Abstract
Objective
To examine contextual (facility and community) and individual factors associated with self-care and mobility outcomes among Medicare hip fracture patients receiving inpatient rehabilitation.
Design
Retrospective cohort study of 3 linked data files: Inpatient Rehabilitation Facility-Patient Assessment Instrument, Provider of Services, and Area Health Resources. Multilevel modeling was used to examine the effects of contextual and individual factors on self-care and mobility outcomes.
Setting
Inpatient Rehabilitation Facilities (IRFs).
Participants
Medicare hip fracture patients (N=35,264) treated in IRFs (N = 1072) in 2012.
Interventions
Not applicable.
Main Outcome Measure(s)
Self-care (eating, grooming, bathing, upper and lower body dressing, and toileting) and mobility (walk/wheelchair and stairs) at discharge.
Results
Mean age was 81 years. Mean self-care and mobility scores at admission were 3.17 (SD=0.87) and 1.24, (SD=0.51), respectively; mean self-care and mobility scores at discharge were 5.03 (SD=1.09) and 3.31 (SD=1.54), respectively. Individual and contextual levels explained 44.4% and 21.6% of the variance in self-care at discharge and 19.5% and 1.9% of the variance in mobility at discharge, respectively. Individual level, age, race/ethnicity, cognitive and motor FIM scores at admission, and Tier comorbidities explained variance in self-care and mobility; gender and length of stay explained variance only in self-care. At the contextual level, facilities’ case mix (mean patient age, percent Non-Hispanic White, mean self-care score at admission) and structural characteristics (rural location, freestanding, and for-profit ownership) explained variance only in self-care; facilities’ case mix (mean patient age, percent Non-Hispanic White, percent living with social support, and mean mobility score at admission) explained variance in mobility. Community variables were non-significant.
Conclusion
Individual and facility factors were significant predictors of discharge self-care and mobility among Medicare hip fracture patients in IRFs. Findings may improve quality of IRF services to hip fracture patients and inform risk adjustment methods.
Keywords: Hip Fractures, Rehabilitation Centers, Health Services Research, Medicare, Outcome Assessment (Health Care)
After an acute hospitalization for hip fracture, over 90% of Medicare beneficiaries use postacute care services including inpatient rehabilitation facilities (IRFs), skilled nursing facilities (SNFs), and home health care for ongoing medical management and rehabilitation.1 In general, evidence suggests hip fracture patients who receive intensive rehabilitation demonstrate positive functional gains;2–4 these studies focused largely on patient factors. Little evidence exists on the influence of facility characteristics (e.g., case mix, structural characteristics) associated functional outcomes among hip fracture patients.2, 5–7 Moreover, rehabilitation researchers have increasingly recognized the importance of environmental contexts of care (e.g., demographic and socioeconomic characteristics of the community) that may result in health disparities2,5–7 and impact the use of rehabilitation services and outcomes.8 To our knowledge, no studies have been conducted that account for both contextual (facility and community) and patient factors that might contribute to the variation in functional outcomes among hip fracture patients following inpatient rehabilitation.
Past studies examining the effectiveness of inpatient rehabilitation among large samples of hip fracture patients used measures such as the Functional Independence Measure™ (FIM) and its motor domain.9–12 Given the intent of IRFs to return patients to community-based settings and the Centers for Medicare and Medicaid Services’ (CMS) focus on measures of IRF quality, research examining self-care and mobility (measures which closely represent patients’ abilities to perform basic tasks and participate in life activities) would inform healthcare practice and policy efforts.
This study builds on previous research by examining (1) clinically meaningful functional outcomes, self-care and mobility, in a national sample of Medicare beneficaries; and (2) important contextual (facility and community) and individual factors that might explain variation in functional outcomes among hip fracture patients following inpatient rehabilitation.
Methods
Design
We conducted a retrospective cohort study of Medicare beneficiaries with hip fracture who received inpatient rehabilitation.
Conceptual Framework
Andersen’s model for health services use (Figure 1)13,14 and evidence from previous research6,10 was used to identify variables for inclusion in this study. Andersen’s model posits that outcomes of care are influenced by factors in three domains: (1) contextual factors, including the external environment (the economic, political, and social context in which health systems operate) and facility characteristics (how the health system is structured to deliver care); (2) individual factors including predisposing (age, race, gender), enabling (social support), and need-factors (health status); and (3) healthcare access (use of IRF services).
Figure 1.
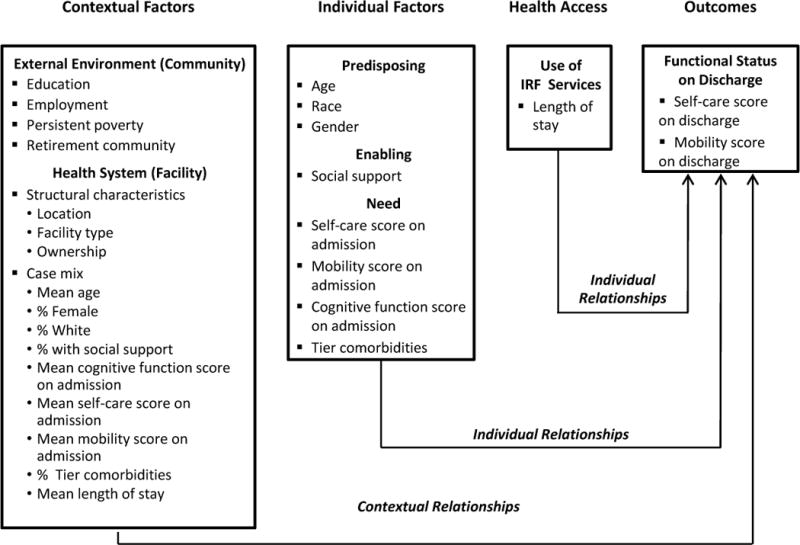
We used Andersen’s model for health services use as a guiding framework for this study.
Data Source and Sample
We used two CMS datasets from calendar year 2012 (Inpatient Rehabilitation Facility-Patient Assessment Instrument [IRF-PAI]15 and the Provider of Services file which included individual and facility variables, respectively, to conduct this study. We also used the typology codes from the 2004 Area Health Resources File16, which included community variables. The sample was limited to Medicare beneficiaries, age 65 years and older, who lived in the community prior to their hip fracture and subsequent hospital admission. Records of these patients, who were later admitted to inpatient rehabilitation between January 2012 and December 2012, were identified based on International Classification of Diseases, Ninth Revision, Clinical Modification codes (ICD-9CM codes 820.0–820.9). Exclusion criteria developed by CMS reflecting patients with an atypical course of rehabilitation17,18 were used to create the final sample and outlined accordingly in a flow diagram (Figure 2). The final sample contained 35,264 patient records from 1,072 US IRFs in 638 counties in 2012. The University institutional review board deemed the study exempt from full review.
Figure 2.
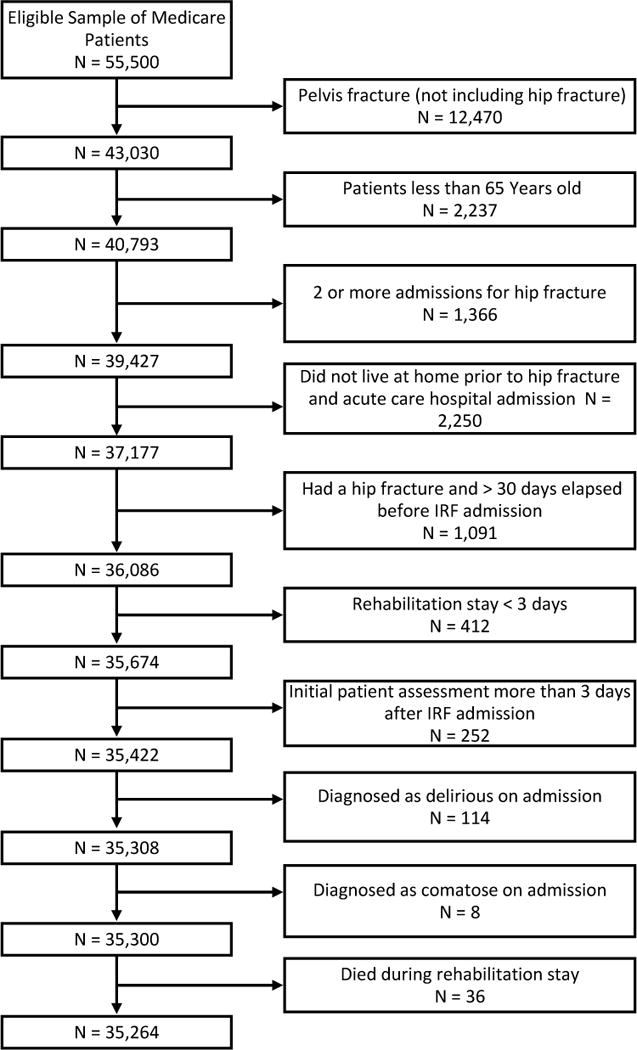
Flow diagram. Adults aged 65 years or older with Medicare fee-for-service insurance treated in an Inpatient Rehabilitation Facility with a primary diagnosis of hip fracture (ICD-9CM codes 820-820.9) in 2012.
Variables
Table 1 presents operational definitions/coding schemes and data sources for all contextual (facility and community) and individual factors as well as the outcomes of interest. Facility factors including facilities’ case mix and structural characteristics were drawn from the IRF-PAI and Provider of Services file, respectively. To measure a facilities’ case mix, patient characteristics of the study sample of hip fracture patients were aggregated to the level of the facility. Structural characteristics included: location (rural vs. urban), facility type (hospital-based unit vs. freestanding facility), and ownership (for-profit vs. nonprofit vs. government-owned). Community characteristics (low education, low employment, persistent poverty, and retirement community status) were operationalized using county typology codes extracted from the Area Health Resources file. Individual factors including predisposing (age, race, and gender), enabling (social support), and need characteristics (motor function [self-care and mobility] at admission, cognitive function at admission, and tier comorbidities) were drawn from the IRF-PAI. Healthcare access (use of IRF services as measured by the number of days spent in the IRF) was also drawn from the IRF-PAI.
Table 1.
Operational Definitions/Coding Schemes and Data Sources for Variables Used in the Multilevel Models.
| Variable | Operational Definition/Coding Schemes | Data Source |
|---|---|---|
| Level-1: Individual Factors | ||
| Predisposing characteristics | ||
| Age | Patient’s age in years at the date of IRF admission | IRF-PAI |
| Gender | Patient’s gender: 0 = male; 1 = female | IRF-PAI |
| Race/ethnicity | Patient’s race/ethnicity: (1) Non-Hispanic White; (2) Minority | IRF-PAI |
| Enabling characteristic | ||
| Social support | Patient living with others pre-hospitalization: 0 = no/1 = yes | IRF-PAI |
| Need characteristics | ||
| Cognitive function at admissiona | Measured by averaging 5 cognitive items of the Functional Independence Measure (FIM): comprehension, expression, social interaction, problem solving, and memory. | IRF-PAI |
| Motor FIM: Self-care at admissiona | Measured by averaging the 6 self-care items from the Functional Independence Measure (FIM): eating, grooming, bathing, upper body dressing, lower body dressing, and toileting. | IRF-PAI |
| Motor FIM: Mobility at admissiona | Measured by averaging 2 locomotion items from the Functional Independence Measure (FIM): walk/wheelchair and stairs. | IRF-PAI |
| Tier comorbidities | Presence or absence of comorbidities categorized at four levels (Tier 1: most severe, Tier 2: moderately severe, Tier 3: mild; No Tier: none of the listed tier comorbidities). | IRF-PAI |
| Health access | ||
|
| ||
| Length of stay in IRF | Number of days spent in inpatient rehabilitation facility | IRF-PAI |
|
| ||
| Level-2: Contextual (Facility and Community) Factors | ||
| Facility: Case mix (aggregated patient characteristics) | ||
| Facility-wide ageb | Age in years (mean) | IRF-PAI |
| Facility-wide genderb | % Female | IRF-PAI |
| Facility-wide race/ethnicityb | % White | IRF-PAI |
| Facility-wide social supportb | % of patients living with others pre-hospitalization | IRF-PAI |
| Cognitive function at admissiona,b | Mean cognitive function on admission (measured by averaging 5 cognitive items of the FIM: comprehension, expression, social interaction, problem solving, and memory. | IRF-PAI |
| Motor FIM: Self-care at admissiona,b | Mean of self-care scores on admission (measured by averaging the 6 self-care items from the FIM: eating, grooming, bathing, upper body dressing, lower body dressing, and toileting) | IRF-PAI |
| Motor FIM: Mobility at admissiona,b | Mean of mobility scores on admission (measured by averaging the 2 locomotion items from the FIM: walk/wheelchair, and stairs) | IRF-PAI |
| Comorbid conditionsb | % of patients at each comorbidity level (Tier 1: most severe; Tier 2: moderately severe; Tier 3: mildly severe; no Tier comorbidities) | IRF-PAI |
| Aggregated Length of stay in IRF | Average number of days spent in an inpatient rehabilitation facility | IRF-PAI |
| Facility: Structural characteristics | ||
| Facility location | Located in Rural/Non-metro area. 0 = no/1 = yes | POS |
| Facility type | Hospital-based unit = 0; freestanding facility = 1 | POS |
| Facility ownership | Ownership: (1) For-profit; (2) Nonprofit; (3) Government | POS |
| Community characteristicsc | ||
| Low education | Low-education county indicator. 0 = no/1 = yes | AHRF |
| Low employment | Low-employment county indicator. 0 = no/1 = yes | AHRF |
| Persistent poverty | Persistent poverty county indicator. 0 = no/1 = yes | AHRF |
| Retirement community | Retirement destination county indicator. 0 = no/1 = yes | AHRF |
|
| ||
| Outcomes | ||
| Self-care at dischargea | Average of scores for the 6 self-care items from the FIM (eating, grooming, bathing, upper dressing, lower dressing, and toileting) on discharge from IRF. | IRF-PAI |
| Mobility at dischargea | Average of scores for the 2 locomotion items from the FIM (walk/wheelchair and stairs) on discharge from IRF. | IRF-PAI |
Notes.
Data Sources: 2012 IRF-PAI: Inpatient Rehabilitation Facility Patient Assessment Instrument; 2012 POS: Provider of Services file; 2004 AHRF: Area Health Resources File.
Each FIM item is rated on a scale of 1 (total dependence) to 7 (complete independence). Per CMS guidelines, any FIM item scored as 0 (activity did not occur) was converted to 1 (total dependence) for analysis. Range for cognitive FIM score (5 items) = 5 ‒ 35; range for self-care FIM score = 1 ‒ 7; range for mobility FIM score = 1 ‒ 7.
Aggregated variable for all Medicare hip fracture patients treated in each facility during 2012.
Community characteristics were taken from the AHRF county typology codes which classifies all U.S. counties according to six non-overlapping categories of economic dependence and seven overlapping categories of policy-relevant themes. The economic types include the following: farming, mining, manufacturing, services, Federal/State government, and unspecialized counties. The policy types (several of which were used in our study) include the following: low education, low employment, persistent poverty, and retirement destination; counties were indicated as persistent poverty if 20 percent or more of its residents were poor; counties were considered low-education, if 25 percent or more of residents had neither a high school diploma nor GED; counties were considered low employment if less than 65% of residents age 25-64 were employed.
Self-care and mobility at discharge, the outcomes of interest in this study, are two subscales of the FIM. FIM items are rated on a scale from 1 (total dependence) to 7 (total independence). Self-care was measured by averaging 6 FIM items (eating, grooming, bathing, upper body dressing, lower body dressing, and toileting). Mobility, operationally defined as locomotion, was measured by averaging 2 items (walk/wheelchair and stairs); transfers were not included in our mobility measure as we were primarily interested in lower extremity impairment. Also, qualitative research shows mobility (described as walking and stair climbing) is most valued by patients recovering from hip fracture.19
Analysis
Multilevel modeling (MLM) was used to examine the effects of individual and contextual (facility and community) factors on self-care and mobility. MLM allows researchers to account for the clustering or nested structure of the data.20 Because these hip fracture patients were nested within facilities and facilities were nested within communities, we initially envisioned a 3-level model, but 60% of the communities (counties) in the dataset had only one IRF, and thus level-specific variance was non-estimable without dropping these IRFs from the analysis. To retain over 98% of the subjects in the analysis, facility and community variables were collapsed into one level (level 2). Thus, in this study, level-1 variables represent individual factors, and level-2 variables represent contextual (facility and community) factors. Specifically, individual level variables included age, gender, race/ethnicity; social support, Tier comorbidities, self-care and mobility scores at admission, and length of stay (LOS). Contextual variables included facilities’ case mix (aggregated patient characteristics) and structural characteristics (location, type, ownership), as well as community characteristics (low education, low employment, poverty, retirement community). Effect size (ES) were measured as the relative regression coefficient to the standard deviation of the residuals, which is analogous to Cohen’s d: small (ES ≥ 0.20 and < 0.50), medium (ES ≥ 0.50 and < 0.80), large (ES ≥ 0.80).21 The HLM version 722 was used for MLM analyses and SAS Version 9.323 was used for all other statistical analyses.
Results
Sample Characteristics
Table 2 summarizes individual characteristics: mean patient age was 81 years; most patients were female (71%) and Non-Hispanic White (88%); and 63% of patients lived with others pre-hospitalization. Overall, 2%, 7%, and 19% were categorized as having a tier 1 (most severe), tier 2 (moderately severe), and tier 3 (mild) comorbidity, respectively. Mean LOS was 13 days. Mean self-care scores increased from 3.17 at admission to 5.03 at discharge; mean mobility scores increased from 1.24 at admission to 3.31 at discharge.
Table 2.
Individual Factors of Medicare Hip Fracture Patients (N = 35,264) Treated in Inpatient Rehabilitation Facilities in 2012.
| Level-1: Individual Factors | Mean (SD) | % |
|---|---|---|
| Predisposing Characteristics | ||
| Age (years) | 81.23 (7.65) | |
| Female | 71% | |
| White | 88% | |
| Enabling Characteristic | ||
| Social support (living with others pre-hospitalization) | 63% | |
| Need Characteristics | ||
| Cognitive FIM score at admission | 23.68 (6.73) | |
| Self-care FIM score at admission | 3.17 (0.87) | |
| Mobility FIM score at admission | 1.24 (0.51) | |
| Comorbidity tier level: | ||
| Tier 1- most severe | 2% | |
| Tier 2- moderately severe | 7% | |
| Tier 3- mildly severe | 19% | |
| No tier comorbidities | 72% | |
| Health access | ||
| Length of stay in IRF (days) | 13.43 (4.62) | |
| Outcomes | ||
| Self-care FIM score at discharge | 5.03 (1.09) | |
| Mobility FIM score at discharge | 3.31 (1.54) |
Table 3 summarizes facility and community characteristics. Most IRFs were located in urban areas (82%), hospital-based units (79%), and nonprofit ownership (60%). Fewer than 10% of counties were classed as low-education, low-employment, or persistent poverty; 11% were considered retirement communities. Facilities’ mean self-care scores increased from 3.29 at admission to 5.05 at discharge; facilities’ mean mobility scores increased from 1.27 at admission to 3.30 at discharge.
Table 3.
Contextual (Facility and Community) Factors for Inpatient Rehabilitation Facilities (N = 1072) and Counties (N = 638) in the Sample.
| Level-2: Contextual (Facility and Community) Factors | Mean (SD) | % |
|---|---|---|
| Facility Factors | ||
| Case Mix (Aggregated Patient Variables) Characteristicsa | ||
| Mean patient age (years) | 80.96 (2.92) | |
| % Female | 70% | |
| % White | 73% | |
| % Living with others pre-hospitalization | 64% | |
| Mean cognitive FIM score at admission | 24.54 (3.54) | |
| Mean self-care FIM score at admission | 3.29 (0.49) | |
| Mean mobility FIM score at admission | 1.27 (0.26) | |
| Comorbidity tier level: | ||
| % Tier 1 – most severe | 2% | |
| % Tier 2 – moderately severe | 7% | |
| % Tier 3 – mildly severe | 20% | |
| No tier comorbidities | 71% | |
| Mean length of stay in IRF (days) | 13.22 (2.47) | |
| Mean self-care FIM score at discharge | 5.05 (0.49) | |
| Mean mobility FIM score at discharge | 3.30 (0.66) | |
| Structural Characteristics | ||
| Facility Location: | ||
| Rural | 18% | |
| Urban | 82% | |
| Facility Type: | ||
| Freestanding | 21% | |
| Hospital-based | 79% | |
| Facility Ownership: | ||
| For-profit | 29% | |
| Nonprofit | 60% | |
| Government | 11% | |
| Community Factors | ||
| Low education | 9% | |
| Low employment | 7% | |
| Persistent poverty | 5% | |
| Retirement community | 11% |
Aggregated variables for all Medicare hip fracture patients treated within each IRF in 2012.
Self-Care at Discharge
In the unconditional self-care model, the ICCs indicated 9.6% of the variance in self-care at discharge was attributed to the heterogeneity between contextual-level units and the rest (90.4%) of the variance was attributed to the heterogeneity between individuals within each contextual-level unit. In the fully adjusted self-care model (Table 4), individual and contextual factors explained 44.4% and 21.6% of the variance, respectively.
Table 4.
Multilevel Linear Model Results for Two Outcomes (FIM Self-Care Score on Discharge and FIM Mobility Score on Discharge) in Hip Fracture Patients Treated in Inpatient Rehabilitation Facilities during 2012.
| Variable | Outcomes: Fixed Effects
|
|||||
|---|---|---|---|---|---|---|
| Self-Care Score at Discharge | Mobility Score at Discharge | |||||
|
|
||||||
| b (SE) | ES | p | b (SE) | ES | p | |
| Level 1: Individual Factors | ||||||
| Predisposing Characteristics | ||||||
| Age | −0.094 (0.003) | −2.95 | <.001 | −0.039 (0.002) | −2.28 | <.001 |
| Femalea | 0.469 (0.057) | 1.38 | <.001 | −0.027 (0.034) | −0.12 | .413 |
| Non-Hispanic Whiteb | 0.511 (0.099) | 0.66 | <.001 | 0.226 (0.052) | 1.17 | <.001 |
| Enabling Characteristic | ||||||
| Living with others pre-hospitalizationc | −0.418 (0.055) | −1.29 | <.001 | −0.205 (0.031) | −1.02 | <.001 |
| Need Characteristics | ||||||
| Cognitive FIM score at admission | 0.268 (0.005) | 3.21 | <.001 | 0.125 (0.002) | 3.83 | <.001 |
| Self-care FIM score at admission | 0.624 (0.009) | 0.33 | <.001 | N/A | ||
| Mobility FIM score at admission | N/A | 0.717 (0.017) | 0.78 | <.001 | ||
| Comorbidities: Tier 1 – most severed | −1.939 (0.217) | −0.95 | <.001 | −1.242 (0.104) | −2.16 | <.001 |
| Comorbidities: Tier 2 – moderately severed | −1.722 (0.129) | −1.02 | <.001 | −0.690 (0.062) | −1.63 | <.001 |
| Comorbidities: Tier 3 – mildly severed | −0.827 (0.066) | −1.72 | <.001 | −0.496 (0.042) | −1.15 | <.001 |
| Health access | ||||||
|
| ||||||
| Length of stay in IRF | 0.199 (0.009) | 1.36 | <.001 | −0.006 (0.004) | −0.09 | .160 |
|
| ||||||
| Level 2: Contextual Factors (Facility and Community Characteristics) | ||||||
| Facility: Case mix (aggregated Patient Characteristicse | ||||||
| Mean patient age | −0.135 (0.030) | −0.07 | <.001 | −0.057 (0.015) | −0.06 | <.001 |
| % Femalea | −1.021 (0.500) | −0.54 | .042 | −0.241 (0.263) | −0.26 | .359 |
| % Non-Hispanic Whiteb | 1.175 (0.403) | 0.62 | .004 | 0.438 (0.191) | 0.48 | .022 |
| % Living with others pre-hospitalizationc | −0.824 (0.484) | −0.44 | .089 | −0.543 (0.241) | −0.59 | .025 |
| Mean Cognitive FIM score at admission | 0.005 (0.023) | 0.00 | .819 | 0.004 (0.010) | 0.00 | .663 |
| Mean Self-care FIM score at admission | 0.530 (0.036) | 0.28 | <.001 | N/A | ||
| Mean Mobility FIM score at admission | N/A | 1.056 (0.098) | 1.15 | <.001 | ||
| % Tier 1 – most severed | −0.171 (1.388) | −0.09 | .902 | −0.581 (0.704) | −0.63 | .409 |
| % Tier 2 – moderately severed | 0.328 (0.960) | 0.17 | .732 | 0.059 (0.477) | 0.06 | .900 |
| % Tier 3 – mildly severed | 0.694 (0.499) | 0.37 | .164 | −0.228 (0.258) | −0.25 | .377 |
| Mean length of stay in IRF | 0.039 (0.035) | 0.02 | .269 | 0.006 (0.016) | 0.01 | .682 |
|
| ||||||
| Facility: Structural Characteristics | ||||||
| Rural location | 0.453 (0.170) | 0.24 | .008 | 0.137 (0.090) | 0.15 | .130 |
| Type: Freestanding (vs. hospital-based) | 1.186 (0.194) | 0.63 | <.001 | 0.101 (0.083) | 0.11 | .225 |
| Ownership: For-profit (vs. nonprofit) | 0.351 (0.176) | 0.19 | .047 | −0.019 (0.079) | −0.02 | .809 |
| Ownership: Government (vs. nonprofit) | 0.047 (0.182) | 0.02 | .797 | −0.178 (0.091) | −0.19 | .052 |
|
| ||||||
| Community Characteristics | ||||||
| Low education | −0.511 (0.261) | −0.27 | .051 | −0.049 (0.136) | −0.05 | .717 |
| Low employment | −0.244 (0.308) | −0.13 | .429 | −0.161 (0.158) | −0.18 | .307 |
| Persistent poverty | −0.280 (0.348) | −0.15 | .421 | 0.142 (0.176) | 0.15 | .421 |
| Retirement community | 0.112 (0.187) | 0.06 | .549 | −0.111 (0.096) | −0.12 | .246 |
| Variable | Outcomes: Random Effects
|
|||||
|---|---|---|---|---|---|---|
| Self-Care Score at Discharge | Mobility Score at Discharge | |||||
|
|
||||||
| Variance | χ2(df) | p | Variance | χ2(df) | p | |
| Level 2 Residual | ||||||
| For Patient-level intercept | 3.54 | 289.64 (209) | <.001 | 0.84 | 294.74 (209) | <.001 |
| For Age | <0.01 | 226.69 (227) | >.500 | <0.01 | 215.71 (227) | >.500 |
| For Femalea | 0.12 | 205.98 (227) | >.500 | 0.05 | 244.59 (227) | .202 |
| For Non-Hispanic Whiteb | 0.59 | 280.82 (227) | .009 | 0.04 | 259.53 (227) | .068 |
| For Living with others pre-hospitalizationc | 0.10 | 204.81 (227) | >.500 | 0.04 | 192.70 (227) | >.500 |
| For Cognitive FIM score at admission | 0.01 | 318.68 (227) | >.500 | <0.01 | 282.11 (227) | .008 |
| For Tier 1 – most severed | 4.15 | 305.15 (227) | .001 | 0.33 | 217.22 (227) | >.500 |
| For Tier 2 – moderately severed | 2.85 | 272.86 (227) | .020 | 0.18 | 216.42 (227) | >.500 |
| For Tier 3 – mildly severed | 0.23 | 221.82 (227) | >.500 | 0.18 | 291.22 (227) | .003 |
| For Length of stay | 0.02 | 365.93 (227) | <.001 | <0.01 | 302.13 (227) | .001 |
|
| ||||||
| Level 1 Residual | 20.22 | 6.79 | ||||
| % of Variance Explained by Multilevel Model | Outcomes
|
|
|---|---|---|
| Self-Care Score at Discharge: % of Variance | Mobility Score at Discharge: % of Variance | |
| Level 1: Individual Factors | 44.4% | 19.5% |
| Level 2: Contextual (Facility and Community) Factors | 21.6% | 1.9% |
Notes: b = unstandardized beta coefficient
Reference group = Male;
Reference group = Non -Hispanic white;
Reference group = Living alone;
Reference group = No tier comorbidities.
Variables in this section are aggregated characteristics for all Medicare hip fracture patients treated within each IRF in 2012.
Individual factors (level-1) associated with better self-care at discharge (p < .001) were: younger age (ES = −2.95), female (ES = 1.38), Non-Hispanic White (ES = 0.66), not living with others pre-hospitalization (ES = −1.29), and better cognitive function scores at admission (ES = 3.21), better self-care scores at admission (ES = 0.33), having less severe comorbidities (Tier 1: [ES= −0.95]; Tier 2: [ES= −1.02]; Tier 3 [ES= −1.72]), and longer LOS (ES= 1.36).
Several contextual factors (level-2) were associated with better self-care at discharge. Specifically, facility case mix associated with better self-care at discharge included: lower mean patient age (p < .001, ES = −0.07), lower percentage of female patients (p < .05, ES = −0.54), higher percentage of Non-Hispanic White patients (p < .01, ES = 0.62), and higher facility mean self-care scores at admission (p < .001, ES = 0.28). Facility structural characteristics associated with better self-care at discharge were: rural location (p < .01, ES = 0.24), freestanding (vs. hospital-based) type (p < .001, ES = 0.63), and for-profit (vs. nonprofit) ownership (p < .05, ES = 0.19). No community characteristics were significantly associated with self-care at discharge.
Mobility at Discharge
In the unconditional mobility model, the ICCs indicated 8.4% of the variance in mobility at discharge was attributed to the heterogeneity between contextual-level units, and the rest (91.6%) of the variance was attributed to the heterogeneity between individuals within each contextual-level unit. In the fully adjusted mobility model, individual and contextual factors explained 19.5% and 1.9% of the variance, respectively.
Individual factors (level-1) associated with better mobility at discharge (p < .001) were: younger age (ES = −2.28), Non-Hispanic White (ES = 1.17), not living with others pre-hospitalization (ES = −1.02), better cognitive function at admission (ES = 3.83), better mobility scores at admission (ES = 0.78), and having less severe comorbidities (Tier 1[ES = −2.16]; Tier 2: [ES = −1.63]; Tier 3[ES = −1.15]).
Several contextual factors (level-2) were associated with better mobility at discharge. Specifically, facilities’ case mix characteristics associated with better mobility at discharge were: lower mean patient age (p < .001, ES = −0.06), higher percentage of Non-Hispanic White patients (p < .05, ES = 0.48), lower percentage of patients living with others pre-hospitalization (p < .05, ES = −0.59), and better aggregated mean mobility scores at admission (p < .001, ES = 1.15). No structural or community characteristics were associated with mobility outcomes.
Discussion
Our study was the first to investigate contextual (facility and community) and individual factors associated with self-care and mobility among a national sample of Medicare hip fracture patients treated in IRFs. Contextual factors (most notably facilities’ case mix [percent female, percent Non-Hispanic White] and facility type) explained a large proportion of the variance in self-care at discharge, but very little of the variance in mobility. However, individual factors explained a larger proportion of the variance in both outcomes than contextual factors. All individual factors were associated with self-care at discharge, and similar factors were associated with mobility at discharge (except gender and LOS) indicating gender and LOS had little to do with recovery of mobility; most individual factors had large effects on self-care (except Non-Hispanic White and self-care at admission) and mobility (except female and LOS).
Individual Factors
Predisposing characteristics
In the current study, older hip fracture patients treated within IRFs were discharged with lower self-care and mobility scores than younger patients. Possible explanations include 1) increased prevalence of multiple coexisting conditions (i.e., arthritis24, diabetes25) in older patients which increases their risk for physical disability26 and 2) frail older hip fracture patients (whose decreased physiologic reserves increase vulnerablilty to stressors) are less likely to experience successful functional outcomes.27 Orthogeriatric models of care involving therapeutic targets developed for the “oldest and frailest” hip fracture subgroups28 might inform care practices for IRF patients.
At discharge, women had higher self-care scores than men but did not differ from men on mobility. Most studies of hip fracture patients in IRFs have not reported gender differences in functional scores at discharge,29 with one exception; this small (N=99) prospective study30 reported higher motor gains in men than in women. These researchers assumed women suffered more from pain which resulted in substantial gender differences in motor outcomes. Pain and function are correlated31 thus inadequate pain therapy may preclude regaining mobility. To date, effective approaches to pain management for hip fracture are largely unexplored in rehabilitation settings.32 Large prospective studies assessing pain management practices in IRFs among specific hip fracture patient groups (e.g., women vs. men) are needed.
Our results are consistent with previous findings that hip fracture patients of minority race/ethnicity, compared to non-Hispanic Whites, were associated with lower functional outcomes among adults receiving inpatient rehabilitation.10,33
Enabling characteristics
Hip fracture patients who lived with others pre-hospitalization had poorer scores on self-care and mobility at discharge than those who lived alone. Some patients living with others may have been unable to live alone due to pre-existing functional limitations and could live in the community only with assistance from others. This is consistent with previous studies indicating hip fracture patients who lived with others prior to admission had poorer self-care and mobility scores at admission.2,10
Need characteristics
Not surprisingly, better self-care and mobility scores at admission were associated with better self-care and mobility scores at discharge. The presence of Tier comorbidities 1, 2, and 3 (vs. no Tier comorbidities) at admission was associated with poorer self-care and mobility scores at discharge. Yet, it remains unclear if specific comorbidities or combinations of comorbidities are related to self-care and mobility. Research determining the effects of specific comorbidities and combinations thereof on rehabilitation outcomes is a priority for our future work.
Contextual Factors
Rural location
Better self-care outcomes were found among patients receiving inpatient rehabilitation in rural areas, but not in mobility outcomes. In a previous study, researchers also reported a positive rural effect on functional outcomes of hip fracture patients receiving inpatient rehabilitation in rural areas; however, the unit of analysis was the IRF (not the patient), and functional outcomes (motor function at discharge and motor change) were aggregated to the facility level.6 Hip fracture patients treated in rural IRFs may have benefited from better access (longer lengths of stay) to services funded by federal initiatives such as the Medicare Rural Hospital Flexibility Program34, which was designed to strengthen the rural healthcare infrastructure.
IRF type and ownership
In this study, self-care scores at discharge were higher for patients in freestanding (vs. hospital-based) IRFs and for-profit (vs. nonprofit) IRFs; IRF type and ownership had no effect on mobility outcomes. We note that two-thirds of freestanding IRFs were also for-profit facilities. Freestanding facilities had longer LOS, which were associated at the individual patient level with better self-care outcomes. Greater medical complexity in patients admitted to freestanding facilities than those admitted to hospital-based units might explain longer LOS among freestanding IRFs.35,36
Case mix (facility aggregated patient characteristics)
Both self-care and mobility at discharge were higher in IRFs treating hip fracture patients with lower mean age and higher percentages of Non-Hispanic White patients. These findings are consistent with previous research on effects of patient age and race/ethnicity on functional status outcomes.6
Health Access
Use of IRF services
Longer IRF LOS was associated with higher self-care scores at discharge; however, LOS was not associated with mobility at discharge. Our findings might be explained by the chronology of hip fracture recovery reported by Magaziner and colleagues37 – upper extremity function (which relates to self-care) is recovered much more quickly than lower extremity function (which relates to mobility), so significant lower extremity improvement may not be realized within the intense but short inpatient rehabilitation period. Additional measures of mobility (i.e. gait speed) that are safe for patients to perform and capable of detecting meaningful change might be more useful than current FIM motor items for assessing short-term mobility improvement in rehabilitation settings.38 Furthermore, reduced muscle strength, weight loss, and inflammation impacting primarily lower extremity functioning represent factors that also likely contribute to the explanation of why greater variance was explained by self-care outcomes (and not mobility outcomes).39,40
Implications for Policy, Management, Clinical Practice
Self-care and mobility represent concepts in the World Health Organization International Classification of Functioning, Disability, and Health.41 Use of these concepts when evaluating rehabilitation outcomes has the potential to promote a common language among clinicians, researchers and policy-makers interested in improving rehabilitation care across the United States and in comparison with other nations.42–44
Adjusting for case-mix is necessary when comparing outcomes among IRFs. MLM, the statistical approach used in this study, allowed for us to model the data structure and partition the variance attributed to contextual and individual levels. This approach should be used in determining its usefulness in detecting case-mix adjusters among other IRF populations.
Successful implementation and knowledge translation of quality initiatives is affected by context.45 Therefore, identifying facility factors associated with rehabilitation outcomes might encourage administrators to benchmark their facilities’ performance against the nationally representative sample of IRFs/Medicare hip fracture patients examined in this study; benchmarking may create opportunities for sharing best practices.
Our findings reveal differences in the predictors of self-care and mobility but not the activities that influence such outcomes. Future research that identifies specific self-care and mobility activities may inform the development of clinical strategies that enable patients to meet self-care and mobility requisites during the IRF stay and impede subsequent disability likely exacerbated in the absence of effective rehabilitation.46,47
Study Limitations
Using administrative datasets maximizes sample size, but limitations include potential coding errors and missing data. Community factors related to service access (e.g., distance between home and post-acute provider), facility factors (e.g., staff mix), and process variables (e.g., treatment guidelines, team processes), were not available in the datasets used and might explain additional variance in self-care and mobility.
Conclusion
In a national sample of Medicare hip fracture patients treated in IRFs, we identified specific individual and facility factors that impact self-care and mobility outcomes, a critical first step in helping to ensure the delivery of quality rehabilitation services. Furthermore, this study highlights the importance of evaluating self-care distinct from mobility which is useful in supporting intervention activities and quality improvement programs targeting vulnerable subgroups of hip fracture patients. Also, these data are useful to IRFs as CMS begins to assess facility performance based on risk-adjusted quality metrics.
Acknowledgments
The study was funded by a grant from the Duke University School of Nursing Office of Research Affairs to the first author (MPC). A portion of Ruth Anderson’s time was supported by a grant from the National Institute of Nursing Research, Center for Adaptive Leadership in Symptom Science (P30NR014139). The authors thank Judith C. Hays and Elizabeth P. Flint for editorial and technical assistance with this manuscript.
List of Abbreviations
- CMS
Centers for Medicare and Medicaid Services
- FIM
Functional Independence Measure
- IRF
Inpatient Rehabilitation Facility
- SNF
Skilled Nursing Facility
- HH
Home Health
- IRF-PAI
Inpatient Rehabilitation Facility-Patient Assessment Instrument
- LOS
Length of Stay
- MLM
Multilevel modeling
Footnotes
Conflict of Interest Disclosure
We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated AND, if applicable, we certify that all financial and material support for this research (eg, NIH or NHS grants) and work are clearly identified in the title page of the manuscript (Cary, Pan, Sloane, Bettger, Hoenig, Merwin, Anderson).
Reprints: No reprints will be ordered.
Contributor Information
Michael P. Cary, Jr., Duke University, School of Nursing, Assistant Professor, DUMC 3322, 307 Trent Drive, Durham, NC 27710, Business Tel.: 1-919-613-6031; Home Tel.: 1-919-471-7730.
Wei Pan, Duke University, School of Nursing, Associate Professor, DUMC 3322, 307 Trent Drive, Durham, NC 27710, 919- 684-9324.
Richard Sloane, Duke University, Biostatistician, Center for the Study of Aging, DUMC 3322, 307 Trent Drive, Durham, NC 27710, 919-668-4599.
Janet Prvu Bettger, Duke University, School of Nursing, Associate Professor of Nursing, DUMC 3322, 307 Trent Drive, Durham, NC 27710, 919-668-4599.
Helen Hoenig, Physical Medicine & Rehabilitation Durham VA Medical Center, 508 Fulton Street, Durham, North Carolina, U.S.A., 919-286-6874.
Elizabeth I. Merwin, Duke University, School of Nursing, Ann Henshaw Gardiner Professor of Nursing, DUMC 3322, 307 Trent Drive, Durham, NC 27710, 919-681-0886.
Ruth A. Anderson, Duke University, School of Nursing, Virginia Stone Professor of Nursing, DUMC 3322, 307 Trent Drive, Durham, NC 27710, 919-668-4599.
References
- 1.Buntin MB, Colla CH, Deb P, Sood N, Escarce JJ. Medicare spending and outcomes after postacute care for stroke and hip fracture. Med Care. 2010;48(9):776–784. doi: 10.1097/MLR.0b013e3181e359df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mallinson T, Deutsch A, Bateman J, et al. Comparison of discharge functional status after rehabilitation in skilled nursing, home health, and medical rehabilitation settings for patients after hip fracture repair. Arch Phys Med Rehabil. 2014;95(2):209–217. doi: 10.1016/j.apmr.2013.05.031. [DOI] [PubMed] [Google Scholar]
- 3.Munin MC, Putman K, Hsieh CH, et al. Analysis of rehabilitation activities within skilled nursing and inpatient rehabilitation facilities after hip replacement for acute hip fracture. Am J Phys Med Rehabil. 2010;89(7):530–540. doi: 10.1097/PHM.0b013e3181e29f54. [DOI] [PubMed] [Google Scholar]
- 4.Munin MC, Seligman K, Dew MA, et al. Effect of rehabilitation site on functional recovery after hip fracture. Arch Phys Med Rehabil. 2005;86(3):367–372. doi: 10.1016/j.apmr.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 5.Graham JE, Deutsch A, O’Connell AA, Karmarkar AM, Granger CV, Ottenbacher KJ. Inpatient rehabilitation volume and functional outcomes in stroke, lower extremity fracture, and lower extremity joint replacement. Med Care. 2013;51(5):404–412. doi: 10.1097/MLR.0b013e318286e3c8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cary M, Baernholdt M, Anderson R, Merwin E. Performance-based outcomes of inpatient rehabilitation facilities treating hip fracture patients in the United States. Arch Phys Med Rehabil. 2015 doi: 10.1016/j.apmr.2015.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McGilton KS, Mahomed N, Davis AM, Flannery J, Calabrese S. Outcomes for older adults in an inpatient rehabilitation facility following hip fracture (HF) surgery. Arch Gerontol Geriatr. 2009;49(1):e23–31. doi: 10.1016/j.archger.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 8.Magasi S, Wong A, Gray DB, et al. Theoretical foundations for the measurement of environmental factors and their impact on participation among people with disabilities. Arch Phys Med Rehabil. 2015;96(4):569–577. doi: 10.1016/j.apmr.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 9.Deutsch A, Granger CV, Fiedler RC, et al. Outcomes and reimbursement of inpatient rehabilitation facilities and subacute rehabilitation programs for Medicare beneficiaries with hip fracture. Med Care. 2005;43(9):892–901. doi: 10.1097/01.mlr.0000173591.23310.d5. [DOI] [PubMed] [Google Scholar]
- 10.Cary MP, Jr, Merwin EI, Oliver MN, Williams IC. Inpatient Rehabilitation Outcomes in a National Sample of Medicare Beneficiaries With Hip Fracture. J Appl Gerontol. 2016;35(1):62–83. doi: 10.1177/0733464814541325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Graham JE, Chang PF, Bergés IM, Granger CV, Ottenbacher KJ. Race/ethnicity and outcomes following inpatient rehabilitation for hip fracture. J Gerontol A Biol Sci Med Sci. 2008;63(8):860–866. doi: 10.1093/gerona/63.8.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ottenbacher KJ, Smith PM, Illig SB, et al. Disparity in health services and outcomes for persons with hip fracture and lower extremity joint replacement. Med Care. 2003;41(2):232–241. doi: 10.1097/01.MLR.0000044902.01597.54. [DOI] [PubMed] [Google Scholar]
- 13.Andersen RM. National health surveys and the behavioral model of health services use. Med Care. 2008;46(7):647–653. doi: 10.1097/MLR.0b013e31817a835d. [DOI] [PubMed] [Google Scholar]
- 14.Litaker D, Koroukian SM, Love TE. Context and healthcare access: looking beyond the individual. Med Care. 2005;43(6):531–540. doi: 10.1097/01.mlr.0000163642.88413.58. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Medicare & Medicaid Services(CMS) The Inpatient Rehabilitation Facility-Patient Assessment Instrument (IRF-PAI) training manual. Baltimore, MD: Centers for Medicare & Medicaid Services (CMS); 2012. [Google Scholar]
- 16.Health Resources and Services Administration. Area Health Resource File (AHRF). National County-level Health Resources Information Database. 2012 http://www.arf.hrsa.gov/
- 17.Carter GM, Buntin MB, Hayden O, et al. Analyses for the initial implementation of the Inpatient Rehabilitation Facility Prospective Payment System (MR-1500-CMS) Santa Monica, CA: RAND Corporation; 2002. [Google Scholar]
- 18.Stineman MG, Escarce JJ, Goin JE, Hamilton BB, Granger CV, Williams SV. A case-mix classification system for medical rehabilitation. Med Care. 1994;32(4):366–379. doi: 10.1097/00005650-199404000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Griffiths F, Mason V, Boardman F, et al. Evaluating recovery following hip fracture: a qualitative interview study of what is important to patients. BMJ Open. 2015;5(1):e005406. doi: 10.1136/bmjopen-2014-005406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cho SH. Using multilevel analysis in patient and organizational outcomes research. Nurs Res. 2003;52(1):61–65. doi: 10.1097/00006199-200301000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Olejnik S, Algina J. Measures of effect size for comparative studies: applications, interpretations, and limitations. Contemp Educ Psychol. 2000;25(3):241–286. doi: 10.1006/ceps.2000.1040. [DOI] [PubMed] [Google Scholar]
- 22.Raudenbush SW, Bryk AS, Cheong AS, Fai YF, Congdon RT, du Toit M. HLM 7: Hierarchical linear and nonlinear modeling. Lincolnwood, IL: Scientific Software International; 2011. [Google Scholar]
- 23.SAS Institute Inc. SAS/STAT 9.3 User’s Guide. Cary, NC: SAS Institute Inc; 2013. [Google Scholar]
- 24.Nguyen-Oghalai TU, Ottenbacher KJ, Granger CV, Smith ST, Goodwin JS. Impact of osteoarthritis on rehabilitation for persons with hip fracture. Arthritis Rheum. 2006;55(6):920–924. doi: 10.1002/art.22345. [DOI] [PubMed] [Google Scholar]
- 25.Reistetter TA, Graham JE, Deutsch A, Markello SJ, Granger CV, Ottenbacher KJ. Diabetes comorbidity and age influence rehabilitation outcomes after hip fracture. Diabetes Care. 2011;34(6):1375–1377. doi: 10.2337/dc10-2220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59(3):255–263. doi: 10.1093/gerona/59.3.m255. [DOI] [PubMed] [Google Scholar]
- 27.Beaupre LA, Binder EF, Cameron ID, et al. Maximising functional recovery following hip fracture in frail seniors. Best Pract Res Clin Rheumatol. 2013;27(6):771–788. doi: 10.1016/j.berh.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Colon-Emeric CS. Recent advances: osteoporosis in the “oldest old”. Curr Osteoporos Rep. 2013;11(4):270–275. doi: 10.1007/s11914-013-0158-z. [DOI] [PubMed] [Google Scholar]
- 29.Sterling RS. Gender and race/ethnicity differences in hip fracture incidence, morbidity, mortality, and function. Clin Orthop Relat Res. 2011;469(7):1913–1918. doi: 10.1007/s11999-010-1736-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arinzon Z, Shabat S, Peisakh A, Gepstein R, Berner YN. Gender differences influence the outcome of geriatric rehabilitation following hip fracture. Arch Gerontol Geriatr. 2010;50(1):86–91. doi: 10.1016/j.archger.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 31.Morrison RS, Magaziner J, McLaughlin MA, et al. The impact of post-operative pain on outcomes following hip fracture. Pain. 2003;103(3):303–311. doi: 10.1016/S0304-3959(02)00458-X. [DOI] [PubMed] [Google Scholar]
- 32.Abou-Setta AM, Beaupre LA, Rashiq S, et al. Comparative effectiveness of pain management interventions for hip fracture: a systematic review. Ann Intern Med. 2011;155(4):234–245. doi: 10.7326/0003-4819-155-4-201108160-00346. [DOI] [PubMed] [Google Scholar]
- 33.Graham JE, Chang PF, Berges IM, Granger CV, Ottenbacher KJ. Race/ethnicity and outcomes following inpatient rehabilitation for hip fracture. J Gerontol A Biol Sci Med Sci. 2008;63(8):860–866. doi: 10.1093/gerona/63.8.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.National Rural Health Resource Center. Flex Program. 2013 http://www.ruralcenter.org/tasc/flex. Accessed Dec. 3, 2013.
- 35.Thompson JM, McCue MJ. Performance of freestanding inpatient rehabilitation hospitals before and after the rehabilitation prospective payment system. Health Care Manage Rev. 2010;35(1):36–45. doi: 10.1097/HMR.0b013e3181b475de. [DOI] [PubMed] [Google Scholar]
- 36.McCue MJ, Thompson JM. HealthSouth’s inpatient rehabilitation facilities: how does their performance compare with other for-profit and nonprofit inpatient rehabilitation facilities? Arch Phys Med Rehabil. 2010;91(5):708–713. doi: 10.1016/j.apmr.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 37.Magaziner J, Hawkes W, Hebel JR, et al. Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci. 2000;55(9):M498–507. doi: 10.1093/gerona/55.9.m498. [DOI] [PubMed] [Google Scholar]
- 38.Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc. 2006;54(5):743–749. doi: 10.1111/j.1532-5415.2006.00701.x. [DOI] [PubMed] [Google Scholar]
- 39.Miller RR, Shardell MD, Hicks GE, et al. Association between interleukin-6 and lower extremity function after hip fracture–the role of muscle mass and strength. J Am Geriatr Soc. 2008;56(6):1050–1056. doi: 10.1111/j.1532-5415.2008.01708.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reider L, Hawkes W, Hebel JR, et al. The association between body mass index, weight loss and physical function in the year following a hip fracture. J Nutr Health Aging. 2013;17(1):91–95. doi: 10.1007/s12603-012-0073-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jette AM. Toward a common language for function, disability, and health. Phys Ther. 2006;86(5):726–734. [PubMed] [Google Scholar]
- 42.Jette AM. Toward a common language of disablement. J Gerontol A Biol Sci Med Sci. 2009;64(11):1165–1168. doi: 10.1093/gerona/glp093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cacace M, Ettelt S, Mays N, Nolte E. Assessing quality in cross-country comparisons of health systems and policies: towards a set of generic quality criteria. Health Policy. 2013;112(1-2):156–162. doi: 10.1016/j.healthpol.2013.03.020. [DOI] [PubMed] [Google Scholar]
- 44.Dijkers MP. Rehabilitation treatment taxonomy: establishing common ground. Arch Phys Med Rehabil. 2014;95(1 Suppl):S1–5.e2. doi: 10.1016/j.apmr.2013.09.023. [DOI] [PubMed] [Google Scholar]
- 45.Kaplan HC, Brady PW, Dritz MC, et al. The influence of context on quality improvement success in health care: a systematic review of the literature. Milbank Q. 2010;88(4):500–559. doi: 10.1111/j.1468-0009.2010.00611.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Allen SM, Piette ER, Mor V. The adverse consequences of unmet need among older persons living in the community: dual-eligible versus medicare-only beneficiaries. J Gerontol B Psychol Sci Soc Sci. 2014;69(Suppl 1):S51–58. doi: 10.1093/geronb/gbu124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tajeu GS, Delzell E, Smith W, et al. Death, debility, and destitution following hip fracture. J Gerontol A Biol Sci Med Sci. 2014;69(3):346–353. doi: 10.1093/gerona/glt105. [DOI] [PMC free article] [PubMed] [Google Scholar]


