Abstract
Objective
The Japan Society of Gynecologic Oncology (JSGO) initiated a nation-wide training system for the education and certification for gynecologic oncologists in 2005. To assess the impact of the quality of the JSGO-accredited institutions, JSGO undertook an analysis of the Uterine Cervical Cancer Registry of the Japan Society of Obstetrics and Gynecology (JSOG) to determine the effectiveness of the JSGO-accredited institutions on the treatment and survival of women with cervical cancer.
Methods
The effectiveness of 119 JSGO-accredited institutions and 125 non-JSGO-accredited institutions on the treatment and survival of women with cervical cancer were compared by analyzing the tumor characteristics, treatment patterns, and survival outcomes of women with stage T1B–T4 cervical cancer utilizing the data in the JSOG nation-wide registry for cervical cancer (2006–2009).
Results
A total of 14,185 eligible women were identified: 10,920 (77.0%) cases for 119 JSGO-accredited institutions and 3,265 (23.0%) cases for 125 non-accredited institutions. A multivariate analysis showed that age, stage, histology type, and treatment pattern were independently associated with mortality. Moreover, women who received treatment at the JSGO-accredited institutions had a significantly decreased mortality risk compared to non-accredited institutions (adjusted hazard ratio [aHR]=0.843; 95% confidence interval [CI]=0.784–0.905). Similar findings on multivariate analysis were seen among subset of women who received surgery alone (aHR=0.552; 95% CI=0.393–0.775) and among women who received radiotherapy (aHR=0.845; 95% CI=0.766–0.931).
Conclusion
Successful implementation of gynecologic oncology accrediting institution was associated with improved survival outcome of women with cervical cancer in Japan.
Keywords: Uterine Cervical Neoplasms; General Surgery; Surgical Procedures, Operative; Gyenecologic Oncologist; Specialization; Fellowship Training
INTRODUCTION
Cervical cancers have high morbidity and mortality among the gynecologic malignant tumors in Japan. For the diagnosis and treatment of these cancers, it is important to know their characteristics, such as prevalence, stages, treatment methods, and survival rates. The morbidity of cervical cancer in Japan ranged from 9,000 to 11,000 women in the 1970s, decreased to 7,000–8,000 women in the 1990s, and increased to 10,908 women in 2012 [1]. For the changes in cervical cancer from 2005 to 2014, the cancer stages I and IV increased, whereas stages II and III decreased in prevalence. Squamous cell carcinoma (SCC) was the main histological type, but adenocarcinoma and neuroendocrine tumors appear to be on the increase [1].
Apart from understanding the tumor biology and epidemiology, the quality and type of patient treatment needs continual reassessment because it is amenable to direct influence and success in regard to the outcome of the disease. In this regard, the physician's specialization and experience and the institutional infrastructure, national training, guidelines, and education programs contribute markedly to the diversity of the treatment results and patient's survival. The treatment guidelines for cervical cancer in Japan recommend the complete surgical resection of cervical cancer and a combination of surgery and adjuvant radiotherapy or adjuvant chemotherapy if required [2,3,4]. Several studies have indicated that the survival of women with gynecologic cancers improve when surgically operated on by gynecologic oncologists rather than gynecologists or general surgeons [5,6,7]. Furthermore, studies have shown that successful surgery was more likely to be performed in teaching hospitals than nonteaching hospitals, and that the survival rate was better for patients treated in teaching or specialist hospitals compared with nonteaching hospitals [8,9,10,11].
Gynecologic oncologists spend a considerable amount of time learning and gaining specific surgical skills such as radical hysterectomies that are essential in the management of gynecological malignancies and in the improved survival rates of cervical cancer patients [6,7]. Sub-specialty training in gynecologic oncology, the care and treatment of women with gynecological cancers, was established in Japan in 1998 with the formation of the Japan Society of Gynecologic Oncology (JSGO) [12]. This society had its origin in the Japan Colposcopy Association, which was founded in August 1975. JSGO currently consists of gynecologists, pathologists, and radiologists totaling well over 3,000 in number, making it the largest Japanese organization conducting research on diagnosis and treatment of gynecologic tumors [12]. More than 2,000 doctors participated in the 2017 annual congress of JSGO in Kumamoto. In 2016, American Society of Clinical Oncology (ASCO) Resource-Stratified Clinical Practice Guideline cited the JSGO 2nd Edition Guidelines of 2011 for cervical cancer as a reference for correct medical practices along with the guidelines of the Canadian Cancer Care Ontario, European Society of Medical Oncology, US National Comprehensive Cancer Network, and the World Health Organization [13,14]. The 2011 guidelines for cervical cancer and other cancers have been continually updated by JSGO [4,15].
JSGO initiated a nation-wide training system for the education and certification for gynecologic oncologists in the diagnosis and treatment of gynecologic tumors in 2005 [16], and 119 hospitals were accredited by JSGO for gynecologic oncology training program in 2006 after meeting a number of recommended criteria such as clinical membership, experience, volume of surgical procedures, qualified managements, registries, board members and specialists, clinical trials, and multidisciplinary resources. In order to assess the quality of the accredited training institutions, the JSGO undertook a survey of the outcome of the survival of women treated for cervical cancer based on the Uterine Cervical Cancer Registry of JSOG. By utilizing the JSOG nation-wide registry for cervical cancer (2006–2009), tumor characteristics, treatment patterns, and survival outcomes of women with stage T1B–T4 cervical cancer were compared based on the JSGO accrediting status. A total of 14,185 eligible women were identified with 10,920 (77.0%) cases for JSGO-accredited institutions and 3,265 (23.0%) cases for non-accredited institutions. Here, we report on the results of our univariate and multivariate analyses undertaken on the survey data to examine the factors associated with survival of women with cervical cancer and their mortality due to age, stage of malignancy, histology type, and treatment pattern.
MATERIALS AND METHODS
1. Medical institutions accredited for gynecologic oncology training programs by JSGO
A total of 119 Japanese teaching and non-teaching institutions were accredited by JSGO for gynecologic oncology training programs in 2005 and 2006 and each institution had fulfilled the following criteria:
1) Appropriate medical facilities include having trained staff and infrastructure operating theatres and radiology, and patient preparatory and after care.
2) The diagnosis and treatment of >40 gynecologic malignancies per year.
3) At least 1 institution board member was a certified gynecologic oncologist.
4) A board-certified radiation oncologist and pathologist were available at the institution.
5) An organized tumor board.
6) Training opportunity for intestinal and urological surgery.
7) Multidisciplinary resources available.
8) An organized institutional review board (IRB).
9) Performance of clinical trials.
10) JSOG-accredited hospital and tumor registry.
11) The publication of an annual report.
To qualify as a JSGO certified gynecologic oncologist, the JSGO requires certification of the physician by the Japanese Board of Cancer Therapy, JSGO membership, treatment of ≥150 invasive cancer cases over 3–5 years, experience of ≥100 operations over 3–5 years, and the performance of ≥30 operations, including 15 radical hysterectomies over 3–5 years.
2. Selection criteria for survey of cervical cancer cases, treatment, and survival data
Investigators reviewed the medical records of the Cervical Cancer Registry that is maintained by Gynecologic Oncology Committee of the Japan Society of Obstetrics and Gynecology (JSOG) and found that 17,576 women were diagnosed with cervical cancer during a 4-year period, 2006–2009. Of these women, survival data was unknown for 3,391 women (19.3%) and they were omitted from the study. The clinical and demographic characteristics of the patients who were treated in non-JSGO-accredited institutions vs. JSGO-accredited institutions are shown in Table 1. The accredited institutions were matched for the year of diagnosis (2006–2009), a 10-year-age of patient, TNM staging system for cervical cancer (classified according to the TNM system into primary tumors T, regional lymph nodes N, and distant metastasis M categories, para-aortic lymph nodes [PANs] metastasis, and unclear), histology (SCC, adenocarcinoma and others), and first treatment as surgery, radiation or chemotherapy. Of the total of 14,185 women with survival data, non-JSGO-accredited institutions treated 3,265 (23.0%) cancer cases, and JSGO-accredited institutions treated 10,920 (77.0%) cancer cases. The number of deaths was 1,022 (31.3%) for the non-JSGO-accredited institutions and 2,911 (26.7%) for the JSGO-accredited institutions.
Table 1. Clinical and demographic characteristics of the cohort comparing between patients treated in non-JSGO-accredited institutions and JSGO-accredited institutions.
| Characteristics | Treated in non-JSGO-accredited institutions (n=3,265) | Treated in JSGO-accredited institutions (n=10,920) | p-value | ||
|---|---|---|---|---|---|
| Year of diagnosis | <0.001 | ||||
| 2006 | 878 (26.8) | 2,317 (21.2) | |||
| 2007 | 738 (22.6) | 2,550 (23.4) | |||
| 2008 | 878 (26.8) | 2,750 (25.2) | |||
| 2009 | 777 (23.8) | 3,303 (30.2) | |||
| Age (yr) | <0.001 | ||||
| ≤40 | 624 (19.1) | 2,683 (24.6) | |||
| ≤50 | 696 (21.3) | 2,428 (22.2) | |||
| ≤60 | 781 (23.9) | 2,503 (22.9) | |||
| ≤70 | 589 (18.0) | 1,827 (16.7) | |||
| >70 | 575 (17.6) | 1,479 (13.5) | |||
| Tumor stage | |||||
| T categories | <0.001 | ||||
| T1B | 1,455 (44.6) | 5,238 (48.0) | |||
| T2 | 982 (30.1) | 3,091 (28.3) | |||
| T3 | 586 (17.9) | 1,956 (17.9) | |||
| T4 | 242 (7.4) | 634 (5.8) | |||
| N categories | 0.021 | ||||
| N0 | 2,436 (74.6) | 7,932 (72.6) | |||
| N1 | 829 (25.4) | 2,997 (27.4) | |||
| M categories | 0.057 | ||||
| M0 | 2,952 (90.4) | 9,791 (89.7) | |||
| M1 | 180 (5.5) | 564 (5.2) | |||
| PAN metastasis | 124 (3.8) | 537 (4.9) | - | ||
| Unclear | 9 (0.3) | 28 (0.3) | - | ||
| Histology | 0.001 | ||||
| SCC | 2,377 (72.8) | 7,754 (71.0) | |||
| Adenocarcinoma | 661 (20.2) | 2,170 (19.9) | |||
| Others | 227 (7.0) | 996 (9.1) | |||
| 1st treatment | 0.004 | ||||
| Surgery | 1,628 (49.9) | 5,607 (51.3) | |||
| Radiation | 1,139 (34.9) | 3,916 (35.9) | |||
| Chemo | 481 (14.7) | 1,347 (12.3) | |||
| Others | 17 (0.5) | 50 (0.5) | |||
Values are presented as number of patients (%).
JSGO, Japan Society of Gynecologic Oncology; M, metastasis; N, node; PAN, para-aortic lymph node; SCC, squamous cell carcinoma; T, tumor.
3. Statistical analysis
All statistical analyses were done in Statistical Package for Social Sciences version 11.01 (SPSS Inc., Chicago, IL, USA). Pearson χ2 test was used in univariate analyses, whereas Mann-Whitney U test was used for continuous variables (mean, median). Kaplan-Meier survival curves were computed and tested statistically by the log-rank test. p-values of equal to or less than 0.05 were considered to be statistically significant. Survival is presented as overall median survival and 5-year survival rates. The Cox proportional hazard models were applied for estimation of prognostic factors of survival. The study was approved by the Ethics Committee of Tokai University (IRB registration No. 15R-101).
RESULTS
Table 1 shows the clinical and demographic characteristics of patients who were treated in non-JSGO-accredited institutions vs. those treated in JSGO-accredited institutions. There were significant differences in the distribution of patients between the 2 groups related to the year of diagnosis, patient's age, tumor (T), node (N), and metastasis (M) categories, histology, and treatment patterns. There was no significant difference (p=0.057) between the 2 groups for the M category of the tumor stage. Most women (30.2%) at the JSGO-accredited institutions were treated in the year 2009, whereas the largest number of women (26.8%) treated at the non JSGO-accredited institutions was in the years 2006 and 2008. Most women (24.6%) diagnosed and treated for cervical cancer at the JSGO-accredited institutions were 40 years of age or less. The fewest women treated at either the accredited or non-accredited institutions were greater than 70 years of age. The most abundant tumors were T1B (cervical carcinoma confined to the cervix) in the T category, N0 (no regional lymph node metastasis) in the N category and M0 (no distant metastasis) in the M category. SCC at 72.8% for non-JSGO and 71% for JSGO was the most common histological finding for the tumor types. Surgery was the preferred first treatment (51.3% and 49.9% for JSGO and non-JSGO, respectively) followed by radiation, chemotherapy and then the ‘others’ category as shown in Table 1.
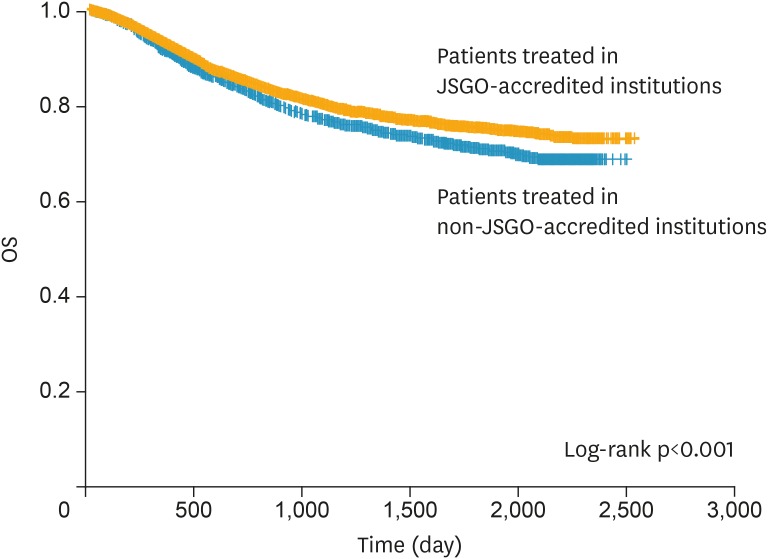
Fig. 1 shows the overall survival of cervical cancer women according to JSGO-accredited status with a significant difference (log-rank, p<0.001) in survival rate between patients treated in JSGO-accredited institutions (73.3%) and non-JSGO-accredited institutions (68.7%) after 2,500 days.
Fig. 1.
Kaplan-Meier survival curve of patients with cervical cancer by treating hospitals, JSGO- accredited institutions (yellow line) and non-JSGO-accredited institutions (blue line). The OS of cervical cancer women (log-rank, p<0.001) was 73.3% for patients treated in JSGO-accredited institutions and 68.7% for patients treated in non-JSGO-accredited institutions after 2,500 days.
JSGO, Japan Society of Gynecologic Oncology; OS, overall survival.
Table 2 shows the univariate models of prognostic factors for the overall survival of women calculated as a 5-year rate (%). Patients treated in JSGO-accredited institutions had a significantly (p<0.001) longer survival rate than patients treated in non JSGO-accredited institutions. The age of the patient in terms of 5-year survival rate was best (81.4%) for women 40 years of age or less, and worst (54.7%) for women over 70 years of age. The prognosis was markedly better for women with the lower T categories (89.3% for T1) than for T4 where the 5-year survival rate was 24.7%. Similarly, N1, M1, and PAN metastasis categories resulted in poor prognosis, the lowest 5-year survival rate of 12.8% was in women diagnosed with M1, distant metastasis (peritoneal spread, PAN, lung, liver, or bone). Surgery as first treatment had a better prognosis (87.6%) than radiation (57.8%), chemotherapy (55.9%), or other treatments (44.6%).
Table 2. Univariate models of prognostic factors.
| Factors | No. (%) | Overall survival | ||
|---|---|---|---|---|
| 5-year rate (%) | p-value | |||
| Age (yr) | <0.001 | |||
| ≤40 | 3,307 (23.3) | 81.4 | ||
| ≤50 | 3,241 (22.0) | 76.1 | ||
| ≤60 | 3,284 (23.2) | 70.5 | ||
| ≤70 | 2,416 (17.0) | 70.9 | ||
| >70 | 2,054 (14.5) | 54.7 | ||
| T categories | <0.001 | |||
| T1B | 6,694 (47.2) | 89.3 | ||
| T2 | 4,073 (28.7) | 71.7 | ||
| T3 | 2,542 (17.9) | 47.1 | ||
| T4 | 876 (6.2) | 24.7 | ||
| N categories | <0.001 | |||
| N0 | 10,359 (73.0) | 84.6 | ||
| N1 | 3,826 (27.0) | 53.1 | ||
| M categories | <0.001 | |||
| M0 | 12,743 (89.8) | 78.1 | ||
| M1 | 744 (5.2) | 12.8 | ||
| PAN metastasis | 661 (4.7) | 38.7 | ||
| Unclear | 37 (0.3) | 53.4 | ||
| Histology | <0.001 | |||
| SCC | 10,131 (71.4) | 73.9 | ||
| Adenocarcinoma | 2,831 (20.0) | 71.4 | ||
| Others | 1,223 (8.6) | 66.6 | ||
| 1st treatment | <0.001 | |||
| Surgery | 7,235 (51.0) | 87.6 | ||
| Radiation | 5,055 (35.6) | 57.8 | ||
| Chemo | 1,828 (12.9) | 55.9 | ||
| Others | 67 (0.5) | 44.6 | ||
| Institutions | <0.001 | |||
| Non-JSGO-accredited | 3,256 (23.0) | 69.0 | ||
| JSGO-accredited | 10,920 (77.0) | 73.9 | ||
JSGO, Japan Society of Gynecologic Oncology; M, metastasis; N, node; PAN, para-aortic lymph node; SCC, squamous cell carcinoma; T, tumor.
Table 3 shows the analysis of the multivariate models of prognostic factors. After simultaneous adjustment for all seven prognostic factors, patients treated in JSGO-accredited institutions still had significantly longer survival rate than patients treated in non-JSGO-accredited institutions. Also, the multivariate model confirmed the findings of the univariate analysis that the age of the patient in terms of 5-year survival rate was worst for women over 70 years of age, the prognosis was markedly worse for women with the higher T categories, N1, M1, and PAN metastasis categories, and that surgery as first treatment had a significantly (p<0.001) better prognosis than radiation, chemotherapy, or other treatments.
Table 3. Multivariate models of prognostic factors.
| Factors | aHR* of overall survival (95% CI) | p-value | |
|---|---|---|---|
| Age (yr) | |||
| ≤40 | Reference | ||
| ≤50 | 0.945 (0.848–1.054) | 0.310 | |
| ≤60 | 0.898 (0.808–0.998) | 0.046 | |
| ≤70 | 0.868 (0.775–0.973) | 0.015 | |
| >70 | 1.489 (1.331–1.665) | <0.001 | |
| T categories | |||
| T1B | Reference | ||
| T2 | 2.116 (1.905–2.351) | <0.001 | |
| T3 | 3.448 (3.053–3.894) | <0.001 | |
| T4 | 4.400 (3.822–5.065) | <0.001 | |
| N categories | |||
| N0 | Reference | ||
| N1 | 1.733 (1.607–1.868) | <0.001 | |
| M categories | |||
| M0 | Reference | ||
| M1† | 2.884 (2.593–3.208) | <0.001 | |
| PAN metastasis | 1.684 (1.506–1.882) | <0.001 | |
| Unclear | 1.655 (1.026–2.688) | 0.039 | |
| Histology | |||
| SCC | Reference | ||
| Adenocarcinoma | 1.928 (1.776–2.094) | <0.001 | |
| Others | 1.869 (1.681–2.077) | <0.001 | |
| 1st treatment | |||
| Surgery | Reference | ||
| Radiation | 1.636 (1.471–1.820) | <0.001 | |
| Chemo | 1.720 (1.538–1.924) | <0.001 | |
| Others | 2.544 (1.831–3.535) | <0.001 | |
| Hospitals | |||
| Non-JSGO-accredited | Reference | ||
| JSGO-accredited | 0.843 (0.784–0.905) | <0.001 | |
aHR, adjusted hazard ratio; CI, confidence interval; HR, hazard ratio; JSGO, Japan Society of Gynecologic Oncology; M, metastasis; N, node; PAN, para-aortic lymph node; SCC, squamous cell carcinoma; T, tumor.
*HRs are adjusted for all variables in the table; †without PAN metastasis.
Table 4 shows the univariate models of prognosis factors in the subgroup of women who received surgery alone. Patients treated in JSGO-accredited institutions also had significantly (p=0.001) longer survival rate (96.2%) than patients treated in non-JSGO-accredited institutions (93.5%). In addition, the 5-year rate (%) was poorest for women over 70 years of age (84%), with T2 tumor category (88.4%), N1 category (79.5%) and the metastasis category of M1 (84.4%). Table 5 shows the multivariate models of prognostic factors among the subset of women who received surgery alone, and this analysis confirms that women who received surgery alone at the JSGO-accredited institutions had a significantly decreased mortality risk compared to non-accredited institutions (adjusted hazard ratio [aHR]=0.552; 95% confidence interval [CI]=0.393–0.775), and the results were consistent with the findings shown in Table 4 (Supplementary Fig. 1).
Table 4. Univariate models of prognostic factors among subset of women who received surgery alone (n=3,407).
| Factors | No. (%) | Overall survival | ||
|---|---|---|---|---|
| 5-year rate (%) | p-value | |||
| Age (yr) | <0.001 | |||
| ≤40 | 1,724 (37.4) | 96.4 | ||
| ≤50 | 945 (27.7) | 96.3 | ||
| ≤60 | 653 (19.2) | 94.5 | ||
| ≤70 | 389 (11.4) | 96.4 | ||
| >70 | 146 (4.3) | 84.0 | ||
| T categories | <0.001 | |||
| T1B | 3,063 (89.9) | 96.5 | ||
| T2 | 342 (10.0) | 88.4 | ||
| N categories | <0.001 | |||
| N0 | 3,303 (96.9) | 96.1 | ||
| N1 | 104 (3.1) | 79.5 | ||
| M categories | <0.001 | |||
| M0 | 3,384 (90.6) | 95.7 | ||
| M1 | 22 (0.7) | 84.4 | ||
| Histology | <0.001 | |||
| SCC | 2,067 (60.7) | 96.7 | ||
| Adenocarcinoma | 1,044 (30.6) | 94.6 | ||
| Others | 296 (8.6) | 92.0 | ||
| Institutions | 0.001 | |||
| Non-JSGO-accredited | 766 (22.5) | 93.5 | ||
| JSGO-accredited | 2,641 (77.5) | 96.2 | ||
JSGO, Japan Society of Gynecologic Oncology; M, metastasis; N, node; SCC, squamous cell carcinoma; T, tumor.
Table 5. Multivariate models of prognostic factors among subset of women who received surgery alone (n=3,407).
| Factors | aHR* of overall survival (95% CI) | p-value | |
|---|---|---|---|
| Age (yr) | |||
| ≤40 | Reference | ||
| ≤50 | 0.978 (0.628–1.522) | 0.920 | |
| ≤60 | 1.368 (0.878–2.129) | 0.166 | |
| ≤70 | 0.807 (0.440–1.483) | 0.490 | |
| >70 | 3.116 (1.836–5.289) | <0.001 | |
| T categories | |||
| T1B | Reference | ||
| T2 | 3.074 (2.089–4.522) | <0.001 | |
| N categories | |||
| N0 | Reference | ||
| N1 | 4.170 (2.569–6.767) | <0.001 | |
| M categories | |||
| M0 | Reference | ||
| M1 | 3.825 (1.203–12.456) | <0.001 | |
| Histology | |||
| SCC | Reference | ||
| Adenocarcinoma | 1.997 (1.401–2.849) | <0.001 | |
| Others | 3.076 (1.957–4.846) | <0.001 | |
| Institutions | |||
| Non-JSGO-accredited | Reference | ||
| JSGO-accredited | 0.552 (0.393–0.775) | 0.004 | |
aHR, adjusted-hazard ratio; CI, confidence interval; HR, hazard ratio; JSGO, Japan Society of Gynecologic Oncology; M, metastasis; N, node; SCC, squamous cell carcinoma; T, tumor.
*HRs are adjusted for all variables in the table.
DISCUSSION
Our retrospective study suggests that the successful implementation of a gynecologic oncology accredited medical institution was associated with improved survival outcome of women with cervical cancer in Japan. The women 40 years or younger have a higher prevalence of early stage cancer, whereas women over 70 years of age have a higher prevalence of late stage cancer, metastasis and significantly poorer prognosis. Patients who underwent surgery as the primary treatment accounted for 63% to 65% of patients and had a significantly better prognosis than patients who underwent radiotherapy or chemotherapy as the primary form of treatment. Our findings conform to others in Japan [1] and to those in various other countries [5].
Both the univariate and the multivariate models of prognosis factors in the subgroup of women who received surgery alone showed that patients treated in JSGO-accredited institutions had significantly decreased mortality risk and longer survival rate than patients treated in non-JSGO-accredited institutions. This is likely due to the experience of the surgeons and the role of highly qualified gynecologic oncologists as well as the strict practical monitoring and treatment criteria applied to the JSGO-accredited institutions [6,7]. To qualify as a JSGO certified gynecologic oncologist, the physician, gynecologist or surgeon is required to treat at least 150 invasive cancer cases over 3–5 years, participate in at least 100 operations over 3–5 years, and perform more than 30 operations including 15 radical hysterectomies over 3–5 years. Radical hysterectomy that was developed for invasive cancer from the Okabayashi method in 1921 [17] is still widely performed in Japan [2,3,4], and a high level of experience in this procedure is considered important for a certified JSGO gynecologic oncologist. Although a critical volume of work to sustain surgical expertise and improve survival is a controversial issue, a number of studies have indicated that considerable experience and training is required to perform infrequent and complicated radical surgery for gynecological cancers, and that this is best met by gynecologic oncologists in teaching hospitals and appropriately accredited institutions [5,6,7,8] such as those accredited by JSGO.
Our retrospective study reports on cervical cancer diagnosis, treatment and survival data from about 8 to 11 years ago (2006–2009). Although the mortality of cervical cancer has remained relatively flat during the past 20 years, the morbidity of cervical cancer in Japan has increased by 46.4% from 7,500 women in the 1990s to 10,908 women in 2012 [1]. Clearly, to determine whether the effect of JSOG training and influence remains on track or should be improved, a more recent study is now needed to compare to the data that we have analyzed and presented here for 2006 to 2009. In this regard, our study forms the baseline for continued future studies on the impact of hospital accreditation by qualified gynecologic oncologists on the treatment and survival of women with cervical cancer. Furthermore, we propose to examine and stratify the quality of individual gynecologic oncologists in Japan in future studies to better assess whether accreditation or physician factors affect the treatment and survival of women with cervical cancer.
There are 3 cancer statistical registries in Japan, the population-based cancer registry maintained by the national Cancer Center Japan, the organ-based cancer registry for gynecologic malignancy maintained by the gynecologic tumor committee of JSOG, and the hospital-based cancer registry maintained by a cooperation of 633 hospitals [1]. In our study, we used the organ-based cancer registry for gynecologic malignancy maintained by the gynecologic tumor committee of the JSOG. One of the advantages of this registry over the other 2 is that it maintains clinicopathological data (including age, clinical stage, postsurgical stage, histological type) as well as treatment and survival data that could be retrieved for analysis of the effect of JSGO-accredited institutions vs. the non-JSOG-accredited institutions. In addition, the gynecologic tumor committee of JSOG has published annual reports on the patients who started treatment in 2005, 2008, 2010, and 2014 [18,19,20,21]. The population-based cancer registry maintained by the National Cancer Center Japan, although valuable for population-based studies, does not have the same level of clinical and treatment detail on JSGO-accredited institutions as the organ-based cancer registry of the JSOG. However, future analyses should incorporate the hospital-based cancer registry because 633 institutions and approximately 80% of all cancer patients participated in this registry in 2012 [1]. While trained staff are in charge of these registries, in future, a greater degree of certified gynecologic oncologists should be encouraged to be involved with the hospital-based cancer registry and improve the survival of the patients with gynecologic malignancies. Because clear incentives have not been offered to oncologists in accordance with their efforts reported here, securing incentives should be discussed and developed to maintain oncologists' motivation.
In conclusion, while the gynecologic oncology training program by JSOG since 2006 is on track and has successfully implemented the diagnosis, management and treatment of gynecological cancers following standardized criteria, there is still room for improvement, particularly in recruiting more gynecological oncologists and changing the emerging restrictions on their registration, particularly on their requirement to perform an exceedingly high number of radical abdominal hysterectomies for cancer of the cervix uteri prior to their registration.
Footnotes
Presentation: Parts of this paper were presented at the Annual Meeting on Women's Cancer 2017, National Harbor, MD, USA, March 12–15, 2017.
Funding: This work was supported in part by a grant-in-aid for scientific research from Ministry of Education, Culture, Sports, Science and Technology (No. 17H04340).
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
- Conceptualization: M.M., K.H., K.J., A.D., Y.N.
- Data curation: M.M., S.M., S.T.
- Formal analysis: M.M., S.M., S.T.
- Methodology: M.S., S.T.
- Project administration: M.M.
- Supervision: M.M.
- Writing - original draft: M.M.
- Writing - review & editing: S.M., S.T., K.H., K.J., A.D., Y.N.
SUPPLEMENTARY MATERIAL
Kaplan-Meier survival curve of patients with cervical cancer among subset of women who received surgery alone (n=3,407) by treating hospitals, JSGO-accredited institutions (yellow line) and non-JSGO-accredited institutions (blue line). The OS of cervical cancer women (log-rank, p<0.001) was 96.2% for patients treated in JSGO-accredited institutions and 93.5% for patients treated in non-JSGO-accredited institutions after 2,500 days.
References
- 1.Yamagami W, Nagase S, Takahashi F, Ino K, Hachisuga T, Aoki D, et al. Clinical statistics of gynecologic cancers in Japan. J Gynecol Oncol. 2017;28:e32. doi: 10.3802/jgo.2017.28.e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nagase S, Inoue Y, Umesaki N, Aoki D, Ueda M, Sakamoto H, et al. Evidence-based guidelines for treatment of cervical cancer in Japan: Japan Society of Gynecologic Oncology (JSGO) 2007 edition. Int J Clin Oncol. 2010;15:117–124. doi: 10.1007/s10147-010-0061-x. [DOI] [PubMed] [Google Scholar]
- 3.Ebina Y, Yaegashi N, Katabuchi H, Nagase S, Udagawa Y, Hachisuga T, et al. Japan Society of Gynecologic Oncology guidelines 2011 for the treatment of uterine cervical cancer. Int J Clin Oncol. 2015;20:240–248. doi: 10.1007/s10147-015-0806-7. [DOI] [PubMed] [Google Scholar]
- 4.Ebina Y, Katabuchi H, Mikami M, Nagase S, Yaegashi N, Udagawa Y, et al. Japan Society of Gynecologic Oncology guidelines 2013 for the treatment of uterine body neoplasms. Int J Clin Oncol. 2016;21:419–434. doi: 10.1007/s10147-016-0981-1. [DOI] [PubMed] [Google Scholar]
- 5.du Bois A, Rochon J, Pfisterer J, Hoskins WJ. Variations in institutional infrastructure, physician specialization and experience, and outcome in ovarian cancer: a systematic review. Gynecol Oncol. 2009;112:422–436. doi: 10.1016/j.ygyno.2008.09.036. [DOI] [PubMed] [Google Scholar]
- 6.Minig L, Padilla-Iserte P, Zorrero C. The relevance of gynecologic oncologists to provide high-quality of care to women with gynecological cancer. Front Oncol. 2016;5:308. doi: 10.3389/fonc.2015.00308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu MF, Li J, Lu HW, Wang LJ, Zhang BZ, Lin ZQ. Impact of the care provided by gynecologic oncologists on outcomes of cervical cancer patients treated with radical hysterectomy. Onco Targets Ther. 2016;9:1361–1370. doi: 10.2147/OTT.S99874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tingulstad S, Skjeldestad FE, Hagen B. The effect of centralization of primary surgery on survival in ovarian cancer patients. Obstet Gynecol. 2003;102:499–505. doi: 10.1016/s0029-7844(03)00579-9. [DOI] [PubMed] [Google Scholar]
- 9.Mowat A, Maher C, Ballard E. Surgical outcomes for low-volume vs high-volume surgeons in gynecology surgery: a systematic review and meta-analysis. Am J Obstet Gynecol. 2016;215:21–33. doi: 10.1016/j.ajog.2016.02.048. [DOI] [PubMed] [Google Scholar]
- 10.Paulsen T, Kjaerheim K, Kaern J, Tretli S, Tropé C. Improved short-term survival for advanced ovarian, tubal, and peritoneal cancer patients operated at teaching hospitals. Int J Gynecol Cancer. 2006;16(Suppl 1):11–17. doi: 10.1111/j.1525-1438.2006.00319.x. [DOI] [PubMed] [Google Scholar]
- 11.Kumpulainen S, Sankila R, Leminen A, Kuoppala T, Komulainen M, Puistola U, et al. The effect of hospital operative volume, residual tumor and first-line chemotherapy on survival of ovarian cancer - a prospective nation-wide study in Finland. Gynecol Oncol. 2009;115:199–203. doi: 10.1016/j.ygyno.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 12.Japan Society of Gynecologic Oncology [Internet] Tokyo: Japan Society of Gynecologic Oncology; 2015. [cited 2017 July 1]. Available from: https://www.jsgo.or.jp/en/index.html. [Google Scholar]
- 13.American Society of Clinical Oncology. Resource-stratified clinical practice guideline [Internet] Alexandria, VA: American Society of Clinical Oncology; 2016. [cited 2017 July 1]. Available from: http://www.asco.org/practice-guidelines/quality-guidelines/guidelines/resource-stratified. [Google Scholar]
- 14.Chuang LT, Temin S, Camacho R, Dueñas-Gonzalez A, Feldman S, Gultekin M, et al. Management and care of women with invasive cervical cancer: American Society of Clinical Oncology resource-stratified clinical practice guideline. J Glob Oncol. 2016;2:311–340. doi: 10.1200/JGO.2016.003954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Komiyama S, Katabuchi H, Mikami M, Nagase S, Okamoto A, Ito K, et al. Japan Society of Gynecologic Oncology guidelines 2015 for the treatment of ovarian cancer including primary peritoneal cancer and fallopian tube cancer. Int J Clin Oncol. 2016;21:435–446. doi: 10.1007/s10147-016-0985-x. [DOI] [PubMed] [Google Scholar]
- 16.Japan Society of Gynecologic Oncology. Gynecologic oncology training programs by JSGO [Internet] Tokyo: Japan Society of Gynecologic Oncology; 2017. [cited 2017 July 1]. Available from: https://jsgo.or.jp/specialist/rule.html. [Google Scholar]
- 17.Okabayashi H. Radical abdominal hysterectomy for cancer of the cervix uteri, modification of the Takayama operation. Surg Gynecol Obstet. 1921;33:335–341. [Google Scholar]
- 18.Saito T, Katabuchi H. Annual report of the Committee on Gynecologic Oncology, Japan Society of Obstetrics and Gynecology: patient annual report for 2013 and treatment annual report for 2008. J Obstet Gynaecol Res. 2016;42:1069–1079. doi: 10.1111/jog.13043. [DOI] [PubMed] [Google Scholar]
- 19.Inaba N. The patient annual report in 2005. Acta Obstet Gynaecol Jpn. 2007;59:901–982. Available from: http://fa.kyorin.co.jp/jsog/readPDF.php?file=to63/59/3/KJ00005049882.pdf. [Google Scholar]
- 20.Aoki Y. The patient annual report in 2010. Acta Obstet Gynaecol Jpn. 2012;64:1029–1077. Available from: http://fa.kyorin.co.jp/jsog/readPDF.php?file=64/3/064031029.pdf. [Google Scholar]
- 21.Aoki D. The patient annual report in 2012. Acta Obstet Gynaecol Jpn. 2014;66:995–1038. Available from: http://fa.kyorin.co.jp/jsog/readPDF.php?file=66/3/066030995.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Kaplan-Meier survival curve of patients with cervical cancer among subset of women who received surgery alone (n=3,407) by treating hospitals, JSGO-accredited institutions (yellow line) and non-JSGO-accredited institutions (blue line). The OS of cervical cancer women (log-rank, p<0.001) was 96.2% for patients treated in JSGO-accredited institutions and 93.5% for patients treated in non-JSGO-accredited institutions after 2,500 days.