Abstract
Purpose
To investigate 100 consecutive cases of videoscopic retrograde intrarenal surgery (RIRS) by a single surgeon and to evaluate factors associated with stone-free status and the learning curve thereof.
Materials and Methods
We analyzed the results of videoscopic RIRS in 100 patients who underwent primary treatment for renal stones from January 2015 to August 2016. Videoscopic RIRS were performed with URF-V and URF-V2 flexible video uteroscopes (Olympus) or a Flex-Xc flexible ureterorenoscope (KARL STORZ). Non-contrast computed tomography was taken at 3 months postoperatively to confirm the absence of stones. The stone characteristics included the location, maximal stone length (MSL), stone heterogeneity index (SHI), and mean stone density (MSD). Fragmentation efficacy was calculated as operative time (min) divided by removed MSL (mm), and was evaluated in the sequential order of operations.
Results
The mean age of the total patient was 60.0±14.0 years. The mean MSL was 13.1±6.2 mm. The average MSD was 734.2±327.6 Hounsfield unit (HU) and the SHI was 241.0±120.0 HU. The mean operation time was 65.1±45.7 min considering each renal unit. The stone-free rate at 3 months post-surgery was 87%. The estimated cut-off of the time-to-MSL ratio below 5 min/mm was 50. Multivariate analyses indicated a lower MSD [odds ratio (OR): 0.998; 95% confidence interval (CI): 0.996–0.999; p=0.047) and the last 50 cases (OR: 5.408, 95% CI: 1.337–30.426; p=0.030) as independent predictors of stone-free status after videoscopic RIRS.
Conclusion
Low MSDs and the last 50 cases were significant predictors of stone-free rate in videoscopic RIRS.
Keywords: Urinary calculi, endoscopes, treatment outcome
INTRODUCTION
Urolithiasis is one of the most common urological diseases.1 An estimated 12% of the global population suffers from urinary stone disease throughout their lifetime, and the recurrence rate thereof is about 50%.2 Several treatment methods have traditionally been used to treat urinary stone disease, including observation (on spontaneous passage), shock wave lithotripsy (SWL), retrograde endoscopic procedures, and percutaneous nephrolithotomy.3 With advances in flexible endoscopy, improved perimeter duration, miniaturization of the endoscope, improved translucence, enhanced field of view, and effective lithotripsy technology, retrograde intrarenal surgery (RIRS) has been widely embraced, and used as a first-line treatment.4,5
In the past 10 years, digital flexible ureteroreno-videoscopes have been introduced, and shown to be superior to fiber-optic ureterorenoscopes, with decreased operative times, better vision, and increased maneuverability with similar stone-free rates.6 Recently introduced digital flexible ureteroreno videoscopes offer improved color reproducibility, two to three times better image resolution, and a larger image size.7 The release of the Flex-Xc digital flexible ureteroreno videoscope (KARL STORZ Endoskope, Tuttlingen, Germany) and the URF-V and URF-V2 flexible video uteroscopes (Olympus Corp., Tokyo, Japan) has expanded the choice of digital videoscopes available to clinicians. The Flex-Xc has been shown to have increased durability, and can be used without damage in more than 100 cases.8 The digital optical systems with URF-V, URF-V2, and Flex-Xc also offer a higher visibility, compared to the classical fiber-optic system.9 Despite these recent technical achievements, there has yet to be a report on digital videoscopic RIRS from Korea. The aim of our study was to retrospectively analyze videoscopic RIRS cases performed by a single surgeon to treat patients with renal stones and to evaluate the factors associated with a stone-free status and learning curves for the procedure.
MATERIALS AND METHODS
Patient cohort
Medical records were obtained from a database of 100 patients who underwent videoscopic RIRS (using Flex-Xc, URF-V, and URF-V2) by a single surgeon (J.Y.L.) at a single institute (Severance Hospital, Seoul, Korea) between January 2015 and August 2016 (Fig. 1). The patients had single or multiple calyceal, renal pelvic, or ureteropelvic stones of >4 mm with symptoms. A retrospective review was conducted of the outcomes of these 100 consecutive patients who underwent videoscopic RIRS as a single-session treatment.
Fig. 1. Three videoscope images of URF-V (A), URF-V2 (B), and Flex-Xc (C).
Good clinical practice protocols
The study was performed in accordance with all applicable laws and regulations, good clinical practices, and the ethical principles described in the Declaration of Helsinki. The Institutional Review Board of the hospital approved this study protocol (number 4-2017-0091). The study was exempt from requiring the participants' written informed consent because of its retrospective design and because the patients' records and information were anonymized and de-identified prior to analysis.
Retrograde intrarenal surgery
The patient was anesthetized with general or spinal anesthesia, and placed in lithotomy position. After cystoscopy, a hydrophilic guidewire (Roadrunner Wire Guide, Cook Medical, Bloomington, IN, USA) was inserted into the ureter. If pre-stenting was performed, using a ureteral stent, a hydrophilic guidewire was installed to the renal pelvis. A dual-lumen catheter was inserted through the hydrophilic guidewire, and retrograde pyelography was performed. Using the dual-lumen catheter, another guidewire (Amplatz Superstiff Guidewire; Boston Scientific, Marlborough, MA, USA) was inserted, and an 11/13 or 12/14 Fr ureteral access sheath (Uropass, Olympus) was inserted into the level of ureteropelvic junction. A flexible ureteroreno-videoscope was inserted through the ureteral access sheath. Lithotripsy was performed with a laser lithotripter (VersaPulse Powersuite 100W, Lumenis, Tel Aviv, Israel) and 200 micron laser fibers. Large fragmented stones were extracted using a 1.9 Fr (Zero-tip, Boston Scientific) or a 1.3 Fr (OptiFlex, Boston Scientific) nitinol stone basket. Dusted particles were not removed to allow for natural drainage. At the end of the procedure, fluoroscopy was performed to evaluate stone clearance. A 6 Fr ureteral stent (Polaris Ultra or Polaris Loop, Boston Scientific) was routinely placed and maintained for 1 to 2 weeks in all patients.
Demographic data and stone characteristics on non-contrast computed tomography
A detailed history of urinary tract stone disease for each patient was obtained, including the number of past stone events, history of pain onset, and stone characteristics. The stone characteristics included the location, maximal stone length (MSL), stone heterogeneity index (SHI), and mean stone density (MSD). The MSL was the longest stone length measured in three dimensions on non-contrast computed tomography (NCCT) images using the GE Centricity system (GE Healthcare Bio-Sciences Corp., Piscataway, NJ, USA). The MSD was measured using bone windows on the magnified axial NCCT image of the stone in the maximal diameter, in which the elliptical region of interest incorporated the largest cross-sectional area of the stone without including adjacent soft tissue.10 The SHI was defined as the standard deviation (SD) of Hounsfield units (HUs) in the same region of interest.11 Stone-free status was defined as either having no identifiable stone or a fragment of <4 mm in size in the post-operative NCCT.12 Complications were assessed according to the modified Clavien-Dindo classification. Fragmentation efficacy was calculated as “operative time (min) divided by removed MSL (mm)” and was evaluated in the sequential order of operations.
Statistical analyses
Statistical comparisons of patient demographic continuous variables were performed using either Student's or Welch's two-sample t-test. Categorical variables were compared using Pearson's chi-squared test with Yates' continuity correction. Univariate and multivariate logistic regression analyses using a binomial method were performed to identify factors significantly associated with one-session success. Statistical analyses were performed using R software (version 3.3.2, R Foundation for Statistical Computing, Vienna, Austria; http://www.r-project.org).
RESULTS
Patient and stone characteristics are listed in Table 1. The mean age of the patients was 60.0±14.0 years, and the female-to-male ratio was 31:69. The mean operation time was 65.1±45.7 minutes, considering each renal unit. The mean MSL was 13.1±6.2 mm, the average MSD was 734.2±327.6 HU, and SHI was 240.1±120.0 HU. The mean operation time of all patients was 65.1±45.7 min. Nineteen patients underwent bilateral operations or other operations at the same time. The changes in serum creatinine, estimated glomerular filtration rate (eGFR), and hemoglobin were 0.0±0.2, -0.1±0.2, and 0.0±0.1, respectively. The mean length of stay (LOS) in the hospital was 2.5±3.7 days. In 20 patients, LOS was more than 2 days, and they consisted of eight cases of hospitalized patients in other departments, seven cases of post-operative monitoring for cardiovascular and pulmonary co-morbidities, four cases of postoperative fever and infection, and one case of ureteral laceration.
Table 1. Demographic Data of All Patients and Two Subgroups of the First 50 Cases and the Last 50 Cases.
| Parameter | Total | First 50 cases | Last 50 cases | p value |
|---|---|---|---|---|
| No. of patients | 100 | 50 | 50 | |
| Age (yrs) | 60.0±14.0 | 61.0±14.1 | 58.9±13.9 | 0.442 |
| Sex (F:M) | 31:69 | 15:35 | 16:34 | 1.000 |
| Pre-stenting, n (%) | 91 (91.0) | 47 (94.0) | 44 (88.0) | 0.295 |
| BMI | 24.2±2.3 | 24.8±3.3 | 23.7±3.2 | 0.102 |
| MSL (mm) | 13.1±6.2 | 12.7±5.6 | 13.4±6.8 | 0.560 |
| MSD (HU) | 734.2±327.6 | 755.0±298.3 | 713.3±356.3 | 0.528 |
| SSD (mm) | 95.4±21.9 | 92.8±20.6 | 98.0±23.0 | 0.229 |
| SHI (HU) | 241.0±120.0 | 250.4±128.0 | 231.5±111.0 | 0.432 |
| Operation time (min) | 65.1±45.7 | 84.1±52.7 | 46.1±26.6 | <0.001 |
| Cr_change | 0.0±0.2 | 0.0±0.2 | 0.0±0.2 | 0.998 |
| eGFR_change | −0.1±0.2 | −0.1±0.2 | −0.1±0.2 | 0.870 |
| Hgb_change | 0.0±0.1 | 0.0±0.1 | 0.0±0.2 | 0.977 |
| LOS (day) | 2.5±3.7 | 2.1±1.8 | 2.9±5.0 | 0.242 |
| Time-to-MSL ratio (min/mm) | 5.5±4.0 | 7.2±4.8 | 3.8±1.8 | <0.001 |
| Auxiliary treatment, n (%) | 5 (5.0) | 5 (10.0) | 0 (0.0) | |
| Stone-free rate, n (%) | 87 (87.0) | 40 (80.0) | 47 (94.0) |
BMI, body mass index; MSL, maximal stone length; MSD, mean stone density; HU, Hounsfield unit; SSD, skin-to-stone distance; SHI, stone heterogeneity index; Cr, creatinine; eGFR, estimated glomerular filtration rate; Hgb, hemoglobin; LOS, length of stay.
The time-to-MSL ratio was 5.5±4.0 min/mm, and the stonefree rate was 87.0%. Postoperative complications occurred in five cases, and these included two cases of fever (Clavien-Dindo classification grade I), two cases of acute pyelonephritis (grade II), and one case of a ureteral laceration (grade III). In the ureteral laceration case, retrograde stent indwelling had failed, and percutaneous antegrade stenting and nephrostomy was performed during the operation. Two weeks later, antegrade pyelography revealed complete ureteral patency. There were no complications of sepsis or ureteral stricture during the follow-up period from 6 to 12 months. Auxiliary treatment (SWL) was performed in five cases postoperatively.
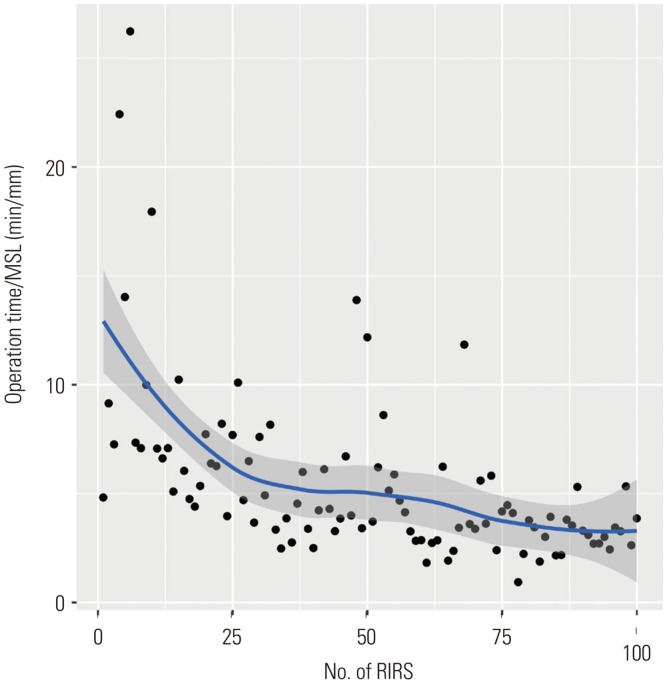
The time-to-MSL ratio is described in the scatter plot shown in Fig. 2. The estimated cut-off of the time-to-MSL ratio below 5 mm/min was 50. The 100 patients were divided into two groups comprising the first 50 cases and last 50 cases. There were no differences in age, sex, body mass index (BMI), MSL, MSD, skin-to-stone distance, and SHI between these two groups. Operation time in the last 50 cases (46.1±26.6 min) was shorter than that in the first 50 cases (84.1±52.7 min, p<0.001). Postoperative changes in serum creatinine, eGFR, and hemoglobin showed no statistical differences between the two groups. The LOS was 2.1±1.8 days in the first 50 cases and 2.9± 5.0 days in the last 50 cases (p=0.242). The time-to-MSL ratios were 7.2±4.8 and 3.8±1.8 min/mm in the first and last 50 cases, respectively (p<0.001). Five cases requiring auxiliary SWL were included in the first 50 cases, and the stone-free rate in the last 50 cases (94.0%) was higher than that in the first 50 cases (80.0%).
Fig. 2. The time-to-MSL ratio (min/mm). The estimated cut-off numbers of the time-to-MSL ratio below 5 min/mm was 50. MSL, maximal stone length; RIRS, retrograde intrarenal surgery.
The univariate logistic regression models revealed the following predictive factors of stone-free status following videoscopic RIRS: shorter MSL [odds ratio (OR): 0.906, 95% confidence interval (CI): 0.827–0.991; p=0.030), lower MSD (OR: 0.998, 95% CI: 0.996–0.999; p=0.007), and last 50 cases (OR: 3.917, 95% CI: 1.110–18.367; p=0.049). Multivariate analyses also demonstrated that a lower MSD (OR: 0.998, 95% CI: 0.996–0.999; p=0.047) and last 50 cases (OR: 5.408, 95% CI: 1.337−30.426; p=0.030) to be independent predictors of stone-free status after videoscopic RIRS (Table 2).
Table 2. Univariate and Multivariate Logistic Regression Model of Stone-Free Rate.
| Parameter | OR | 95% CI | p value |
|---|---|---|---|
| Univariate | |||
| Age | 0.986 | 0.943–1.028 | 0.515 |
| BMI | 1.029 | 0.861–1.234 | 0.754 |
| Sex | 0.364 | 0.054–1.470 | 0.207 |
| MSL | 0.906 | 0.827–0.991 | 0.030 |
| MSD | 0.998 | 0.996–0.999 | 0.007 |
| SSD | 1.013 | 0.986–1.043 | 0.347 |
| SHI | 0.995 | 0.990–1.000 | 0.052 |
| Last 50 cases (vs. first 50 cases) | 3.917 | 1.110–18.367 | 0.049 |
| Multivariate | |||
| MSL | 0.917 | 0.815–1.030 | 0.137 |
| MSD | 0.998 | 0.996–0.999 | 0.047 |
| Last 50 cases (vs. first 50 cases) | 5.408 | 1.337–30.426 | 0.030 |
BMI, body mass index; MSL, maximal stone length; MSD, mean stone density; SSD, skin-to-stone distance; SHI, stone heterogeneity index; OR: odds ratio, CI: confidence interval.
In Table 3, the logistic regression model showed factors related to lower time-to-MSL ratio (<5 min/mm). In the univariate model, lower BMI (OR: 0.869, 95% CI: 0.760−0.986; p=0.033) and last 50 cases (OR: 6.000, 95% CI: 2.522–15.260; p<0.001) were significant factors for lower time-to-MSL ratio. The multivariate model demonstrated that the last 50 cases was an independent factor for lower time-to-MSL ratio (OR: 5.591, 95% CI: 2.317−14.382; p<0.001).
Table 3. Univariate and Multivariate Logistic Regression Model of Lower Time-to-Maximal Stone Length Ratio (<5 min/mm).
| Parameter | OR | 95% CI | p value |
|---|---|---|---|
| Univariate | |||
| Age | 0.989 | 0.960–1.018 | 0.467 |
| BMI | 0.869 | 0.760–0.986 | 0.033 |
| Sex | 1.123 | 0.469–2.654 | 0.791 |
| MSD | 1.000 | 0.999–1.002 | 0.192 |
| SSD | 0.992 | 0.973–1.010 | 0.390 |
| SHI | 1.000 | 0.997–1.004 | 0.880 |
| Last 50 cases (vs. first 50 cases) | 6.000 | 2.522–15.260 | <0.001 |
| Multivariate | |||
| BMI | 0.891 | 0.772–1.021 | 0.100 |
| Last 50 cases (vs. first 50 cases) | 5.591 | 2.317–14.382 | <0.001 |
BMI, body mass index; MSD, mean stone density; SSD, skin-to-stone distance; SHI, stone heterogeneity index; OR: odds ratio, CI: confidence interval.
DISCUSSION
Recently, RIRS has become one of the most popular minimally invasive surgeries in urology. With its low morbidity and its use of a natural orifice, this technique is accepted as the first-line treatment for upper ureter and renal stones by both patients and surgeons.4 Experiences with RIRS have shown stone-free rates comparable to other therapeutic modalities, although with a lower risk of renal damage and bleeding.13,14 Moreover, many recent studies have reported that RIRS is used as the first-choice treatment for patients with renal stones requiring active treatment and provides a higher stone-free rate with low morbidity, a shorter hospital stay, better patient comfort, and a faster return to daily activities in cases of larger calculi.15 The European Association of Urology (EAU) Urolithiasis Guidelines recommend that RIRS can be performed if percutaneous nephrolithotomy or SWL is not possible for treatment of stones >2 cm. In addition, EAU Urolithiasis Guidelines state that digital videoscopes demonstrate shorter operation times due to their improved image quality.16
In 2010, Binbay, et al.17 compared the outcomes of patients who were treated using digital and fiber-optic flexible ureterorenoscopy for kidney stones. They performed RIRS using DUR-D (Gyrus ACMI, Olympus) and Flex-X2 (KARL STORZ) ureterorenoscopes, and reported on a total of 76 patients who were treated with either a fiber-optic flexible ureterorenoscopes (n=34; fiber-optic group) or digital flexible ureterorenoscopes (n=42; digital group). The operation time of RIRS was 46.5±13.4 min in the fiber-optic group, but only 38.3±17.4 min in the digital group (p=0.001). Mean fragmented stone area per minute was 2.43±0.81 mm2/min in the digital group and 1.96±0.80 mm2/min in the fiber-optic group (p=0.01). Somani, et al.18 also compared the outcomes of RIRS using digital and fiber-optic scopes for kidney stones using URF-V and URF-P5 flexible video uteroscopes (Olympus). They concluded that digital videoscopes significantly reduced the operative time, compared with fiber-optic videoscopes (53.8±15.2 min vs. 44.5±14.9 min; p<0.05). These authors reported the disadvantage that the digital videoscopes (DUR-D; 9.3 Fr and URF-V; 9.9 Fr) were thicker in diameter than fiber-optic ureteroscopes (Flex-X2; 7.5 Fr and URF-P5; 8.4 Fr). They concluded that the digital videoscope had less maneuverability, but could reduce the operation time. Two recently released digital videoscopes have smaller diameters (Flex-Xc; 8.5 Fr and URF-V2; 8.4 Fr), and the maneuverability of these scopes can surpass that of a fiber-optic ureteroscope.8 Multescu, et al.8 studied the durability and lifespan of three Flex-Xc videoscopes. The first videoscope was used in 96 procedures for a total of 67.1 hours. However, the second and third videoscopes were used in more procedures (151 and 159, respectively) and for longer times (107.7 h and 107.2 h, respectively). These results confirm the longer usage time of this type of videoscope, which also has improved durability and significantly improved visibility and image quality due to continuous technological development. The auauthors concluded that the use of a ureteral access sheath and avoidance of overstressing the deflection mechanism, by relocating lower pole stones, offers substantial advantages in prolonging the lifespan of these expensive instruments.8 This prolonged lifespan is important because the biggest disadvantage of the digital videoscopes, since the launch of Flex-Xc and URF-V2 with narrow diameters, is their high prices. In particular, the use of digital videoscopes in medical environments, such as those in Korea, has been very difficult because of limited medical resources. Until now, due to the high prices of digital videoscopes in Korea and developing countries, no relevant digital videoscope studies have been published. Therefore, this study is the first digital videoscopic RIRS study involving a Korean patient population.
In a notable study, Cho, et al.19 investigated the learning curve for surgeons using a fiber-optic scope (Flex-X2) for RIRS in patients with mid-sized stones. Statistical analysis of their RIRS learning experience results revealed that 56 cases were required to reach a plateau in the learning curve without a proper instructor. In our studies, the estimated cut-off numbers of the time-to-MSL ratio of <5 min/mm was 50 cases. Operation time in the last 50 cases (46.1±26.6 min) was also shorter than that in the first 50 cases (84.1±52.7 min, p<0.001). Five cases requiring auxiliary SWL occurred in the first 50 cases, and the stone-free rate in the last 50 cases (94.0%) was higher than that in the first 50 cases (80.0%). Considering these two studies, it is possible to deduce that more than 50 cases of experience using both a fiber-optic scope and a digital videoscope should be completed to overcome the learning curve. Furthermore, considering the high price of digital videoscopes, it would be most economical to implement RIRS with a digital videoscope for surgeons who have performed more than 50 cases requiring a fiber-optic ureteroscope. In our results, the factor related to lower time-to-MSL ratio (<5 min/mm) was also only the last 50 cases. In the early experiences, the accumulation of experience can be more important than the characteristics of the stone. There are several reasons why the MSL in the logistic regression model is not a factor affecting the stone-free rate. First, the MSL in the total patient population may not be as large as 13.1±6.2 mm. The EAU guidelines recommend that RIRS be performed for stones <2 cm in size. Therefore, it is possible that the MSL did not affect the stone-free rate because this study included patients with stones that were <2 cm in length. Another reason is that, unlike SWL,20 there is a subjective difference in an operator's ability to assess stone-free status according to the surgeon's proficiency. Therefore, we suggest that MSL may be identified as a significant factor affecting stone-free status if we analyze larger stones in future studies. Also, SHI was not a predicting factor for stone-free rate. SHI was previously shown to be a novel predictor of SWL success based on HU attenuation as the SD of HU.21 However, the reason why SHI was not a meaningful factor in our study can be explained by several hypotheses. First, like MSL, it is possible that SHI did not affect the stone-free rate because RIRS was performed on patients with stones that were <2 cm in most cases. Second, stone dusting and fragmentation using a Holmium laser may be able to break down stones more precisely than shock-waves from SWL, so SHI may be analyzed as an insignificant factor for stone-free rate. However, further studies are needed to analyze the factors affecting the stone-free rate of RIRS, which may help interpret the influence of MSL or SHI. In our study, 91 patients had pre-stenting before RIRS. Assimos, et al.22 demonstrated that preoperative ureteral stenting increases stone-free rates and decreases complications in patients with renal stones. In their study, for renal stone treatment, preoperative stent placement increased the stone-free rate, and there was a borderline significant decrease in intraoperative complications. Thus, we performed pre-stenting to increase stone-free rates and decrease complications.
This study has some inherent limitations due to its retrospective design, which may have introduced sampling bias. Nonetheless, this is the first report on digital videoscopic RIRS for the Korean population. The results of this study will be reinforced through continuous future research, which will provide new results that will be the basis for further development of digital videoscopes.
In summary, videoscopic RIRS resulted in a high stone-free rate of 87%, and 5% of the patients who received additional treatment after surgery. The estimated cut-off numbers of the time-to-MSL ratio below 5 mm/min was 50. Operation time in the last 50 cases was shorter than that in the first 50 cases. Low MSDs and last 50 cases were significant predictors of stone-free rate in videoscopic RIRS. To overcome the learning curve, a surgeon should perform an initial 50 cases of videoscopic RIRS.
ACKNOWLEDGEMENTS
This study was supported by a faculty research grant from the Yonsei University College of Medicine for 2016 (6-2016-0119).
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Kang DH, Cho KS, Ham WS, Chung DY, Kwon JK, Choi YD, et al. Ureteral stenting can be a negative predictor for successful outcome following shock wave lithotripsy in patients with ureteral stones. Investig Clin Urol. 2016;57:408–416. doi: 10.4111/icu.2016.57.6.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Teichman JM. Clinical practice. Acute renal colic from ureteral calculus. N Engl J Med. 2004;350:684–693. doi: 10.1056/NEJMcp030813. [DOI] [PubMed] [Google Scholar]
- 3.Kang SK, Cho KS, Kang DH, Jung HD, Kwon JK, Lee JY. Systematic review and meta-analysis to compare success rates of retrograde intrarenal surgery versus percutaneous nephrolithotomy for renal stones >2 cm: an update. Medicine. 2017;96:e9119. doi: 10.1097/MD.0000000000009119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xu Y, Min Z, Wan SP, Nie H, Duan G. Complications of retrograde intrarenal surgery classified by the modified Clavien grading system. Urolithiasis. 2017 doi: 10.1007/s00240-017-0961-6. [DOI] [PubMed] [Google Scholar]
- 5.Chang KD, Lee JY, Park SY, Kang DH, Lee HH, Cho KS. Impact of pretreatment hydronephrosis on the success rate of shock wave lithotripsy in patients with ureteral stone. Yonsei Med J. 2017;58:1000–1005. doi: 10.3349/ymj.2017.58.5.1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dale J, Kaplan AG, Radvak D, Shin R, Ackerman A, Chen T, et al. Evaluation of a novel single-use flexible ureteroscope. J Endourol. 2017 doi: 10.1089/end.2016.0237. [Epub] [DOI] [PubMed] [Google Scholar]
- 7.Zilberman DE, Lipkin ME, Ferrandino MN, Simmons WN, Mancini JG, Raymundo ME, et al. The digital flexible ureteroscope: in vitro assessment of optical characteristics. J Endourol. 2011;25:519–522. doi: 10.1089/end.2010.0206. [DOI] [PubMed] [Google Scholar]
- 8.Multescu R, Geavlete B, Georgescu D, Geavlete P. Improved durability of flex-Xc digital flexible ureteroscope: how long can you expect it to last? Urology. 2014;84:32–35. doi: 10.1016/j.urology.2014.01.021. [DOI] [PubMed] [Google Scholar]
- 9.Sakamoto S. Editorial Comment to Retrograde flexible ureteroscopic approach of upper urinary tract pathology: what is the status in 2014? Int J Urol. 2014;21:1085. doi: 10.1111/iju.12645. [DOI] [PubMed] [Google Scholar]
- 10.Chung DY, Cho KS, Lee DH, Han JH, Kang DH, Jung HD, et al. Impact of colic pain as a significant factor for predicting the stone free rate of one-session shock wave lithotripsy for treating ureter stones: a Bayesian logistic regression model analysis. PLoS One. 2015;10:e0123800. doi: 10.1371/journal.pone.0123800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee JY, Kim JH, Kang DH, Chung DY, Lee DH, Jung HD, et al. Stone heterogeneity index as the standard deviation of Hounsfield units: A novel predictor for shock-wave lithotripsy outcomes in ureter calculi. Sci Rep. 2016;6:23988. doi: 10.1038/srep23988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rizvi SAH, Hussain M, Askari SH, Hashmi A, Lal M, Zafar MN. Surgical outcomes of percutaneous nephrolithotomy in 3402 patients and results of stone analysis in 1559 patients. BJU Int. 2017;120:702–709. doi: 10.1111/bju.13848. [DOI] [PubMed] [Google Scholar]
- 13.Ramón de, García-Tello A, Andrés G, Redondo C, Meilán E, Gimbernat H, et al. Comparative study of retrograde intrarenal surgery and micropercutaneous nephrolithotomy in the treatment of intermediate-sized kidney stones. Actas Urol Esp. 2014;38:576–583. doi: 10.1016/j.acuro.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 14.Gao X, Peng Y, Shi X, Li L, Zhou T, Xu B, et al. Safety and efficacy of retrograde intrarenal surgery for renal stones in patients with a solitary kidney: a single-center experience. J Endourol. 2014;28:1290–1294. doi: 10.1089/end.2014.0295. [DOI] [PubMed] [Google Scholar]
- 15.Baş O, Tuygun C, Dede O, Sarı S, Çakıcı MÇ, Öztürk U, et al. Factors affecting complication rates of retrograde flexible ureterorenoscopy: analysis of 1571 procedures-a single-center experience. World J Urol. 2017;35:819–826. doi: 10.1007/s00345-016-1930-3. [DOI] [PubMed] [Google Scholar]
- 16.Türk C, Petřík A, Sarica K, Seitz C, Skolarikos A, Straub M, et al. EAU guidelines on interventional treatment for urolithiasis. Eur Urol. 2016;69:475–482. doi: 10.1016/j.eururo.2015.07.041. [DOI] [PubMed] [Google Scholar]
- 17.Binbay M, Yuruk E, Akman T, Ozgor F, Seyrek M, Ozkuvanci U, et al. Is there a difference in outcomes between digital and fiberoptic flexible ureterorenoscopy procedures? J Endourol. 2010;24:1929–1934. doi: 10.1089/end.2010.0211. [DOI] [PubMed] [Google Scholar]
- 18.Somani BK, Al-Qahtani SM, de Medina SD, Traxer O. Outcomes of flexible ureterorenoscopy and laser fragmentation for renal stones: comparison between digital and conventional ureteroscope. Urology. 2013;82:1017–1019. doi: 10.1016/j.urology.2013.07.017. [DOI] [PubMed] [Google Scholar]
- 19.Cho SY, Choo MS, Jung JH, Jeong CW, Oh S, Lee SB, et al. Cumulative sum analysis for experiences of a single-session retrograde intrarenal stone surgery and analysis of predictors for stone-free status. PLoS One. 2014;9:e84878. doi: 10.1371/journal.pone.0084878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cho KS, Jung HD, Ham WS, Chung DY, Kang YJ, Jang WS, et al. Optimal skin-to-stone distance is a positive predictor for successful outcomes in upper ureter calculi following extracorporeal shock wave lithotripsy: a Bayesian model averaging approach. PLoS One. 2015;10:e0144912. doi: 10.1371/journal.pone.0144912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abdelhamid M, Mosharafa AA, Ibrahim H, Selim HM, Hamed M, Elghoneimy MN, et al. A prospective evaluation of high-resolution CT parameters in predicting extracorporeal shockwave lithotripsy success for upper urinary tract calculi. J Endourol. 2016;30:1227–1232. doi: 10.1089/end.2016.0364. [DOI] [PubMed] [Google Scholar]
- 22.Assimos D, Crisci A, Culkin D, Xue W, Roelofs A, Duvdevani M, et al. Preoperative JJ stent placement in ureteric and renal stone treatment: results from the Clinical Research Office of Endourological Society (CROES) Ureteroscopy (URS) Global Study. BJU Int. 2016;117:648–654. doi: 10.1111/bju.13250. [DOI] [PubMed] [Google Scholar]



