ABSTRACT
Globally, Xpert MTB/RIF (Xpert) is the most widely used PCR test for the diagnosis of tuberculosis (TB). Positive results in previously treated patients, which are due to old DNA or active disease, are a diagnostic dilemma. We prospectively retested sputum from 238 patients, irrespective of current symptoms, who were previously diagnosed to be Xpert positive and treated successfully. Patients who retested as Xpert positive and culture negative were exhaustively investigated (repeat culture, chest radiography, bronchoscopy with bronchoalveolar lavage, long-term clinical follow-up). We evaluated whether the duration since previous treatment completion, mycobacterial burden (the Xpert cycle threshold [CT] value), and reclassification of Xpert-positive results with a very low semiquantitation level to Xpert-negative results reduced the rate of false positivity. A total of 229/238 (96%) of patients were culture negative. Sixteen of 229 (7%) were Xpert positive a median of 11 months (interquartile range, 5 to 19 months) after treatment completion. The specificity was 93% (95% confidence interval [CI], 89 to 96%). Nine of 15 (40%) Xpert-positive, culture-negative patients reverted to Xpert negative after 2 to 3 months (1 patient declined further participation). Patients with false-positive Xpert results had a lower mycobacterial burden than patients with true-positive Xpert results (CT, 28.7 [95% CI, 27.2 to 30.4] versus 17.6 [95% CI, 16.9 to 18.2]; P < 0.001), an increased likelihood of a chest radiograph not compatible with active TB (5/15 patients versus 0/5 patients; P = 0.026), and less-viscous sputum (15/16 patients versus 2/5 patients whose sputum was graded as mucoid or less; P = 0.038). All patients who initially retested as Xpert positive and culture negative (“Xpert false positive”) were clinically well without treatment after follow-up. The duration since the previous treatment poorly predicted false-positive results (a duration of ≤2 years identified only 66% of patients with false-positive results). Reclassifying Xpert-positive results with a very low semiquantitation level to Xpert negative improved the specificity (+3% [95% CI, +2 to +5%]) but reduced the sensitivity (−10% [95% CI, −4 to −15%]). Patients with previous TB retested with Xpert can have false-positive results and thus not require treatment. These data inform clinical practice by highlighting the challenges in interpreting Xpert-positive results, underscore the need for culture, and have implications for next-generation ultrasensitive tests.
KEYWORD: Mycobacterium tuberculosis
INTRODUCTION
Xpert MTB/RIF (Xpert) is a widely used DNA-based PCR test for the diagnosis of active tuberculosis (TB) (1). Mycobacterial DNA and Xpert positivity can persist in the absence of culturable bacilli for years after treatment (2–4). However, the significance of Xpert-positive, culture-negative results (Xpert false-positive results) remains uncertain because culture is an imperfect “gold standard” susceptible to sampling error and technical variation (5, 6). Understanding these Xpert false-positive results is critical given the large global burden of symptomatic patients who present for investigation for active TB but have previously been treated for active TB (∼15% of the 10 million cases in 2015) (7, 8), Xpert's routine use as a frontline test in those with previous TB (20 to 30% of presumptive TB patients in South Africa) (9), and Xpert-based active case finding in people with previous TB (10).
This issue is compounded by the imminent introduction of a new, highly sensitive version of Xpert called the Xpert MTB/RIF Ultra test (Ultra) that, by virtue of its superior limit of detection (11), is likely confounded by residual mycobacterial DNA to a greater extent than the current-generation Xpert cartridge. For example, as described in a recent World Health Organization policy document, Ultra's preliminary specificity (relative to the results of culture) was lower in patients with a history of TB than in those with no history of TB, and this specificity reduction was greater than that seen with Xpert (−5.4% [95% confidence interval {CI}], −9.1 to −3.1%) versus −2.4% [95% CI, −4.0 to −1.3%] (12). The significance, however, of supposedly false-positive results is not well understood. Furthermore, the persistence of PCR positivity in the absence of culturable bacilli may predict relapse or subclinical disease (13, 14); however, few studies have monitored Xpert-positive patients after treatment completion.
Previously, in a retrospective evaluation using biobanked sputa from patients with presumptive TB, we described the frequency and predictors of Xpert false positivity in previously treated patients (2). We also showed that Xpert detects DNA from nonintact cells, suggesting that dead bacilli contribute to the false positivity. However, as culture is a suboptimal reference standard (15) and adjunct diagnostic tools like chest radiography have poor specificity, especially in high-risk populations infected with HIV (16, 17), we could not discriminate whether Xpert-positive, culture-negative patients were true Xpert false positives in the absence of prospective follow-up and further investigations. In the current study, we performed repeat microbiological testing, bronchoscopy, and prospective clinical follow-up in a new cohort of patients with previous TB to discern the characteristics, profiles, and frequencies of patients with Xpert-positive, culture-negative results. We also present the results of new analyses performed using pooled data from both our new cohort and a previous study (2).
MATERIALS AND METHODS
Participant recruitment.
We consecutively recruited adults (age, ≥18 years) from April 2015 to June 2016, irrespective of whether they were symptomatic, from Cape Town, South Africa, who were previously diagnosed to be sputum Xpert positive in diagnostic research studies at the University of Cape Town (18, 19). Patients had been successfully treated for TB in the program. Through the details provided previously, patients were contacted and asked to return for enrollment in this study. Thus, all enrolled patients had been previously treated for proven TB and were recontacted for opportunistic sampling. We excluded patients currently on treatment. This study was approved by the University of Cape Town Faculty of Health Sciences Ethics Committee (approval 698/2014).
Diagnostic tests, procedures, and clinical follow-up.
At recruitment, patients gave two induced sputum specimens (20) and received a previously validated morbidity score, administered by a research nurse (21). One sputum specimen was randomly selected for testing with Xpert, and the other was used for both Ziehl-Neelsen smear microscopy and liquid culture with the MGIT 960 system. Prior to the addition of the Xpert sample reagent, the viscosity of the Xpert sputum was subjectively graded (as mucopurulent, purulent, mucosalivary, or salivary) as previously described (22). At the first visit, patients who tested Xpert positive and culture negative were referred for a clinical examination prior to bronchoscopy. We recorded the semiquantitative level of Xpert-positive results, which are automatically reported by the GeneXpert software on the basis of predefined cycle threshold (CT) values (CT values are inversely proportional to the concentration of mycobacterial DNA in a specimen) (23, 24). At examination, patients underwent another round of sputum-based testing with Xpert and culture, as well as chest radiography. Irrespective of the test results from this prebronchoscopy visit, all Xpert-positive, culture-negative patients from enrollment were asked to undergo bronchoscopy with bronchoalveolar lavage as previously described (25). Testing by Xpert and culture was done on the bronchoalveolar lavage fluid (BALF). Patients who were culture positive from any specimen were referred to the program for treatment and exited the study. Patients who initially retested Xpert false positive were visited at home or contacted telephonically in December 2016 to ascertain their health status.
Statistical analyses.
We defined patients who were Xpert positive, culture negative using sputa from their first visit as false positive. The χ2 and Mann-Whitney tests were used to compare the proportions and differences in nonparametric continuous data, respectively. McNemar's test was used to calculate the changes in sensitivity and specificity after reclassification of Xpert-positive results on the basis of their semiquantitative levels. All specificity calculations were done using the paired Xpert and culture result from the first visit (culture served as a reference standard). To analyze how Xpert specificity changed over time since previous treatment completion, we constructed fractional polynomial prediction plots locally weighted to the number of Xpert-negative, culture-negative (true-negative) patients at each time point. Exact binomial 95% confidence intervals were calculated. We used a sliding time window (e.g., at 2 months, only patients for whom 2 months or longer had passed since the completion of treatment for their previous case of TB were included in the specificity calculation). To achieve greater statistical power for analyses involving years, we combined our data with those from a previously described cohort of patients with a history of TB who were symptomatic and underwent Xpert testing (2). We used GraphPad Prism (version 6.0; GraphPad Software) and Stata (version 14; StataCorp) software. All statistical tests were two-sided at an α level of 0.05.
RESULTS
Xpert-positive results in previously treated TB patients.
Of the 262 patients recruited, 24 were excluded (Fig. 1). A median of 11 months (interquartile range [IQR], 5 to 19 months) passed between the completion of treatment for the previous episode and recruitment. As determined using sputa collected at recruitment, 9 of the 238 (4%) included patients were culture positive and 5/9 (55%) were Xpert positive. Sixteen of 229 (7%) culture-negative patients were Xpert positive (specificity, 93%; 213/229 [95% CI, 89 to 96%]). False-positive patients had a lower bacillary burden (mycobacterial DNA) than true-positive patients (median Xpert CT, 28.66 [IQR, 27.21 to 30.4] versus 17.64 [16.86 to 18.20]; P < 0.001), an increased likelihood of a chest radiograph not compatible with active TB (5/15 patients versus 0/5 patients; P = 0.026), sputum that was less viscous (15/16 patients versus 2/5 patients had a grade of mucoid or less; P = 0.038), and trends toward more recent previous TB (5 months [IQR, 5 to 6 months] versus 11 months [IQR, 4 to 16 months] since treatment completion; P = 0.112) and a lower morbidity score (0 [IQR, 0 to 1] versus 3 [IQR, 3 to 4]; P = 0.067). Internal positive control CT values, used to detect possible PCR inhibition (26), did not differ between false- and true-positive patients (24.8 [IQR, 22.4 to 26.1] versus 25.4 [IQR, 24.5 to 26.2]; P = 0.561). Six of the 16 Xpert-positive, culture-negative patients (38%) met WHO symptom criteria for TB testing (Table 1) (10).
FIG 1.
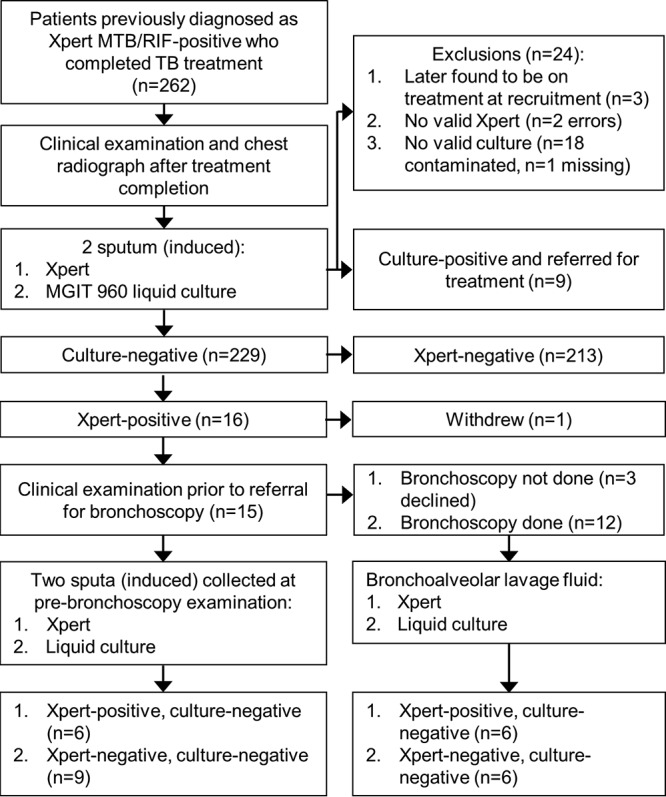
Study flow diagram and test results.
TABLE 1.
Overview of Xpert-positive, culture-negative (false-positive) patients with a history of previous TBa
| Patient no. | HIV infection status | Morbidity score at recruitmentb | No. of WHO TB symptoms (symptom type) at recruitmentc | WHO symptom criteria for active TB investigation metd | Chest radiography findings | Sputum Xpert and culture results prior to bronchoscopy | Time (mo) from enrollment to repeat sputum testing | BALF Xpert and culture results |
|---|---|---|---|---|---|---|---|---|
| RX059 | P | 0 | 1 (current cough) | Yes | Compatible with active TB, right unilateral cavitation | Xpert negative, culture negative | 2 | Bronchoscopy declined |
| RX061 | N | 0 | 1 (cough for ≥2 wk) | Yes | Compatible with old TB | Xpert negative, culture negative | 2 | Xpert negative, culture negative |
| RX065 | P | 0 | 0 | No | Compatible with active TB, no cavitation | Xpert negative, culture negative | 2 | Xpert negative, culture negative |
| RX076 | P | 0 | 0 | No | Compatible with active TB, no cavitation | Xpert positive, culture negative | 2 | Xpert positive, culture negative |
| RX099 | P | 2 | 3 (cough for ≥2 wk, wt loss, fatigue) | Yes | Compatible with active TB, bilateral cavitation | Xpert negative, culture negative | 2 | Xpert positive, culture negative |
| RX101 | P | 0 | 0 | No | Compatible with active TB, no cavitation | Xpert positive, culture negative | 2 | Xpert negative, culture negative |
| RX102 | P | 1 | 0 | No | Compatible with active TB, no cavitation | Xpert negative, culture negative | 2 | Bronchoscopy not done |
| RX108 | N | 0 | 1 (current cough) | No | Compatible with active TB, no cavitation | Xpert positive, culture negative | 2 | Xpert positive, culture negative |
| RX115 | P | 0 | 0 | No | Compatible with active TB, left unilateral cavitation | Xpert negative, culture negative | 2 | Xpert positive, culture negative |
| RX122 | P | 2 | 3 (wt loss, fever, chest pain) | Yes | Compatible with old TB | Xpert negative, culture negative | 2 | Bronchoscopy declined |
| RX124 | P | 1 | 1 (cough for ≥2 wk) | Yes | Compatible with old TB | Xpert positive, culture negative | 1 | Xpert positive, culture negative |
| RX146 | P | 0 | 0 | No | Compatible with active TB, no cavitation | Declined further participation after first visit | NA | Bronchoscopy declined |
| RX502 | P | 0 | 0 | No | Not done | Xpert positive, culture negative | 3 | Xpert negative, culture negative |
| RX512 | P | 7 | 6 (cough for ≥2 wk, wt loss, fever, night sweats, fatigue, chest pain) | Yes | Compatible with active TB, no cavitation | Xpert positive, culture negative | 1 | Xpert negative, culture negative |
| RX539 | P | 1 | 0 | No | Compatible with active TB, right unilateral cavitation | Xpert negative, culture negative | 2 | Xpert negative, culture negative |
| RX565 | N | 0 | 0 | No | Compatible with active TB, cavitation present but extent unrecorded | Xpert negative, culture negative | 1 | Xpert positive, culture negative |
All patients were clinically well without treatment after long-term follow-up. Abbreviations: BALF, bronchoalveolar lavage fluid; P, positive; N, negative; TB, tuberculosis; WHO, World Health Organization; NA, not applicable.
The morbidity score refers to the TBscore, which has been described previously (21).
See reference 32.
Repeat Xpert and culture results in false-positive patients with a history of TB.
Fifteen false-positive patients were successfully referred for clinical examination (median time since recruitment, 2 months [IQR 2 to 3 months]) prior to bronchoscopy. Xpert and culture were repeated with sputum, and the number of Xpert-positive patients decreased to six (nine were now Xpert negative). We detected no significant differences, including the time between repeat testing (2 months [IQR, 2 to 2 months] versus 2 months [IQR, 1 to 2.25 months]; P = 0.723), between patients whose Xpert result remained positive and those whose Xpert result changed to negative. All 15 patients were still sputum culture negative. Of the 12 patients who underwent bronchoscopy (Fig. 1; three patients declined bronchoscopy), 6 patients were BALF Xpert positive and 6 were BALF Xpert negative (all 12 were BALF culture negative). The results of Xpert with BALF had a poor concordance with the results of Xpert with sputum collected at the prebronchoscopy clinical examination visit: half of sputum Xpert-positive patients were BALF Xpert negative (3/6), and half of BALF Xpert-positive patients were sputum Xpert negative (3/6). An overview of each false-positive patient, their clinical characteristics, and their results are provided in Table 1.
Clinical follow-up.
Of the 16 Xpert false-positive patients, 15 were successfully followed up after a median time of 17 months (IQR, 16 to 18 months) (patient RX102 relocated). Fourteen patients were reported to be healthy and asymptomatic, including the 3 (patients RX59, RX122, and RX146) who opted out of bronchoscopy. One patient (patient RX124; a heavy smoker) reported a persistent cough but had recently been screened for TB at the local clinic and was Xpert and culture negative.
Period since previous TB and Xpert false positivity.
Of the 229 culture-negative patients, 214 (94%) had data on the number of months that had passed since their previous TB treatment. A total of 172/214 (80%) had treatment within 24 months, including 15 false-positive patients (1 false-positive patient was missing this information). Hence, when the data for culture-negative patients who had received treatment within the last 2 years were excluded (Fig. 2A), the specificity rose from 93% (95% CI, 89 to 96%; 213/229) to 100% (95% CI, 92 to 100%; 42/42).
FIG 2.
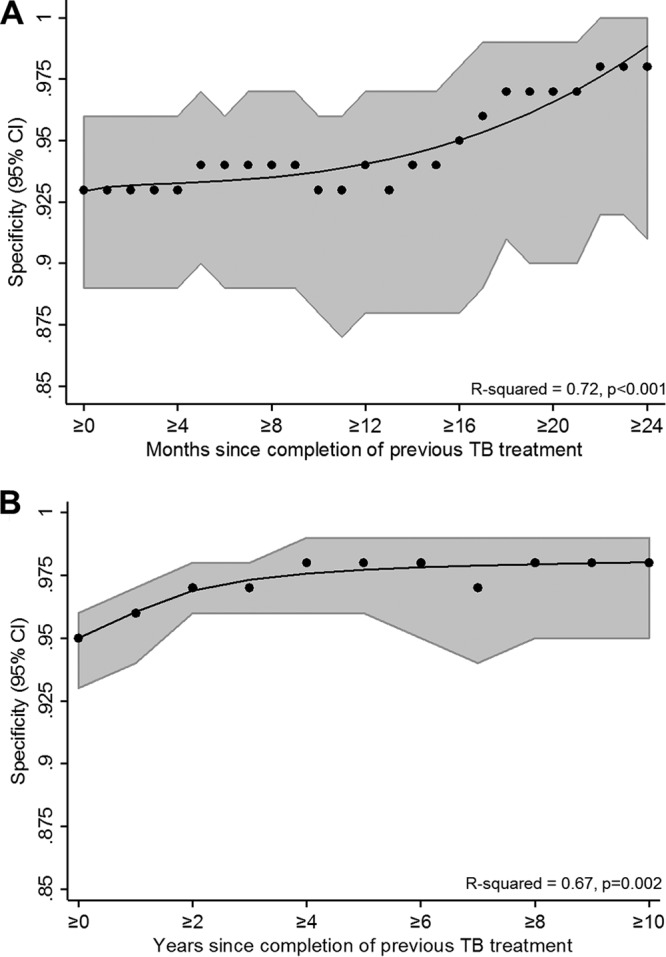
Specificity of Xpert MTB/RIF at different time points, in months (A) and years (B), after the completion of treatment for the previous episode of TB. Sliding windows including patients at each time point or thereafter were used to calculate specificity. When the analyses were restricted to patients without recent previous TB, the specificity improved.
As our cohort of retested patients included those with relatively recent TB, to explore the impact of time since previous treatment on a larger scale (years), we did new analyses with data pooled with data from another cohort of patients with a history of TB (2). Using these pooled data, the overall specificity in patients with previous TB was 94% (95% CI, 93 to 95%; 951/1,011), and the specificity increased to 95% (95% CI, 94 to 96%; 974/920) and 97% (95% CI, 95 to 98%; 689/713) when the data for patients who had completed treatment within 1 and 2 years, respectively, were excluded from calculations (Fig. 2B). The specificity plateaued thereafter.
We next evaluated whether the time (in years) since previous treatment completion could accurately classify false-positive patients in our pooled data (Fig. 3). This could be useful to channel patients into different diagnostic algorithms for those with a recent history of TB that account for Xpert's compromised specificity. If a same-year cutoff point were used, 30% (95% CI, 24 to 35%; 52/203) of Xpert false-positive patients would be correctly classified, increasing to 52% (95% CI, 46 to 58%; 106/203) and 64% (95% CI, 58 to 70%; 130/203) when cutoff points of ≤2 and ≤3 years, respectively, were used. However, high proportions of patients with active TB who would be correctly detected by Xpert would be erroneously excluded as likely false positive (83% [95% CI, 82 to 85%; 1,315/1,582], 67% [95% CI, 65 to 69%; 1,062/1,582], and 54% [95% CI, 52 to 56%; 854/1,582] for each of the three cutoff points, respectively). The amount of time since the previous treatment alone is, hence, unsuitable for accurately discriminating between patients that are likely to be Xpert false or true positive.
FIG 3.
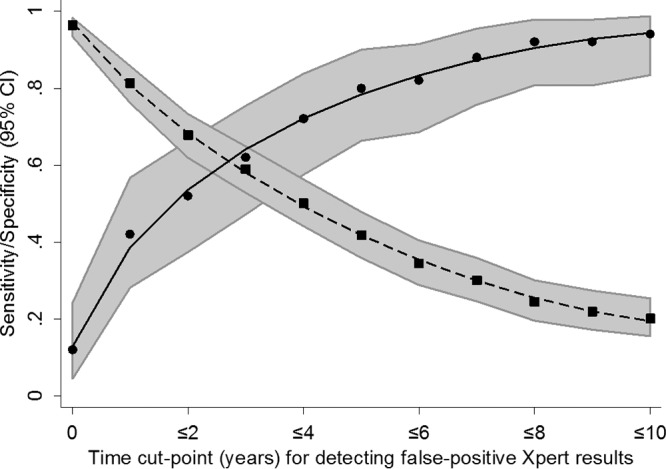
Suboptimal sensitivity (squares, dashed line) and specificity (circles, solid line) of different cutoff points (years) for classifying patients with previous TB as likely to be false or true positive with Xpert.
Reclassification of Xpert MTB/RIF-positive patients with a semiquantitative level of very low as Xpert negative.
Using pooled data, Xpert's sensitivity and specificity in previously treated patients were 84% (95% CI, 80 to 88%; 326/388) and 93% (95% CI, 88 to 96%; 984/1,049), respectively, whereas after reclassification they were 75% (95% CI, 70 to 79%; 289/388; P = 0.001) and 97% (95% CI, 96 to 98%; 1,020/1,049; P < 0.001), respectively. The specificity hence improved (+3% [95% CI, +2 to +5%]), but sensitivity was reduced (−10% [95% CI, −4 to −15%]).
DISCUSSION
This study is the first to undertake a prospective follow-up and an exhaustive investigation to correctly classify Xpert-positive, culture-negative results in patients with previous TB. The key findings are as follows: (i) false-positive Xpert results occur in a significant minority of patients with previous TB, (ii) Xpert-positive, culture-negative patients remained healthy (or had minimal symptoms) and were consistently culture negative without treatment, suggesting that they do not have active disease, (iii) although the characteristics of false-positive patients differ significantly from those of true-positive patients, these characteristics (most importantly, the time since previous TB) have a poor predictive capability for identifying patients likely to be false positive, and (iv) Xpert-positive results in previously treated patients were transient, and about half transitioned to Xpert-negative results after later retesting.
We have previously described the increased likelihood of Xpert false-positive results in symptomatic patients with previous TB; however, here we show for the first time that this can occur in patients who are healthy or have minimal symptoms. In a routine context, such individuals may be tested with highly sensitive nucleic acid amplification tests as contacts of index cases or as part of targeted active case finding in special populations. Xpert has been reported to have a high specificity in the community-based screening of healthy individuals; however, this was in a setting with a very low prevalence of previous TB (27). This requires confirmation in settings with a high burden of patients with previous TB.
Importantly, we found that the amount of time since previous treatment was likely not useful to programs or clinicians looking to accurately discriminate between patients with a history of TB who are likely to be Xpert false positive and those who are true positive. Although the decreasing likelihood of Xpert false positivity since the time since previous treatment has been described before (2, 3), here we describe this phenomenon for the first time on a fine scale (i.e., months), which is important, as most recurrences occur within 1 to 2 years of treatment completion and the use of this more granular time scale may be more sensitive than the use of a blunter years-based approach (28, 29). This finding regarding time is similar to our previous findings regarding the mycobacterial load (CT value), where, although patients with false-positive results had significantly fewer bacilli in their sputum than patients with true-positive results, this did not translate into clinically useful predictive values (2). Interestingly, we also found patients with false-positive results to have less-viscous sputum. This is congruent with our findings regarding CT values, as more salivary sputum has previously been shown to be associated with a lower bacillary load (30).
Importantly, Xpert false positivity was transient. After an average of 2 months between recruitment and repeat sputum testing (prior to bronchoscopy), over half of Xpert false-positive patients were Xpert negative. Thus, detection of DNA from a previous TB episode can be stochastic (this may be due to sampling error or the gradual elimination of pathogen DNA by the host). HIV-positive patients, even those on antiretroviral therapy, have compromised pulmonary immune clearance (31) and may thus be more susceptible to sustained false positivity.
After long-term follow-up, false-positive patients remained culture negative and asymptomatic without treatment, indicating that they were highly unlikely to go on to develop active TB. This is despite the fact that most false-positive patients, including those with HIV infection, had a chest radiograph compatible with active TB. This complicates the management of Xpert-positive patients with prior TB. Thus, in our cohort of retested patients with a history of previous TB and minimal symptoms, all Xpert-positive, culture-negative patients overall had little evidence of active TB after an intensive workup.
We found that reclassifying Xpert false-positive patients with the lowest semiquantitative level as negative increased the specificity. However, the resultant reduction in sensitivity was more than 2-fold the specificity gained. This may limit the attractiveness of this approach, which has been mooted for the new Ultra's trace level. Such a reclassification in Ultra may result in changes in sensitivity different from those in Xpert (12); however, the payoffs should be modeled in different patients and settings.
In terms of limitations, first, at the time of our study, Ultra was not available, and its specificity requires investigation in patients with previous TB. Our findings also require validation in different populations, settings, and studies containing larger sample sizes. Second, we targeted known previous TB cases irrespective of their symptoms. Although many had symptoms upon retesting, they are a population distinct from self-presenting patients with prior TB. It is also possible that patients who are Xpert positive after treatment completion might still benefit from treatment, despite being culture negative (e.g., to reduce relapse); however, this requires prospective investigation.
In conclusion, these findings have implications for the interpretation of Xpert-positive results in patients with previous TB and provide evidence of Xpert's suboptimal specificity. It also informs how clinicians should manage false-positive patients. Importantly, given that clinical and test characteristics (including the CT values) and the time since previous treatment cannot accurately classify which patients will likely have a false-positive Xpert result, careful clinical assessment and additional tools (e.g., culture, clinical follow-up) remain essential for the management of Xpert-positive patients with previous TB.
ACKNOWLEDGMENTS
We are indebted to the patients who participated. We thank Marietjie Pretorius, Ruth Wilson, Eleanor Pretorius, and members of the Groote Schuur Hospital E16 Respiratory Clinic for their invaluable assistance.
G.T. acknowledges funding from a South African Medical Research Council career development fellowship, the European and Developing Countries Clinical Trials Partnership (EDCTP), and the Faculty of Medicine and Health Sciences, Stellenbosch University. R.V. acknowledges the financial assistance of the National Research Foundation (NRF). K.D. is supported by the South African Medical Research Council and the European and Developing Countries Clinical Trials Partnership.
G.T. and K.D. conceived and designed the study. All authors collected the data. G.T. performed the analysis and prepared the first draft. All authors interpreted the findings and provided important intellectual input.
We have no conflicts of interest to declare.
REFERENCES
- 1.Dheda K, Barry CE III, Maartens G. 2016. Tuberculosis. Lancet 387:1211–1226. doi: 10.1016/S0140-6736(15)00151-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Theron G, Venter R, Calligaro G, Smith L, Limberis J, Meldau R, Chanda D, Esmail A, Peter J, Dheda K. 2016. Xpert MTB/RIF results in patients with previous tuberculosis: can we distinguish true from false positive results? Clin Infect Dis 62:995–1001. doi: 10.1093/cid/civ1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Metcalfe JZ, Makumbirofa S, Makamure B, Mutetwa R, Peñaloza RA, Sandy C, Bara W, Mungofa S, Hopewell PC, Mason P. 2015. Suboptimal specificity of Xpert MTB/RIF among treatment-experienced patients. Eur Respir J 45:1504–1506. doi: 10.1183/09031936.00214114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boyles TH, Hughes J, Cox V, Burton R, Meintjes G, Mendelson M. 2015. False-positive Xpert (®) MTB/RIF assays and previous treatment. Int J Tuberc Lung Dis 19:495–496. doi: 10.5588/ijtld.14.0800-2. [DOI] [PubMed] [Google Scholar]
- 5.Monkongdee P, McCarthy KD, Cain KP, Tasaneeyapan T, Dung NH, Lan NTN, Yen NTB, Teeratakulpisarn N, Udomsantisuk N, Heilig C. 2009. Yield of acid-fast smear and mycobacterial culture for tuberculosis diagnosis in people with human immunodeficiency virus. Am J Respir Crit Care Med 180:903. doi: 10.1164/rccm.200905-0692OC. [DOI] [PubMed] [Google Scholar]
- 6.Hanna BA, Ebrahimzadeh A, Elliott LB, Morgan MA, Novak SM, Rusch-Gerdes S, Acio M, Dunbar DF, Holmes TM, Rexer CH. 1999. Multicenter evaluation of the BACTEC MGIT 960 system for recovery of mycobacteria. J Clin Microbiol 37:748–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zignol M, Wright A, Jaramillo E, Nunn P, Raviglione MC. 2007. Patients with previously treated tuberculosis no longer neglected. Clin Infect Dis 44:61–64. doi: 10.1086/509328. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization. 2016. Global tuberculosis report. World Health Organization Geneva, Switzerland. [Google Scholar]
- 9.World Health Organization. 2011. Policy statement: automated real-time nucleic acid amplification technology for rapid and simultaneous detection of tuberculosis and rifampicin resistance: Xpert MTB/RIF system. World Health Organization, Geneva, Switzerland. [PubMed] [Google Scholar]
- 10.World Health Organization. 2013. Systematic screening for active tuberculosis—principles and recommendations. World Health Organization, Geneva, Switzerland. [PubMed] [Google Scholar]
- 11.Chakravorty S, Simmons AM, Rowneki M, Parmar H, Cao Y, Ryan J, Banada PP, Deshpande S, Shenai S, Gall A. 2017. The new Xpert MTB/RIF Ultra: improving detection of Mycobacterium tuberculosis and resistance to rifampin in an assay suitable for point-of-care testing. mBio 8:e00812-17. doi: 10.1128/mBio.00812-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization. 2017. WHO meeting report of a technical expert consultation: non-inferiority analysis of Xpert MTB/RIF Ultra compared to Xpert MTB/RIF. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 13.Chierakul N, Chaiprasert A, Tingtoy N, Arjratanakul W, Pattanakitsakul SN. 2001. Can serial qualitative polymerase chain reaction monitoring predict outcome of pulmonary tuberculosis treatment? Respirology 6:305–309. doi: 10.1046/j.1440-1843.2001.00355.x. [DOI] [PubMed] [Google Scholar]
- 14.García-Basteiro AL, Saavedra B, Cobelens F. 2017. The good, the bad and the ugly of the next-generation Xpert Mtb/Rif (®) Ultra test for tuberculosis diagnosis. Arch Bronconeumol 53:665–666. doi: 10.1016/j.arbres.2017.05.023. [DOI] [PubMed] [Google Scholar]
- 15.Cruciani M, Scarparo C, Malena M. 2004. Meta-analysis of BACTEC MGIT 960 and BACTEC 460 TB, with or without solid media, for detection of mycobacteria. J Clin Microbiol 42:2321–2325. doi: 10.1128/JCM.42.5.2321-2325.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Theron G, Pooran A, Peter J, van Zyl-Smit R, Mishra H, Meldau R, Calligaro G, Allwood B, Sharma S, Dawson R. 2011. Do adjunct TB tests, when combined with Xpert MTB/RIF, improve accuracy and the cost of diagnosis in a resource-poor setting? Eur Respir J 40:161–168. doi: 10.1183/09031936.00145511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pinto LM, Dheda K, Theron G, Allwood B, Calligaro G, van Zyl-Smit R, Peter J, Schwartzman K, Menzies D, Bateman E. 2013. Development of a simple reliable radiographic scoring system to aid the diagnosis of pulmonary tuberculosis. PLoS One 8:e54235. doi: 10.1371/journal.pone.0054235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Theron G, Zijenah L, Chanda D, Clowes P, Rachow A, Lesosky M, Bara W, Mungofa S, Pai M, Hoelscher M. 2014. Feasibility, accuracy, and clinical effect of point-of-care Xpert MTB/RIF testing for tuberculosis in primary-care settings in Africa: a multicentre, randomised, controlled trial. Lancet 383:424–435. doi: 10.1016/S0140-6736(13)62073-5. [DOI] [PubMed] [Google Scholar]
- 19.Peter JG, Theron G, Pooran A, Thomas J, Pascoe M, Dheda K. 2013. Comparison of two methods for acquisition of sputum samples for diagnosis of suspected tuberculosis in smear-negative or sputum-scarce people: a randomised controlled trial. Lancet Respir Med 1:471–478. doi: 10.1016/S2213-2600(13)70120-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peter JG, Theron G, Singh N, Singh A, Dheda K. 2014. Sputum induction to aid the diagnosis of smear-negative or sputum-scarce TB in adults from a HIV-endemic setting. Eur Respir J 43:185–194. doi: 10.1183/09031936.00198012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wejse C, Gustafson P, Nielsen J, Gomes VF, Aaby P, Andersen PL, Sodemann M. 2008. TBscore: signs and symptoms from tuberculosis patients in a low-resource setting have predictive value and may be used to assess clinical course. Scand J Infect Dis 40:111–120. doi: 10.1080/00365540701558698. [DOI] [PubMed] [Google Scholar]
- 22.Rieder HL, Chonde TM, Myking H, Urbanczik R, Laszlo A, Kim S, Van Deun A. 1998. The public health service national tuberculosis reference laboratory and the national laboratory network; minimum requirements, role and operation in a low-income country. International Union against Tuberculosis and Lung Disease, Paris, France. [Google Scholar]
- 23.Cepheid. 2009. Xpert MTB/RIF package insert. 300-7810 Rev A. Cepheid, Sunnyvale, CA. [Google Scholar]
- 24.van Zyl-Smit RN, Binder A, Meldau R, Mishra H, Semple PL, Theron G, Peter J, Whitelaw A, Sharma SK, Warren R. 2011. Comparison of quantitative techniques including Xpert MTB/RIF to evaluate mycobacterial burden. PLoS One 6:e28815. doi: 10.1371/journal.pone.0028815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Theron G, Peter J, Meldau R, Khalfey H, Gina P, Matinyena B, Lenders L, Calligaro G, Allwood B, Symons G. 2013. Accuracy and impact of Xpert MTB/RIF for the diagnosis of smear-negative or sputum-scarce tuberculosis using bronchoalveolar lavage fluid. Thorax 68:1043–1051. doi: 10.1136/thoraxjnl-2013-203485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Theron G, Peter J, Calligaro G, Meldau R, Hanrahan C, Khalfey H, Matinyenya B, Muchinga T, Smith L, Pandie S. 2014. Determinants of PCR performance (Xpert MTB/RIF), including bacterial load and inhibition, for TB diagnosis using specimens from different body compartments. Sci Rep 4:5658. doi: 10.1038/srep05658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ho J, Nguyen PTB, Nguyen TA, Tran KH, Van Nguyen S, Nguyen NV, Nguyen HB, Luu KB, Fox GJ, Marks GB. 2016. Reassessment of the positive predictive value and specificity of Xpert MTB/RIF: a diagnostic accuracy study in the context of community-wide screening for tuberculosis. Lancet Infect Dis 16:1045–1051. doi: 10.1016/S1473-3099(16)30067-6. [DOI] [PubMed] [Google Scholar]
- 28.Marx FM, Dunbar R, Enarson DA, Williams BG, Warren RM, van der Spuy GD, van Helden PD, Beyers N. 2014. The temporal dynamics of relapse and reinfection tuberculosis after successful treatment: a retrospective cohort study. Clin Infect Dis 58:1676–1683. doi: 10.1093/cid/ciu186. [DOI] [PubMed] [Google Scholar]
- 29.Nunn A, Phillips P, Mitchison D. 2010. Timing of relapse in short-course chemotherapy trials for tuberculosis. Int J Tuberc Lung Dis 14:241–242. [PubMed] [Google Scholar]
- 30.Blakemore R, Nabeta P, Davidow AL, Vadwai V, Tahirli R, Munsamy V, Nicol M, Jones M, Persing DH, Hillemann D. 2011. A multisite assessment of the quantitative capabilities of the Xpert MTB/RIF assay. Am J Respir Crit Care Med 184:1076–1084. doi: 10.1164/rccm.201103-0536OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gingo MR, Morris A. 2013. Pathogenesis of HIV and the lung. Curr HIV/AIDS Rep 10:42–50. doi: 10.1007/s11904-012-0140-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.World Health Organization. 2013. Systematic screening for active tuberculosis: principles and recommendations. World Health Organization, Geneva, Switzerland. [PubMed] [Google Scholar]
- 33.World Health Organization. 2011. Guidelines for intensified tuberculosis case-finding and isoniazid preventive therapy for people living with HIV in resource-constrained settings. World Health Organization, Geneva, Switzerland. [Google Scholar]


