Abstract
Alzheimer’s disease (AD) is a progressive neurodegenerative disorder leading to dementia caused by advanced neuronal dysfunction and death. The most significant symptoms of AD are observed at late stages of the disease when interventions are most likely too late to ameliorate the condition. Currently, the predominant theory for AD is the “amyloid hypothesis,” which states that abnormally increased levels of amyloid β (Aβ) peptides result in the production of a variety of aggregates that are neurotoxic. The specific mechanisms for Aβ peptide-induced cytotoxicity have not yet been completely elucidated. However, since the majority of Aβ is released into the extracellular milieu, it is reasonable to assume that toxicity begins outside the cells and makes its way inside where it disrupts the basic cellular process resulting in cell death. There is increasing evidence that hsp, particularly Hsp70, are exported into the extracellular milieu by an active export mechanism independent of cell death. Therefore, both Aβ peptides and Hsp70 may coexist in a common environment during pathological conditions. We observed that Hsp70 affected the Aβ assembling process in vitro preventing oligomer formation. Moreover, the presence of Hsp70 reduced the Aβ peptide-induced toxicity of cultured neurons (N2A cells). These results suggest a potential mechanism for the reduction of the detrimental effects of Aβ peptides in AD.
Keywords: Alzheimer’s disease, Amyloid β, Heat shock proteins, Hsp70, Neurons, Cytotoxicity
Introduction
Alzheimer’s disease (AD) is a progressive neurodegenerative disorder resulting in dementia due to advanced neuron dysfunction and death. The cost of AD treatment is a major expense for the healthcare system and is expected to rise in the future with the upsurge of the aging population (Cummings et al. 2017). In addition, the development of AD is a major emotional, social, and economic burden for the patient’s family members who provide most of the care (Crews and Masliah 2010; Lobello et al. 2012). Except for genetic forms, there are no current early predictors or diagnostics for the onset of AD. The most perceivable symptoms are observed when the patient is already in the late stages of the disease, making any treatment difficult. AD is a multifactorial condition modulated by several confounding factors, including genetics, ethnicity, sex, environment, physiology, and trauma (Crews and Masliah 2010; Lobello et al. 2012). Currently, the predominant theory for the incidence of AD is the “amyloid hypothesis,” that states that abnormal levels of amyloid β (Aβ) peptides result in the production of cytotoxic complexes (Benilova et al. 2012). Aβ peptides are produced by cleavage from the membrane-anchored amyloid β precursor protein (APP) by several proteases, but predominantly by β and γ secretases, leading mostly to Aβ peptides and fragments (Thinakaran and Koo 2008). Once in the external milieu, Aβ peptides follow a natural aggregation process resulting in a variety of oligomeric forms that act as active neurotoxins, causing neuronal dysfunction, loss of synaptic connections, and cell death. Aβ peptides are also the main precursor of amyloid plaques that are the hallmark for the postmortem diagnosis of AD (Haass and Selkoe 2007). The toxicity of Aβ complexes appears to be mediated by small oligomers rather than by the higher molecular weight aggregates, protofibrils, and fibers (Bieschke et al. 2011). Aβ peptide cytotoxicity has been associated with increases in intracellular calcium levels, production of oxygen radicals, lipid peroxidation, mitochondrial dysfunction, and inflammation (Crews and Masliah 2010; Lobello et al. 2012). In addition, Aβ peptide oligomers interact with the plasma membranes forming ion conductance pathways, called the Aβ channels (Arispe et al. 1993a, b), which appear to be responsible for cellular toxicity (Simakova and Arispe 2006). Based on these observations, it is likely that Aβ toxicity begins outside the cells and makes its way inside to disrupt basic cellular processes. Therefore, ideal therapeutic interventions should be directed at the early stages of the oligomerization process to prevent extracellular Aβ peptide-induced cytotoxicity.
There is extensive evidence suggesting that the expression of heat shock proteins (hsp) protects cells from Aβ peptide toxicity (Kirby et al. 1994; Muchowski and Wacker 2005; Brown 2007; King et al. 2009; Hoshino et al. 2011; Toth et al. 2013; Bobkova et al. 2014). Hsp include a large family of well-conserved proteins that are classified by their molecular mass. The Hsp70 family of hsp is composed of Hsp70 (HSPA1A), the major stress-inducible form, whereas other Hsp70s such as Hsc70 (HSPA8) and Grp78 (BIP, HSPA5) are constitutively expressed (Lindquist and Craig 1988; De Maio 1999; Kampinga et al. 2009). The expression of Hsp70 after heat shock in the brain is different between neurons in the cerebellum and hippocampus (Sprang and Brown 1987). Moreover, glial cells and neurons expressed different levels of Hsp70 and Hsc70 (Brown 2007; Marini et al. 1990; Chow et al. 2014). The mechanism for hsp protection from Aβ peptide toxicity has not been elucidated. Since hsp are molecular chaperones playing a key role in protein folding and solubilization of misfolded polypeptides, it has been assumed that they might modulate Aβ peptide oligomerization. However, there is a compartmental discrepancy with this assumption. Hsp are present in the cytosol and other subcellular compartments, such as ER and mitochondria, whereas the toxic forms of Aβ peptides are located outside cells. This discrepancy has been solved by evidence demonstrating that hsp could be detected outside cells (Hightower and Guidon 1989; De Maio 2011), exported by either an active mechanism or released after necrotic cell death (De Maio and Vazquez 2013; Gastpar et al. 2005). Extracellular hsp have been shown to play multiple roles, including stimulation of immune cells, activation of phagocytosis, and interaction with extracellular protein complexes, a process that has been named the stress observation system (De Maio 2011). Consequently, the export of Hsp70 could ameliorate Aβ peptide toxicity by preventing their oligomerization and/or interfering with the interaction of Aβ oligomers with cells. In this investigation, we tested this hypothesis and found that indeed Hsp70 interferes with Aβ peptide oligomerization preventing the formation of the cytotoxic complexes.
Methods
Monomerization and oligomerization of Aβ1-42 peptides
Aβ1-42 peptides were monomerized by incubation with hexafluoroisopropanol (HFIP) as previously described (Capone et al. 2009). Briefly, 5 mg of Aβ1-42 peptides (Bachem, cat# H1368) was resuspended in 1.5 mL of HFIP (Regis, cat# 270702) and gently shaken for over 20 h at room temperature. Two volumes of water (3 mL) were added and the solution was immediately aliquoted into glass vials (125 μg/vial) prestanding on a dry ice/acetone bath until fully frozen. The frozen aliquots were lyophilized for 72 h at maximum vacuum (0.021 mbar), which was terminated by exposure to dry prefiltered argon gas and stored at − 80 °C. Before use, monomerized Aβ1-42 peptides were thawed in ice and dissolved in water. The addition of water is counted as time zero since aggregation starts immediately.
Aβ42 aggregation in the presence of hsp proteins
Monomerized Aβ1-42 peptides (1 μg) were incubated in the absence or in the presence of increasing concentrations of Hsp70, Hsc70, Grp78, and Hsp40 dissolved in 4.5 mM Tris pH 7.4. Incubations were initially set on ice followed by incubations at 37 °C for 24 h, after which reactions were frozen in − 80 °C until analysis. Samples were thawed on ice and 5 μL of LDS sample buffer 4× (NuPAGE) was added, mixed, not boiled, and loaded into 4–12% Bis-Tris gradient gels (Novex, 1.5 mm × 10 wells), run at 200 V for 50–53 min in MOPS SDS running buffer. Gels were transferred to nitrocellulose membranes using Bolt transfer buffer at 30 V for 1 h. Membranes were blocked with 5% BSA dissolved in TBS-Tween 0.1% for 2 h and incubated overnight with mouse anti-Aβ mAb 4G8 (Covance) at a concentration of 1 μg/mL in 5% BSA at 4 °C with moderate shaking, rinsed 3 times with TBS-T, and incubated for 1 h at RT with anti-mouse conjugated to HRP (ThermoFisher) diluted 1:1000 and rinsed 3 times with TBS-T. Images were developed using ECL (Pierce, SuperSignal) and acquired using a BioRad detection system under linear conditions of detection. Then, blots were stripped using Re-Blot Plus Mild (Millipore) for 20 min, treated as above but incubated with 1:1000 dilutions of rabbit anti-Hsp70 (ADI-SPA-812), rat anti-Hsc70 (ADI-SPA-815), rabbit anti-Grp78 (StressMarq, SPC-180), and rabbit anti-Hsp40 (Cell Signal # 48685) and secondary antibodies (ThermoFisher #32460 and Invitrogen #619520).
Cell viability by flow cytometry
N2A neuroblastoma cells were incubated or not with Aβ1-42 peptides in DMEM medium (1% FBS) at 37 °C for 48 h. Cells were then harvested and stained with APC-conjugated annexin V and propidium iodide (PI) for flow cytometry analysis.
Results
The degree of Aβ1-42 peptide oligomerization induced different forms of cellular toxicity
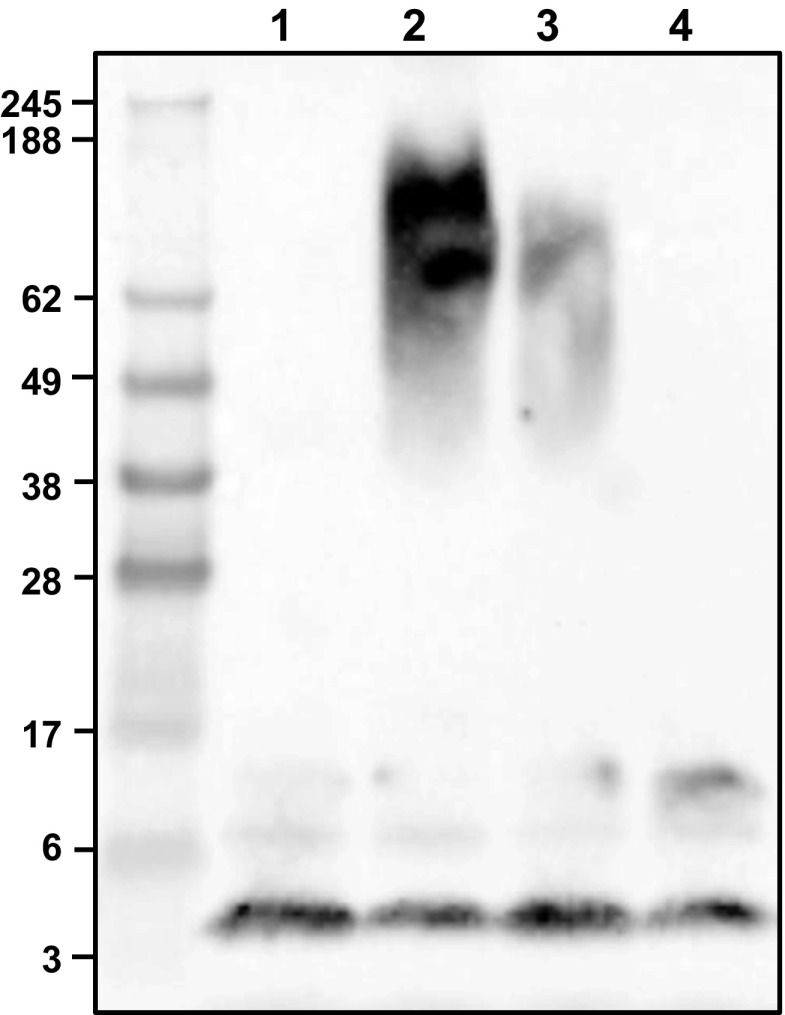
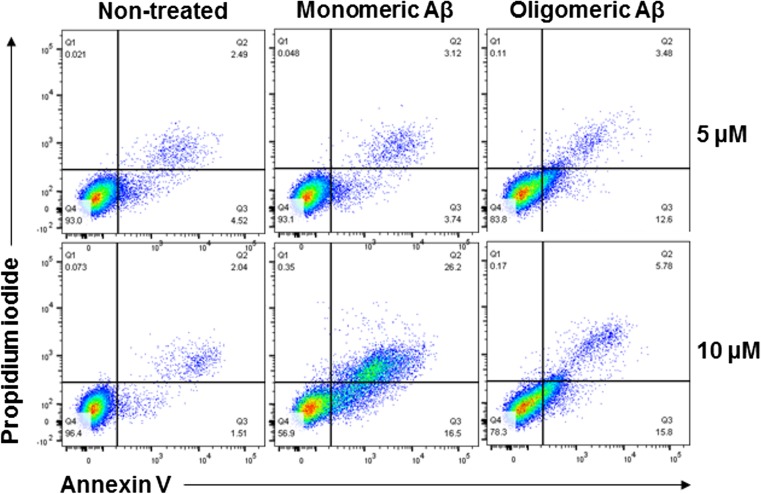
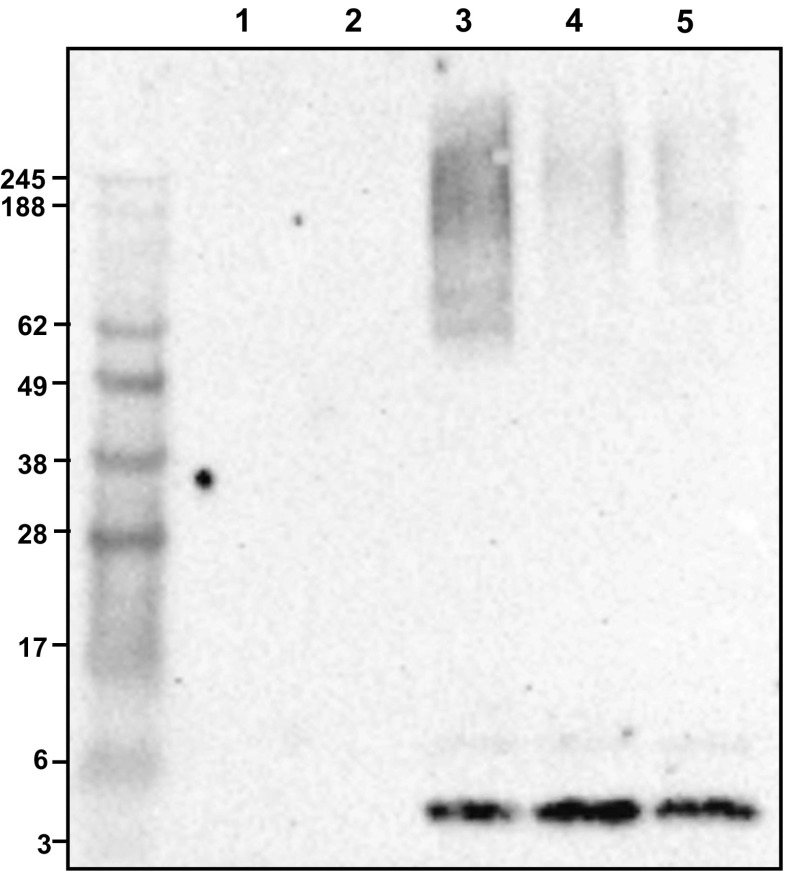
Aβ1-42 peptides were monomerized by incubation with HFIP followed by extensive lyophilization to eliminate the solvent. Then, the monomeric Aβ1-42 peptides (4.5 kDa) were incubated at 37, 25, or 4 °C for 20 h. Samples were electrophoresed and analyzed by Western blotting using Clone 4G8 antibody. HFIT treatment indeed resulted in the monomerization of Aβ1-42 peptides, as illustrated in Fig. 1 (lane 1). Incubation of the monomeric peptides at 37 °C resulted in the appearance of oligomers between 52 and 150 kDa (Fig. 1, lane 2), whereas incubation at 25 °C decreased the intensity of the oligomeric signal (Fig. 1, lane 3) and no oligomers were detected after incubation at 4 °C (Fig. 1, lane 4). N2A cells (mouse neuroblastoma) were initially incubated with Aβ1-42 peptides, in the monomeric or pre-oligomerized forms, at a concentration of 5 or 10 μM, which have been widely used in prior studies (Simakova and Arispe 2006, 2007), in DMEM medium containing 1% FBS at 37 °C for 48 h. Cell viability was monitored by staining with annexin V and PI and analyzed by flow cytometry. Cell death, as indicated by the appearance of annexin V and PI-positive signals, was more prominent at 10 μM (Fig. 2, bottom panel) than at 5 μM (Fig. 2, top panel). Exposure of cells to the initial monomeric forms, which form oligomers upon incubation with the cells, showed a higher level of cell death in comparison with cells incubated with the pre-oligomerized peptides (Fig. 2). A typical apoptotic pattern of cell death was observed after incubation with Aβ1-42 peptide monomers, as indicated by initial staining with annexin V followed by membrane permeabilization as indicated by PI uptake (Fig. 2, middle panel). In contrast, cells incubated with the pre-oligomerized peptides displayed a sharp increase in the staining of both annexin V and PI simultaneously, suggesting that cells are not dying of apoptosis, but rather by a necrotic-like process (Fig. 2, right panel).
Fig. 1.
Oligomerization of Aβ peptides at different temperatures. Monomerized Aβ1-42 peptides (1 μg) were kept as a monomer (lane 1) or were incubated at 37 °C (lane 2), 25 °C (lane 3), or 4 °C (lane 4), for 20 h in 4.5 mM Tris pH 7.4. Samples were electrophoresed, transferred onto nitrocellulose membranes, and analyzed by Western blotting using Clone 4G8 antibody followed by an HRP-conjugated secondary antibody
Fig. 2.
Aβ peptides induced cell death of N2A neuroblastoma cells. N2A cells were incubated in DMEM medium containing 1% FBS at 37 °C for 48 h in the absence or presence of two concentrations (5 and 10 μM) of monomerized or pre-oligomerized Aβ1-42 peptides. Cell death was evaluated by annexin V and propidium iodide staining and flow cytometry analysis
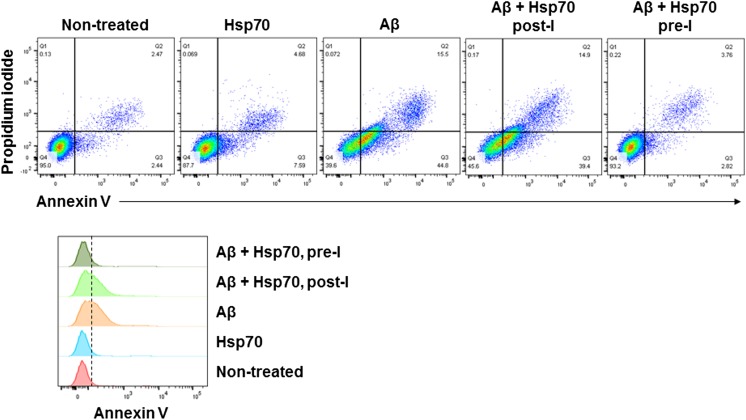
Hsp70 altered Aβ peptide oligomerization and reduced cellular toxicity
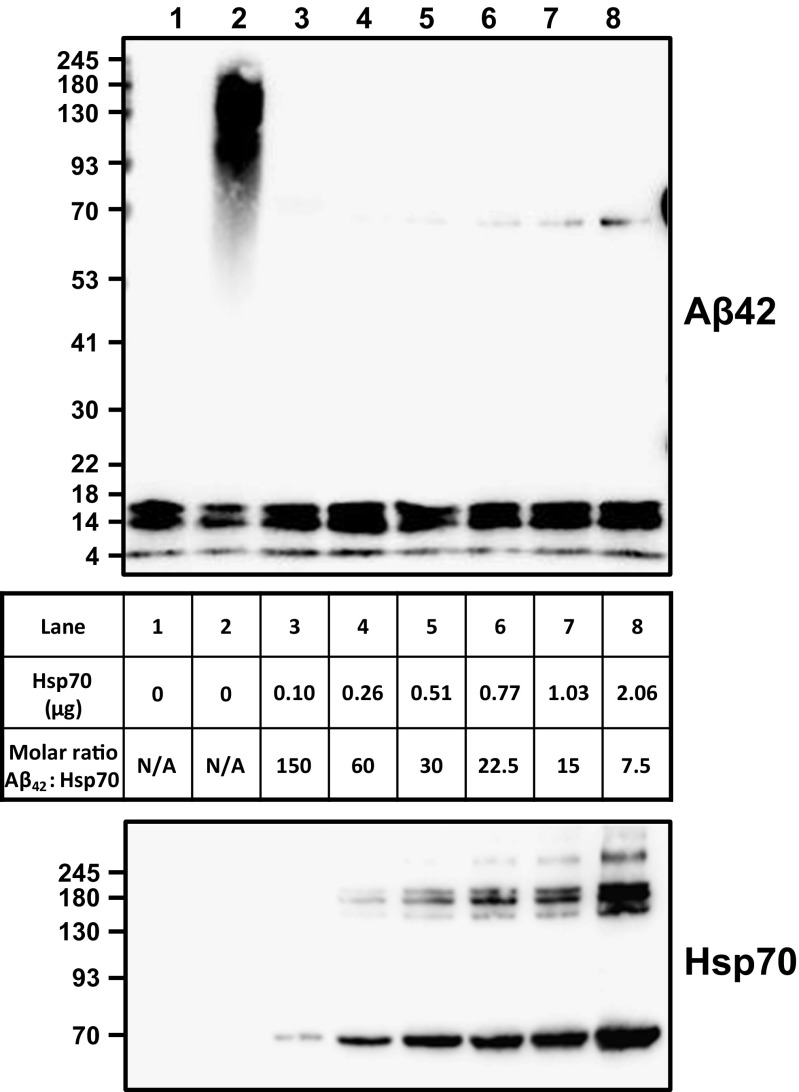
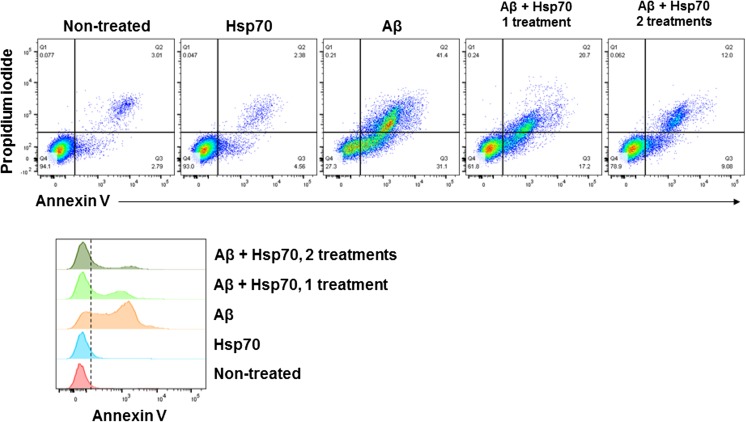
Aβ1-42 peptides in the monomeric form were incubated with increasing concentrations of Hsp70 at 37 °C for 20 h in the absence of nucleotides. As controls, Aβ1-42 peptides were maintained either as a monomer or oligomerized at 37 °C. All samples were analyzed by Western blotting. The addition of Hsp70 to Aβ monomers resulted in a reduction of the oligomerization process (Fig. 3), even when the molecular ratio between Hsp70 and Aβ1-42 peptides was 1:150. Although the addition of Hsp70 to Aβ1-42 peptides resulted in inhibition of large molecular weight complexes, it did not apparently affect the presence of dimer, trimer, and tetramer complexes (Fig. 3). Then, N2A cells were incubated with Hsp70 (0.2 μM) alone, Aβ1-42 peptide monomers (10 μM), or a combination of Aβ1-42 peptide monomers and Hsp70 (1:50 ratio) at 37 °C for 48 h. A reduction in 50% of cell mortality was observed in cells co-incubated with Aβ1-42 peptides and Hsp70 in comparison with cells incubated with Aβ1-42 peptides alone (Fig. 4). A second addition of Hsp70 (0.32 μg, 0.4 μM final) after 24 h of co-incubation with Aβ1-42 peptides and Hsp70 resulted in a further decrease of cell death (70%) as opposed to cells incubated with Aβ1-42 peptides alone (Fig. 4). No toxic effect was observed by incubation of cells with Hsp70 (0.2 μM) alone (Fig. 4). At the end of the incubation process (48 h), the extracellular medium of cells exposed to Aβ1-42 peptides and Hsp70 as described above was collected, and the presence of Aβ1-42 forms was detected by Western blotting. Oligomerization of Aβ was observed in samples collected from cells that were initially incubated with monomeric Aβ1-42 alone (Fig. 5, lane 3), indicating that the monomers formed oligomers during incubation conditions with cells at 37 °C. In contrast, the presence of Aβ1-42 oligomers was significantly reduced in medium of cells co-incubated with Aβ1-42 peptides and Hsp70 (Fig. 5, lanes 4 and 5). This observation corroborates that Hsp70 interferes with Aβ1-42 peptide oligomerization, therefore, resulting in reduced cell toxicity.
Fig. 3.
Hsp70 interferes with the oligomerization of Aβ peptides. Monomerized Aβ1-42 peptides (1 μg) were kept as a monomer (lane 1), or incubated at 37 °C for 20 h (lane 2), or were incubated with various concentrations of Hsp70 (from 0.1 to 2.06 μg) in 4.5 mM Tris pH 7.4 at 37 °C for 24 h (lanes 3–8). Samples were electrophoresed, transferred onto nitrocellulose membranes, and analyzed by Western blotting using Clone 4G8 antibody followed by an HRP-conjugated secondary antibody. Membranes were stripped and incubated with 1:1000 dilutions of rabbit anti-Hsp70 (ADI-SPA-812), followed by an HRP-conjugated secondary antibody
Fig. 4.
Hsp70 reduces Aβ peptide-induced cellular toxicity. N2A cells were incubated with Hsp70 (0.2 μM) alone, Aβ1-42 peptide monomers (10 μM), or a combination of Aβ1-42 peptide monomers and Hsp70 (10 and 0.2 μM, respectively, 1 treatment) at 37 °C for 48 h. In some experiments, a second dose of Hsp70 (0.2 μM, 2 treatments) was added after 24 h of co-incubation with Aβ1-42 peptides and Hsp70. Cell death was evaluated by annexin V and propidium iodide staining and flow cytometry analysis. Upper panels show representative annexin V/PI density plots for each condition, and the lower panel shows histograms representing annexin V-positive cells
Fig. 5.
Aβ peptides are oligomerized during incubation with cells and reduced by co-incubation with Hsp70. Cells (N2A) were incubated in DMEM medium containing 1% FBS at 37 °C for 48 h in the absence (lane 1) or presence of Hsp70 (0.32 μg) (lane 2). Cells were also incubated with monomerized Aβ1-42 peptides (10 μM) (lane 3) or co-incubated with Hsp70 (0.32 μg) added on day 1 or added on days 1 (lane 4) and 2 (lane 5). At the end of the incubation period, the extracellular medium was collected, depleted of any floating cells by centrifugation and electrophoresed, transferred onto nitrocellulose membranes, and analyzed by Western blotting using Clone 4G8 antibody followed by an HRP-conjugated secondary antibody
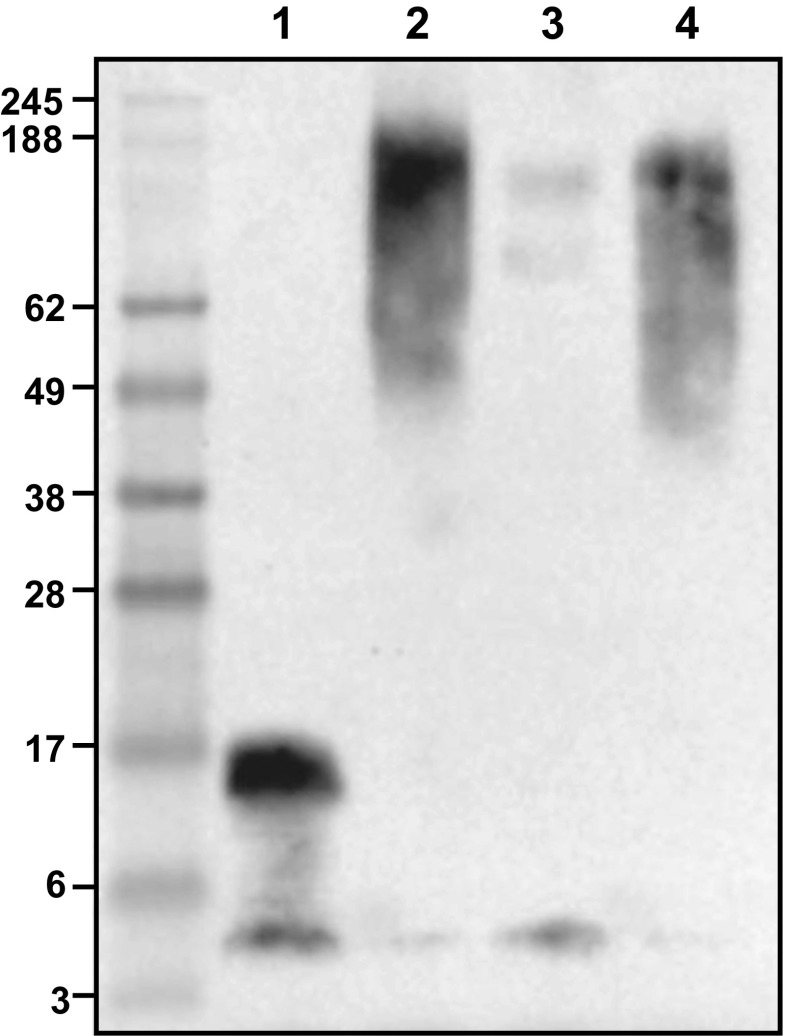
The addition of Hsp70 did not affect the toxicity of pre-oligomerized Aβ peptides
Aβ1-42 peptide monomers (Fig. 6, lane 1) were incubated in the absence (Fig. 6, lane 2) or presence of Hsp70 (Fig. 6, lane 2), at a ratio of 1 to 50 between Hsp70 and Aβ1-42 peptides, respectively, at 37 °C for 20 h. In addition, pre-oligomerized Aβ1-42 peptide complexes were incubated with Hsp70 at 37 °C for 20 h (Fig. 6, lane 4). Samples were electrophoresed and analyzed by Western blotting. As previously shown, the addition of Hsp70 interfered with Aβ1-42 peptide oligomerization. However, the addition of Hsp70 after Aβ1-42 peptide oligomerization did not reverse the process. It is important to note that the incubation of Hsp70 and Aβ1-42 peptides was performed in the absence of nucleotides. Then, N2A cells were exposed to Aβ1-42 peptides (5 μM) that were oligomerized in the absence or presence of Hsp70 (0.2 μM), or with Aβ1-42 peptides (5 μM) that were incubated with Hsp70 (0.2 μM) after the oligomerization process, and all incubations were carried out at 37 °C for 48 h. A dramatic reduction in cell death (90%) was observed when cells were incubated with medium containing pre-oligomerized Aβ1-42 peptides in the presence of Hsp70 as opposed to cells incubated with pre-oligomerized Aβ1-42 peptides in the absence of Hsp70 (Fig. 7). In contrast, the addition of Hsp70 after oligomerization of Aβ1-42 peptides displayed the same level of toxicity as pre-oligomerized Aβ peptides alone (Fig. 7). No toxic effect was observed after the addition of Hsp70 in the absence of Aβ peptides (Fig. 7).
Fig. 6.
Hsp70 interferes with the oligomerization of Aβ peptides but does not affect pre-oligomerized peptides. Monomerized Aβ1-42 peptides (1 μg) were kept as a monomer (lane 1), or incubated at 37 °C for 20 h (lane 2), or incubated with Hsp70 (0.32 μg) (lane 3) in 4.5 mM Tris pH 7.4 at 37 °C for 20 h. Oligomerized Aβ1-42 peptides (1 μg) were incubated with Hsp70 (0.32 μg) in 4.5 mM Tris pH 7.4 at 37 °C for 20 h (lane 4). Samples were electrophoresed, transferred onto nitrocellulose membranes, and analyzed by Western blotting using Clone 4G8 antibody followed by an HRP-conjugated secondary antibody. Membranes were stripped and incubated with 1:1000 dilutions of rabbit anti-Hsp70 (ADI-SPA-812), followed by an HRP-conjugated secondary antibody
Fig. 7.
Hsp70 improves Aβ peptide-induced cellular toxicity only by preventing the formation of Aβ peptide oligomers. N2A cells were exposed to Aβ1-42 peptides (5 μM) monomers in the absence (Aβ) or presence of Hsp70 (0.2 μM, Aβ+Hsp70 pre-I), or with oligomerized Aβ1-42 peptides (5 μM) incubated with Hsp70 (0.2 μM, Aβ+Hsp70 post-I) after the oligomerization process. All incubations were carried out at 37 °C for 48 h. Hsp70 toxicity in the absence of Aβ peptides was also tested by incubating N2A cells with Hsp70 (0.2 μM, Hsp70) at 37 °C for 48 h. Cell death was evaluated by annexin V and propidium iodide staining and flow cytometry analysis. Upper panels show representative annexin V/PI density plots for each condition, and the lower panel shows histograms representing annexin V-positive cells
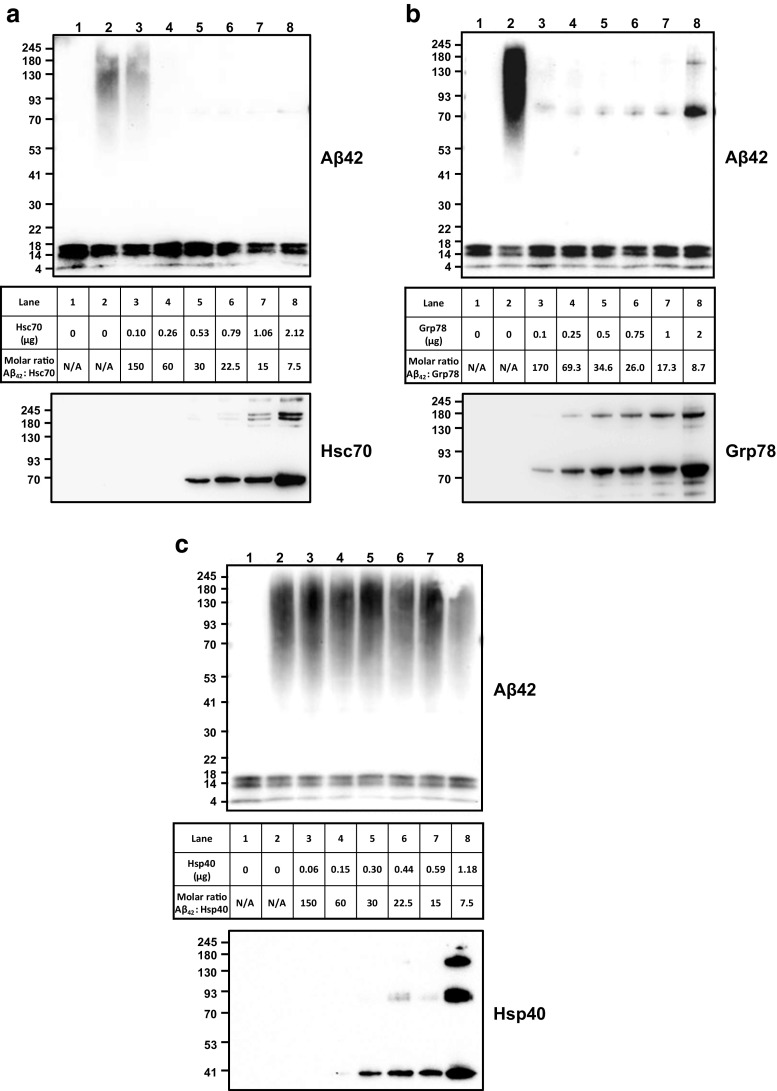
Other members of the Hsp70 family also interfered with Aβ peptide oligomerization
Based on the prior observations indicating that Hsp70 reduced Aβ1-42 oligomerization in in vitro conditions, it was important to test whether this effect was specific to other members of the Hsp70 family. Monomeric Aβ1-42 peptides were incubated with various concentrations of Hsc70 (HSPA8) or Grp78 (HSPA5) at 37 °C for 20 h. In addition, Aβ peptides were incubated with Hsp40 (DNAJB1) in the same conditions described above. The products of the incubations were analyzed by Western blotting. All members of the Hsp70 family (Hsc70 and Grp78) reduced the oligomerization of Aβ1-42 peptides in a concentration-dependent manner (Fig. 8a, b). In contrast, Hsp40 did not affect the oligomerization process of Aβ1-42 (Fig. 8c).
Fig. 8.
Hsc70 and Grp78 interfere with the oligomerization of Aβ peptides. Monomerized Aβ1-42 peptides (1 μg) were kept as a monomer (lane 1), or incubated at 37 °C for 20 h (lane 2), or incubated with various concentrations of a Hsc70 (from 0.1 to 2.12 μg) (lanes 3–8), b Grp78 (from 0.1 to 2 μg) (lanes 3–8), or c Hsp40 (from 0.1 to 1.18 μg) (lanes 3–8), in 4.5 mM Tris pH 7.4 at 37 °C for 24 h. Samples were electrophoresed, transferred onto nitrocellulose membranes, and analyzed by Western blotting using Clone 4G8 antibody followed by an HRP-conjugated secondary antibody. Membranes were stripped and incubated with 1:1000 dilutions of rat anti-Hsc70 (ADI-SPA-815), rabbit anti-Grp78 (StressMarq, SPC-180), or rabbit anti-Hsp40 (Cell Signal # 48685) and the respective secondary HRP-conjugated secondary antibody
Discussion
AD is likely to become the major health problem of the current century due to the growth of the aging population, the increasing cost to the healthcare system, and the social and emotional burden for relatives and caregivers (Crews and Masliah 2010; Lobello et al. 2012; Cummings et al. 2017). Therapeutic interventions to ameliorate the incidence of AD are not envisioned in the near future since the initial causes and manifestations of AD are not well understood. The current theory for the incidence of AD is the “amyloid hypothesis,” indicating that increasing levels of Aβ peptides are responsible for neuronal toxicity (Benilova et al. 2012). Aβ peptides are prone to aggregate very rapidly, probably due to a conformational change forming β-sheet-rich structures that stabilize within oligomeric complexes of different sizes that eventually develop into amyloid-type fibrils that accumulate in the brain and correspond to the most widely known hallmark of AD (Bitan et al. 2003; Haass and Selkoe 2007; Roychaudhuri et al. 2009). Aβ peptide intermediates have been shown to be transient and heterogeneous with some displaying an annular pore-like structure (Kotler et al. 2014). The major peptides that are released from cells correspond to Aβ1–40 and Aβ1-42 that displayed differences in their aggregation process and cytotoxicity (Bitan et al. 2003; Fu et al. 2017). Currently, it has been proposed that Aβ oligomeric complexes show differences in their cytotoxicity with the low molecular weight oligomers being the most toxic (Lambert et al. 1998; Kirkitadze et al. 2002; Dahlgren et al. 2002; Zhao et al. 2012).
In the present study, we compare the cytotoxicity of monomeric or pre-oligomerized forms of Aβ1-42 peptides, finding that both complexes induced N2A cell death after incubation at 37 °C for 48 h. Moreover, the monomeric forms of Aβ1-42 were observed to oligomerize within the culture medium during the incubation period at 37 °C, perhaps resulting in low molecular weight cytotoxic complexes. Although toxicity was observed after incubation with both monomers and pre-oligomers, cell death was elevated when cells were initially exposed to Aβ1-42 peptide monomers as opposed to pre-oligomerized complexes. Moreover, it appears that incubation with Aβ1-42 monomers induced cell death by apoptosis, whereas exposure to pre-oligomerized complexes induced a necrotic-like process. The trigger of apoptosis after exposure to Aβ1-42 monomers may be related to an increase in intracellular calcium levels, as it has been previously reported (Arispe et al. 2007; Lin and Arispe 2015). In this regard, extensive studies have shown that low molecular weight Aβ complexes get incorporated in both artificial and in natural membranes opening ion conductance pathways or channels (Arispe et al. 1993a, b, 1996; Kawahara et al. 1997; Capone et al. 2009), that are selective for calcium (Arispe et al. 1993b, 1996). Thus, we speculate that incubation of cells with Aβ monomers resulted in a slow production of low molecular weight complexes that get inserted in the plasma membrane opening a channel activity, increasing the flow of calcium inside the cells activating the apoptotic process. The proposed structures for these Aβ channels are annular oligomeric conformation formed by intermediate oligomers (Durell et al. 1994; Arispe et al. 2010; Shafrir et al. 2010a, b; Connelly et al. 2012; Lee et al. 2016; Jang et al. 2010). High molecular weight Aβ peptide complexes could also interact with cell membranes but result in the formation of larger nonselective pores that induce cell death by necrosis. This idea was previously considered when comparing the effect of aggregates from freshly prepared Aβ peptide solutions to larger aggregates from aged Aβ peptide solutions (Simakova and Arispe 2006). These aged aggregates produce nonselective increases in membrane permeability, which permits the passage of molecules greater than the size cutoff for most ion channels. Other studies suggested that membrane disruption by Aβ peptides occurs by a two-step process, with the initial formation of ion-selective pores followed by nonspecific, noncation selective, fragmentation of the lipid membrane during amyloid fiber formation (Sciacca et al. 2012).
Our studies indicate that the cytotoxicity of Aβ peptides builds up during the process of oligomerization. Therefore, interfering with this process may be critical to reducing the neuron degeneration that is associated with the development of AD. Prior studies have shown that induction of the stress response and expression of hsp resulted in protection from Aβ peptide toxicity (Kirby et al. 1994; Muchowski and Wacker 2005; Brown 2007; King et al. 2009; Hoshino et al. 2011; Toth et al. 2013; Bobkova et al. 2014). In these investigations, the assumption was that Hsp70 as a molecular chaperone could indeed interrupt Aβ peptide oligomerization. However, hsp are mainly localized in the intracellular compartments, separating them from the toxic Aβ peptides that are present in the extracellular environment. This potential discrepancy is resolved by the increasing evidence that hsp are present outside cells (Hightower and Guidon 1989; De Maio 2011). Therefore, it is possible that the protective effect of hsp is related to their export into the extracellular milieu. We tested this hypothesis and certainly found that Hsp70 could interfere with Aβ peptide oligomerization in vitro reducing cytotoxicity in culture conditions. The reduction in Aβ peptide oligomerization after incubation with Hsp70 echoes prior observations in vitro (Evans et al. 2006). In contrast, the addition of Hsp70 to pre-oligomerized Aβ peptides neither disperses the oligomeric complexes nor decreases cytotoxicity. Other studies have shown that the release of Hsp70 into the extracellular milieu by glial cells conferred protection to neighboring neurons (Guzhova et al. 2001). Recent investigations using a modified Hsp70 containing a secretory signal that allows the protein to be secreted also showed protection in a Drosophila model of AD (Fernandez-Funez et al. 2016). In addition, exogenous intranasal administration of Hsp70 reached the brain and ameliorated some symptoms associated with AD in a mouse model (Bobkova et al. 2014).
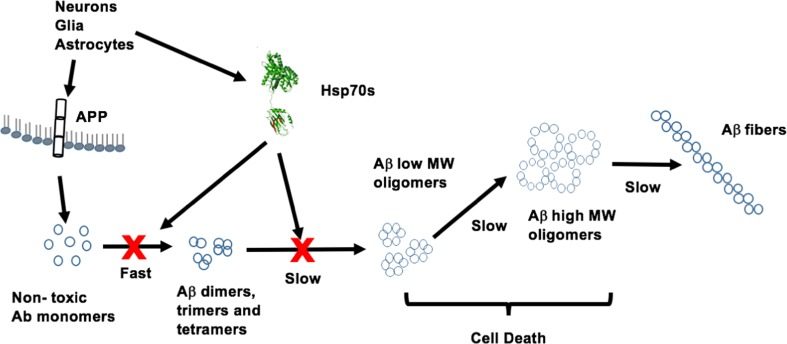
A major finding from our studies is that the inhibition of Aβ1-42 oligomerization could be observed at a molar ratio 1:150 between Hsp70 and Aβ1-42, in the absence of nucleotides. A similar substoichiometric phenomenon was observed in the inhibition of Aβ fiber formation by Hsp70 in an ATP-dependent fashion (Evans et al. 2006). Our observations are not compatible with a chaperone activity for Hsp70 in which one Hsp70 binds to one Aβ1-42 peptide in a nucleotide-dependent manner. An alternative is that Hsp70 interferes with the conversion of small Aβ peptide complexes (dimers, trimers, or tetramers) into larger oligomers in a nonchaperone mode (Fig. 9). Thus, it is possible that Hsp70 interferes with an early step in the oligomerization process, which has been reported to result in a conformational change from a radon coil structure to a β-sheet conformation assembling into oligomers of different sizes (Roche et al. 2016; Seo et al. 2017; Bobo et al. 2017). Indeed, some amyloid complexes are the product of stable antiparallel cross-β-sheet complexes (Balbirnie et al. 2001), which have been modulated in silico (Dorosh and Stepanova 2016). It has been hypothesized that the initial step in Aβ peptide oligomerization is related to the formation of a “seed” complex that triggers the oligomerization process (Harper et al. 1997). Thus, Hsp70 may be interfering with this initial seeding step in a very efficient manner, perhaps acting as a buffer system. Therefore, the question that emerges is whether the interaction of Hsp70 with the initial seeding of Aβ peptide complexes is reversible or whether Hsp70 stabilized this initial complex in a form that is incapable of further oligomerization. A study on small hsp has shown that this protein sequestered Aβ oligomers into large aggregates that are not toxic. In addition, they proposed that the small hsp underwent a conformational change upon interaction with Aβ peptides (Ojha et al. 2011). In contrast with these observations, we did not detect any activity of Hsp70 disrupting very large peptide aggregates. Similarly, DNAJB6 was reported to reduce the aggregation of Aβ1-42 peptides also in a nonstoichiometric mode (Mansson et al. 2014), as we described herewith for the Hsp70 family. Interestingly, the decrease in Aβ1-42 high molecular weight complexes by DNAJB6 was not observed by other members of the DNAJ family, including DNAJB1 (Hsp40), in agreement with our results.
Fig. 9.
Model of Aβ peptide oligomerization and interference by Hsp70. Aβ peptides and Hsp70s are released from neurons, glial cells, and astrocytes into the extracellular environment. Aβ monomers are produced by enzymatic cleavage of the membrane-anchored amyloid β precursor protein APP. Once released, Aβ initiates a very rapid oligomerization process with the formation of dimers, trimers, and tetrameters, followed by the slow assembly of large molecular weight oligomers, which are the cytotoxic complexes, and fibers. Hsp70s interfere with the assembly of these large molecular weight oligomers resulting in reduced cytotoxicity
Our findings also indicated that other members of the Hsp70 family, including Hsc70 and Grp78, are also capable of preventing Aβ peptide oligomerization. Therefore, it is possible that the export of any Hsp70 family member during normal physiological conditions could control the oligomerization of Aβ peptides. Thus, the presence of Hsp70 in the extracellular environment might help to maintain Aβ peptides in the monomeric form that could be cleared from the brain by a natural process (Fig. 9). Indeed, Aβ peptides are cleared from the brain very efficiently (Shibata et al. 2000; Bu 2009; Kanekiyo et al. 2013; Liu et al. 2017). Moreover, the imbalance between production and clearance has been proposed as a cause of AD (Bu 2009; Selkoe and Hardy 2016). Thus, we can speculate that altering the balance between extracellular Hsp70 and Aβ peptides may increase the level of neurotoxicity contributing to the development of AD. A disparity between Aβ peptides and Hsp70 may occur during aging. Expression of hsp (Heydari et al. 1995; Pahlavani et al. 1995; Nitta et al. 1994; Faassen et al. 1989) and their circulating levels (Rea et al. 2001; Njemini et al. 2011a, b) have both been reported to decay during aging. In contrast, circulating levels of Aβ peptides increased with age (Shoji et al. 2001). Consequently, it is possible that the reduction in hsp expression and the parallel increase in Aβ peptide release during aging are a cause for the development of advanced neuronal dysfunction and the progression of AD.
Acknowledgements
We would like to thank Barbara Rho for her excellent editing of the manuscript.
Funding
This work was supported by National Institutes of Health (NIH) Grant R01 GM11447 and UC San Diego Academic Senate grant.
References
- Arispe N, Pollard HB, Rojas E. Giant multilevel cation channels formed by Alzheimer disease amyloid beta-protein [A beta P-(1-40)] in bilayer membranes. Proc Natl Acad Sci U S A. 1993;90(22):10573–10577. doi: 10.1073/pnas.90.22.10573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arispe N, Rojas E, Pollard HB. Alzheimer disease amyloid beta protein forms calcium channels in bilayer membranes: blockade by tromethamine and aluminum. Proc Natl Acad Sci U S A. 1993;90(2):567–571. doi: 10.1073/pnas.90.2.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arispe N, Pollard HB, Rojas E. Zn2+ interaction with Alzheimer amyloid beta protein calcium channels. Proc Natl Acad Sci U S A. 1996;93(4):1710–1715. doi: 10.1073/pnas.93.4.1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arispe N, Diaz JC, Simakova O. Abeta ion channels. Prospects for treating Alzheimer’s disease with Abeta channel blockers. Biochim Biophys Acta. 2007;1768(8):1952–1965. doi: 10.1016/j.bbamem.2007.03.014. [DOI] [PubMed] [Google Scholar]
- Arispe N, et al. Polyhistidine peptide inhibitor of the Abeta calcium channel potently blocks the Abeta-induced calcium response in cells. Theoretical modeling suggests a cooperative binding process. Biochemistry. 2010;49(36):7847–7853. doi: 10.1021/bi1006833. [DOI] [PubMed] [Google Scholar]
- Balbirnie M, Grothe R, Eisenberg DS. An amyloid-forming peptide from the yeast prion Sup35 reveals a dehydrated beta-sheet structure for amyloid. Proc Natl Acad Sci U S A. 2001;98(5):2375–2380. doi: 10.1073/pnas.041617698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benilova I, Karran E, De Strooper B. The toxic Abeta oligomer and Alzheimer’s disease: an emperor in need of clothes. Nat Neurosci. 2012;15(3):349–357. doi: 10.1038/nn.3028. [DOI] [PubMed] [Google Scholar]
- Bieschke J, et al. Small-molecule conversion of toxic oligomers to nontoxic beta-sheet-rich amyloid fibrils. Nat Chem Biol. 2011;8(1):93–101. doi: 10.1038/nchembio.719. [DOI] [PubMed] [Google Scholar]
- Bitan G, et al. Amyloid beta -protein (Abeta) assembly: Abeta 40 and Abeta 42 oligomerize through distinct pathways. Proc Natl Acad Sci U S A. 2003;100(1):330–335. doi: 10.1073/pnas.222681699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bobkova NV, et al. Therapeutic effect of exogenous hsp70 in mouse models of Alzheimer’s disease. J Alzheimers Dis. 2014;38(2):425–435. doi: 10.3233/JAD-130779. [DOI] [PubMed] [Google Scholar]
- Bobo C, et al. Synthetic toxic Abeta1-42 oligomers can assemble in different morphologies. Biochim Biophys Acta. 2017;1861(5 Pt A):1168–1176. doi: 10.1016/j.bbagen.2017.03.001. [DOI] [PubMed] [Google Scholar]
- Brown IR. Heat shock proteins and protection of the nervous system. Ann N Y Acad Sci. 2007;1113:147–158. doi: 10.1196/annals.1391.032. [DOI] [PubMed] [Google Scholar]
- Bu G. Apolipoprotein E and its receptors in Alzheimer’s disease: pathways, pathogenesis and therapy. Nat Rev Neurosci. 2009;10(5):333–344. doi: 10.1038/nrn2620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capone R, et al. Amyloid-beta-induced ion flux in artificial lipid bilayers and neuronal cells: resolving a controversy. Neurotox Res. 2009;16(1):1–13. doi: 10.1007/s12640-009-9033-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow AM, et al. Localization of heat shock proteins in cerebral cortical cultures following induction by celastrol. Cell Stress Chaperones. 2014;19(6):845–851. doi: 10.1007/s12192-014-0508-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connelly L, et al. Atomic force microscopy and MD simulations reveal pore-like structures of all-D-enantiomer of Alzheimer’s beta-amyloid peptide: relevance to the ion channel mechanism of AD pathology. J Phys Chem B. 2012;116(5):1728–1735. doi: 10.1021/jp2108126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crews L, Masliah E. Molecular mechanisms of neurodegeneration in Alzheimer’s disease. Hum Mol Genet. 2010;19(R1):R12–R20. doi: 10.1093/hmg/ddq160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings J, et al. Alzheimer’s disease drug development pipeline: 2017. Alzheimers Dement. 2017;3:367–384. doi: 10.1016/j.trci.2017.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlgren KN, et al. Oligomeric and fibrillar species of amyloid-beta peptides differentially affect neuronal viability. J Biol Chem. 2002;277(35):32046–32053. doi: 10.1074/jbc.M201750200. [DOI] [PubMed] [Google Scholar]
- De Maio A. Heat shock proteins: facts, thoughts, and dreams. Shock. 1999;11(1):1–12. doi: 10.1097/00024382-199901000-00001. [DOI] [PubMed] [Google Scholar]
- De Maio A (2011) Extracellular heat shock proteins, cellular export vesicles, and the stress observation system: a form of communication during injury, infection, and cell damage. Cell Stress Chaperones 16(3):235–249 [DOI] [PMC free article] [PubMed]
- De Maio A, Vazquez D. Extracellular heat shock proteins: a new location, a new function. Shock. 2013;40(4):239–246. doi: 10.1097/SHK.0b013e3182a185ab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorosh L, Stepanova M. Probing oligomerization of amyloid beta peptide in silico. Mol BioSyst. 2016;13(1):165–182. doi: 10.1039/C6MB00441E. [DOI] [PubMed] [Google Scholar]
- Durell SR, et al. Theoretical models of the ion channel structure of amyloid beta-protein. Biophys J. 1994;67(6):2137–2145. doi: 10.1016/S0006-3495(94)80717-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans CG, Wisen S, Gestwicki JE. Heat shock proteins 70 and 90 inhibit early stages of amyloid beta-(1-42) aggregation in vitro. J Biol Chem. 2006;281(44):33182–33191. doi: 10.1074/jbc.M606192200. [DOI] [PubMed] [Google Scholar]
- Faassen AE, et al. Diminished heat-shock protein synthesis following mitogen stimulation of lymphocytes from aged donors. Exp Cell Res. 1989;183(2):326–334. doi: 10.1016/0014-4827(89)90393-5. [DOI] [PubMed] [Google Scholar]
- Fernandez-Funez P, et al. Holdase activity of secreted Hsp70 masks amyloid-beta42 neurotoxicity in Drosophila. Proc Natl Acad Sci U S A. 2016;113(35):E5212–E5221. doi: 10.1073/pnas.1608045113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu L, et al. Comparison of neurotoxicity of different aggregated forms of Abeta40, Abeta42 and Abeta43 in cell cultures. J Pept Sci. 2017;23(3):245–251. doi: 10.1002/psc.2975. [DOI] [PubMed] [Google Scholar]
- Gastpar R, et al. Heat shock protein 70 surface-positive tumor exosomes stimulate migratory and cytolytic activity of natural killer cells. Cancer Res. 2005;65(12):5238–5247. doi: 10.1158/0008-5472.CAN-04-3804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guzhova I, et al. In vitro studies show that Hsp70 can be released by glia and that exogenous Hsp70 can enhance neuronal stress tolerance. Brain Res. 2001;914(1–2):66–73. doi: 10.1016/S0006-8993(01)02774-3. [DOI] [PubMed] [Google Scholar]
- Haass C, Selkoe DJ. Soluble protein oligomers in neurodegeneration: lessons from the Alzheimer’s amyloid beta-peptide. Nat Rev Mol Cell Biol. 2007;8(2):101–112. doi: 10.1038/nrm2101. [DOI] [PubMed] [Google Scholar]
- Harper JD, Lieber CM, Lansbury PT., Jr Atomic force microscopic imaging of seeded fibril formation and fibril branching by the Alzheimer’s disease amyloid-beta protein. Chem Biol. 1997;4(12):951–959. doi: 10.1016/S1074-5521(97)90303-3. [DOI] [PubMed] [Google Scholar]
- Heydari AR, Conrad CC, Richardson A. Expression of heat shock genes in hepatocytes is affected by age and food restriction in rats. J Nutr. 1995;125(3):410–418. doi: 10.1093/jn/125.3.410. [DOI] [PubMed] [Google Scholar]
- Hightower LE, Guidon PT., Jr Selective release from cultured mammalian cells of heat-shock (stress) proteins that resemble glia-axon transfer proteins. J Cell Physiol. 1989;138(2):257–266. doi: 10.1002/jcp.1041380206. [DOI] [PubMed] [Google Scholar]
- Hoshino T, et al. Suppression of Alzheimer’s disease-related phenotypes by expression of heat shock protein 70 in mice. J Neurosci. 2011;31(14):5225–5234. doi: 10.1523/JNEUROSCI.5478-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang H, et al. beta-Barrel topology of Alzheimer’s beta-amyloid ion channels. J Mol Biol. 2010;404(5):917–934. doi: 10.1016/j.jmb.2010.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kampinga HH, et al. Guidelines for the nomenclature of the human heat shock proteins. Cell Stress Chaperones. 2009;14(1):105–111. doi: 10.1007/s12192-008-0068-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanekiyo T, et al. Neuronal clearance of amyloid-beta by endocytic receptor LRP1. J Neurosci. 2013;33(49):19276–19283. doi: 10.1523/JNEUROSCI.3487-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawahara M, Arispe N, Kuroda Y, Rojas E (1997) Alzheimer’s disease amyloid beta-protein forms Zn(2+)-sensitive, cation-selective channels across excised membrane patches from hypothalamic neurons. Biophys J 73(1):67–75 [DOI] [PMC free article] [PubMed]
- King M, et al. The small heat shock protein Hsp27 protects cortical neurons against the toxic effects of beta-amyloid peptide. J Neurosci Res. 2009;87(14):3161–3175. doi: 10.1002/jnr.22145. [DOI] [PubMed] [Google Scholar]
- Kirby BA, et al. Heat shock proteins protect against stress-related phosphorylation of tau in neuronal PC12 cells that have acquired thermotolerance. J Neurosci. 1994;14(9):5687–5693. doi: 10.1523/JNEUROSCI.14-09-05687.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkitadze MD, Bitan G, Teplow DB. Paradigm shifts in Alzheimer’s disease and other neurodegenerative disorders: the emerging role of oligomeric assemblies. J Neurosci Res. 2002;69(5):567–577. doi: 10.1002/jnr.10328. [DOI] [PubMed] [Google Scholar]
- Kotler SA, et al. Differences between amyloid-beta aggregation in solution and on the membrane: insights into elucidation of the mechanistic details of Alzheimer’s disease. Chem Soc Rev. 2014;43(19):6692–6700. doi: 10.1039/C3CS60431D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert MP, et al. Diffusible, nonfibrillar ligands derived from Abeta1-42 are potent central nervous system neurotoxins. Proc Natl Acad Sci U S A. 1998;95(11):6448–6453. doi: 10.1073/pnas.95.11.6448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee M, et al. Conformational changes of Abeta (1-42) monomers in different solvents. J Mol Graph Model. 2016;65:8–14. doi: 10.1016/j.jmgm.2016.02.003. [DOI] [PubMed] [Google Scholar]
- Lin H, Arispe NJ. Single-cell screening of cytosolic [Ca(2+)] reveals cell-selective action by the Alzheimer’s Abeta peptide ion channel. Cell Stress Chaperones. 2015;20(2):333–342. doi: 10.1007/s12192-014-0551-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindquist S, Craig EA. The heat-shock proteins. Annu Rev Genet. 1988;22:631–677. doi: 10.1146/annurev.ge.22.120188.003215. [DOI] [PubMed] [Google Scholar]
- Liu CC, et al. Astrocytic LRP1 mediates brain Abeta clearance and impacts amyloid deposition. J Neurosci. 2017;37(15):4023–4031. doi: 10.1523/JNEUROSCI.3442-16.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobello K, et al. Targeting beta amyloid: a clinical review of immunotherapeutic approaches in Alzheimer’s disease. Int J Alzheimers Dis. 2012;2012:628070. doi: 10.1155/2012/628070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansson C, et al. Interaction of the molecular chaperone DNAJB6 with growing amyloid-beta 42 (Abeta42) aggregates leads to sub-stoichiometric inhibition of amyloid formation. J Biol Chem. 2014;289(45):31066–31076. doi: 10.1074/jbc.M114.595124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marini AM, et al. 70-kilodalton heat shock protein induction in cerebellar astrocytes and cerebellar granule cells in vitro: comparison with immunocytochemical localization after hyperthermia in vivo. J Neurochem. 1990;54(5):1509–1516. doi: 10.1111/j.1471-4159.1990.tb01198.x. [DOI] [PubMed] [Google Scholar]
- Muchowski PJ, Wacker JL. Modulation of neurodegeneration by molecular chaperones. Nat Rev Neurosci. 2005;6(1):11–22. doi: 10.1038/nrn1587. [DOI] [PubMed] [Google Scholar]
- Nitta A, et al. beta-Amyloid protein-induced Alzheimer’s disease animal model. Neurosci Lett. 1994;170(1):63–66. doi: 10.1016/0304-3940(94)90239-9. [DOI] [PubMed] [Google Scholar]
- Njemini R, et al. Circulating heat shock protein 70 in health, aging and disease. BMC Immunol. 2011;12:24. doi: 10.1186/1471-2172-12-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Njemini R, et al. Circulating heat shock protein 70 (Hsp70) in elderly members of a rural population from Cameroon: association with infection and nutrition. Arch Gerontol Geriatr. 2011;53(3):359–363. doi: 10.1016/j.archger.2011.01.005. [DOI] [PubMed] [Google Scholar]
- Ojha J, et al. Sequestration of toxic oligomers by HspB1 as a cytoprotective mechanism. Mol Cell Biol. 2011;31(15):3146–3157. doi: 10.1128/MCB.01187-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pahlavani MA, et al. The expression of heat shock protein 70 decreases with age in lymphocytes from rats and rhesus monkeys. Exp Cell Res. 1995;218(1):310–318. doi: 10.1006/excr.1995.1160. [DOI] [PubMed] [Google Scholar]
- Rea IM, McNerlan S, Pockley AG. Serum heat shock protein and anti-heat shock protein antibody levels in aging. Exp Gerontol. 2001;36(2):341–352. doi: 10.1016/S0531-5565(00)00215-1. [DOI] [PubMed] [Google Scholar]
- Roche J, et al. Monomeric Abeta(1-40) and Abeta(1-42) peptides in solution adopt very similar Ramachandran map distributions that closely resemble random coil. Biochemistry. 2016;55(5):762–775. doi: 10.1021/acs.biochem.5b01259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roychaudhuri R, et al. Amyloid beta-protein assembly and Alzheimer disease. J Biol Chem. 2009;284(8):4749–4753. doi: 10.1074/jbc.R800036200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sciacca MF, et al. Two-step mechanism of membrane disruption by Abeta through membrane fragmentation and pore formation. Biophys J. 2012;103(4):702–710. doi: 10.1016/j.bpj.2012.06.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selkoe DJ, Hardy J. The amyloid hypothesis of Alzheimer’s disease at 25 years. EMBO Mol Med. 2016;8(6):595–608. doi: 10.15252/emmm.201606210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seo J, et al. An infrared spectroscopy approach to follow beta-sheet formation in peptide amyloid assemblies. Nat Chem. 2017;9(1):39–44. doi: 10.1038/nchem.2615. [DOI] [PubMed] [Google Scholar]
- Shafrir Y et al (2010a) Beta-barrel models of soluble amyloid beta oligomers and annular protofibrils. Proteins 78(16):3458–3472 [DOI] [PMC free article] [PubMed]
- Shafrir Y et al (2010b) Models of membrane-bound Alzheimer’s Abeta peptide assemblies. Proteins 78(16):3473–3487 [DOI] [PMC free article] [PubMed]
- Shibata M, et al. Clearance of Alzheimer’s amyloid-ss(1-40) peptide from brain by LDL receptor-related protein-1 at the blood-brain barrier. J Clin Invest. 2000;106(12):1489–1499. doi: 10.1172/JCI10498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoji M, et al. The levels of cerebrospinal fluid Abeta40 and Abeta42(43) are regulated age-dependently. Neurobiol Aging. 2001;22(2):209–215. doi: 10.1016/S0197-4580(00)00229-3. [DOI] [PubMed] [Google Scholar]
- Simakova O, Arispe NJ. Early and late cytotoxic effects of external application of the Alzheimer’s Abeta result from the initial formation and function of Abeta ion channels. Biochemistry. 2006;45(18):5907–5915. doi: 10.1021/bi060148g. [DOI] [PubMed] [Google Scholar]
- Simakova O, Arispe NJ. The cell-selective neurotoxicity of the Alzheimer’s Abeta peptide is determined by surface phosphatidylserine and cytosolic ATP levels. Membrane binding is required for Abeta toxicity. J Neurosci. 2007;27(50):13719–13729. doi: 10.1523/JNEUROSCI.3006-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprang GK, Brown IR. Selective induction of a heat shock gene in fibre tracts and cerebellar neurons of the rabbit brain detected by in situ hybridization. Brain Res. 1987;427(1):89–93. doi: 10.1016/0169-328X(87)90049-0. [DOI] [PubMed] [Google Scholar]
- Thinakaran G, Koo EH. Amyloid precursor protein trafficking, processing, and function. J Biol Chem. 2008;283(44):29615–29619. doi: 10.1074/jbc.R800019200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toth ME, et al. Overexpression of Hsp27 ameliorates symptoms of Alzheimer’s disease in APP/PS1 mice. Cell Stress Chaperones. 2013;18(6):759–771. doi: 10.1007/s12192-013-0428-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao LN, et al. The toxicity of amyloid beta oligomers. Int J Mol Sci. 2012;13(6):7303–7327. doi: 10.3390/ijms13067303. [DOI] [PMC free article] [PubMed] [Google Scholar]