors to the development of joint degeneration and premature osteoarthritis. Prior studies show cartilage composition, including structure, morphology, and biochemistry,45–47 varies in the weight-bearing area of cartilage, suggesting that local regions of cartilage have adapted to specific mechanical loading environments. Thus, even a small change in load-bearing position due to altered kinematics can shift loading in the cartilage to regions not adapted to withstand the new mechanical environment experienced during repetitive ambulatory loading. As seen in Figures 1 and 2, there was a distribution in the kinematic and kinetic data at 2 years post-ACL reconstruction, which in part could be due to factors such as surgical technique, rehabilitation success, or differing levels of neuromuscular adaptation. Those with greater differences in knee mechanics would be more likely to have shifted ambulatory loading onto areas of articular cartilage not as well adapted to the conditions leading to joint degeneration and the observed deterioration of clinical outcomes years later.
In conclusion, this study demonstrated that greater side-to-side differences in kinematics (greater varus rotation and less anterior femoral displacement in the ACLR knee) and kinetics (greater peak knee flexion, adduction, and internal rotation moments in the ACLR knee) during walking at an early time point of 2 years following ACL reconstruction were associated with poorer longer-term patient-reported outcomes. The ability to identify early risk factors for subsequent poor clinical outcomes is critically important to the development of early interventions. The data suggests that evaluation of gait biomechanics at a relatively early time point following surgery may be useful to understand initiation of joint degeneration and subsequent OA in this patient population, and could serve as a basis for designing interventions to modify gait to improve long-term clinical outcomes after ACL reconstruction. The findings strongly support larger and more comprehensive studies of the predictive potential and effects of early changes to gait mechanics that affect the knee joint after ACL reconstruction on development of joint degeneration and clinical OA evaluated through MRI, radiographs, and patient-reported outcomes.
Acknowledgments
Grant sponsor: National Institute of Health; Grant numbers: AR039421, AR052784.
The funding sources had no role in the study design, collection or analysis of data, or manuscript preparation or submission. The authors would like to thank Sean Scanlan and Michael Zabala for their assistance in data collection.
Footnotes
Conflict of interest: None.
AUTHORS’ CONTRIBUTIONS
Dr. JCE-H participated in conceptualization of the research study, acquisition, analysis, and interpretation of the data, and drafting of the manuscript. Drs. TPA and CRC each participated in conceptualization of the research study, interpretation of the data, and drafting of the manuscript. Ms. JLA participated in acquisition and analysis of the data and drafting of the manuscript. Dr. JCE-H takes responsibility for content of the manuscript. All authors have read and approved the final submitted manuscript.
References
- 1.Miyasaka KC, Daniel DM, Stone ML. The incidence of knee ligament injuries in the general population. Am J Knee Surg. 1991;4:43–48. [Google Scholar]
- 2.Daniel DM, Stone ML, Dobson BE, et al. Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med. 1994;22:632–644. doi: 10.1177/036354659402200511. [DOI] [PubMed] [Google Scholar]
- 3.Lohmander LS, Ostenberg A, Englund M, et al. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50:3145–3152. doi: 10.1002/art.20589. [DOI] [PubMed] [Google Scholar]
- 4.Meuffels DE, Favejee MM, Vissers MM, et al. Ten year follow-up study comparing conservative versus operative treatment of anterior cruciate ligament ruptures. A matched-pair analysis of high level athletes. Br J Sports Med. 2009;43:347–351. doi: 10.1136/bjsm.2008.049403. [DOI] [PubMed] [Google Scholar]
- 5.von Porat A, Roos EM, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis. 2004;63:269–273. doi: 10.1136/ard.2003.008136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Andriacchi TP, Koo S, Scanlan SF. Gait mechanics influence healthy cartilage morphology and osteoarthritis of the knee. J Bone Joint Surg Am. 2009;91:95–101. doi: 10.2106/JBJS.H.01408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andriacchi TP, Mündermann A. The role of ambulatory mechanics in the initiation and progression of knee osteoarthritis. Curr Opin Rheumatol. 2006;18:514–551. doi: 10.1097/01.bor.0000240365.16842.4e. [DOI] [PubMed] [Google Scholar]
- 8.Shelbourne KD, Gray T. Minimum 10-year results after anterior cruciate ligament reconstruction: how the loss of normal knee motion compounds other factors related to the development of osteoarthritis after surgery. Am J Sports Med. 2009;37:471–480. doi: 10.1177/0363546508326709. [DOI] [PubMed] [Google Scholar]
- 9.Harner CD, Irrgang JJ, Paul J, et al. Loss of motion after anterior cruciate ligament reconstruction. Am J Sports Med. 1992;20:499–506. doi: 10.1177/036354659202000503. [DOI] [PubMed] [Google Scholar]
- 10.Ferber R, Osternig LR, Woollacott MH, et al. Gait mechanics in chronic ACL deficiency and subsequent repair. Clin Biomech (Bristol, Avon) 2002;17:274–285. doi: 10.1016/s0268-0033(02)00016-5. [DOI] [PubMed] [Google Scholar]
- 11.Gokeler A, Schmalz T, Knopf E, et al. The relationship between isokinetic quadriceps strength and laxity on gait analysis parameters in anterior cruciate ligament reconstructed knees. Knee Surg Sports Traumatol Arthrosc. 2003;11:372–378. doi: 10.1007/s00167-003-0432-1. [DOI] [PubMed] [Google Scholar]
- 12.Hunt MA, Di Ciacca SR, Jones IC, et al. Effect of anterior tibiofemoral glides on knee extension during gait in patients with decreased range of motion after anterior cruciate ligament reconstruction. Physiother Can. 2010;62:235–241. doi: 10.3138/physio.62.3.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scanlan SF, Favre J, Andriacchi TP. The relationship between peak knee extension at heel-strike of walking and the location of thickest femoral cartilage in ACL reconstructed and healthy contralateral knees. J Biomech. 2013;46:849–854. doi: 10.1016/j.jbiomech.2012.12.026. [DOI] [PubMed] [Google Scholar]
- 14.Webster KE, Feller JA, Wittwer JE. Longitudinal changes in knee joint biomechanics during level walking following anterior cruciate ligament reconstruction surgery. Gait Posture. 2012;36:167–171. doi: 10.1016/j.gaitpost.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 15.Scanlan SF, Chaudhari AM, Dyrby CO, et al. Differences in tibial rotation during walking in ACL reconstructed and healthy contralateral knees. J Biomech. 2010;43:1817–1822. doi: 10.1016/j.jbiomech.2010.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tashman S, Kolowich P, Collon D, et al. Dynamic function of the ACL-reconstructed knee during running. Clin Orthop. 2007;454:66–73. doi: 10.1097/BLO.0b013e31802bab3e. [DOI] [PubMed] [Google Scholar]
- 17.Yoo JD, Papannagari R, Park SE, et al. The effect of anterior cruciate ligament reconstruction on knee joint kinematics under simulated muscle loads. Am J Sports Med. 2005;33:240–246. doi: 10.1177/0363546504267806. [DOI] [PubMed] [Google Scholar]
- 18.Tashman S, Collon D, Anderson K, et al. Abnormal rotational knee motion during running after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32:975–983. doi: 10.1177/0363546503261709. [DOI] [PubMed] [Google Scholar]
- 19.Abebe ES, Utturkar GM, Taylor DC, et al. The effects of femoral graft placement on in vivo knee kinematics after anterior cruciate ligament reconstruction. J Biomech. 2011;44:924–929. doi: 10.1016/j.jbiomech.2010.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Papannagari R, Gill TJ, Defrate LE, et al. In vivo kinematics of the knee after anterior cruciate ligament reconstruction: a clinical and functional evaluation. Am J Sports Med. 2006;34:2006–2012. doi: 10.1177/0363546506290403. [DOI] [PubMed] [Google Scholar]
- 21.Andriacchi TP, Mündermann A, Smith RL, et al. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann Biomed Eng. 2004;32:447–457. doi: 10.1023/b:abme.0000017541.82498.37. [DOI] [PubMed] [Google Scholar]
- 22.Hosseini A, Van de Velde S, Gill TJ, et al. Tibiofemoral cartilage contact biomechanics in patients after reconstruction of a ruptured anterior cruciate ligament. J Orthop Res. 2012;30:1781–1788. doi: 10.1002/jor.22122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bush-Joseph CA, Hurwitz DE, Patel RR, et al. Dynamic function after anterior cruciate ligament reconstruction with autologous patellar tendon. Am J Sports Med. 2001;29:36–41. doi: 10.1177/03635465010290011101. [DOI] [PubMed] [Google Scholar]
- 24.Hooper D, Morrissey M, Drechsler W. Gait analysis 6 and 12 months after anterior cruciate ligament reconstruction surgery. Clin Orthop Relat Res. 2002;403:168–178. doi: 10.1097/00003086-200210000-00025. [DOI] [PubMed] [Google Scholar]
- 25.Webster K, Wittwer J, O’Brien J, et al. Gait patterns after anterior cruciate ligament reconstruction are related to graft type. Am J Sports Med. 2005;33:247–254. doi: 10.1177/0363546504266483. [DOI] [PubMed] [Google Scholar]
- 26.Zabala ME, Favre J, Scanlan SF, et al. Three-dimensional knee moments of ACL reconstructed and control subjects during gait, stair ascent, and stair descent. J Biomech. 2013;46:515–520. doi: 10.1016/j.jbiomech.2012.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Patterson MR, Delahunt E, Caulfield B. Peak knee adduction moment during gait in anterior cruciate ligament reconstructed females. Clin Biomech. 2014;29:138–142. doi: 10.1016/j.clinbiomech.2013.11.021. [DOI] [PubMed] [Google Scholar]
- 28.Webster K, Feller J. The knee adduction moment in hamstring and patellar tendon anterior cruciate ligament reconstructed knees. Knee Surg Sports Traumatol Arthrosc. 2011;20:2214–2219. doi: 10.1007/s00167-011-1835-z. [DOI] [PubMed] [Google Scholar]
- 29.Butler RJ, Minick KI, Ferber R, et al. Gait mechanics after ACL reconstruction: implications for the early onset of knee osteoarthritis. Br J Sports Med. 2009;43:366–370. doi: 10.1136/bjsm.2008.052522. [DOI] [PubMed] [Google Scholar]
- 30.Chehab EF, Favre J, Erhart-Hledik JC, et al. Baseline knee adduction and flexion moments during walking are both associated with 5 year cartilage changes in patients with medial knee osteoarthritis. Osteoarthritis Cartilage. 2014;11:1833–1839. doi: 10.1016/j.joca.2014.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Henriksen M, Hinman RS, Creaby MW, et al. Rotational knee load predicts cartilage loss over 12 months in knee osteoarthritis. Osteoarthritis Cartilage Abstract. 2012;20:S17–S18. [Google Scholar]
- 32.Miyazaki T, Wada M, Kawahara H, et al. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis. 2002;61:617–622. doi: 10.1136/ard.61.7.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Andriacchi TP, Alexander EJ, Toney MK, et al. A point cluster method for in vivo motion analysis: applied to a study of knee kinematics. J Biomech Eng. 1998;120:743–749. doi: 10.1115/1.2834888. [DOI] [PubMed] [Google Scholar]
- 34.Dyrby CO, Andriacchi TP. Secondary motions of the knee during weight bearing and non-weight bearing activities. J Orthop Res. 2004;22:794–800. doi: 10.1016/j.orthres.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 35.Favre J, Erhart-Hledik JC, Andriacchi TP. Age-related differences in sagittal-plane knee function at heel-strike of walking are increased in osteoarthritic patients. Osteoarthritis Cartilage. 2014;22:464–471. doi: 10.1016/j.joca.2013.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng. 1983;105:136–144. doi: 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- 37.Andriacchi TP, Johnson TS, Hurwitz DE, et al. Musculoskeletal dynamics, locomotion, and clinical applications. In: Mow VC, Huiskes R, editors. Basic orthopaedic biomechanics and mechano-Biology. 3. Philadelphia, PA: Lippincott Williams & Wilkins; 2005. pp. 91–122. [Google Scholar]
- 38.Dempster WT, Gaughran GRL. Properties of body segments based on size and weight. Am J Anat. 1967;120:33–54. [Google Scholar]
- 39.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 40.Roos EM, Roos HP, Lohmander LS, et al. Knee Injury and Osteoarthritis Outcome Score (KOOS): development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 41.Zampeli F, Pappas E, Giotis D, et al. Kinematic predictors of subjective outcome after anterior cruciate ligament reconstruction: an in vivo motion analysis study. Knee Surg Sports Traumatol Arthrosc. 2012;20:785–792. doi: 10.1007/s00167-012-1902-0. [DOI] [PubMed] [Google Scholar]
- 42.Kalawadia J, Thorhauer E, Vicente Arilla F, et al. Knee kinematics are related to patient-reported outcomes 6 months after anatomic ACL reconstruction. Orthop J Sports Med. 2015:3. doi: 10.1177/2325967115S00031. [DOI] [Google Scholar]
- 43.Erhart JC, Dyrby CO, D’Lima DD, et al. Changes in in vivo knee loading with a variable-stiffness intervention shoe correlate with changes in the knee adduction moment. J Orthop Res. 2010;28:1548–1553. doi: 10.1002/jor.21183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Walter JP, D’Lima DD, Colwell CW, et al. Decreased knee adduction moment does not guarantee decreased medial contact force during gait. J Orthop Res. 2010;28:1348–1354. doi: 10.1002/jor.21142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Appleyard RC, Burkhardt D, Ghosh P, et al. Topographical analysis of the structural, biochemical and dynamic biomechanical properties of cartilage in an ovine model of osteoarthritis. Osteoarthritis Cartilage. 2003;11:65–77. doi: 10.1053/joca.2002.0867. [DOI] [PubMed] [Google Scholar]
- 46.Bullough PG, Yawitz PS, Tafra L, et al. Topographical variations in the morphology and biochemistry of adult canine tibial plateau articular cartilage. J Orthop Res. 1985;3:1–16. doi: 10.1002/jor.1100030101. [DOI] [PubMed] [Google Scholar]
- 47.Clark JM. Variation of collagen fiber alignment in a joint surface: a scanning electron microscope study of the tibial plateau in dog, rabbit, and man. J Orthop Res. 1991;9:246–257. doi: 10.1002/jor.1100090213. [DOI] [PubMed] [Google Scholar]