Abstract
Objective
To examine rates of readmission after parathyroidectomy in chronic kidney disease patients and determine primary etiologies, timing, and risk factors for these unplanned readmissions.
Study Design
Retrospective cohort study
Setting
Nationwide Readmissions Database
Subjects and Methods
The Nationwide Readmissions Database was queried for parathyroidectomy procedures performed in chronic kidney disease patients between 1/2013 - 11/2013. Patient, admission, and hospital-level characteristics were compared for patients with and without at least one unplanned thirty-day readmission. Outcomes of interest included rates, etiology, and timing of readmission. Multivariate logistic regression was used to identify predictors of thirty-day readmission.
Results
There were 2756 parathyroidectomies performed in patients with chronic kidney disease with an unplanned readmission rate of 17.2%. Hypocalcemia/hungry bone syndrome accounted for 40% of readmissions. Readmissions occurred uniformly throughout the thirty days after discharge, however readmissions for hypocalcemia/hungry bone syndrome peaked in the first 10 days and decreased over time. Weight loss/malnutrition at time of parathyroidectomy and length of stay of 5-6 days conferred increased risk of readmission with adjusted odds ratios (aOR) of 3.31 (95% CI 1.55 – 7.05, P = 0.002) and 1.87 (95% CI 1.10 – 3.19, P = 0.02), respectively. Relative to primary hyperparathyroidism, parathyroidectomies performed for secondary hyperparathyroidism (aOR 2.53, 95% CI 1.07-5.95, P = 0.03) were associated with higher risk of readmission.
Conclusion
Post-parathyroidectomy readmission rates for chronic kidney disease patients are nearly 5-times that of the general population. Careful consideration of post-operative care and electrolyte management is crucial to minimize preventable readmissions in this vulnerable population.
Keywords: Parathyroidectomy, CKD, Readmission
Introduction
Parathyroidectomy is a common procedure performed for the management of hyperparathyroidism not amenable to medical therapy. 10,000-14,000 inpatient parathyroidectomies are performed annually, most often for primary hyperparathyroidism, though secondary hyperparathyroidism (SHPT) refractory to medical therapy (also termed “tertiary hyperparathyroidism”) is another frequent indication.1,2 Parathyroid hormone (PTH) is responsible for maintaining total body calcium homeostasis by utilizing feedback loops maintained by the parathyroid glands and several end-organs, notably the bones, kidneys, and intestines.
Strictly speaking, hyperparathyroidism refers to the state wherein PTH levels in the blood are elevated. Primary hyperparathyroidism results from autonomous hyper-secretion of parathyroid hormone (PTH) with resulting hypercalcemia. Most commonly, the cause of primary hyperparathyroidism is a sporadic parathyroid adenoma, but diffuse parathyroid gland hyperplasia, carcinoma, and familial endocrine disorders are other potential etiologies. SHPT characterized by elevated parathyroid hormone (PTH) levels and parathyroid gland hyperplasia as a physiological response to a chronically hypocalcemic state. SHPT is most commonly associated with chronic kidney disease (CKD), though it can be seen in malabsorption states. In CKD, declining renal function results in impaired mineral homeostasis, namely hyperphosphatemia and decreased production of active 1,25-dihydroxyvitamin D, which together lead to precipitation of insoluble calcium phosphate and decreased intestinal calcium absorption.3 In response to the hypocalcemic sate, elevations in PTH occur early in the course of CKD, and worsen as renal function further declines.4 Tertiary hyperparathyroidism refers to the state of excess PTH secretion and hypercalcemia associated with longstanding SHPT; the term is sometimes reserved for hyperparathyroidism that persists after renal transplantation.5,6
Primary hyperparathyroidism is classically thought of as a surgical disease, with surgery indicated for symptomatic patients or those at risk of developing complications of hyperparathyroidism. Although medical management is possible, it is more commonly employed for poor surgical candidates, or for management of SHPT. Medical management of SHPT has improved, notably with the 2004 approval of the calcimimetic medication cinacalcet, yet rates of parathyroidectomy for refractory SHPT in the United States have not declined substantially in CKD patients.2 Due to the complex interaction between the parathyroid glands and the renal function of CKD patients, SHPT patients are at increased risk for endocrine and electrolyte derangements in the post-operative period, and therefore more likely to be admitted for observation after surgery.7,8 Previous studies utilizing the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database have found that preoperative hemodialysis and renal impairment are both risk factors for readmission after parathyroidectomy, with readmission rates of 2.9-3.8%.9,10
Unplanned readmissions are a significant burden for patients as well as the healthcare system. Thirty-day readmission rate is considered to be a quality metric upon which hospitals are graded and compared by the Centers for Medicare and Medicaid Services (CMS).11 In general, patients with CKD have higher rates of hospital readmissions than the general population after any hospitalization. Patients with CKD stage V, or end-stage renal disease (ESRD), have nearly double the 30-day readmission rate compared to the general population.12–14 Readmission in the ESRD population has recently come under scrutiny by the CMS, and consequently, CMS has rolled out the ESRD Quality Incentive Program, which penalizes dialysis centers and hospitals with hemodialysis units for higher-than-expected unplanned 30-day readmissions.15 Additionally, the Hospital Readmissions Reduction Program, which penalizes hospital reimbursements for excess readmissions, is expected to expand its list of surgical procedures.16
With the reduction of unplanned readmissions being critically important to the national healthcare system, it is imperative to understand the epidemiology of readmissions, especially in high-risk populations. In this study, we examine rates of readmission in CKD patients undergoing parathyroidectomy, determine the primary causes and timing of unplanned readmissions, and identify risk factors for readmission.
Methods
Study Data Source
A retrospective cohort study was performed using the 2013 Nationwide Readmissions Database (NRD) of the Healthcare Cost and Utilization Project (HCUP) from the Agency for Healthcare Research and Quality (AHRQ). HCUP is a group of healthcare databases with data representing approximately 97% of all inpatient hospital discharges in the United States. The 2013 NRD samples from 21 geographically dispersed states, accounting for 49.1% of all US hospitalizations, and contains data from over 14 million hospital admissions, estimated to represent over 35 million discharges nationally. Patients included in the NRD have unique linkage numbers that allow investigators to track admissions across hospitals. For each hospital stay, the NRD contains demographics, diagnoses, procedures, hospital characteristics, length of stay, charges for hospitalization, severity and comorbidity measures, in addition to other clinical and nonclinical data.16
Study Population and Design
We queried the 2013 NRD using the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) procedure codes 06.81 (complete parathyroidectomy) and 06.89 (other parathyroidectomy) to identify index admissions with parathyroidectomy. Only admissions for patients with diagnosis codes indicating CKD (Table S1) were included.2 We excluded patients younger than 18, pregnant, receiving chemotherapy, or diagnosed with malignant thyroid or parathyroid neoplasms. Additionally, we excluded patients who died during their index hospitalization and those with a same-day readmission, since this could be considered a continuation of the index admission or a transfer to another institution. Patients admitted for parathyroidectomy in December were also excluded because of inadequate follow-up time (Figure S1).
Definition of Index Admission and Readmission
Index admissions were defined as hospitalizations during which the patient underwent a complete or partial parathyroidectomy. Readmissions were identified as any non-elective admission occurring within 30 days of an index admission. Patients could have more than one readmission in the 30-day period after surgery; however, comparisons of baseline characteristics and modeling predictors of readmissions were done at the index admission level only. Primary diagnoses for readmissions were defined by ICD-9-CM codes. For given time intervals, we reported the top five reasons for readmission.
Definition of Covariates
Risk adjustment factors included demographics (age, gender, household income category by zip code), primary payer (Medicaid, Medicare, private, self-pay, no charge, or others), and index admission characteristics (admission source, elective vs. non-elective, hospital size, hospital type, hospital control, length of stay, and discharge disposition). Discharge disposition was categorized as routine (defined as home or self care), discharge to skilled nursing facility, discharge with home health care, or against medical advice (AMA).
Knowing that comorbid conditions impact risk of readmission, we adjusted using twelve AHRQ defined comorbidity measures (weight loss/malnutrition, coagulopathy, ESRD, congestive heart failure, depression, peripheral vascular disease, chronic pulmonary disease, obesity, anemia, diabetes mellitus, neurologic disease, and hypertension). These were assigned using software that identifies ICD-9 coded comorbidities in hospital discharge records and groups them into clinically relevant categories.17 In addition to these comorbidities, we also adjusted for implant or graft complications, coronary artery disease, and hypocalcemia using their respective Clinical Classification Software (CCS) or ICD-9-CM codes.18 We used validated All Patient Refined Diagnosis-Related Groups (APR-DRG) scores to account for disease severity.19
Indications for index parathyroidectomy were categorized into primary hyperparathyroidism, SHPT, or other indications. The “other indications” category contains ICD-9 codes for a variety of conditions which includes unspecified hyperparathyroidism, other hyperparathyroidism, benign thyroid neoplasm, nontoxic multinodular goiter, and other less common diagnoses.
Statistical Analysis
We compared baseline characteristics for patient with and without a 30-day readmission. Chi-Square test was used to compare categorical variables, and Kruskal-Wallis tests were used for continuous variables.
The NRD is a complex health survey that implements stratification and clustering to provide discharge weights that can be used to generate national estimates. We used survey logistic regression, a regression technique for survey sample designs, to identify predictors of unplanned 30-day readmission for this unequally weighted dataset.20 Logistic regression was adjusted for demographics, comorbidities, admission and hospital characteristics. Results of the multivariable logistic regression are reported as adjusted odds ratios and 95% confidence intervals for each covariate in the model.
All analyses were performed using R Version 3.3.0 (R Foundation for Statistical Computing, Vienna, Austria). We considered two-tailed P-value ≤ 0.05 as statistically significant. This study was determined to be exempt by the Institutional Review Board of Mount Sinai Hospital.
Results
Parathyroid procedures and Readmission
2756 inpatient parathyroidectomies were performed in patients with CKD in the United States in 2013, accounting for approximately one-third of all inpatient parathyroidectomies performed that year. The indications for these procedures were SHPT (50%), primary hyperparathyroidism (22%), and unspecified hyperparathyroidism (13.5%). Of these, 475 (17.2%) had at least one unplanned readmission within 30 days and 65 (2.4%) had more than one readmission. Patients who underwent surgery for primary and secondary hyperparathyroidism had readmission rates of 11.8% and 17.3%, respectively.
Baseline Characteristics
Patient characteristics at index admission were compared for patients with no readmissions and those with ≥ 1 readmission. In general, patients were similar with respect to age, gender, comorbid conditions, and income. However, readmitted patients were significantly more likely to have a concurrent diagnosis of congestive heart failure (17.5% vs. 10.8%, P = 0.02) and weight loss/malnutrition (7.9% vs. 2.3%, P <0.001). Additionally, readmitted patients had higher scores on the APR-DRG Severity Scale (major/extreme loss of function 43.1% vs. 34.8%, P = 0.002) and APR-DRG Risk of Mortality Scale (major/extreme likelihood of dying 23.5% vs. 13.9%, P = 0.001). There was also a trend toward more coagulation disorders (6.5% vs. 3.2%, P = 0.06) and diabetic complications (16.3% vs. 10.8%, P = 0.06) for patients with unplanned readmissions. With respect to indication for parathyroidectomy, approximately 50% of total readmissions were seen in patients being treated for SHPT (Table 1).
Table 1.
Patient-level characteristics for parathyroidectomy patients without and with at least one readmission
| Parathyroidectomy patients with no 30-day readmissions (n=2280) | Parathyroidectomy patients with at least one 30-day readmission (n= 475) | p | |
|---|---|---|---|
| PATIENT CHARACTERISTICS | |||
| Age in years, No. (%) | |||
| Median (IQR) | 53 (41.0 – 64.0) | 50 (39.00 - 65.00) | 0.52 |
| 18-34 | 335 (14.7) | 69 (14.6) | |
| 35-49 | 615 (27.0) | 159 (33.4) | |
| 50-64 | 753 (33.0) | 120 (25.3) | |
| ≥65 | 578 (25.3) | 127 (26.8) | |
| Gender, n (%) | 0.26 | ||
| Male | 1146 (50.3) | 216 (45.5) | |
| Female | 1134 (49.7) | 259 (54.5) | |
| Comorbidities, n (%) | |||
| Acquired Immunodeficiency Sydrome | 15 (0.6) | 6 (1.2) | 0.45 |
| Alcohol Abuse | 22 (1.0) | 6 (1.3) | 0.63 |
| Anemia | 1159 (50.8) | 266 (55.9) | 0.23 |
| Coronary Artery Disease | 463 (20.3) | 115 (24.3) | 0.26 |
| Congestive Heart Failure | 246 (10.8) | 83 (17.5) | 0.02 |
| Chronic Pulmonary Disease | 278 (12.2) | 70 (14.8) | 0.40 |
| Coagulopathy | 74 (3.2) | 31 (6.5) | 0.06 |
| Depression | 225 (9.9) | 57 (12.0) | 0.40 |
| Diabetes Mellitus | 459 (20.1) | 98 (20.6) | 0.88 |
| Diabetes with Chronic Complications | 247 (10.8) | 77 (16.3) | 0.06 |
| Dialysis | 1338 (58.7) | 293 (61.6) | 0.48 |
| Drug Abuse | 65 (2.8) | 18 (3.8) | 0.56 |
| End Stage Renal Disease | 1239 (54.3) | 277 (58.2) | 0.35 |
| Fluid and Electrolyte Disorders | 596 (26.1) | 143 (30.0) | 0.30 |
| Hypertension | 1012 (44.4) | 208 (43.6) | 0.86 |
| Hypocalcemia on Index Admission | 317 (13.9) | 48 (10.1) | 0.17 |
| Hypothyroidism | 69 (3.0) | 21 (4.4) | 0.37 |
| Implant Complications | 235 (10.3) | 54 (11.4) | 0.69 |
| Liver Disease | 39 (1.7) | 15 (3.1) | 0.20 |
| Neurological Disorder | 165 (7.2) | 39 (8.2) | 0.66 |
| Obesity | 430 (18.9) | 95 (20.1) | 0.72 |
| Paralysis | 26 (1.1) | 1 (0.3) | 0.18 |
| Peripheral Vascular Disease | 155 (6.8) | 37 (7.8) | 0.67 |
| Psychoses | 61 (2.7) | 20 (4.3) | 0.26 |
| Pulmonary Circulation Disorder | 59 (2.6) | 12 (2.4) | 0.90 |
| Valvular Disease | 100 (4.4) | 33 (7.0) | 0.20 |
| Weight Loss/Malnutrition | 54 (2.3) | 38 (7.9) | <0.001 |
| Indication for Parathyroidectomy | 0.01 | ||
| Primary Hyperparathyroid | 531 (23.3) | 71 (14.9) | |
| Secondary Hyperparathyroid | 1151 (50.5) | 241 (50.7) | |
| Othera | 598 (26.2) | 164 (34.4) | |
| APRDRG Severity Scaleb, n (%) | 0.002 | ||
| Minor loss of function | 146 (6.4) | 8 (1.6) | |
| Moderate loss of function | 1339 (58.7) | 262 (55.2) | |
| Major loss of function | 753 (33.0) | 181 (38.1) | |
| Extreme loss of function | 42 (1.8) | 24 (5.0) | |
| APRDRG Risk of Mortalityb, n (%) | 0.001 | ||
| Minor likelihood of dying | 249 (10.9) | 41 (8.6) | |
| Moderate likelihood of dying | 1714 (75.2) | 323 (67.9) | |
| Major likelihood of dying | 276 (12.1) | 80 (16.7) | |
| Extreme likelihood of dying | 42 (1.8) | 32 (6.8) | |
Abbreviations: IQR: Inter Quartile range;
“Other” consists of diagnosis codes that include unspecified hyperparathyroidism, other hyperparathyroidism, benign neoplasm of thyroid, nontoxic multinodular goiter, and other less common diagnoses.
Variables defined by HCUP criteria.32
Regarding index admission characteristics, readmitted patients were more likely to have been admitted from the Emergency Department (20.1% vs. 11.9%, P = 0.005) and to have a non-elective index admission (34.6% vs. 22.3%, P = 0.001). Readmitted patients had longer lengths of stay (LOS) during the index admission (median 5 days vs. 4 days, P <0.001), lower proportion of routine discharges (75.5% vs. 87.6%, P <0.001), and higher costs of index hospitalization ($15424 vs. $12005, P <0.001). Hospital characteristics including bed size, teaching status, ownership/control, and urban-rural designation were similar for patients with and without readmissions (Table 2).
Table 2.
Admission and hospital-level characteristics for parathyroidectomy patients without and with at least one 30-day readmission.
| Parathyroidectomy patients with no 30-day readmissions (n=2424) | Parathyroidectomy patients with at least one 30-day readmission (n= 475) | p | |
|---|---|---|---|
| INDEX ADMISSION CHARACTERISTICS | |||
| Admission Sourcea, n (%) | 0.005 | ||
| Non-Emergency Department | 2152 (88.1) | 400 (79.9) | |
| Emergency Department | 272 (11.9) | 96 (20.1) | |
| Admission Type, n (%) | 0.001 | ||
| Non-Elective | 653 (22.3) | 186 (34.6) | |
| Elective | 1771 (77.7) | 309 (65.4) | |
| Length of Stay in Days, n (%) | |||
| Median (IQR) | 4 (2.0- 7.0) | 5 (3.0-11.0) | <.001 |
| <2 days | 806 (35.3) | 113 (23.7) | |
| 3-4 days | 584 (25.6) | 89 (18.8) | |
| 5-6 days | 283 (12.4) | 89 (18.9) | |
| ≥ 7 days | 608 (26.7) | 184 (38.7) | |
| Primary Payer type, n (%) | 0.07 | ||
| Medicare | 1785 (78.3) | 406 (85.4) | |
| Medicaid | 148 (6.5) | 29 (6.1) | |
| Private | 281 (12.3) | 33 (6.8) | |
| Self pay or No Charge or Others | 65 (2.8) | 8 (1.6) | |
| Discharge Disposition | <.001 | ||
| Routine | 1994 (87.6) | 359 (75.5) | |
| Skilled Nursing Facility | 120 (5.3) | 74 (15.6) | |
| Home Health Care or AMA | 162 (7.1) | 42 (8.9) | |
| Cost of Hospitalization in USD, Median (IQR) | 12006 (8629.50-17387.80) | 15425 (9964.60 -24498.95) | <.001 |
| HOSPITAL CHARACTERISTICS | |||
| Hospital bed sizea, n (%) | 0.38 | ||
| Small | 121 (5.3) | 16 (3.3) | |
| Medium | 472 (20.7) | 87 (18.2) | |
| Large | 1688 (74.0) | 377 (75.9) | |
| Hospital Typea, n (%) | 0.09 | ||
| Metropolitan non-teaching | 553 (24.2) | 106 (22.3) | |
| Metropolitan teaching | 1622 (71.1) | 363 (76.4) | |
| Non-metropolitan hospital | 106 (4.6) | 6 (1.3) | |
| Hospital Controla, n (%) | 0.41 | ||
| Government, Nonfederal | 278 (12.2) | 61 (12.8) | |
| Private, Not for Profit | 1734 (76.0) | 374 (78.7) | |
| Private, For Profit | 268 (11.8) | 40 (8.4) | |
| Hospital urban-rural designation, n (%) | 0.22 | ||
| Large metropolitan | 1337 (59.1) | 280 (58.8) | |
| Small metropolitan | 838 (37.0) | 190 (39.9) | |
| Micropolitan areas | 89 (3.9) | 6 (1.3) | |
Frequencies (%) in the columns may not sum to 100% since there might be missing data
Abbreviations: IQR: Inter Quartile range
Variables defined by HCUP criteria.32
Etiology and Timing of Readmission
Readmissions occurred uniformly throughout the 30 days after parathyroidectomy with 33.6%, 35.5%, and 30.9% of readmissions occurring between days 1-10, 11-20, 21-30 after discharge, respectively (Figure 1). However, readmission for hypocalcemia/hungry bone syndrome decreased throughout the 30 days with these conditions accounting for 40.0%, 28.3%, and 25.1% (P = 0.014) of readmissions at 1-10, 11-20, 21-30 days after discharge, respectively (Figure 2). Detailed representation of this data, as well as the most common other reasons for readmission, are depicted in graphical form in Figure 3. Common complications of surgical procedures only accounted for 2.5% of readmissions in the entire 30-day window after discharge.
Figure 1.
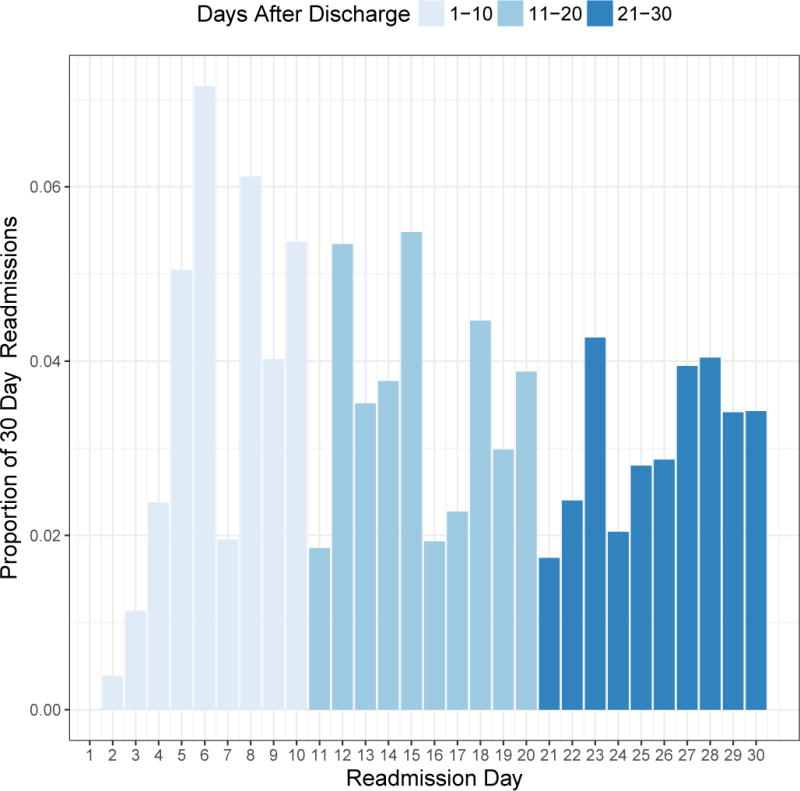
Timing of unplanned readmissions are uniformly distributed throughout the 30 days after discharge.
Figure 2.
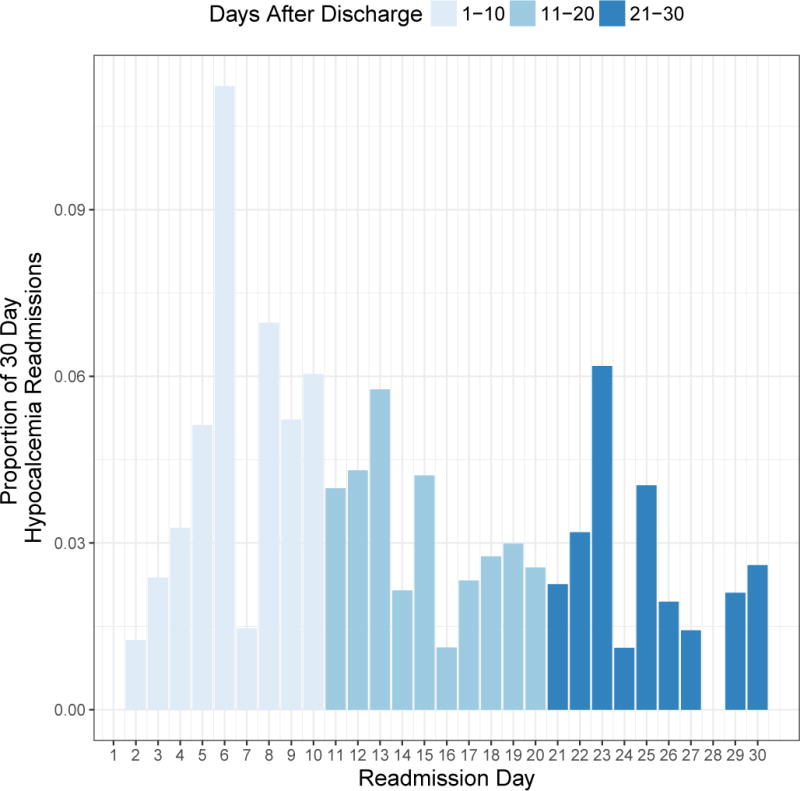
Readmissions for hypocalcemia decrease over the course of 30 days.
Figure 3.
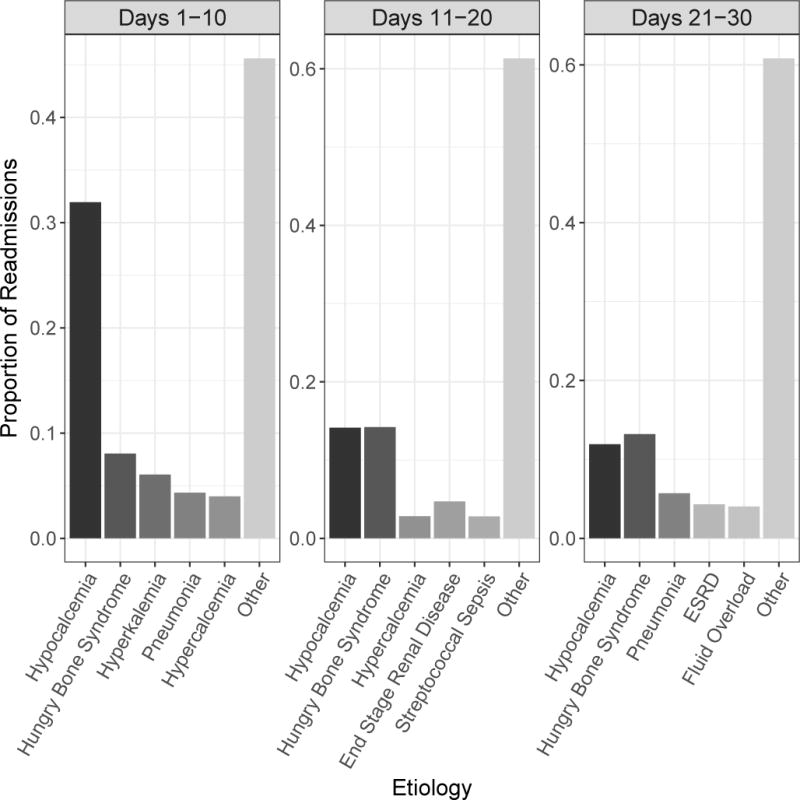
Etiologies for readmission broken down by time intervals after discharge.
Predictors of Unplanned 30-day Readmission
Few patient-specific predictors of unplanned 30-day readmission in CKD patients were identified with survey logistic regression. Weight loss/malnutrition and length of stay of 5-6 days conferred increased risk of readmission with adjusted odds ratios (aOR) of 3.31 (95% CI 1.55 – 7.05, P = 0.002) and 1.87 (95% CI 1.10 – 3.19, P = 0.02), respectively. Parathyroidectomies performed for SHPT (aOR 2.53, 95% CI 1.07-5.95, P = 0.03) and for other indications (aOR 2.39, 95% CI 1.37-4.19, P <0.001) were also associated with higher risk of readmission. Finally, trends toward increased risk of readmission were associated with ESRD (aOR 1.75, 95% CI 0.97-3.14, P= 0.06), moderate loss of function on the APR-DRG Severity Scale (aOR 2.91, 95% CI 0.99-8.49, P = 0.05), and discharge to skilled nursing facility (aOR 2.00, 95% CI 0.93-4.28, P= 0.08). Hypocalcemia on index admission was not predictive of unplanned readmission (aOR 0.66, 95% CI 0.37 – 1.15, P = 0.14) (Table 3 and 4).
Table 3.
Multivariable Analysis of predictors of 30-day readmission.
| Adjusted OR (95% CI) | P-value | |
|---|---|---|
| PATIENT CHARACTERISTICS | ||
| Age in years, n (%) | ||
| 18-34 | 1.16 (0.61-2.21) | 0.65 |
| 35-49 | 1.3 (0.76-2.21) | 0.34 |
| 50-64 | 0.74 (0.44-1.26) | 0.27 |
| ≥65 | 1 [Reference] | |
| Gender, n (%) | ||
| Male | 1 [Reference] | |
| Female | 1.21 (0.85-1.73) | 0.29 |
| Comorbidities, n (%) | ||
| Weight Loss/Malnutrition | 3.31 (1.55-7.05) | 0.002 |
| End Stage Renal Disease | 1.73 (0.96-3.12) | 0.07 |
| Coagulopathy | 1.73 (0.75-3.96) | 0.2 |
| Coronary Artery Disease | 1.48 (0.96-2.30) | 0.08 |
| Depression | 1.34 (0.77-2.32) | 0.3 |
| Congestive Heart Failure | 1.32 (0.79-2.23) | 0.29 |
| Peripheral Vascular Disease | 1.08 (0.57-2.06) | 0.81 |
| Obesity | 1.06 (0.68-1.67) | 0.79 |
| Chronic Pulmonary Disease | 1.00 (0.58-1.73) | 0.99 |
| Implant Complications | 1.00 (0.52-1.94) | 0.99 |
| Anemia | 0.97 (0.68-1.38) | 0.85 |
| Diabetes Mellitus | 0.95 (0.62-1.48) | 0.84 |
| Neurologic Disease | 0.94 (0.48-1.85) | 0.86 |
| Hypertension | 0.92 (0.49-1.71) | 0.78 |
| Hypocalcemia | 0.66 (0.38-1.15) | 0.14 |
| Indication for Parathyroidectomy | ||
| Primary Hyperparathyroidism | 1 [Reference] | |
| Secondary Hyperparathyroidism | 2.53 (1.07-5.95) | 0.03 |
| Othera | 2.39 (1.37-4.19) | 0.002 |
| Median household income category for patient’s zip codeb, n (%) | ||
| 0-25th percentile | 1 [Reference] | |
| 26-50th percentile | 1.18 (0.75-1.85) | 0.46 |
| 51-75th percentile | 1.23 (0.76-1.96) | 0.4 |
| 76-100th percentile | 0.95 (0.56-1.59) | 0.83 |
“Other” consists of diagnosis codes that include unspecified hyperparathyroidism, other hyperparathyroidism, benign neoplasm of thyroid, nontoxic multinodular goiter, and other less common diagnoses.
Variables defined by HCUP criteria.32
Table 4.
Multivariable analysis of index admission and hospital-level predictors of 30-day readmission.
| Adjusted OR (95% CI) | P-value | |
|---|---|---|
| INDEX ADMISSION CHARACTERISTICS | ||
| Admission Sourcea, n (%) | ||
| Emergency Department | 0.97 (0.49-1.92) | 0.93 |
| Non-Emergency Department | 1 [Reference] | |
| Admission Type, n (%) | ||
| Elective | 0.73 (0.45-1.19) | 0.21 |
| Non-Elective | 1 [Reference] | |
| APRDRG Severity Scalea, n (%) | ||
| Minor loss of function | 1 [Reference] | |
| Moderate loss of function | 2.47 (0.89-6.85) | 0.082 |
| Major loss of function | 1.90 (0.65-5.55) | 0.24 |
| Extreme loss of function | 2.80 (0.64-12.3) | 0.17 |
| Length of Stay in Days, n (%) | ||
| ≤ 2 days | 1 [Reference] | |
| 3-4 days | 0.95 (0.56-1.62) | 0.85 |
| 5-6 days | 1.87 (1.10-3.19) | 0.02 |
| ≥ 7 days | 1.23 (0.73-2.07) | 0.44 |
| Primary Payer type, n (%) | ||
| Medicaid | 1 [Reference] | |
| Medicare | 1.45 (0.69-3.05) | 0.33 |
| Private | 0.89 (0.36-2.23) | 0.81 |
| Self pay or No Charge or Others | 0.53 (0.14-1.97) | 0.35 |
| Discharge Disposition | ||
| Routine | 1 [Reference] | |
| Skilled Nursing Facility | 2.04 (0.95-4.38) | 0.07 |
| Home Health Care or AMA | 1.10 (0.58-2.09) | 0.77 |
| HOSPITAL CHARACTERISTICS | ||
| Hospital bed sizea, n (%) | ||
| Large | 1 [Reference] | |
| Small | 0.58 (0.21-1.56) | 0.28 |
| Medium | 0.76 (0.48-1.21) | 0.25 |
| Hospital Typea, n (%) | ||
| Metropolitan teaching | 1 [Reference] | |
| Metropolitan non-teaching | 0.83 (0.56-1.22) | 0.34 |
| Non-metropolitan hospital | 0.27 (0.06-1.32) | 0.11 |
| Hospital Controla, n (%) | ||
| Government, Nonfederal | 1 [Reference] | |
| Private, Not for Profit | 0.94 (0.57-1.56) | 0.81 |
| Private, For Profit | 0.81 (0.38-1.74) | 0.59 |
Abbreviations: AMA is “Against Medical Advice”
Variables defined by HCUP criteria.32
Discussion
Using a nationally representative cohort of patients with CKD, we found that nearly one-fifth of patients were readmitted within 30 days of parathyroidectomy, with some experiencing multiple readmissions within those 30 days. Weight loss/malnutrition, parathyroidectomy for SHPT or other indications, and hospital length of stay 5-6 days after parathyroidectomy were predictive of 30-day readmission in this population. Readmissions occurred uniformly throughout the 30 days after discharge; however, readmissions for hypocalcemia typically occurred earlier and decreased with time.
We found that the rate of readmissions after parathyroidectomy in CKD patients is nearly five-fold higher than the rate found in non-CKD patients who underwent parathyroidectomy.9,10 Unsurprisingly, patients with ESRD on hemodialysis have higher readmission rates, 23.8%, due to their multimorbidity.12,21
The comorbidity measure for weight loss, which includes ICD-9-CM codes for malnutrition, loss of weight, and low bodyweight, was the only patient-specific predictor for unplanned 30-day readmission in this cohort. This finding is consistent with previously published NSQIP data, which cites malnutrition as a predictor for readmission after thyroidectomy and parathyroidectomy.9 We also observed that post-parathyroidectomy hospital length of stay for 5-6 days was associated with increased risk of 30-day readmission. Length of stay greater than 1 day was previously identified as a predictor of readmission in the general population.9,10 Hospital length of stay greater than 7 days did not predict readmission in the regression analysis, likely because the increased comorbidity burden in these patients displaced the risk that could be attributed to length of stay. While it did not reach statistical significance, ESRD trended toward being a predictor of 30-day readmission, again agreeing with prior literature.9,10 The trend toward increased readmissions for patients discharged to skilled nursing facilities may be a reflection of baseline debilitation in these patients. Alternatively, this finding may suggest a possible communication breakdown that occurs when patients are discharged to these facilities.
Compared to readmission rates for parathyroidectomies performed for primary hyperparathyroidism, those performed for SHPT and other indications had greater risk of readmission. Primary hyperparathyroidism and SHPT represent different disease mechanisms with primary arising from adenomas and SHPT due to CKD. In contrast to primary hyperparathyroidism, with surgery as the mainstay, SHPT can be managed medically, with parathyroidectomy only indicated in late stages. Thus, it is expected that SHPT patients would have a greater comorbidity burden at the time of parathyroidectomy and are prone to readmission. Patients undergoing parathyroidectomy for other indications may also have more comorbidity burden, but it is not possible to identify a specific reason for readmission with the variety of indications.
Readmissions occurred uniformly over the course of the 30 days after discharge, but the etiologies for readmission changed with time. Hypocalcemia/hungry bone syndrome was the most common reason for unplanned 30-day readmission, accounting for 31.2% of readmissions. These rates were comparable to the 36% identified in a recent NSQIP study.10 Hypocalcemia and hungry bone syndrome commonly occur after parathyroidectomy due to the abrupt reduction in PTH at surgery, which results in increased bone formation and decreased bone resorption. Although we found a peak in readmissions for hypocalcemia/hungry bone syndrome in the first 10 days after discharge, this is a serious complication that should be monitored for days to weeks after surgery.
The results of our study highlight areas for improvement in reducing readmissions. While we have not tested any specific interventions, thorough literature review reveals several strategies. Of utmost importance is careful attention to medication reconciliation.22,23 Given the high rates of polypharmacy and elevated risk of adverse drug reactions in CKD patients, careful review of all medications and appropriate discontinuation of medications like cinacalcet are necessary after parathyroidectomy.12,24 Furthermore, patients should be educated about hypocalcemic symptoms and the importance of adherence to calcium and vitamin D supplementation. Since hypocalcemia readmissions tend to occur more frequently in the early postoperative period, providers should consider earlier prescriptions of calcium/vitamin D supplements, either at the preoperative visit or at least 24 hours before discharge, allowing adequate time for patients to acquire these critical medications. Where available, efforts should be made to have medications delivered to the patient prior to discharge.25 Additionally, CKD patients may benefit from endocrine consult services during their hospital admission, as their calcium demands may exceed those of patients without CKD and should be optimized pre-discharge.26,27
For dialysis patients or patients who are discharged to skilled nursing facilities, appropriate communication with these outside facilities is critical. Miscommunication during transitions of care is an important risk factor for adverse events, with omission of ordered medications occurring most frequently.28–30 These patients may benefit from increased outpatient nephrology involvement as they can monitor for and intervene on complications.31 Appropriate communication between hospitals and outpatient dialysis units may allow providers to make necessary adjustments. Lastly, given the level of complexity in patients with CKD, it may be beneficial to have a multi-disciplinary outpatient approach to reduce readmissions.
As with many retrospective database studies, the use of administrative data does not allow us to capture factors, including race, not coded in patient discharge summaries. Additionally, we rely on the accuracy of ICD9 codes, which can be variable in administrative databases. Excellent outcomes in many endocrine surgeries have encouraged outpatient parathyroidectomy with same-day discharge for eligible patients, but the NRD database only includes patients with an inpatient hospital stay. We cannot rule out the possibility that some healthier CKD patients had outpatient surgery and therefore were not captured in this analysis. However, it is reassuring to note that our sample size does roughly agree with a recent publication evaluating national trends in parathyroidectomy.2 Finally, we could not capture patients who died outside of the hospital within 30 days.
The major strength of our study lies in the nationally representative sample size and the ability to track inter-hospital readmissions within the same state. To our knowledge, this is the first study to examine readmission rates after parathyroidectomy in this clinically and economically important population.
Conclusion
As the healthcare system moves towards a model that rewards the quality of patient-centered care, minimization of costly and unnecessary readmissions becomes paramount. In this study, we describe that readmission rates for CKD patients undergoing parathyroidectomy are nearly five times the rate of the general population. While there are few patient-specific predictors of readmission, we note that the bulk of these readmissions can be attributed to hypocalcemia. To improve readmission rates after parathyroidectomy in CKD patients, we propose focusing on accurate, appropriate medication reconciliation, and optimizing communication and transitions of care to outside facilities (skilled nursing, dialysis, etc.) to facilitate the comprehensive care of this high-risk patient population.
Supplementary Material
Flow diagram for cohort selection.
List of International Disease Classification 9 (ICD-9) and Clinical Classification Software (CCS) codes.
References
- 1.Kim SM, Shu AD, Long J, et al. Declining Rates of Inpatient Parathyroidectomy for Primary Hyperparathyroidism in the US. PloS one. 2016;11(8):e0161192. doi: 10.1371/journal.pone.0161192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim SM, Long J, Montez-Rath ME, Leonard MB, Norton JA, Chertow GM. Rates and Outcomes of Parathyroidectomy for Secondary Hyperparathyroidism in the United States. Clin J Am Soc Nephrol. 2016;11(7):1260–1267. doi: 10.2215/CJN.10370915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Slatopolsky E, Brown A, Dusso A. Pathogenesis of secondary hyperparathyroidism. Kidney Int Suppl. 1999;73:S14–19. doi: 10.1046/j.1523-1755.1999.07304.x. [DOI] [PubMed] [Google Scholar]
- 4.Levin A, Bakris GL, Molitch M, et al. Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease. Kidney international. 2007;71(1):31–38. doi: 10.1038/sj.ki.5002009. [DOI] [PubMed] [Google Scholar]
- 5.Okada M, Tominaga Y, Izumi K, et al. Tertiary hyperparathyroidism resistant to cinacalcet treatment. Ther Apher Dial. 2011;15(Suppl 1):33–37. doi: 10.1111/j.1744-9987.2011.00924.x. [DOI] [PubMed] [Google Scholar]
- 6.Ahmad R, Hammond JM. Primary, secondary, and tertiary hyperparathyroidism. Otolaryngol Clin North Am. 2004;37(4):701–713. vii–viii. doi: 10.1016/j.otc.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 7.Seliger SL, Zhan M, Hsu VD, Walker LD, Fink JC. Chronic kidney disease adversely influences patient safety. Journal of the American Society of Nephrology: JASN. 2008;19(12):2414–2419. doi: 10.1681/ASN.2008010022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ackland GL, Moran N, Cone S, Grocott MP, Mythen MG. Chronic kidney disease and postoperative morbidity after elective orthopedic surgery. Anesthesia and analgesia. 2011;112(6):1375–1381. doi: 10.1213/ANE.0b013e3181ee8456. [DOI] [PubMed] [Google Scholar]
- 9.Mullen MG, LaPar DJ, Daniel SK, Turrentine FE, Hanks JB, Smith PW. Risk factors for 30-day hospital readmission after thyroidectomy and parathyroidectomy in the United States: An analysis of National Surgical Quality Improvement Program outcomes. Surgery. 2014;156(6):1423–1431. doi: 10.1016/j.surg.2014.08.074. [DOI] [PubMed] [Google Scholar]
- 10.Iannuzzi JC, Fleming FJ, Kelly KN, Ruan DT, Monson JR, Moalem J. Risk scoring can predict readmission after endocrine surgery. Surgery. 2014;156(6):1432–1440. doi: 10.1016/j.surg.2014.08.023. [DOI] [PubMed] [Google Scholar]
- 11.Measures and current data collection periods. https://www.medicare.gov/hospitalcompare/Data/Data-Updated.html. Accessed December 20, 2016.
- 12.Mason NA. Polypharmacy and medication-related complications in the chronic kidney disease patient. Current opinion in nephrology and hypertension. 2011;20(5):492–497. doi: 10.1097/MNH.0b013e328349c261. [DOI] [PubMed] [Google Scholar]
- 13.Donzé J, Lipsitz S, Bates DW, Schnipper JL. Causes and patterns of readmissions in patients with common comorbidities: retrospective cohort study. BMJ: British Medical Journal. 2013:347. doi: 10.1136/bmj.f7171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.United States Renal Data System. USRDS annual data report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2016. https://www.usrds.org/2016/view/Default.aspx Accessed December 16, 2016. [Google Scholar]
- 15.ESRD Quality Incentive Program. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/ESRDQIP/index.html. Accessed Dec 12, 2016.
- 16.Readmissions Reduction Program (HRRP) www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html. Accessed April 24, 2017.
- 17.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 18.HCUP CCS. Healthcare Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality; Rockville, MD: Oct, 2016. www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed December 11, 2016. [PubMed] [Google Scholar]
- 19.Baram D, Daroowalla F, Garcia R, et al. Use of the All Patient Refined-Diagnosis Related Group (APR-DRG) Risk of Mortality Score as a Severity Adjustor in the Medical ICU. Clinical Medicine Circulatory, Respiratory and Pulmonary Medicine. 2008;2:19–25. doi: 10.4137/ccrpm.s544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rader KA, Lipsitz SR, Fitzmaurice GM, Harrington DP, Parzen M, Sinha D. Bias-corrected estimates for logistic regression models for complex surveys with application to the United States’ Nationwide Inpatient Sample. Statistical methods in medical research. 2015;0(0):1–16. doi: 10.1177/0962280215596550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ishani A, Liu J, Wetmore JB, et al. Clinical outcomes after parathyroidectomy in a nationwide cohort of patients on hemodialysis. Clin J Am Soc Nephrol. 2015;10(1):90–97. doi: 10.2215/CJN.03520414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.St Peter WL. Improving medication safety in chronic kidney disease patients on dialysis through medication reconciliation. Adv Chronic Kidney Dis. 2010;17(5):413–419. doi: 10.1053/j.ackd.2010.06.001. [DOI] [PubMed] [Google Scholar]
- 23.Ledger S, Choma G. Medication reconciliation in hemodialysis patients. CANNT J. 2008;18(4):41–43. [PubMed] [Google Scholar]
- 24.Corsonello A, Pedone C, Corica F, et al. Concealed renal insufficiency and adverse drug reactions in elderly hospitalized patients. Arch Intern Med. 2005;165(7):790–795. doi: 10.1001/archinte.165.7.790. [DOI] [PubMed] [Google Scholar]
- 25.Kirkham HS, Clark BL, Paynter J, Lewis GH, Duncan I. The effect of a collaborative pharmacist-hospital care transition program on the likelihood of 30-day readmission. Am J Health Syst Pharm. 2014;71(9):739–745. doi: 10.2146/ajhp130457. [DOI] [PubMed] [Google Scholar]
- 26.Florescu MC, Islam KM, Plumb TJ, Smith-Shull S, Nieman J, Mandalapu P. Calcium supplementation after parathyroidectomy in dialysis and renal transplant patients. Int J Nephrol Renovasc Dis. 2014;7:183–190. doi: 10.2147/IJNRD.S56995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stack BC, Jr, Bimston DN, Bodenner DL, et al. American Association of Clinical Endocrinologists and American College of Endocrinology Disease State Clinical Review: Postoperative Hypoparathyroidism–Definitions and Management. Endocr Pract. 2015;21(6):674–685. doi: 10.4158/EP14462.DSC. [DOI] [PubMed] [Google Scholar]
- 28.Garrick R, Kliger A, Stefanchik B. Patient and facility safety in hemodialysis: opportunities and strategies to develop a culture of safety. Clin J Am Soc Nephrol. 2012;7(4):680–688. doi: 10.2215/CJN.06530711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pennsylvania Patient Safety Advisory: Hemodialysis administration: Strategies to ensure safe patient care. Pa Patient Saf Advis. 2010;7:87–96. Available at: http://patientsafetyauthority.org/ADVISORIES/AdvisoryLibrary/2010/Sep7(3)/Pages/87.aspx. Accessed May 24, 2017. [Google Scholar]
- 30.Holley JL. A descriptive report of errors and adverse events in chronic hemodialysis units. Nephrol News Issues. 2006;20(12):57–58. 60–61, 63. [PubMed] [Google Scholar]
- 31.Erickson KF, Winkelmayer WC, Chertow GM, Bhattacharya J. Physician visits and 30-day hospital readmissions in patients receiving hemodialysis. Journal of the American Society of Nephrology: JASN. 2014;25(9):2079–2087. doi: 10.1681/ASN.2013080879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.NRD Description of Data Elements. Healthcare Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality; Rockville, MD: Apr, 2017. www.hcup-us.ahrq.gov/db/nation/nrd/nrddde.jsp. Accessed May 24, 2017. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Flow diagram for cohort selection.
List of International Disease Classification 9 (ICD-9) and Clinical Classification Software (CCS) codes.


