Abstract
Aims and Objectives
The purpose of this literature review was to summarize the current state of knowledge of symptom clusters research from studies that included, as part of their sample, patients who were receiving primary or adjuvant chemotherapy.
Background
Since the concept of a symptom cluster was first introduced into the oncology literature in 2001, only four comprehensive reviews of symptom clusters research in oncology patients were identified that provide insights into this important concept in symptom management research.
Design
A comprehensive review of the literature.
Methods
A comprehensive literature search was conducted for the years 2000 to 2016. Only 19 studies met the inclusion criteria for this literature review. These studies were evaluated in terms of the symptom assessment instruments used; the statistical analysis methods used; the symptom dimension(s) used to create the symptom cluster(s); the number and types of symptom clusters identified; and whether the specific symptom clusters changed over time.
Results
The number of symptom clusters identified ranged from one to seven. The majority of the studies used some type of factor analysis to create the symptom clusters. The most common symptom dimension used to create the clusters was symptom severity. A “gastrointestinal symptom cluster” was the most common symptom cluster identified. Across the eight longitudinal studies, for half of these studies the symptom clusters remained relatively stable over time.
Conclusions
Additional research is needed in oncology patients to address the assessment of symptom clusters, the specific nature of symptom clusters, and whether symptom clusters change over time.
Keywords: symptoms, symptom clusters, oncology, chemotherapy
INTRODUCTION
Over 15 years ago, Dodd and colleagues published the first study on symptom clusters in oncology patients (Dodd, Miaskowski, & Paul, 2001). In that paper, a symptom cluster was defined as: “Three or more concurrent symptoms that are related to each other but are not required to have the same etiology”[p.468]. In 2005, Kim and colleagues,(Kim, McGuire, Tulman, & Barsevick, 2005) revised the definition of a symptom cluster to be: “two or more symptoms that are related to each other and occur together. Symptom clusters are composed of stable groups of symptoms, are relatively independent of other clusters and may reveal specific underlying concepts of symptoms. Relationships among symptoms within a cluster should be stronger than relationships among symptoms across different clusters. Symptoms in a cluster may or may not share the same etiology” [p. 278].
More recently, an expert panel called for a comprehensive evaluation of symptom clusters research (Miaskowski et al., 2017). Given that patients with chronic conditions rarely present with a single symptom, the concept of a symptom cluster has important implications for clinical practice. However, as noted in the report from the expert panel, numerous questions remain unanswered in the area of symptom cluster research.
Since most of the research on symptom clusters was done in oncology patients, one way to evaluate the “state of the science” in symptom clusters research in oncology patients is to conduct a review of the literature. A synthesis of the current state of knowledge, that is organized around some of the key questions in symptom clusters research will provide a foundation for future studies in this important area of scientific inquiry
Previous reviews of symptom clusters research in oncology
Since the concept of a symptom cluster was first introduced into the oncology literature in 2001, only four comprehensive reviews were identified that provide insights into this important concept in symptom management research (Dodd, Miaskowski, & Lee, 2004; Fan, Filipczak, & Chow, 2007; Nguyen et al., 2011; Xiao, 2010). While several additional reviews of symptom clusters research were published on a variety of topics, (E. Chen et al., 2011; Dong, Butow, Costa, Lovell, & Agar, 2014; Thavarajah et al., 2012) we critiqued the four reviews that included studies whose samples, at least in part were receiving primary or adjuvant chemotherapy (CTX).
In the first review published by Dodd and colleagues (Dodd et al., 2004), only three studies were identified that evaluated symptom clusters in oncology patients. All three of these studies evaluated the association between a pre-specified symptom cluster and a patient outcome (e.g., functional status). In two of these studies that evaluated patients with heterogeneous cancer diagnoses (Dodd et al., 2001; Given, Given, Azzouz, & Stommel, 2001), pain, fatigue, and sleep disturbance was the pre-specified symptom cluster. In the third study of patients with breast cancer (Gaston-Johansson, Fall-Dickson, Bakos, & Kennedy, 1999), the pre-specified symptom cluster was pain, fatigue, and depression. All of the symptoms in these studies were selected because previous research had demonstrated that they were moderately to highly correlated with each other. Findings from this review suggest that none of the studies identified a symptom cluster “de novo” using analytic techniques like cluster analysis or factor analysis (Miaskowski, Aouizerat, Dodd, & Cooper, 2007). In addition, no studies were found that evaluated the occurrence of symptom clusters in children or adolescents, or by stage of cancer, or across the continuum of cancer care. The authors concluded their review by enumerating key areas for future research on symptom clusters (e.g., whether the occurrence of a symptom cluster influences patient outcomes).
The second review of symptom clusters research spanned the years 1997 to 2006 (Fan et al., 2007). The purposes of this review were to identify the occurrence of common symptom clusters in oncology patients and to evaluate for predictors of symptom clusters. Of the twelve studies identified, seven evaluated patients with heterogeneous cancer diagnoses (M. L. Chen & Tseng, 2006; Cleeland et al., 2000; Ivanova et al., 2005; Okuyama et al., 2003; Walsh & Rybicki, 2006; X. S. Wang et al., 2006; X. S. Wang et al., 2004) and five evaluated patients with a single cancer diagnosis (i.e., three evaluated symptom clusters in breast cancer patients (Bender, Ergyn, Rosenzweig, Cohen, & Sereika, 2005; Glaus et al., 2006; Ridner, 2005), two evaluated symptom clusters in lung cancer patients ((Gift, Jablonski, Stommel, & Given, 2004; Sarna & Brecht, 1997)). Across these studies, sample sizes ranged from 60 (Sarna & Brecht, 1997) to 922 (Walsh & Rybicki, 2006).
For the seven studies that evaluated for symptom clusters in patients with a variety of cancer diagnoses (M. L. Chen & Tseng, 2006; Cleeland et al., 2000; Ivanova et al., 2005; Okuyama et al., 2003; Walsh & Rybicki, 2006; X. S. Wang et al., 2006; X. S. Wang et al., 2004), several observations are worth noting. First, the MD Anderson Symptom Inventory (MDASI) (Cleeland et al., 2000) was used to assess symptoms in six of the seven studies. Rather than evaluate a pre-specified symptom cluster, all seven studies created symptom clusters “de novo” (Miaskowski et al., 2007). Factor analysis was used in six of the seven studies to identify the symptom clusters (M. L. Chen & Tseng, 2006; Cleeland et al., 2000; Ivanova et al., 2005; Okuyama et al., 2003; X. S. Wang et al., 2006; X. S. Wang et al., 2004). The two most common symptom clusters were a “general” symptom cluster and a “gastrointestinal” (GI) symptom cluster.
As part of this second review (Fan et al., 2007), three studies evaluated symptom clusters in patients with breast cancer (Bender et al., 2005; Glaus et al., 2006; Ridner, 2005) and two included patients with lung cancer (Gift et al., 2004; Sarna & Brecht, 1997). Across these five studies, with homogenous samples in terms of their cancer diagnoses, no consistent symptom assessment tool or statistical approach was used to identify the symptom clusters. In addition, the symptom clusters identified within each cancer diagnosis were inconsistent. Based on the findings from their review (Fan et al., 2007), Fan and colleagues concluded that it may be too early to confirm or deny the existence of common symptom clusters in oncology patients. In addition, they suggested that a consensus needed to be reached on the definition of a symptom cluster; as well as on the symptoms that should be assessed and the statistical methods that should be used to identify symptom clusters.
An updated review of the literature on symptom clusters spanned the years 1999 to 2010 (Xiao, 2010). A total of 61 studies were evaluated of which 22 used a longitudinal design. The sample sizes ranged from 15 to 2,161. The majority of these studies evaluated heterogeneous samples in terms of cancer diagnoses. A wide variety of symptom assessment tools were used across the 61 studies. The studies were divided into two groups: the “most common symptoms” approach (i.e., researchers evaluated the most common symptoms experienced by oncology patients and used these symptoms to identify symptom clusters) and the “all-possible symptoms” approach (i.e., a more commonly used approach, where the researchers evaluated a large number of symptoms that oncology patients may experience to identify symptom clusters rather than using only the most common symptoms). In the “most-common symptoms” approach, which included 20 studies, 80.0% of the studies used a combination of correlation and/or regression analyses to identify symptom clusters. In the “all-possible symptoms” approach, factor analysis was used in 27.0% of the studies and cluster analyses in 21.0% of the studies to create the symptom clusters.
Across the 61 studies, the types of symptom clusters identified were highly variable. However, the most common symptom clusters were: pain and fatigue; pain and sleep disturbance; depression, fatigue and pain; and a cluster labeled GI. At the end of their review (Xiao, 2010), Xiao recommended that additional research was needed to operationally define a symptom cluster; develop theoretical frameworks for the use of symptom clusters in oncology; determine the best methods of analysis; diversify the populations of patients evaluated; and explore how symptom clusters influence patient outcomes.
In the most recent review of symptom clusters research (Nguyen et al., 2011), the five studies that were evaluated included only patients with breast cancer (Bender et al., 2005; Fu et al., 2009; Glaus et al., 2006; Kim, Barsevick, Tulman, & McDermott, 2008; Ridner, 2005). Across these studies, the sample sizes ranged from 64 (Ridner, 2005) to 373 (Glaus et al., 2006). To identify the symptom clusters de novo, two studies used factor analysis (Fu et al., 2009; Kim et al., 2008), two used cluster analysis (Bender et al., 2005; Glaus et al., 2006), and one used analysis of variance (ANOVA) (Ridner, 2005). One of the five studies assessed symptom clusters in women experiencing menopausal symptoms (Glaus et al., 2006) and another evaluated women with lymphedema (Ridner, 2005). The instruments used to evaluate for symptom clusters, as well as the symptoms identified, varied across these five studies. No common symptom cluster was found across these five studies.
Nguyen and colleagues concluded that even though symptom clusters were evaluated in patients with a single cancer diagnosis, several issues warrant consideration (Nguyen et al., 2011). For example, among the five studies (Bender et al., 2005; Fu et al., 2009; Glaus et al., 2006; Kim et al., 2008; Ridner, 2005), three different methods of analysis were used; symptom data were measured at varying time points; and only one study used a longitudinal design. Of note, while several symptoms were found within a number of symptom clusters, none of these symptoms were included in the same symptom cluster. In addition, type of treatment, the symptom dimension used to create the symptom clusters, and temporal measurements of the symptom clusters were not described in this literature review of patients with breast cancer.
Issues in symptom clusters research
While these four reviews provide an excellent overview of symptom clusters research in oncology patients, none of them provided a detailed evaluation of the major issues in this field of inquiry. In fact, based on the findings from these four reviews (Dodd et al., 2004; Fan et al., 2007; Nguyen et al., 2011; Xiao, 2010), numerous unanswered questions remain about this emerging area of symptom management research. For example, which analytical approaches (e.g., cluster analysis, factor analysis) and which dimensions of the symptom experience (e.g., occurrence, severity, distress) should be used to identify symptom clusters. An equally important consideration that warrants additional evaluation includes whether or not the number of symptoms evaluated influences the number of symptom clusters identified and the specific symptoms within a cluster. In addition, questions regarding whether or not the number and types of symptom clusters vary based on cancer diagnoses (i.e., whether the number and types of symptom clusters vary based on whether the sample includes patients who are heterogeneous or homogeneous with respect to their cancer diagnosis), cancer treatments (i.e., whether the number and types of symptom clusters vary based on whether the sample includes patient who are heterogeneous or homogeneous with respect to their cancer treatment), and timing of the symptom assessments warrant consideration in future reviews.
Given the numerous questions and issues that warrant investigation in symptom clusters research, as well as the heterogeneous nature of the four reviews conducted to date (Dodd et al., 2004; Fan et al., 2007; Nguyen et al., 2011; Xiao, 2010), this review of symptom clusters research focused on studies that included, as part of their sample, patients who were receiving primary or adjuvant cancer CTX.
This review was designed with the following objectives: to summarize the current state of knowledge of symptom clusters’ research from studies that included, as part of their sample, patients who received primary or adjuvant CTX; to identify the most common symptom assessment instruments used; to determine the most common statistical approaches used to create the clusters; to identify the symptom dimensions used to create the symptom clusters; to determine the average number of symptom clusters identified; to evaluate the specific symptoms identified within each cluster; and to determine whether symptom clusters changed over time.
METHODS
A comprehensive literature search was conducted for the years 2000 to 2016. The following databases were accessed for this review: PubMed, the Cochrane Library, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Google Scholar, and PsycINFO. The key words used were: symptom clusters AND cancer not syndrome; symptom cluster AND cancer; symptoms, AND clusters, AND cancer; and symptom clusters, AND CTX, AND patients; and neoplasms, symptom clusters, AND cancer patients, AND CTX, AND treatment. Studies were included if they met all of the following criteria: (1) the entire sample had a cancer diagnosis; (2) the sample included, at least in part, patients who were receiving primary (i.e., initial treatment) or adjuvant (i.e., CTX following primary cancer treatment) CTX; (3) patients were ≥18 years of age; and (4) identified a symptom cluster in the analysis. Studies were excluded if patients were in the advanced stage of their cancer (i.e., receiving palliative or hospice care); if patients had completed cancer treatment and were described as cancer survivors; or if the study evaluated a pre-specified symptom cluster.
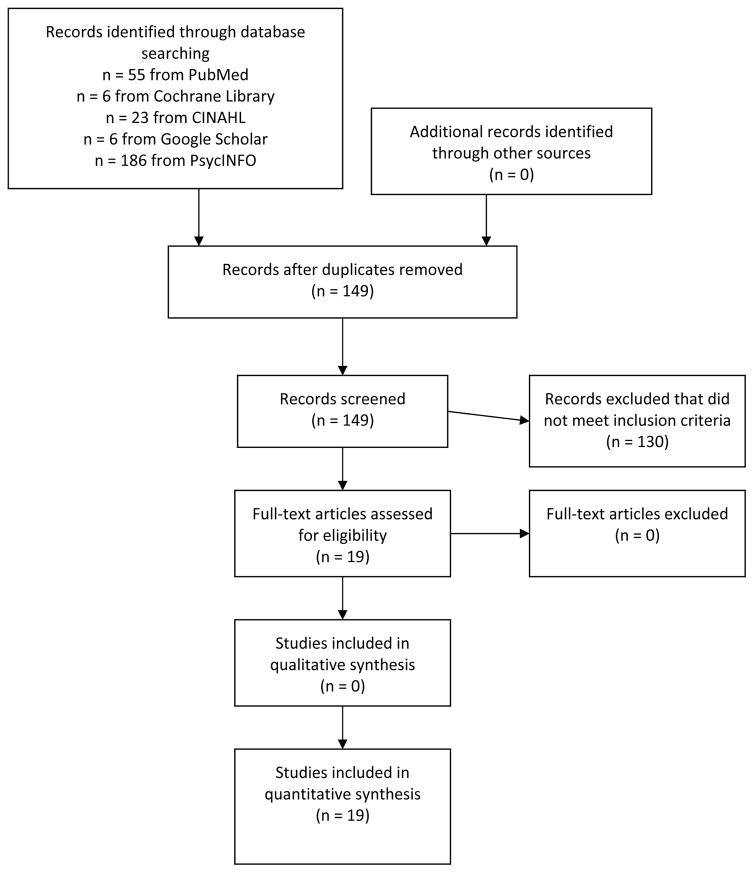
As shown in Figure 1, in the final search with a reference librarian, 55 papers were identified using the PubMed database; 6 from the Cochrane Library; 23 from CINAHL; 6 from Google Scholar; and 186 from PsycINFO. The majority of these papers were eliminated because they did not directly relate to symptom clusters in cancer patients. Duplicate articles found across the databases were eliminated. Using our pre-specified inclusion and exclusion criteria, 13 studies were selected from the PubMed, four from the Google Scholar, and two from the PsycINFO searches. A total of nineteen studies met the criteria for inclusion in this literature review (J. K. Brown, Cooley, Chernecky, & Sarna, 2011; M. L. Chen & Lin, 2007; M. L. Chen & Tseng, 2006; Gift et al., 2004; Gift, Stommel, Jablonski, & Given, 2003; Huang et al., 2016; Hwang, Cho, & Yoo, 2016; Karabulut, Erci, Ozer, & Ozdemir, 2010; Kim et al., 2008; Molassiotis, Wengstrom, & Kearney, 2010; Phligbua et al., 2013; Ryu et al., 2010; Skerman, Yates, & Battistutta, 2012a; Suwisith et al., 2008; Thomas et al., 2014; D. Wang & Fu, 2014; S. Y. Wang, Tsai, Chen, Lin, & Lin, 2008; Yamagishi, Morita, Miyashita, & Kimura, 2009; Yates et al., 2015).
Figure 1.
PRISMA diagram of the literature search
To be able to answer the specific aims of this review, findings from these nineteen studies are summarized in Tables 1 through 4. The tables are grouped by study design (i.e., cross-sectional or longitudinal) and by whether or not the sample included only a single cancer diagnosis (i.e., homogeneous sample) or multiple cancer diagnoses (i.e., heterogeneous sample). The studies are summarized in four tables (i.e., cross-sectional heterogeneous samples (Table 1); cross-sectional homogeneous samples (Table 2); longitudinal heterogeneous samples (Table 3); and longitudinal homogeneous samples (Table 4)). This organizational approach was chosen to be able to evaluate whether symptom clusters were different when samples included patients with only a single cancer diagnosis or heterogeneous cancer diagnoses and whether or not the symptom clusters changed over time.
Table 1.
Cross-sectional Studies of Symptom Clusters in Heterogeneous Samples of Oncology Patients
| Author, Year, Title, Purpose, and Design | Sample Size, Patient Characteristics, Time of Symptom Assessment | Symptom Assessment Instrument(s), Number of Symptoms on Instrument; Statistical Analysis Method, Symptom Dimension(s) Used to Create Symptom Clusters | Number of Symptom Clusters, Specific Symptoms Within Each Cluster | Strengths and Limitations |
|---|---|---|---|---|
|
Chen et al., 2006 Title: Symptom Clusters in Cancer Patients Purpose(s): To identify symptom clusters experienced by patients with various cancer diagnoses and validate the conceptual meanings of the identified clusters Design: Cross-sectional |
N=151 Mean age: 50.1 (SD=14.41), range: 18–79 Female: 40.4% Inpatients: n=128 Outpatients: n=23 Diagnosis:
Time of symptom assessment: Range: 0–394 days; median of 24 days since cancer diagnosis
|
Instrument(s): MDASI: 13 items Depression Subscale of the HADS-D: 14 items Analysis: EFA with principal axis factoring Dimension(s): Severity |
3 symptom clusters identified: Sickness symptoms: pain, fatigue, sleep disturbance, lack of appetite, drowsiness GI symptoms: nausea, vomiting Emotional symptoms: distress, sadness |
Strengths: Evaluated conceptual meanings of symptom clusters Limitations: MDASI assessed only 13 symptoms Disease specific symptoms were not evaluated Symptom clusters created using only symptom severity scores Cross-sectional design Primarily evaluated inpatients |
|
Chen et al., 2007 Title: Cancer Symptom Clusters: A Validation Study Purpose(s): To validate the 3 factor symptom structure by using CFA in a larger sample of cancer patients and to examine how 4 disease/treatment variables (diagnosis, disease stage, cancer treatment, hospitalization) and one outcome variable (functional status) were associated with the 3 symptom factors (sickness symptoms, GI symptoms, emotional symptoms) Design: Cross-sectional |
N=321 Mean age: 60.7 (SD=13.78), range: 22–97 Female: 54.5% Outpatients: 76.9% Diagnosis:
|
Instrument(s): MDASI-T: 13 items Analysis: CFA with maximum likelihood estimation. 9 MDASI symptoms used to build the measurement model Dimension(s): Severity |
3 symptom clusters identified: Sickness symptoms: pain, fatigue, disturbed sleep, lack of appetite, drowsiness GI symptoms: nausea, vomiting Emotional symptoms: distress, sadness |
Strengths Evaluated relationships between symptom cluster “scores” and disease and treatment characteristics Demonstrated that higher symptom cluster “scores” were associated with decreased functional status Limitations: Used only 9 symptoms from the MDASI-T Heterogeneous cancer diagnoses Cross-sectional design |
|
Karabulu et al., 2010 Title: Symptom Clusters and Experiences of Patients with Cancer Purpose(s): To characterize the prevalence and severity of symptoms in Turkish patients with cancer and describe the clustering symptoms Design: Cross-sectional |
N=287 Female: 44.3% Diagnosis:
2.9 years after diagnosis |
Instrument(s): MDASI: 13 items Analysis: Hierarchical cluster analysis Dimension(s): Severity Interference |
3 symptom clusters identified: Cluster 1: general activity, mood, work, relations with other people, walking, enjoyment of life. Cluster 2: sleep disturbance, difficulty in remembering, pain, distress, sadness, fatigue, dry mouth, appetite loss Cluster 3: nausea, vomiting, shortness of breath, numbness, drowsiness |
Strengths: First study in Turkish oncology patients Relatively large sample size Limitations: Cross-sectional design Inclusion of interference items in the symptom cluster analysis Symptom clusters were not named MDASI assesses only 13 items |
|
Yamagishi, et al., 2009 Title: Symptom Prevalence and Longitudinal Follow-Up in Cancer Outpatients Receiving Chemotherapy Purpose(s): To clarify the prevalence of physical symptoms and concerns among a representative sample of cancer patients receiving CTX in the outpatient setting; to evaluate symptom clusters in this study population and; to explore longitudinal change and the effects of physical symptoms on the DT Design: Cross-sectional |
N=462 Mean age: 62.0 (SD=11.0), range: 52–74 Female: 55% Diagnosis:
Time of symptom assessment: At start of initial CTX |
Instrument(s): Investigators developed the instrument using 8 physical symptoms from the MDASI; presence or absence of oral problems, fever, and insomnia; overall rating of QOL from EORTC questionnaires; distress thermometer Analysis: Cluster analysis Dimension(s): Authors did not specify what items were included in the cluster analysis |
4 symptom clusters identified: Cluster 1: fatigue, somnolence Cluster 2: pain, dyspnea, numbness Cluster 3: nausea, appetite loss, constipation Cluster 4: psychological distress |
Strengths: Large sample size Single treatment at the induction of CTX Limitations: Cross-sectional study Type of cluster analysis not specified Heterogeneous cancer diagnoses Symptom clusters not named Unclear which symptoms and dimensions were included in the cluster analysis |
|
Yates et al., 2015 Title: Differences in Composition of Symptom Clusters Between Older and Younger Patients Purpose(s): To identify and compare symptom clusters in younger (<60 years) and older (≥60 years) patients undergoing cancer treatment Design: Three combined studies: Symptom Clusters Study: Prospective, longitudinal Fatigue, Pain, and Sleep Study: Longitudinal Symptom Prevalence Study: Descriptive, cross-sectional |
N=263 (<60 years), mean age: 50.3 (SD=7.7) N=330 (≥60 years), mean age: 70.1 (SD=6.5) Group mean age: 61.3 Female: 54.6% Outpatients: 100% Diagnosis (<60, ≥60):
For the longitudinal studies, at the time of recruitment into the study |
Instrument(s): MSAS: 32 items ECOG: functional status rated by clinician (i.e., Australian study) on a 0 to 4 scale KPS: functional status (i.e., U.S. study) on a 0 to 100 scale ECOG: used for combined study on a 0 to 4 scale Analysis: Exploratory factor analysis Dimension(s): Occurrence |
For patients <60 years: 7 symptom clusters were identified: Treatment related: dry mouth, difficulty swallowing, SOB, lack of appetite, nausea, vomiting, lack of energy, change in food tastes, feeling dizzy, cough, weight loss, constipation, pain, feeling drowsy, mouth sores, feeling nervous, I do not look like myself, difficulty concentrating, feeling bloated Mood/Cognitive: worrying, feeling sad, feeling nervous, feeling irritable, difficulty concentrating, lack of energy, difficulty sleeping, problems with sexual interest, I do not look like myself Malaise: lack of energy, feeling drowsy, lack of appetite, nausea, difficulty concentrating, diarrhea, feeling bloated, feeling nervous, difficulty sleeping Treatment related GI: vomiting, nausea, not itching GU: problems with urination, problems with sexual interest Hormonal: sweats, difficulty sleeping, pain, not weight loss CTX toxicity: hair loss, change in food tastes, I do not look like myself, mouth sores, constipation, feeling bloated, swelling of arms/legs, dry mouth For patients ≥60 years: 7 symptom clusters were identified: Malaise: feeling drowsy, lack of energy, difficulty concentrating, difficulty sleeping, feeling nervous, feeling sad, feeling irritable, feeling dizzy, problems with sexual interest, sweats Mood/Cognitive: worrying, feeling sad, feeling nervous, feeling irritable, lack of energy, difficulty concentrating, lack of appetite, nausea, feeling drowsy, change in food tastes, constipation, I do not look like myself, feeling bloated, numbness/tingling in hands/feet Aerodigestive: SOB, cough, dry mouth, difficulty swallowing, lack of appetite, feeling bloated, feeling nervous, lack of energy, nausea, swelling of arms/legs, feeling dizzy, feeling sad, pain, feeling drowsy, difficulty sleeping GU: problems with urination, diarrhea, problems with sexual interest, feeling irritable Nutrition: weight loss, lack of appetite, constipation, change in food tastes, I do not look like myself, lack of energy, feeling drowsy, nausea Aging related: difficulty swallowing, dry mouth, constipation, feeling drowsy, change in food tastes, nausea CTX toxicity: skin changes, hair loss, I do not look like myself, swelling of arms/legs, feeling sad |
Strengths: First study to identify four core symptom clusters and differentiate between symptom clusters based on age groups Found that those ≥60 years had consistently lower symptom occurrence rates Identified that cancer treatment approaches may differ between older and younger patients Large sample size Combined three studies from two geographic regions Limitations: Only used one symptom dimension to create the clusters across the three studies Included patients with metastatic disease which may have had an effect on the symptom experience Excluded patients who had surgery Race/ethnicity not identified |
Abbreviations: CNS, Central Nervous System; CTX, chemotherapy; CFA, Confirmatory Factor Analysis; DT, Distress Thermometer; EORTC, European Organization for Research and Treatment of Cancer; EFA, Exploratory Factor Analysis; GI, gastrointestinal; HADS, Hospital Anxiety and Depression Scale; MDASI, MD Anderson Symptom Inventory; MDASI-T, MD Anderson Symptom Inventory-Taiwanese; MSAS, Memorial Symptom Assessment Scale; QOL, quality of life; RT, radiation therapy; SOB, shortness of breath; UGI, upper-gastrointestinal.
Table 4.
Longitudinal Studies of Symptom Clusters in Homogeneous Samples of Oncology Patients
| Author, Year, Title, Purpose, and Design | Sample Size, Patient Characteristics, Time of Symptom Assessment | Symptom Assessment Instrument(s), Number of Symptoms on Instrument, Statistical Analysis Method, Symptom Dimension(s) Used to Create Symptom Clusters | Number of Symptom Clusters, Number of Symptoms Within Each Cluster, Change in Symptom Clusters Over Time | Strengths and Limitations |
|---|---|---|---|---|
|
Brown et al., 2011 Title: A Symptom Cluster and Sentinel Symptom Experienced by Women With Lung Cancer Purpose(s): Describe the occurrence, severity, and clusters of symptoms experienced by women with NSCLC; describe the relationships of demographic and clinical characteristics, health status factors, and meaning of illness with symptom experience and symptom clusters; and determine if a co-occurring sentinel symptom was associated with the presence of symptom clusters Design: Prospective, longitudinal |
N=196 Mean age: 65.4 (SD=11.4), range: 33–89 Female: 100% Outpatients: 100% Diagnosis: NSCLC: 100% Treatment:
|
Instrument(s): Lung Cancer Symptom Scale: 6 items Symptom Query Questionnaire: self report of symptoms during past 4 weeks obtained during a semi-structured interview Center for Epidemiologic Studies-Depression scale: 20 items Charlson Comorbidity Index: measures the presence of multiple co-morbidities Analysis: Symptoms on the LCSS were coded uniquely and analyzed to determine patterns of co-occurring symptoms Dimension(s): Occurrence |
1 un-named symptom cluster identified: Fatigue, shortness of breath, poor appetite, cough, pain Change in symptom clusters over time: The assessment of symptoms on the previous day revealed a 5-item symptom cluster for 64% of the patients. No predominant symptom cluster was identified for the assessment of the past 4 weeks. |
Strengths: First study to evaluate symptom experience of women with early stage NSCLC who were treated surgically Identified a co-occurring sentinel symptom (i.e., pain) that was the most highly correlated symptom with the presence of the 5-symptom cluster Limitations: Use of SQQ depended on patient’s recall of symptoms over the past 4 weeks which may have contributed to under-reporting Did not address sleep problems, weight loss or decreased concentration reported by 10%–23% of sample Did not use a standard statistical approach to identify symptom clusters Used an instrument with only 6 symptoms to assess symptom clusters |
|
Gift et al., 2003 Title: A Cluster of Symptoms Over Time in Patients With Lung Cancer Purpose(s): Determine whether symptom cluster identified at time of diagnosis remained at 3 and 6 months later; determine whether there was a difference in mean symptom number and mean level of symptom severity over time Design: Prospective, longitudinal |
N=112 Mean age: 72, (SD=4.9), range: 65–83 Female: 48% Outpatients: 100% Diagnosis: Lung cancer: 100% Treatment:
Time of diagnosis At 3 months At 6 months |
Instrument(s): Physical Symptom Experience Tool: 37 items, only 32 items were used in this analysis Analysis: Factor analysis Dimension(s): Occurrence |
1 un-named symptom cluster identified Fatigue, weakness, nausea, vomiting, loss of appetite, weight loss, altered taste Change in symptom clusters over time: Based on an evaluation of Cronbach’s alpha, the symptom cluster met the requisite reliability for a summated rating scale |
Strengths: Symptom cluster identified as an independent predictor of mortality Evaluated mean symptom severity and the number of symptoms at diagnosis Evaluated symptoms in patients ≥ 65 of age Limitations: Secondary analysis Primarily White patients Only patients over 65 were eligible to participate; symptom reporting may be different in a younger age group |
|
Huang et al., 2016 Title: Symptom Clusters in Ovarian Cancer Patients with Chemotherapy After Surgery Purpose(s): To investigate ovarian cancer patients receiving adjuvant CTX throughout treatment; to identify symptom clusters; and to explore changes in symptom clusters over 4 time points. Design: Convenient sample, longitudinal |
N=111 Mean age: 53.7 (SD=10.89), range: 19–78 Female: 100% Outpatients: 100% Diagnosis: Ovarian cancer: 100% Treatment: CTX Time of symptom assessment: Time 1= before surgery Time 2= after first cycle Time 3= after third cycle Time 4= after sixth cycle of CTX |
Instrument(s): MSAS-Chinese: 32 items, only 20 items were used in this analysis Analysis: Exploratory factor analysis Dimension(s): Severity |
Number of symptom clusters a each Time point: T1=3 symptom clusters T2=5 symptom clusters T3=6 symptom clusters T4=6 symptom clusters T1: Pain-related: pain, feeling bloated, dizziness, weight loss Psychological: feeling nervous, feeling sad, anxiety Menopausal: lack of energy, dry mouth, difficulty sleeping, sweats, lack of appetite, feeling irritated T2: Pain-related: pain, feeling bloated, dizziness, weight loss Psychological: feeling nervous, feeling sad, anxiety, feeling irritated Menopausal: lack of energy, dry mouth, difficulty sleeping, sweats, lack of appetite, feeling irritated GI: lack of appetite, nausea, vomiting, weight loss Body image: hair loss, constipation T3: Pain-related: pain, feeling bloated, weight loss Psychological: feeling nervous, feeling sad, anxiety, feeling irritated Menopausal: lack of energy, dry mouth, difficulty sleeping, sweats, lack of appetite, feeling irritated GI: lack of appetite, nausea, vomiting, weight loss, change in the way food tastes Body image: hair loss, constipation, do not look like himself/herself Neurologic: numbness/tingling in hands/feet, dizziness T4: Pain-related: pain, feeling bloated, weight loss Psychological: feeling nervous, feeling sad, anxiety, feeling irritated Menopausal: lack of energy, dry mouth, difficulty sleeping, sweats, lack of appetite, feeling irritated GI: lack of appetite, nausea, vomiting, weight loss, change in the way food tastes Body image: hair loss, constipation, do not look like himself/herself Peripheral Neurologic: numbness/tingling in hands/feet, dizziness Change in symptom clusters over time: Three symptom clusters (i.e., pain-related, psychological, menopausal) remained relatively stable over time |
Strengths: Evaluated symptoms using a multidimensional symptom assessment instrument Evaluated changes in symptom clusters over 4 time points Evaluated symptom clusters in a sample of women not frequently studied in terms of the symptom experience Identified 3 symptom clusters consistent with previous studies (i.e., GI, psychological, menopausal) The majority of the patients received one type of CTX regimen Limitations: Symptom clusters were not evaluated after the completion of CTX Patients with disease recurrence were not evaluated Relatively small sample size |
|
Kim et al., 2008 Title: Treatment-Related Symptom Clusters in Breast Cancer: A Secondary Analysis Purpose(s): To identify treatment-related symptom clusters in breast cancer patients across three points in the treatment trajectory and to examine the influence of demographic/clinical variables on symptom clustering Design: Secondary analysis from a randomized clinical trial |
N=282 Mean age: 55.2 (SD=12.1), range: 30–83 Female: 100% Outpatients: 100% Diagnosis: Breast: 100% Treatment:
For CTX patient: Prior to CTX (Time 1), 48 hours after the second cycle of CTX (Time 2), and 48 hours after the third cycle of CTX (Time 3) For RT patients: Prior to RT (Time 1), during the last week of RT (Time 2), and one month after the completion of RT (Time 3) |
Instrument(s): General Fatigue Scale: 1 item Profile of Mood States-Short Form: Depression and Confusion subscales were used 10 items Pittsburgh Sleep Quality Index: 19 items Side Effect Checklist: 16 items Analysis: Common factor analysis with principal axis factoring Dimension(s): Severity |
2 symptom clusters identified: Psycho-neurological: depressed mood, cognitive disturbance, fatigue, insomnia, pain, hot flashes UGI: nausea, vomiting, decreased appetite Change in symptom clusters over time: The psycho-neurological symptom cluster was present at all three time points. The UGI symptom cluster was present at the second and third assessments |
Strengths: Investigated treatment-related symptom clusters and the influence of selected demographic and clinical characteristics at 3 time points across two treatments (i.e., CTX, RT) Limitations: Use of a single item to rate symptom severity The effect of confounding variables on symptom clustering were not controlled for in the analyses Under-representation of minorities and late stage breast cancer patients |
|
Phligbua et al., 2013 Title: Symptom Clusters and Quality of Life in Women with Breast Cancer Receiving Adjuvant Chemotherapy Purpose(s): To identify the existence of symptom clusters; to examine the influence of distressing symptoms on QOL in women with breast cancer at before, during, and 1 month after completion of neoadjuvant CTX Design: Prospective, longitudinal |
N=112 Mean age: 49.7 (SD=10.70), range: 19–73 Female: 100% Outpatients: 100% Diagnosis: Breast: 100% Treatment: Adjuvant CTX Time of symptom assessment: T1: before CTX T2: before receiving 2nd cycle T3: 1 month after CTX |
Instrument(s): Modified MSAS: 39 items FACT-B, 4.0: 36 items Analysis: Exploratory factor analysis with principal components (varimax) Dimension(s): Distress |
Time 1: 5 symptom clusters Time 2: 5 symptom clusters Time 3: 5 symptom clusters Time 1 Menopausal: sweats, night sweats, hot flashes, mood swings, feeling irritable, difficulty concentrating Discomfort: dizziness, joint pain, vaginal itching/irritation, constipation Postoperative: coughing, itching, numbness/tingling in hands/feet Fatigue: lack of energy and difficulty sleeping Psychological: feeling sad, worrying Time 2 GI-related fatigue: lack of energy, nausea, lack of appetite, pain, feeling drowsy, dizziness, taste changes Disturbed in mood: feeling irritable, feeling nervous, pain Psychologically-related self-image: “I don’t look like myself”, worrying, difficulty concentrating, hair loss, skin changes Discomfort: constipation, problems with urination, difficulty sleeping, feeling bloated Oral: mouth sore, dry mouth Time 3 GI-related fatigue: lack of energy, feeling drowsy, lack of appetite, taste changes Menopausal: sweats, hot flashes, night sweats, difficulty concentrating, difficulty sleeping, worrying, pain Disturbed in mood: mood swings, feeling irritable, joint pain Discomfort: numbness/tingling in hands/feet, dry mouth Self-image: “ I don’t look like myself”, hair loss, skin changes Change in symptom clusters over time: One symptom cluster (i.e., discomfort) remained relatively stable over time |
Strengths: Evaluated for differences across symptom dimensions and time points Evaluated menopausal symptoms (i.e., sweats, night sweats, hot flashes, mood swings) and its clustering with other symptoms commonly associated with menopause, after receiving CTX Identified a significant increase in menopausal symptoms associated with receiving adjuvant CTX Identified a menopausal cluster, psychologically-related self-image, and a GI-related fatigue symptom clusters that remained stable over CTX cycles Limitations: Symptoms and symptom clusters identified in text were inconsistent with the tables at each of the three time points Relatively small sample size Investigated only women with breast cancer who received adjuvant CTX at one university hospital |
Abbreviations: CTX, chemotherapy; FACT-B, Functional Assessment of Cancer Therapy Cancer-Breast, 4.0; GI, gastrointestinal; LCSS, Lung Cancer Symptom Scale; MSAS, Memorial Symptom Assessment Scale; NSCLC, non-small cell lung cancer; RT, radiation therapy; SQQ, Symptom Query Questionnaire; UGI, upper gastrointestinal.
Table 2.
Cross-sectional Studies of Symptom Clusters in Homogeneous Samples of Oncology Patients
| Author, Year, Title, Purpose, and Design | Sample Size, Patient Characteristics, Time of Symptom Assessment | Symptom Assessment Instrument(s), Number of Symptoms on Instrument; Statistical Analysis Method, Symptom Dimension(s) Used to Create Symptom Clusters | Number of Symptom Clusters, Specific Symptoms Within Each Cluster | Strengths and Limitations |
|---|---|---|---|---|
|
Gift et al., 2004 Title: Symptom Clusters in Elderly Patients with Lung Cancer Purpose(s): To determine whether symptoms co-occur in patients newly diagnosed with lung cancer; whether symptoms vary according to antecedents of stage of disease, comorbidities, treatment, or gender and; whether co-occurring symptoms affect performance Design: Cross-sectional |
N=220 Mean age: 72.0 (SD=5.02), range: 65–89 Female: 41% Outpatients: 100% Diagnosis: Lung cancer: 100% Treatment:
Four to eight weeks after diagnosis |
Instrument(s): Medical Outcomes Study (SF-36): only 16 items used in this analysis Physical Symptom Experience: 37 items Analysis: Exploratory maximum likelihood factor analysis Dimension(s): Occurrence Severity |
Only 1 stable symptom cluster was identified: Un-named cluster with 7 symptoms: nausea, fatigue, weakness, appetite loss, weight loss, altered taste, vomiting |
Strengths: Evaluated a homogeneous cancer type with a varying stage of disease Evaluated symptoms in elderly patients ≥ 65 Used physical symptom scales that are known to primarily address the physical dimension of symptoms Limitations: Did not find stable clusters in 3 of the 4 factor loadings Analysis consisted of predominantly white males The effects of age on functional status were not controlled for in this study Symptoms cluster groupings were different from other studies |
|
Hwang et al., 2016 Title: Symptom Clusters of Ovarian Cancer Patients Undergoing Chemotherapy, and Their Emotional Status and Quality of Life Purpose(s): To identify the symptoms experienced by ovarian cancer patients and the impact on their quality of life. Design: Cross-sectional |
N =192 Mean age: 49.3 (SD=12.9), range: 18–79 Female: 100% Inpatients: 100% Diagnosis: Ovarian: 100% Treatment: adjuvant CTX Time of symptom assessment: Receipt of adjuvant CTX following surgery, exact time not specified |
Instrument(s): Investigators developed a 48 item questionnaire: 32 items from the MSAS-SF, 13 items from the MDASI-Korean version, and 3 additional questions were added. HADS: 14 items FACT-O-Korean version, 4: 39 items that assess the quality of life in cancer patients Analysis: Factor analysis; analysis of variance; Scheffe test Dimension(s): Severity |
7 symptom clusters identified: Psychological distress: depression, worry, feeling sad, being sensitive, frequently being irritated, dissatisfaction with one’s appearance Fatigue-pain: lack of energy, fatigue, difficulty in concentration, changes in appetite, pain, nausea Abdominal discomfort: abdominal bloating, indigestion, abdominal pain, weight loss Flu-like symptom: cough, mild fever or body aches, feeling drowsy, fever, SOB Fluid accumulation: swelling in the legs, feeling swollen, weight gain, frequent urination Sexual disturbance: decreased interest in sex, difficulty performing the sexual act Neuropathy: numbness in hands and feet, insensitive in hands and feet |
Strengths: Identified an association between higher levels of anxiety and depression and a higher level of symptom burden Identified that all of the symptom clusters had a significant impact on patients’ QOL First study to evaluate the occurrence and severity of symptoms experienced by patients with ovarian cancer receiving CTX Identified fatigue, lack of energy, and numbness in hands/feet as the most frequently occurring symptoms Identified differences in symptom cluster factor scores by patient characteristics and emotional status Limitations: Recruited inpatients from only 2 university hospitals in South Korea Symptom questionnaires were not tested for criterion validity or test-retest reliability Did not assess symptoms over the course of treatment |
|
Ryu et al., 2010 Title: Symptom Clusters and Quality of Life in Korean Patients with Hepatocellular Carcinoma Purpose(s): To describe symptom experience in Korean patients with HCC; to explore whether multiple symptoms are clustered into groups of symptoms; to validate the conceptual meanings of the identified symptom clusters; and to explore the effect of the identified symptom clusters on QOL and mood in Korean patients with HCC Design: Cross-sectional |
N=180 Mean age: 55.3 (SD=10.1), range: not reported Female: 10.6% Inpatients: 100% Diagnosis: HCC: 100% Treatment: active treatment for HCC Time of symptom assessment:
|
Instrument(s): HADS: 14 items Symptom Checklist: 21 items FACT-H--Korean Version: 27 items ECOG: 1 item Child-Pugh Status: 3 classifications used to assess liver function; class A (5–6 points, mildly impaired); class B (7–9 points, moderately impaired); class C (10 or more, severely impaired) Analysis: EFA with principal axis factoring Dimension(s): Severity |
4 symptom clusters identified: Pain-appetite cluster: pain, nausea, loss of appetite, fever, change in taste Fatigue related cluster: feeling fatigued, back pain, lack of energy, sadness GI cluster: jaundice, stomach pain/discomfort, stomach swelling/cramps, diarrhea Itching-constipation cluster: Itching, constipation |
Strengths: Used 15 signs and symptoms that are common in patients with HCC to create symptom clusters Only study of symptom clusters in patients with HCC Limitations: Convenience sample, which limits the generalizability of the findings Cross-sectional design does not allow for an evaluation of changes in symptom clusters over time The majority of the patients were Buddhist and may have underreported their symptom experiences |
|
Suwisith, et al., 2008 Title: Symptom Clusters and Functional Status of Women with Breast Cancer Purpose(s): To investigate the existence of symptom clusters and their consequences in women with breast cancer undergoing CTX across two symptom dimensions (i.e., severity, distress) Design: Cross-sectional |
N =320 Mean age: 47.3 (SD=8.8), range: 17–68 Female: 100% Outpatients: 100% Diagnosis: Breast:100% Treatment: CTX Time of symptom assessment: After receiving CTX for seven days |
Instrument(s): MSAS: 32 items IFS-C: 39 items Analysis: Factor analysis; multiple regression Dimension(s): Severity Distress |
4 symptom clusters identified using severity ratings 3 symptom clusters identified using distress ratings Severity symptom clusters: Emotions related symptoms: Feeling sad, worrying, feeling irritable, feeling nervous, “I don’t look like myself”, difficulty concentrating, sleeping difficulty, sweating, constipation GI and fatigue related symptoms: Vomiting, lack of energy, lack of appetite, dizziness, feeling drowsy, SOB, feeling bloated Image related cutaneous symptoms: Hair loss, changes in food taste, mouth sore, skin change, difficulty swallowing Pain related discomfort symptoms: Numbness/tingling, pain, dry mouth Distress symptom clusters: Emotions and pain related discomfort symptoms: feeling nervous, difficulty concentrating, worrying, feeling sad, numbness/tingling, feeling irritable, sleeping difficulty, SOB, feeling bloated, sweating, pain GI symptoms: nausea, vomiting, lack of appetite, lack of energy, dizziness, feeling drowsy Image related cutaneous symptoms: mouth sore, hair loss, skin change, changes in food taste, difficulty swallowing, “I don’t look like myself”, constipation, dry mouth |
Strengths: Found that the GI and fatigue related symptom cluster explained the largest amount of variance in patients’ functional status Found that symptom clusters based on severity and distress ratings were not identical Limitations: The majority of the sample had stage II breast cancer The majority of the sample received a modified radical mastectomy Did not evaluate for symptoms experienced prior to mastectomy or prior to CTX |
|
Wang et al., 2008 Title: Symptom Clusters and Relationships to Symptom Interference with Daily Life in Taiwanese Lung Cancer Patients Purpose(s): To explore the experience of symptoms and to examine symptom clusters and their relationships to symptom interference in Taiwanese patients with lung cancer Design: Cross-sectional |
N=108 Mean age: 67.5 (SD=10.48), range: 41–90 Female: 36.1% Inpatients: 62% Outpatients: 38% Diagnosis: Lung cancer: 100% Treatment:
Not reported |
Instrument(s): MDASI-T: 13 items Analysis: EFA, CFA, and HCA Dimension(s): Severity |
2 symptom clusters identified using both CFA and HCA General symptoms: pain, fatigue, sleep disturbance, distress, shortness of breath, difficulty remembering, lack of appetite, drowsiness, dry mouth, sadness, numbness GI symptoms: nausea, vomiting |
Strengths: Identified symptom clusters similar to ones found in samples of patients with heterogeneous cancer diagnoses The general symptom cluster was highly correlated with symptom interference scores First study to explore the effect of symptom clusters on daily activities of Taiwanese patients with lung cancer Limitations: The rationale for using EFA, CFA, and HCA is not specified in the manuscript Evaluated only patients with localized lung cancer Cross-sectional design did not allow for the evaluation of changes in symptom clusters over time |
|
Wang et al., 2014 Title: Symptom Clusters and Quality of Life in China Patients With Lung Cancer Undergoing Chemotherapy Purpose(s): To describe symptom experienced by patients with lung cancer undergoing CTX; to explore whether multiple symptoms were clustered into groups of symptoms; to examine whether symptom clusters were related to demographic characteristics, to health characteristics; and to identify the impact of symptom clusters on QOL dimensions Design: Cross-sectional |
N=183 Mean age: 58.3 (SD=10.31), range: 32–84 Female: 36.1% Diagnosis: Lung cancer: 100% Treatment: CTX: 100% Time of symptom assessment: Not reported |
Instrument(s): FACT-L, 4.0: 27 items divided into 4 domains: physical—7 items; social/family-7 items; emotional—6 items; functional well being—7 items; lung specific—9 items MDASI-Chinese: 13 core symptom severity items Analysis: EFA with principal axis factoring Dimension(s): Severity |
3 symptom clusters identified: GI: nausea, vomiting Emotional: distressed, sad Fatigued related: feeling fatigued, disturbed sleep, pain |
Strengths: Investigated symptom clusters in patients at any stage of lung cancer First study in mainland China to investigate symptom clusters and test the relationship between symptom clusters and QOL in a homogeneous sample Limitations: Reported that patients from China experienced a similar level of symptom distress to patients in Europe and North America However, they did not directly measure symptom distress Cross-sectional design |
Abbreviations: CTX, chemotherapy; CFA, Confirmatory Factor Analysis; ECOG, Eastern Cooperative Oncology Group Performance Status; EFA, Exploratory Factor Analysis; FACT-H, Functional Assessment of Cancer Therapy-Hepatobiliary Cancer; FACT-L, Functional Assessment of Cancer Therapy-Lung Cancer 4.0; FACT-O, Functional Assessment of Cancer Therapy-Ovarian Cancer; GI, gastrointestinal; HADS, Hospital Anxiety and Depression Scale; HCC, Hepatocellular cancer; HCA, Hierarchical Cluster Analysis; IFS-CA, Inventory Functional Status-Cancer; MDASI, MD Anderson Symptom Inventory; MDASI-T, MD Anderson Symptom Inventory-Taiwanese; MSAS-SF, Memorial Symptom Assessment Scale-Short Form; QOL, quality of life; RT, radiation therapy; SOB, shortness of breath; SD, standard deviation.
Table 3.
Longitudinal Study of Symptom Clusters in a Heterogeneous Sample of Oncology Patients
| Author, Year, Title, Purpose, and Design | Sample Size, Patient Characteristics, Time of Symptom Assessment | Symptom Assessment Instrument(s), Number of Symptoms on Instrument; Statistical Analysis Method, Symptom Dimension(s) Used to Create Symptom Clusters | Number of Symptom Clusters Number of Symptoms Within Each Cluster, Change in Symptom Clusters Over Time |
Strengths and Limitations |
|---|---|---|---|---|
|
Molassiotis et al., 2010 Title: Symptom Cluster Patterns During the First Year After Diagnosis with Cancer Purpose(s): To explore the patterns of clusters over time, the stability, the statistical strength of any given clusters, and the symptom experience of patients who reported symptoms in a cluster Design: Prospective, longitudinal |
N=143 Mean age: not reported Age range: 30–93 Female: 45.7% Outpatients: 100% Diagnosis:
4 time points for up to one year: Peri-diagnosis 3 months 6 months 12 months |
Instrument(s): MSAS: 32 items Analysis: EFA with principal components analysis Dimension(s): Not reported |
6 symptom clusters identified: GI: nausea, vomiting, feeling bloated Emotional: with a number of psychological symptoms Respiratory: shortness of breath, cough Hand/foot: numbness; tingling of hand/feet, swelling of arms and legs Body image: hair loss, skin changes, one item “I do not like myself” Nutritional: weight-loss, difficulty swallowing, lack of appetite Change in symptom clusters over time: With slight variations, the six symptom clusters were relatively stable over time |
Strengths: First study to explore clusters of symptoms in cancer patients over the first 12 months after diagnosis, reporting cluster patterns, structure, and factor coefficients Used two criterion to evaluate the relationships among symptoms within a cluster (i.e., Cronbach alpha and inter-factor coefficients) Longitudinal study design Limitations: Did not report the results from the EFA or cluster analysis Patients were primarily of European descent Evaluated patients on a variety of treatment regimens |
|
Skerman et al., 2012 Title: Cancer-related Symptom Clusters for Symptom Management in Outpatients after Commencing Adjuvant Chemotherapy at 6 months and 12 months Purpose(s): To investigate symptom clusters over time for symptom management of a patient group after commencing adjuvant CTX Design: Descriptive, longitudinal |
N=219 Mean age: 52, range 18–79 Female: 63.9% Outpatients: 100% Diagnosis:
Time of symptom assessment:
|
Instrument(s): Rotterdam Symptom Checklist: 42 items (clinician modified) Analysis: Common factor analysis with oblique rotation Dimension(s): Distress |
5 symptom clusters identified: Vasomotor: headache, sweating, hot/cold spells, night sweats, dizziness, numbness/tingling, chest pains, heart pounding/palpitations Oral discomforts: sore throat, sore mouth/pain swallowing, difficulty swallowing, bad taste, loss of taste, dry mouth, deafness UGI: indigestion, heartburn, belching, stomach pain, nausea, low abdominal pain, constipation GI toxicities: poor appetite, vomiting, nausea, shivering, trembling, low abdominal pain, stomach pain, diarrhea, belching, loss of taste, sleepiness, fatigue, weakness Musculoskeletal discomforts/lethargy: weakness, muscle soreness, joint pain, heavy feelings in arms/legs, generalized pain, lower back pains, fatigue, sleepy during day, deafness Change in symptom clusters over time: all five symptom clusters identified were consistent across all three assessments |
Strengths: First longitudinal study to empirically derive symptom clusters Used a symptom inventory with a large number of symptoms Relatively large sample Single cancer treatment Longitudinal study Heterogeneous sample in terms of cancer diagnosis Used sophisticated statistical procedures to determine the number of symptom clusters (i.e. pattern coefficients) and specific symptoms within a cluster (i.e. structure coefficients) Limitations: Did not assess symptoms prior to treatment Only assessed physical symptoms |
|
Thomas et al., 2014 Title: A Longitudinal Analysis of Symptom Clusters in Cancer Patients and Their Sociodemographic Predictors Purpose(s): To identify the presence of symptom clusters from the time of diagnosis over the course of a full year; to explore the possible associations between the identified symptom clusters and demographic and medical characteristics; and to examine the association between the identified symptom clusters and emotional distress Design: Longitudinal |
N=877 at baseline; N=505 retained at 12 months Mean age: 60.7 (14.41), range: not reported Female: 41.5% Outpatients: 100% Diagnosis:
At least one month prior to screening
4 Time points: Time of diagnosis 3 months 6 months 12 months |
Instrument(s): Fatigue Thermometer: fatigue level within the past week on a 0 to 10 scale Pain Thermometer: pain level within the past week on a 0 to 10 scale Psychosocial Screen for Cancer (Part C): 10 items that assess anxiety and depression Sleep Problems (From Canadian Problem Checklist): Evaluated the presence/absence of sleep problems within past week Nutrition items: 2 items; patients indicated changes in weight and food intake Distress Thermometer: patients rate their distress level Analysis: Factor analysis Panel regression Dimension(s): Severity |
3 symptom clusters identified: Somatic: pain, fatigue, sleep Psychological: anxiety, depression Nutrition: weight, intake Change in symptom clusters over time: The three symptom clusters were relatively stable over time |
Strengths: Large sample size Longitudinal study design First study to evaluate symptom clusters at 4 time points from time of diagnosis up to one year in a heterogeneous sample Limitations: Did not use a comprehensive symptom assessment instrument to assess symptoms Unable to determine if changes in patients’ symptom experience differed by cancer diagnosis |
Abbreviations: CTX, chemotherapy; ECOG, Eastern Cooperative Oncology Group Performance Status; GI, gastrointestinal; GU, genito-urinary; HT, hormone treatment; KPS, Karnofsky Performance Status Scale; MSAS, Memorial Symptom Assessment Scale; UGI, upper-gastrointestinal; SOB, shortness of breath.
Each of the studies was reviewed by the first and last author to answer the pre-specified objectives of this review that were created after reviewing three papers that identified unanswered questions in symptom clusters research (Molassiotis et al., 2010; Skerman, Yates, & Battistutta, 2009; Skerman et al., 2012a). If discrepancies occurred during these reviews, they were discussed and a consensus was reached.
From a methodological perspective, the following criteria were evaluated: study design, sample size, and patient characteristics. To describe the nature of the symptom clusters, the following criteria were evaluated: timing of the symptom assessment; symptom assessment instrument used; number of symptoms included in the instrument; statistical analysis method used to create the symptom clusters; symptom dimension used to create the symptom clusters; number of symptom clusters identified; specific symptoms within each cluster; and changes in symptom clusters over time. The final objective of this review was to evaluate the strengths and limitations of each of the studies.
RESULTS
Cross-sectional studies with heterogeneous samples
As shown in Table 1, five cross-sectional studies evaluated for symptom clusters in samples of patients with heterogeneous cancer diagnoses (M. L. Chen & Lin, 2007; M. L. Chen & Tseng, 2006; Karabulut et al., 2010; Yamagishi et al., 2009; Yates et al., 2015). The sample sizes ranged from 151 (M. L. Chen & Tseng, 2006) to 462 (Yamagishi et al., 2009). Across these studies, the majority of the patients were female (i.e., weighted grand mean of 51.9%). Ages ranged from 18 to 97 with a weighted grand mean of 60.3 years. Of the three studies that included setting, two recruited patients primarily from an outpatient setting (M. L. Chen & Lin, 2007; Yates et al., 2015). Across these five studies, CTX was the most prevalent treatment modality used.
Three of the five studies used the MDASI to assess symptoms (M. L. Chen & Lin, 2007; M. L. Chen & Tseng, 2006; Karabulut et al., 2010). Of these three studies, one used a modified version of MDASI (M. L. Chen & Lin, 2007). Only one of these three studies used the Depression Subscale of Hospital Anxiety and Depression Scale (HADS-D) in conjunction with the MDASI (M. L. Chen & Tseng, 2006). The fourth study developed a population specific instrument using eight items from the MDASI and several additional items (Yamagishi et al., 2009). The fifth study used the Memorial Symptom Assessment Scale (MSAS) to assess the symptoms (Yates et al., 2015). The statistical methods used to identify the symptom clusters varied across the five studies. Two studies used cluster analysis (Karabulut et al., 2010; Yamagishi et al., 2009); two studies used exploratory factor analysis (EFA) (M. L. Chen & Tseng, 2006; Yates et al., 2015); and the other study used confirmatory factor analysis (CFA) (M. L. Chen & Lin, 2007).
In two studies (M. L. Chen & Lin, 2007; M. L. Chen & Tseng, 2006), severity was the dimension used to create the symptom clusters. One study did not specify the symptom dimension used (Yamagishi et al., 2009) and the fourth study used occurrence as the dimension to create the symptom clusters (Yates et al., 2015). The fifth study used severity and interference to identify the clusters (Karabulut et al., 2010).
Three of the five studies identified three symptom clusters (M. L. Chen & Lin, 2007; M. L. Chen & Tseng, 2006; Karabulut et al., 2010). One study identified four symptom clusters (Yamagishi et al., 2009). In the study that evaluated for differences in older versus younger oncology patients (Yates et al., 2015), seven symptom clusters were identified for both age groups. However, between the two age groups, the symptom clusters were not identical.
In terms of the types of symptom clusters, in the two studies conducted by Chen and colleagues (M. L. Chen & Lin, 2007; M. L. Chen & Tseng, 2006), the same symptom clusters and the same symptoms within each cluster were identified. In the study by Karabulut and colleagues (Karabulut et al., 2010), the clusters were identified only as “cluster 1, cluster 2, and cluster 3.” In the study that identified four symptom clusters (Yamagishi et al., 2009), the clusters were named: “cluster 1, cluster 2, cluster 3, and cluster 4.” In the study that evaluated for age differences in symptom clusters (Yates et al., 2015), four of the seven symptom clusters (i.e., mood-cognitive, malaise, genitourinary (GU), CTX toxicity) were given the same names and the symptoms within each cluster were relatively similar. The three unique symptom clusters in the younger age group (i.e., <60 years of age) were: treatment-related, treatment-related GI, and hormonal. The three unique symptom clusters in the older age group (i.e., ≥60 years of age) were: aerodigestive, nutrition, and age-related. Across the five cross-sectional studies with heterogeneous samples, the most common symptom clusters were: the GI symptom cluster and the mood or emotional symptom cluster.
Cross-sectional studies with homogeneous samples
As shown in Table 2, six cross-sectional studies evaluated for symptom clusters in samples of patients with homogeneous cancer diagnoses (Gift et al., 2004; Hwang et al., 2016; Ryu et al., 2010; Suwisith et al., 2008; D. Wang & Fu, 2014; S. Y. Wang et al., 2008). Three studies evaluated patients with lung cancer (Gift et al., 2004; D. Wang & Fu, 2014; S. Y. Wang et al., 2008), one study evaluated patients with breast cancer (Suwisith et al., 2008), another study evaluated patients with ovarian cancer (Hwang et al., 2016), and the sixth study evaluated patients with hepatocellular carcinoma (Ryu et al., 2010). The sample sizes ranged from 108 (S. Y. Wang et al., 2008) to 320 (Suwisith et al., 2008) and women accounted for more than half of the participants (i.e., weighted grand mean of 60.4%). For the five studies that reported an age range (Gift et al., 2004; Hwang et al., 2016; Suwisith et al., 2008; D. Wang & Fu, 2014; S. Y. Wang et al., 2008), ages ranged from 18 to 90 years with a weighted grand mean of 56.8 years. The majority of the patients were recruited from outpatient settings. Of the five studies that specified various treatment modalities (Gift et al., 2004; Hwang et al., 2016; Suwisith et al., 2008; D. Wang & Fu, 2014; S. Y. Wang et al., 2008), CTX was the most common treatment.
In the four studies that reported the timing of the symptom assessments (Gift et al., 2004; Hwang et al., 2016; Ryu et al., 2010; Suwisith et al., 2008), patients reported symptoms from the time period following surgery (Hwang et al., 2016) up to ≥5 years after their cancer diagnoses (Ryu et al., 2010). While one study used five different instruments to assess symptoms (Ryu et al., 2010), the other five studies (Gift et al., 2004; Hwang et al., 2016; Suwisith et al., 2008; D. Wang & Fu, 2014; S. Y. Wang et al., 2008) used from one to four instruments. All six studies used some type of factor analysis to identify the symptom clusters. In addition, one study used CFA and hierarchical cluster analysis (HCA) in conjunction with EFA (S. Y. Wang et al., 2008); one study used ANOVA and the Scheffe test in conjunction with EFA (Hwang et al., 2016); and another study used multiple regression in conjunction with EFA (Suwisith et al., 2008).
Across all six studies (Gift et al., 2004; Hwang et al., 2016; Ryu et al., 2010; Suwisith et al., 2008; D. Wang & Fu, 2014; S. Y. Wang et al., 2008), symptom severity was the dimension used to create the symptom clusters. However, one study used symptom occurrence in addition to severity to create the symptom clusters (Gift et al., 2004) and another study used symptom distress in addition to severity to create the symptom clusters (Suwisith et al., 2008).
While only one of these six studies identified seven symptom clusters (Hwang et al., 2016), one identified a single symptom cluster (Gift et al., 2004), one identified two symptom clusters (S. Y. Wang et al., 2008), one identified three symptom clusters (D. Wang & Fu, 2014), and two identified four symptom clusters (Ryu et al., 2010; Suwisith et al., 2008). Of note, a GI cluster was the only symptom cluster that was common among four of the studies (Ryu et al., 2010; Suwisith et al., 2008; D. Wang & Fu, 2014; S. Y. Wang et al., 2008). However, the symptoms within the GI cluster were not consistent across the four studies nor were the number of symptoms identified within this GI cluster consistent. In two of the studies (D. Wang & Fu, 2014; S. Y. Wang et al., 2008), nausea and vomiting were the only common symptoms in the GI symptom cluster
Longitudinal studies with heterogeneous samples
As shown in Table 3, three longitudinal studies evaluated for changes in symptom clusters in samples of patients with heterogeneous cancer diagnoses (Molassiotis et al., 2010; Skerman et al., 2012a; Thomas et al., 2014). The sample sizes ranged from 143 (Molassiotis et al., 2010) to 877 (Thomas et al., 2014). The gender distribution of women was 45.9% (i.e., weighted grand mean). Ages ranged from 18 to 93 with a weighted grand mean of 58.9 years. All three of these studies recruited patients from outpatient settings. Across these three studies, CTX was the most prevalent treatment modality used. Among the cancer diagnoses, lung (21.7%) and GI (23.3%) cancers were the most common in one study (Molassiotis et al., 2010) and GI (21.5%) and breast (28.8%) cancers in the other study (Skerman et al., 2012a). In the third study (Thomas et al., 2014), prostate (20.0%) and GI ( 26.2%) cancers were the most common diagnoses. Timing of the longitudinal symptom assessments occurred at peri-diagnosis and at three, six, and 12 months in one study (Molassiotis et al., 2010); at time of diagnosis, three, six, and 12 months in another study (Thomas et al., 2014); and at one, six, and 12 months after the initiation of CTX in the other study (Skerman et al., 2012a).
One study used the MSAS (32 items) to evaluate symptoms (Molassiotis et al., 2010), one study used the Rotterdam Symptom Checklist (RSC) (42 items - clinician modified) to evaluate symptoms (Skerman et al., 2012a), and the third study used the Fatigue Thermometer, Pain Thermometer, Psychosocial Screen for Cancer, Sleep Problems (i.e., from the Canadian Problem Checklist), Nutrition checklist, and the Distress Thermometer to evaluate symptoms (Thomas et al., 2014). Common factor analysis (Skerman et al., 2012a), EFA (Molassiotis et al., 2010; Thomas et al., 2014), and panel regression (Thomas et al., 2014) were used to identify the symptom clusters.
To create the symptom clusters, while one study did not specify the dimension used (Molassiotis et al., 2010), symptom distress was used in one study (Skerman et al., 2012a) and symptom severity in the other study (Thomas et al., 2014). In terms of the number of symptom clusters identified, one found three clusters (Thomas et al., 2014), one found five clusters (Skerman et al., 2012a), and one found six clusters (Molassiotis et al., 2010). A GI cluster was common in two of the studies (Molassiotis et al., 2010; Skerman et al., 2012a) and a nutrition cluster was common in two of the studies (Molassiotis et al., 2010; Thomas et al., 2014). The number of symptoms identified within each symptom cluster was higher in the study with the five symptom clusters. In all three of these studies, the symptom clusters identified remained relatively consistent over time.
Longitudinal studies of homogeneous samples
As shown in Table 4, five longitudinal studies evaluated for changes in symptom clusters in samples of patients with homogeneous cancer diagnoses (J. K. Brown et al., 2011; Gift et al., 2003; Huang et al., 2016; Kim et al., 2008; Phligbua et al., 2013). The sample sizes ranged from 111 (Huang et al., 2016) to 282 (Kim et al., 2008). Across these studies, the majority of the patients were female (weighted grand mean of 92.8%). Ages ranged from 19 (Huang et al., 2016) to 89 (J. K. Brown et al., 2011) with a weighted grand mean of 59.0 years. All patients were recruited in outpatient settings. Radiation therapy was the primary treatment modality in two of the studies (Gift et al., 2003; Kim et al., 2008) and one study evaluated patients whose primary treatment modality was surgery (J. K. Brown et al., 2011). CTX was the primary treatment modality in two studies (Huang et al., 2016; Phligbua et al., 2013). Two studies evaluated patients with lung cancer (J. K. Brown et al., 2011; Gift et al., 2003), two evaluated women with breast cancer (Kim et al., 2008; Phligbua et al., 2013), and one evaluated patients with ovarian cancer (Huang et al., 2016). The timing of the symptom assessments ranged from two (i.e., the previous day and past four weeks in one study) (J. K. Brown et al., 2011) to four (i.e., before surgery, after first cycle, after third cycle, after sixth cycle CTX) (Huang et al., 2016) time points.
Nine different symptom assessment instruments were used to assess symptoms across these studies. One study used the Lung Cancer Symptom Scale (LCSS) (J. K. Brown et al., 2011) and another study used the Physical Symptom Experience Tool (PSE) (Gift et al., 2003). The third study used four instruments (i.e., General Fatigue Scale (GFS), Profile of Mood States-Short Form (PMS-SF), Pittsburgh Sleep Quality Index (PSQI), Side Effect Checklist (SEC)) (Kim et al., 2008). The fourth study used the Chinese version of the MSAS (Huang et al., 2016). The fifth study used a modified version of the MSAS with 39 symptoms (Phligbua et al., 2013). The statistical methods used to identify the symptom clusters varied across the five studies. Four of the studies used factor analysis (Gift et al., 2003; Huang et al., 2016; Kim et al., 2008; Phligbua et al., 2013) and one study (J. K. Brown et al., 2011) uniquely coded symptoms on the LCSS to analyze and to determine patterns of co-occurring symptoms.
Symptom occurrence (J. K. Brown et al., 2011; Gift et al., 2003), symptom severity (Huang et al., 2016; Kim et al., 2008), and symptom distress (Phligbua et al., 2013) were the dimensions used to create the symptom clusters. Two studies identified one un-named symptom cluster at the two (J. K. Brown et al., 2011) and three (Gift et al., 2003) time points that were assessed. A third study identified a psychoneurological and an upper GI symptom cluster at all three of the assesssments (Kim et al., 2008). In a fourth study that assessed for symptom clusters at four time points (Huang et al., 2016), three symptom clusters were identified at Time 1 (T1), five symptom clusters at T2, six symptom clusters at T3, and six symptom clusters at T4. In the fifth study that assessed for symptom clusters at three time points (Phligbua et al., 2013), five symptom clusters were identified at T1, five symptom clusters at T2, and five symptom clusters at T3. In two of the studies that evaluated patients with breast (Phligbua et al., 2013) and ovarian (Huang et al., 2016) cancer, the following symptom clusters were found in both studies: GI, psychological, and menopausal.
In the two studies with an un-named symptom cluster, that both assessed patients with lung cancer (J. K. Brown et al., 2011; Gift et al., 2003), fatigue and poor appetite were the two symptoms that were consistent within this symptom cluster in both studies. In terms of changes in symptom clusters over time, one study found that a single, un-named symptom cluster remained stable over time (Gift et al., 2003). In the studies that identified two to six symptom clusters across the time points assessed (Huang et al., 2016; Kim et al., 2008; Phligbua et al., 2013), only one identified a psychoneurological symptom cluster that was present at all three time points (Kim et al., 2008). In another study that found four to six symptom clusters across four time points (Huang et al., 2016), the following three symptom clusters were relatively consistent over time: pain-related, psychological, and menopausal. In the fifth study that identified five symptom clusters, at each of the three time points assessed (Phligbua et al., 2013), the only symptom cluster that was consistent over time was labeled discomfort.
DISCUSSION
In this review, various aspects of symptom cluster research were evaluated in studies that included, as part of their sample, oncology patients who received primary or adjuvant CTX. Of note, across the nineteen studies included in this review, only seven studies (36.8%) (Huang et al., 2016; Hwang et al., 2016; Phligbua et al., 2013; Skerman et al., 2012a; Suwisith et al., 2008; D. Wang & Fu, 2014; Yamagishi et al., 2009) included patients who received only CTX. The remaining studies included patients undergoing a variety of cancer treatments. Given this limitation, it is difficult to determine which symptom clusters are associated with a specific cancer treatment. In addition, because only 42.1% of the studies were longitudinal and included patients with both heterogeneous (Molassiotis et al., 2010; Skerman et al., 2012a; Thomas et al., 2014) and homogeneous (J. K. Brown et al., 2011; Gift et al., 2003; Huang et al., 2016; Kim et al., 2008; Phligbua et al., 2013) cancer diagnoses, definitive conclusions cannot be made about how symptom clusters change over time. However, based on the pre-specified objectives for this review, some interesting trends were identified.
Symptom assessment instruments
The MDASI was used in 26.3% of the studies. The MDASI evaluates the severity of 13 common symptoms reported by oncology patients (i.e., pain, fatigue, nausea, sleep disturbance, distress, shortness of breath, problems remembering, lack of appetite, drowsiness, dry mouth, sadness, vomiting, numbness)(Cleeland et al., 2000). However, the MDASI only evaluates the severity of these thirteen symptoms. The MSAS was used in 26.3% of the studies. The original version of the MSAS evaluates 32 symptoms commonly reported by oncology patients (Portenoy, Thaler, Kornblith, Lepore, Friedlander-Klar, et al., 1994; Portenoy, Thaler, Kornblith, Lepore, Friedlanderklar, et al., 1994). Of note, the MSAS evaluates multiple dimensions of the symptom experience (i.e., occurrence, frequency, severity, distress). Both instruments are valid and reliable and are widely used to investigate symptoms in oncology patients (Cleeland et al., 2000) (Portenoy, Thaler, Kornblith, Lepore, Friedlander-Klar, et al., 1994; Portenoy, Thaler, Kornblith, Lepore, Friedlanderklar, et al., 1994).
Of the five studies that used the MDASI (M. L. Chen & Lin, 2007; M. L. Chen & Tseng, 2006; Karabulut et al., 2010; D. Wang & Fu, 2014; S. Y. Wang et al., 2008), one study identified two symptom clusters (S. Y. Wang et al., 2008) and four studies identified three symptom clusters (M. L. Chen & Lin, 2007; M. L. Chen & Tseng, 2006; Karabulut et al., 2010; D. Wang & Fu, 2014). The only symptom cluster that was common across four of these studies was labeled a GI symptom cluster that included the symptoms of nausea and vomiting.
While all of the symptoms in the cluster were not completely identical, a “sickness behavior” symptom cluster was identified in all five of the studies that used the MDASI (M. L. Chen & Lin, 2007; M. L. Chen & Tseng, 2006; Karabulut et al., 2010; D. Wang & Fu, 2014; S. Y. Wang et al., 2008). The identification of this sickness behavior symptom cluster is consistent with a number of reviews that suggest that inflammatory responses associated with cancer and its treatment contribute to the development and severity of symptoms in oncology patients (Cleeland et al., 2003; Miaskowski & Aouizerat, 2007). Of note, an emotional symptom cluster, that included sadness, was identified in three of the studies that used the MDASI (M. L. Chen & Lin, 2007; M. L. Chen & Tseng, 2006; D. Wang & Fu, 2014).
Of the five studies that used the MSAS (Huang et al., 2016; Molassiotis et al., 2010; Phligbua et al., 2013; Suwisith et al., 2008; Yates et al., 2015), one study identified four symptom clusters (Suwisith et al., 2008), another identified five clusters (Phligbua et al., 2013), another identified six clusters (Molassiotis et al., 2010), another identified seven clusters (Yates et al., 2015), and one identified from three to six clusters (Huang et al., 2016). Across all five studies that used the MSAS, a GI symptom cluster was identified. In addition, in all five of these studies, an “emotional” or “mood cognitive” cluster was identified. Finally, in four of the five studies (Huang et al., 2016; Molassiotis et al., 2010; Phligbua et al., 2013; Suwisith et al., 2008), a body image symptom cluster was identified. It should be noted that the specific symptoms within the GI, emotional, and body image clusters were not consistent across the five MSAS studies.
For both the MDASI (M. L. Chen & Lin, 2007; M. L. Chen & Tseng, 2006; Karabulut et al., 2010; D. Wang & Fu, 2014; S. Y. Wang et al., 2008) and the MSAS (Huang et al., 2016; Molassiotis et al., 2010; Phligbua et al., 2013; Suwisith et al., 2008; Yates et al., 2015) studies, the inconsistencies in the number and types of symptom clusters identified as well as the specific symptoms within each cluster may be related to variations in cancer diagnoses and treatments, as well as the timing of the symptom assessments within the context of cancer treatment. For the MSAS studies, the dimension of the symptom experience that was used to create the symptom clusters (i.e., occurrence, severity, distress) may have contributed to the variability in the number and types of symptom clusters identified.
However, the consistent findings across the studies that used the MDASI or the MSAS suggest that substantial progress could be made in symptom cluster research if investigators used a single (e.g., MDASI) or multidimensional (e.g., MSAS) symptom assessment instrument on a more consistent basis. Of note, the identification of a GI symptom cluster and a psychological symptom cluster using both the MDASI and the MSAS suggests that these two symptom clusters warrant additional investigation.
Statistical approaches
While a debate exists on the most appropriate statistical approach to use to identify symptom clusters (Skerman et al., 2009; Skerman, Yates, & Battistutta, 2012b), 72.7% of the cross-sectional studies and 87.5% of the longitudinal studies used some type of factor analysis to create the symptom clusters. However, the specific type of factor analysis (i.e., EFA, CFA) varied across these studies.
A growing body of literature (Miaskowski et al., 2007; Miaskowski et al., 2017; Skerman et al., 2012b) suggests that factor analysis may be the best analytical method to create symptom clusters. One reason for using factor analysis is that this analytical method assesses all data and any missing data does not influence the extraction of specific factors (Skerman et al., 2012b). Additionally, using factor analysis to extract symptom clusters allows for individual symptoms to load on more than one factor. While in test construction, a single item cannot load on more than one factor; it is possible that a single symptom may load on multiple factors (i.e., multiple symptom clusters). This hypothesis is supported by the fact that in several studies included in this review (M. L. Chen & Tseng, 2006; Karabulut et al., 2010; S. Y. Wang et al., 2008), pain and fatigue loaded on more than one factor (i.e., symptom cluster).
According to Skerman and colleagues (Skerman et al., 2012b), once the factor analysis is completed, clinicians need to determine whether the symptoms that load on a particular factor make sense as a “symptom cluster”. They suggested that one reason a symptom may load on more than one symptom cluster is that this symptom contributes to the causal mechanisms underlying each specific symptom cluster. Additional research is warranted to determine the most common symptoms that load on multiple symptom clusters. This level of analysis may provide insights into which symptom clusters share common versus unique underlying mechanisms.
Symptom dimensions
Seventeen of the 19 studies reported the symptom dimension that was used to create the symptom cluster. Across these 17 studies, 47.1% used symptom severity (M. L. Chen & Lin, 2007; M. L. Chen & Tseng, 2006; Huang et al., 2016; Kim et al., 2008; Ryu et al., 2010; Thomas et al., 2014; D. Wang & Fu, 2014; S. Y. Wang et al., 2008), 17.6% used symptom occurrence (J. K. Brown et al., 2011; Gift et al., 2003; Yates et al., 2015), 11.8% used symptom distress (Phligbua et al., 2013; Skerman et al., 2012a), and 5.9% used either severity and interference (Karabulut et al., 2010), occurrence and severity (Gift et al., 2004), or severity and distress (Suwisith et al., 2008) to create the symptom clusters. Of the nine studies that used the severity dimension of the symptom experience to create the symptom clusters, one used the MSAS (Huang et al., 2016), three used the MDASI (M. L. Chen & Lin, 2007; M. L. Chen & Tseng, 2006; S. Y. Wang et al., 2008), and five used a combination of instruments (J. C. Brown et al., 2014; Kim et al., 2008; Ryu et al., 2010; Thomas et al., 2014; D. Wang & Fu, 2014) to create the symptom clusters.
Only one study out of the nineteen included in this review evaluated for differences in symptom clusters based on the dimension of the symptom evaluated (Suwisith et al., 2008). In this study, four symptom clusters (i.e., emotions-related, GI and fatigue-related, image-related/cutaneous, pain related discomfort) were identified using severity ratings. Using distress ratings, three symptom clusters were identified (i.e., emotions and pain-related discomfort, GI symptoms, image-related/cutaneous).
Given the extreme variability in the dimensions used to create the symptom clusters, additional research is warranted that compares the number and types of symptom clusters that are created when occurrence, severity, frequency, and/or distress are used in the same set of analyses. This evaluation needs to be done using a valid and reliable instrument like the MSAS and in samples of patients who are relatively homogenous in terms of their cancer diagnoses, cancer treatments, and/or stage of disease (e.g., curative, palliative, survivor).
Number and types of symptom clusters
Across the 19 studies, the number of symptom clusters identified ranged from one to seven. Both cluster analysis and factor analysis approaches yielded approximately the same number of symptom clusters. However, the number and specific symptoms within each symptom cluster were highly variable.
The “GI” symptom cluster (M. L. Chen & Lin, 2007; M. L. Chen & Tseng, 2006; Huang et al., 2016; Kim et al., 2008; Molassiotis et al., 2010; Phligbua et al., 2013; Ryu et al., 2010; Skerman et al., 2012a; Suwisith et al., 2008; D. Wang & Fu, 2014; S. Y. Wang et al., 2008; Yates et al., 2015) or an un-named symptom cluster that contained GI symptoms (Karabulut et al., 2010; Yamagishi et al., 2009) was the most common symptom cluster identified in thirteen of the nineteen studies included in this review. However, the specific symptoms and number of symptoms found within the GI symptom cluster varied considerably. Across these thirteen studies, the symptoms of nausea and vomiting were found in ten of the studies that identified a GI symptom cluster.
The second most common symptom cluster identified was a “psychological” symptom cluster. While this symptom cluster was identified in twelve studies (M. L. Chen & Lin, 2007; M. L. Chen & Tseng, 2006; Huang et al., 2016; Hwang et al., 2016; Kim et al., 2008; Molassiotis et al., 2010; Phligbua et al., 2013; Suwisith et al., 2008; Thomas et al., 2014; D. Wang & Fu, 2014; Yamagishi et al., 2009; Yates et al., 2015), it had a variety of labels including: emotional symptoms, mood/cognitive, psychological distress, psychological, and psycho-neurological. Across these twelve studies, the common symptoms in the “psychological” symptom cluster were: feeling sad, worry, depression, and anxiety.
The third most common symptom cluster identified was a “sickness behavior” symptom cluster. This symptom cluster was named “sickness symptoms” in two studies by the same researchers (M. L. Chen & Lin, 2007; M. L. Chen & Tseng, 2006), was named “general symptoms” in another study (S. Y. Wang et al., 2008), was referred to as “malaise” in another study (Yates et al., 2015), was labeled fatigue-related in another study, and was un-named in another study (Karabulut et al., 2010). Across these five studies the common symptoms in the “sickness behavior” symptom cluster were: pain, fatigue, disturbed sleep, drowsiness, and lack of appetite.
The variability in the number and types of symptom clusters may relate to the diversity of the patients included in these studies based on their cancer diagnoses and types of treatments; the diversity in the symptom assessment instruments used, as well as in the methods used to create the symptom clusters. Of note, across these nineteen studies, neither the use of instruments with a larger number of items nor the use of multiple instruments to evaluate symptom clusters yielded a larger number of symptom clusters.
Changes in symptom clusters over time
Of the nineteen studies evaluated in this review, 42.1% were longitudinal (J. K. Brown et al., 2011; Gift et al., 2003; Huang et al., 2016; Kim et al., 2008; Molassiotis et al., 2010; Phligbua et al., 2013; Skerman et al., 2012a; Thomas et al., 2014). The timing of the assessments ranged from the previous day to the past 4 weeks (two assessments) (J. K. Brown et al., 2011), to around the time of diagnosis to a maximum of 12 months after diagnosis (i.e., four time points) (Huang et al., 2016; Molassiotis et al., 2010; Thomas et al., 2014). Across these eight longitudinal studies, only 37.5% found that the symptom clusters were relatively stable over time (Gift et al., 2003; Molassiotis et al., 2010; Thomas et al., 2014).
Limitations of this review of the literature
While a comprehensive review of the literature was done, some studies may have been missed due to the various search terms used for cancer symptom clusters research. In addition, the timing of the last search of the literature for cancer symptom clusters may have not captured the final studies published in 2016. Of note, the findings from this review may not generalize to pediatric oncology patients and to oncology patients who are receiving palliative or hospice care.
Areas for future research
To date, many questions about symptom clusters research in oncology patients remain unanswered. These research questions, which are organized, based on the themes and findings from this review are summarized in Table 5. Answering these questions will advance our understanding of symptom clusters, as well as the role that symptom clusters play in the symptom experience of oncology patients receiving CTX. In addition, information on common symptom clusters may lead to the development and the testing of novel symptom management interventions for oncology patients. Given that findings from initial studies suggest that symptom clusters occur in patients with other chronic medical conditions (Amro et al., 2016; Amro, Waldum, Dammen, Miaskowski, & Os, 2014; Burgel et al., 2010; Song, Moser, Rayens, & Lennie, 2010), the questions raided in this review warrant consideration in future studies. An important area for research is whether common symptom clusters exist across chronic conditions and which symptom clusters are unique to chronic conditions like diabetes, heart failure, chronic renal disease, and chronic obstructive pulmonary disease.
Table 5.
Questions That May Be Useful to Guide Future Cancer Symptom Clusters Research
Assessment of Symptom Clusters
|
Specificity of Symptom Clusters by Patient Characteristics, Cancer Diagnosis and Treatments
|
Changes in Symptom Clusters Over Time
|
What does this paper contribute to the wider global clinical community?
Given the international interest in symptom clusters research in oncology patients, the findings from this review clearly identify gaps in our knowledge and directions for future research
Across the studies in this review a gastrointestinal and a psychological symptom cluster were identified consistently and warrant evaluation in oncology patients.
The information provided in this review can be used by nurse scientists to design studies that evaluate symptom clusters in oncology patients.
Acknowledgments
This study was funded by a grant from the National Cancer Institute (NCI, CA134900). Dr. Christine Miaskowski is an American Cancer Society Clinical Research Professor and is funded by a K07 award from the NCI (CA168960). Ms. Ward-Sullivan was funded by a National Institute of Health (NIH) T32 grant (3T32NR007088).
Footnotes
Conflicts of interest: The authors have no conflicts of interest to declare.
References
- Amro A, Waldum-Grevbo B, von der Lippe N, Brekke FB, Miaskowski C, Os I. Symptom clusters from dialysis to renal transplantation: A five-year longitudinal study. Journal of Pain and Symptom Management. 2016;51(3):512–519. doi: 10.1016/j.jpainsymman.2015.10.012. [DOI] [PubMed] [Google Scholar]
- Amro A, Waldum B, Dammen T, Miaskowski C, Os I. Symptom clusters in patients on dialysis and their association with quality-of-life outcomes. Journal of Renal Care. 2014;40(1):23–33. doi: 10.1111/jorc.12051. [DOI] [PubMed] [Google Scholar]
- Bender CM, Ergyn FS, Rosenzweig MQ, Cohen SM, Sereika SM. Symptom clusters in breast cancer across 3 phases of the disease. Cancer Nursing. 2005;28(3):219–225. doi: 10.1097/00002820-200505000-00011. 00002820-200505000-00011. [DOI] [PubMed] [Google Scholar]
- Brown JC, Mao JJ, Stricker C, Hwang WT, Tan KS, Schmitz KH. Aromatase inhibitor associated musculoskeletal symptoms are associated with reduced physical activity among breast cancer survivors. Breast Journal. 2014;20(1):22–28. doi: 10.1111/tbj.12202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown JK, Cooley ME, Chernecky C, Sarna L. A symptom cluster and sentinel symptom experienced by women with lung cancer. Oncology Nursing Forum. 2011;38(6):E425–435. doi: 10.1188/11.ONF.E425-E435. [DOI] [PubMed] [Google Scholar]
- Burgel PR, Paillasseur JL, Caillaud D, Tillie-Leblond I, Chanez P, Escamilla R … Initiatives, B. S. C. Clinical COPD phenotypes: a novel approach using principal component and cluster analyses. European Respiratory Journal. 2010;36(3):531–539. doi: 10.1183/09031936.00175109. 09031936.00175109. [DOI] [PubMed] [Google Scholar]
- Chen E, Nguyen J, Cramarossa G, Khan L, Leung A, Lutz S, Chow E. Symptom clusters in patients with lung cancer: a literature review. Expert Revies in Pharmacoeconomics Outcomes Research. 2011;11(4):433–439. doi: 10.1586/erp.11.56. [DOI] [PubMed] [Google Scholar]
- Chen ML, Lin CC. Cancer symptom clusters: a validation study. Journal of Pain and Symptom Management. 2007;34(6):590–599. doi: 10.1016/j.jpainsymman.2007.01.008. [DOI] [PubMed] [Google Scholar]
- Chen ML, Tseng HC. Symptom clusters in cancer patients. Supportive Care in Cancer. 2006;14(8):825–830. doi: 10.1007/s00520-006-0019-8. [DOI] [PubMed] [Google Scholar]
- Cleeland CS, Bennett GJ, Dantzer R, Dougherty PM, Dunn AJ, Meyers CA, … Lee BN. Are the symptoms of cancer and cancer treatment due to a shared biologic mechanism? A cytokine-immunologic model of cancer symptoms. Cancer. 2003;97(11):2919–2925. doi: 10.1002/cncr.11382. [DOI] [PubMed] [Google Scholar]
- Cleeland CS, Mendoza TR, Wang XS, Chou C, Harle MT, Morrissey M, Engstrom MC. Assessing symptom distress in cancer patients: the M.D. Anderson Symptom Inventory. Cancer. 2000;89(7):1634–1646. doi: 10.1002/1097-0142(20001001)89:7<1634. [DOI] [PubMed] [Google Scholar]
- Dodd MJ, Miaskowski C, Lee KA. Occurrence of symptom clusters. Journal of the National Cancer Institute. 2004;32:76–78. doi: 10.1093/jncimonographs/lgh0082004/32/76. [DOI] [PubMed] [Google Scholar]
- Dodd MJ, Miaskowski C, Paul SM. Symptom clusters and their effect on the functional status of patients with cancer. Oncology Nursing Forum. 2001;28(3):465–470. [PubMed] [Google Scholar]
- Dong ST, Butow PN, Costa DS, Lovell MR, Agar M. Symptom clusters in patients with advanced cancer: a systematic review of observational studies. Journal of Pain and Symptom Management. 2014;48(3):411–450. doi: 10.1016/j.jpainsymman.2013.10.027. [DOI] [PubMed] [Google Scholar]
- Fan G, Filipczak L, Chow E. Symptom clusters in cancer patients: a review of the literature. Current Oncology. 2007;14(5):173–179. doi: 10.3747/co.2007.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu OS, Crew KD, Jacobson JS, Greenlee H, Yu G, Campbell J, … Hershman DL. Ethnicity and persistent symptom burden in breast cancer survivors. Journal of Cancer Survivorship. 2009;3(4):241–250. doi: 10.1007/s11764-009-0100-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaston-Johansson F, Fall-Dickson JM, Bakos AB, Kennedy MJ. Fatigue, pain, and depression in pre-autotransplant breast cancer patients. Cancer Practice. 1999;7(5):240–247. doi: 10.1046/j.1523-5394.1999.75008.x. [DOI] [PubMed] [Google Scholar]
- Gift AG, Jablonski A, Stommel M, Given CW. Symptom clusters in elderly patients with lung cancer. Oncology Nursing Forum. 2004;31(2):202–212. doi: 10.1188/04.ONF.202-212. [DOI] [PubMed] [Google Scholar]
- Gift AG, Stommel M, Jablonski A, Given W. A cluster of symptoms over time in patients with lung cancer. Nursing Research. 2003;52(6):393–400. doi: 10.1097/00006199-200311000-00007. [DOI] [PubMed] [Google Scholar]
- Given B, Given C, Azzouz F, Stommel M. Physical functioning of elderly cancer patients prior to diagnosis and following initial treatment. Nursing Research. 2001;50(4):222–232. doi: 10.1097/00006199-200107000-00006. [DOI] [PubMed] [Google Scholar]
- Glaus A, Boehme C, Thurlimann B, Ruhstaller T, Hsu Schmitz SF, Morant R, … von Moos R. Fatigue and menopausal symptoms in women with breast cancer undergoing hormonal cancer treatment. Annals of Oncology. 2006;17(5):801–806. doi: 10.1093/annonc/mdl030. mdl030. [DOI] [PubMed] [Google Scholar]
- Huang J, Gu L, Zhang L, Lu X, Zhuang W, Yang Y. Symptom Clusters in Ovarian Cancer Patients With Chemotherapy After Surgery: A Longitudinal Survey. Cancer Nursing. 2016;39(2):106–116. doi: 10.1097/NCC.0000000000000252. [DOI] [PubMed] [Google Scholar]
- Hwang KH, Cho OH, Yoo YS. Symptom clusters of ovarian cancer patients undergoing chemotherapy, and their emotional status and quality of life. European Journal of Oncol Nursing. 2016;21:215–222. doi: 10.1016/j.ejon.2015.10.007. [DOI] [PubMed] [Google Scholar]
- Ivanova MO, Ionova TI, Kalyadina SA, Uspenskaya OS, Kishtovich AV, Guo H, … Wang XS. Cancer-related symptom assessment in Russia: validation and utility of the Russian M. D. Anderson Symptom Inventory. Journal of Pain and Symptom Management. 2005;30(5):443–453. doi: 10.1016/j.jpainsymman.2005.04.015. S0885-3924(05)00499-9. [DOI] [PubMed] [Google Scholar]
- Karabulut N, Erci B, Ozer N, Ozdemir S. Symptom clusters and experiences of patients with cancer. Journal of Advanced Nursing. 2010;66(5):1011–1021. doi: 10.1111/j.1365-2648.2009.05254.xJAN5254. [DOI] [PubMed] [Google Scholar]
- Kim HJ, Barsevick AM, Tulman L, McDermott PA. Treatment-related symptom clusters in breast cancer: a secondary analysis. Journal of Pain and Symptom Management. 2008;36(5):468–479. doi: 10.1016/j.jpainsymman.2007.11.011. [DOI] [PubMed] [Google Scholar]
- Kim HJ, McGuire DB, Tulman L, Barsevick AM. Symptom clusters: concept analysis and clinical implications for cancer nursing. Cancer Nursing. 2005;28(4):270–282. doi: 10.1097/00002820-200507000-00005. 00002820-200507000-00005. [DOI] [PubMed] [Google Scholar]
- Miaskowski C, Aouizerat BE. Is there a biological basis for the clustering of symptoms? Seminars in Oncology Nursing. 2007;23(2):99–105. doi: 10.1016/j.soncn.2007.01.008. [DOI] [PubMed] [Google Scholar]
- Miaskowski C, Aouizerat BE, Dodd M, Cooper B. Conceptual issues in symptom clusters research and their implications for quality-of-life assessment in patients with cancer. Journal of the National Cancer Institute. 2007;37(37):39–46. doi: 10.1093/jncimonographs/lgm003. [DOI] [PubMed] [Google Scholar]
- Miaskowski C, Barsevick A, Berger A, Casagrande R, Grady PA, Jacobsen P, … Marden S. Advancing symptom science through symptom cluster research: Expert panel proceedings and recommendations. Journal of the National Cancer Institute. 2017;109(4) doi: 10.1093/jnci/djw253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molassiotis A, Wengstrom Y, Kearney N. Symptom cluster patterns during the first year after diagnosis with cancer. Journal of Pain and Symptom Management. 2010;39(5):847–858. doi: 10.1016/j.jpainsymman.2009.09.012. [DOI] [PubMed] [Google Scholar]
- Nguyen J, Cramarossa G, Bruner D, Chen E, Khan L, Leung A, … Chow E. A literature review of symptom clusters in patients with breast cancer. Expert Reviews in Pharmacoeconomic Outcomes Research. 2011;11(5):533–539. doi: 10.1586/erp.11.55. [DOI] [PubMed] [Google Scholar]
- Okuyama T, Wang XS, Akechi T, Mendoza TR, Hosaka T, Cleeland CS, Uchitomi Y. Japanese version of the MD Anderson Symptom Inventory: a validation study. Journal of Pain and Symptom Management. 2003;26(6):1093–1104. doi: 10.1016/j.jpainsymman.2003.05.003. S0885392403004196 [pii] [DOI] [PubMed] [Google Scholar]
- Phligbua W, Pongthavornkamol K, Knobf TM, Junda T, Viwatwongkasem C, Srimuninnimit V. Symptom clusters and quality of life in women with breast cancer receiving adjuvant chemotherapy. Pacific Rim International Journal of Nursing Research. 2013;17(3):249–266. [Google Scholar]
- Portenoy RK, Thaler HT, Kornblith AB, Lepore JM, Friedlander-Klar H, … Coyle N, et al. Symptom prevalence, characteristics and distress in a cancer population. Quality of Life Research. 1994;3(3):183–189. doi: 10.1007/BF00435383. [DOI] [PubMed] [Google Scholar]
- Portenoy RK, Thaler HT, Kornblith AB, Lepore JM, Friedlanderklar H, Kiyasu E, … Scher H. The Memorial Symptom Assessment Scale - an Instrument for the Evaluation of Symptom Prevalence, Characteristics and Distress. European Journal of Cancer. 1994;30a(9):1326–1336. doi: 10.1016/0959-8049(94)90182-1. [DOI] [PubMed] [Google Scholar]
- Ridner SH. Quality of life and a symptom cluster associated with breast cancer treatment-related lymphedema. Supportive Care in Cancer. 2005;13(11):904–911. doi: 10.1007/s00520-005-0810-y. [DOI] [PubMed] [Google Scholar]
- Ryu E, Kim K, Cho MS, Kwon IG, Kim HS, Fu MR. Symptom clusters and quality of life in Korean patients with hepatocellular carcinoma. Cancer Nursing. 2010;33(1):3–10. doi: 10.1097/NCC.0b013e3181b4367e. [DOI] [PubMed] [Google Scholar]
- Sarna L, Brecht ML. Dimensions of symptom distress in women with advanced lung cancer: a factor analysis. Heart and Lung. 1997;26(1):23–30. doi: 10.1016/s0147-9563(97)90006-6. S0147-9563(97)90006-6. [DOI] [PubMed] [Google Scholar]
- Skerman HM, Yates PM, Battistutta D. Multivariate methods to identify cancer-related symptom clusters. Research in Nursing and Health. 2009;32(3):345–360. doi: 10.1002/nur.20323. [DOI] [PubMed] [Google Scholar]
- Skerman HM, Yates PM, Battistutta D. Cancer-related symptom clusters for symptom management in outpatients after commencing adjuvant chemotherapy, at 6 months, and 12 months. Supportive Care in Cancer. 2012a;20(1):95–105. doi: 10.1007/s00520-010-1070-z. [DOI] [PubMed] [Google Scholar]
- Skerman HM, Yates PM, Battistutta D. Identification of cancer-related symptom clusters: an empirical comparison of exploratory factor analysis methods. Journal of Pain and Symptom Management. 2012b;44(1):10–22. doi: 10.1016/j.jpainsymman.2011.07.009S0885-3924(12)00069-3. [DOI] [PubMed] [Google Scholar]
- Song EK, Moser DK, Rayens MK, Lennie TA. Symptom clusters predict event-free survival in patients with heart failure. Journal of Cardiovascular Nursing. 2010;25(4):284–291. doi: 10.1097/JCN.0b013e3181cfbcbb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suwisith N, Hanucharururnkul S, Dodd M, Vorapongsathorn T, Pongthavorakamol K, Asavametha N. Symptom clusters and functional status of women with breast cancer. Thai Journal of Nursing Research. 2008;12(3):153–165. [Google Scholar]
- Thavarajah N, Chen E, Zeng L, Bedard G, Di Giovanni J, Lemke M, … Chow E. Symptom clusters in patients with metastatic cancer: a literature review. Expert Reviews in Pharmacoeconomics Outcomes Research. 2012;12(5):597–604. doi: 10.1586/erp.12.41. [DOI] [PubMed] [Google Scholar]
- Thomas BC, Waller A, Malhi RL, Fung T, Carlson LE, Groff SL, Bultz BD. A longitudinal analysis of symptom clusters in cancer patients and their sociodemographic predictors. Journal of Pain and Symptom Management. 2014;47(3):566–578. doi: 10.1016/j.jpainsymman.2013.04.007. [DOI] [PubMed] [Google Scholar]
- Walsh D, Rybicki L. Symptom clustering in advanced cancer. Supportive Care in Cancer. 2006;14(8):831–836. doi: 10.1007/s00520-005-0899-z. [DOI] [PubMed] [Google Scholar]
- Wang D, Fu J. Symptom clusters and quality of life in China patients with lung cancer undergoing chemotherapy. African Health Science. 2014;14(1):49–55. doi: 10.4314/ahs.v14i1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang SY, Tsai CM, Chen BC, Lin CH, Lin CC. Symptom clusters and relationships to symptom interference with daily life in Taiwanese lung cancer patients. Journal of Pain and Symptom Management. 2008;35(3):258–266. doi: 10.1016/j.jpainsymman.2007.03.017. [DOI] [PubMed] [Google Scholar]
- Wang XS, Laudico AV, Guo H, Mendoza TR, Matsuda ML, Yosuico VD, … Cleeland CS. Filipino version of the M. D. Anderson Symptom Inventory: validation and multisymptom measurement in cancer patients. Journal of Pain and Symptom Management. 2006;31(6):542–552. doi: 10.1016/j.jpainsymman.2005.11.011. S0885-3924(06)00257-0. [DOI] [PubMed] [Google Scholar]
- Wang XS, Wang Y, Guo H, Mendoza TR, Hao XS, Cleeland CS. Chinese version of the M. D. Anderson Symptom Inventory: validation and application of symptom measurement in cancer patients. Cancer. 2004;101(8):1890–1901. doi: 10.1002/cncr.20448. [DOI] [PubMed] [Google Scholar]
- Xiao C. The state of science in the study of cancer symptom clusters. European Journal of Oncology Nursing. 2010;14(5):417–434. doi: 10.1016/j.ejon.2010.05.011S1462-3889(10)00092-X. [DOI] [PubMed] [Google Scholar]
- Yamagishi A, Morita T, Miyashita M, Kimura F. Symptom prevalence and longitudinal follow-up in cancer outpatients receiving chemotherapy. Journal of Pain and Symptom Management. 2009;37(5):823–830. doi: 10.1016/j.jpainsymman.2008.04.015. [DOI] [PubMed] [Google Scholar]
- Yates P, Miaskowski C, Cataldo JK, Paul SM, Cooper BA, Alexander K, … Skerman H. Differences in composition of symptom clusters between older and younger oncology patients. Journal of Pain and Symptom Management. 2015;49(6):1025–1034. doi: 10.1016/j.jpainsymman.2014.11.296. [DOI] [PubMed] [Google Scholar]