Abstract
A case series was used to evaluate the efficacy of half-fluence photodynamic therapy (PDT) for chronic central serous chorioretinopathy (CSCR). Patients were treated with standard-dose verteporfin and half-fluence PDT. Totally 13 eyes from 11 patients were included. The mean patient age was 52.0y. There was a mean reduction in central retinal thickness of 107.0 microns. Totally 7/13 eyes (53.8%) achieved resolution of subretinal fluid (SRF) on optical coherence tomography (OCT) scan after 1 treatment with PDT. Four eyes had further treatment with PDT; of these 1 eye achieved resolution of SRF. Seven of the 13 eyes (53.8%) achieved an improvement of more than 5 ETDRS letters. One patient experienced acute macula oedema 1d post PDT treatment. These results support the hypothesis that half-fluence PDT can have a positive effect in chronic CSCR for a gain in visual acuity and reduction in sub-retinal fluid. Acute macula oedema is a rare but potential adverse effect of half-fluence PDT.
Keywords: central serous chorioretinopathy, photodynamic therapy, fluence
INTRODUCTION
Central serous chorioretinopathy (CSCR) is an idiopathic disease characterised by serous detachment of the sensory neuroretina at the posterior pole. It can be a recurrent but is mostly a self limiting disease with good natural history.
In acute CSCR, fluid tends to resolve spontaneously within 3mo and in most cases without lasting sequelae[1]. When fluid does not resolve spontaneously after a given time, treatment options are often considered. The timeframe after which treatment is considered varies and the designation of acute chronic CSCR in the literature is fairly unsystematic. Some studies have cited timeframe definitions such as non-resolution of fluid specific timeframes ranging from six weeks[2] to six months[3]. Others suggest the condition becomes chronic once permanent damage has occurred due to long-term subretinal fluid (SRF) leakage, resulting in atrophic retinal changes[4]–[5]. The general consensus seems to agree that CSCR is considered chronic if long term accumulation of SRF leads to irreversible retinal damage resulting in a long term impact on visual acuity.
In order to limit this damage and prevent visual decline, effective treatments have been sought. Photodynamic therapy (PDT) has been shown to be an effective treatment for chronic CSCR[6]. There are currently no set guidelines or protocols regarding the treatment of CSCR. PDT has been applied with a variety of strategies including full or half dose verteporphin and full or half dose fluence which aim to address concerns of the long term impact on the normal choroidal vasculature and retinal pigment epithelium to conventional PDT. Some studies have compared half-fluence and standard-fluence treatments and found both strategies equal in terms of visual and anatomical outcomes[7]–[8]. Long term outcome data following treatment with PDT is still lacking, nor is there a general consensus of what the best treatment protocol may be. We aim to report long-term outcomes on a patient cohort treated with half fluence, full dose PDT.
METHODS
We performed a retrospective analysis of a consecutive cohort of 13 eyes who received half-fluence, full-dose PDT between February 2011 and February 2015. The study adhered to the principles of the Helsinki Declaration. All patients who were aged 18 and above and had symptomatic chronic CSCR for more than 6mo were included. Initial diagnosis was made based on fundoscopy, optical coherence tomography (OCT), fundus fluorescein angiography (FFA) and indocyanine green angiography (ICG). Baseline visual acuity and OCT scans were recorded pre-treatment. OCT scanning was performed using a Topcon 2000, macula scans of 6×6 mm2 were carried out with both radial and line OCT scanning. The OCT images were analysed using the viewing platform Topcon Imagenet6. After informed consent, half-fluence PDT was performed. A standard dose of 6 mg/m2 intravenous Visudyne (Verteporfin) was used and infused over 10min. The laser power (Quantel medical PDT laser) was set at half fluence of 25 mJ/cm2 (standard is 50 mJ/cm2) and was applied over 83s. The laser was applied 15min after the commencement of infusion. The laser spot size varied in each patient, related to the size of the treated area; the lesion itself was covered in each patient. At follow up visits BCVA were assessed and OCT scanning performed. Patients were seen in at 3 monthly intervals before treatment. Post-treatment with PDT the patients were seen initially 1mo post treatment, the ongoing follow up interval after this time generally extended the longer the patient remained in follow up.
RESULTS
Totally 13 eyes from 11 patients were included in the cohort, comprising of 7 men (63.6%) and 4 women (36.4%). Two patients had bilateral disease, one male and one female. Mean age was 52.0y [range 34-72y, standard deviation (SD) =14.2]. One patients had previously been treated for suspected neovascular age-related macular degeneration with anti-vascular endothelial growth factor therapy; she had received 4 Lucentis injections before being diagnosed with CSCR. All patients had been symptomatic for a minimum of 6mo prior to treatment with PDT.
The mean time between diagnosis in clinic and treatment with PDT was 107d (SD=94.2). The mean baseline best corrected visual acuity (BCVA) was 0.30 logMAR (range 1.0 to 0, SD=0.28) and the mean final BCVA was 0.28 logMAR (range 0.84 to -0.12, SD=0.33). The improvement in BCVA was not found to be statistically significant (P=0.61, Wilcoxon signed-rank test, two-tailed). The mean pre-treatment macula cube volume (mm cube) was 8.2 (range 6.94 to 9.65, SD=0.80) and the mean final macula cube volume (mm cube) post-treatment was 7.10 (range 6.15 to 8.67, SD=0.67). The change in macula cube volume was found to be statistically significant (P=0.004, paired t-test, two-tailed).
The mean baseline central retinal thickness (CRT) on OCT was 297 µm (range 180-394 µm, SD=72.9) and the mean final baseline CRT was 190 µm (range 142-320 µm, SD=49.5). The improvement in CRT was found to be statistically significant, P=0.01 (Wilcoxon signed-rank test, two-tailed). Seven out of 13 eyes (53.8%) achieved a visual improvement of more than 5 ETDRS letters.
Patients remained under review for a mean average of 27.3mo from presentation (range 4-51mo, SD=17.7). The mean average of PDT treatments was 1.31 per eye (SD=0.48), with 4 eyes having further treatment with PDT. Of 7/13 eyes (53.8%) achieved resolution of SRF on OCT scan after one treatment with PDT (Table 1).
Table 1. Patient characteristics pre- and post-treatment with PDT.
| Eye | Macular volume (mm3) |
BCVA (logMAR) |
Followup (mo) | OCT |
|||
| Pre-treatment | Post-treatment | Pre-treatment | Post-treatment | Pre-treatment | Post-treatment | ||
| 1 | 6.94 | 6.15 | 1 | 0.6 | 17 | 1. Serous detachment | 1. Hyper-reflective foci resolved 12mo following treatment with PDT |
| 2. Multiple subretinal hyper-reflective foci | 2. Ellipsoid zone appears intact | ||||||
| 3. Thickened choroid observed with dilated choroidal vessels | |||||||
| 2 | 7.77 | 7.61 | 0 | 0.24 | 51 | 1. Serous detachment | 1. Focal disruption of ellipsoid zone |
| 2. Thickened choroid observed with dilated choroidal vessels | 2. Choroidal vessels remain dilated | ||||||
| 3 | 9.65 | 6.77 | 0.48 | 0.8 | 48 | 1. Serous detachment | 1. Focal disruption of ellipsoid zone |
| 2. Thickened choroid observed with dilated choroidal vessels | 2. Choroidal vessels remain dilated | ||||||
| 4 | 7.42 | 6.47 | 0.18 | 0.84 | 32 | 1. Serous detachment | 1. Focal disruption of ellipsoid zone |
| 2. Thickened choroid observed with dilated choroidal vessels | 2. Choroidal vessels thickening improved | ||||||
| 3. Resolution of hyper-reflective foci | |||||||
| 5 | 8.34 | 6.98 | 0.18 | 0 | 48 | 1. Serous detachment | 1. No disruption in ellipsoid zone |
| 2. No thickening of choroid seen | |||||||
| 6 | 8.75 | 7.29 | 0.18 | 0 | 48 | 1. Serous detachment | 1. Hyper-reflective foci resolved |
| 2. Multiple subretinal hyper-reflective foci | 2. Ellipsoid zone appears intact | ||||||
| 7 | 7.73 | 6.98 | 0.18 | 0.3 | 38 | 1. Serous detachment | 1. Hyper-reflective foci resolved |
| 2. Multiple subretinal hyper-reflective foci | 2. Focal disruption of ellipsoid zone | ||||||
| 8 | 7.99 | 7.08 | 0 | -0.12 | 24 | 1. Multiple subretinal hyper-reflective foci | 1. Hyper-reflective foci resolved |
| 2. Ellipsoid zone appears intact | |||||||
| 9 | 7.38 | 8.67 | 0.48 | 0.46 | 14 | 1. Sensory detatchment | 1. Persistance and increase in volume of the sensory detachment |
| 2. Loss of ellipsoid zone architecture | |||||||
| 10 | 8.12 | 7.35 | 0.22 | 0.1 | 4 | 1. Sensory detatchment | 1. Focal disruption of ellipsoid zone |
| 11 | 8.82 | 6.23 | 0.48 | 0.48 | 5 | 1. Serous detachment | 1. Hyper-reflective foci resolved |
| 2. Multiple subretinal hyper-reflective foci | 2. Focal disruption of ellipsoid zone | ||||||
| 12 | 8.33 | 7.7 | 0 | -0.12 | 16 | 1. Serous detachment | 1. Hyper-reflective foci resolved |
| 2. Multiple subretinal hyper-reflective foci | 2. Focal disruption of ellipsoid zone | ||||||
| 13 | 9.4 | 6.85 | 0.48 | 0.1 | 10 | 1. Serous detachment | 1. Hyper-reflective foci resolved |
| 2. Multiple subretinal hyper-reflective foci | 2. Focal disruption of ellipsoid zone | ||||||
| 3. Intraretinal fluid | |||||||
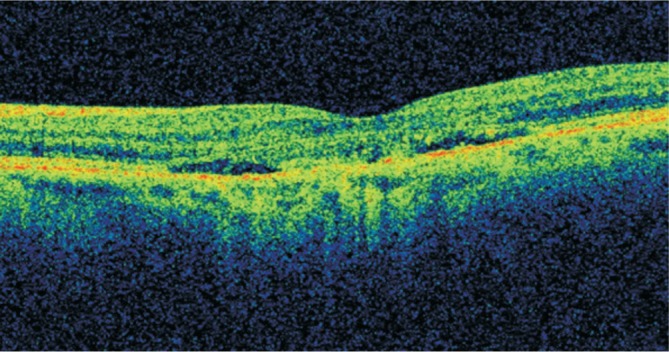
4 eyes underwent further treatment with PDT due to ongoing SRF after the first treatment with PDT. Two patients had unilateral disease and persistent SRF after initial PDT treatment received retreatment at 4.5mo and 6.5mo. The first patient had complete resolution at his last follow up but the second patient had persistent SRF and decided against any further treatment. One patient with a bilateral disease had retreatment in both eyes: left eye for non resolution at 4.5mo and right eye at 6mo. Right eye developed acute macular oedema 1d (Case 4) following their second treatment with PDT (Figure 1) which responded to intravitreal triamcinolone (Figure 2). Left eye also had another reoccurance at month 27 but decided against any treatment due to experience with her right eye.
Figure 1. Acute exudative maculopathy seen day 1 post treatment with half-fluence PDT.
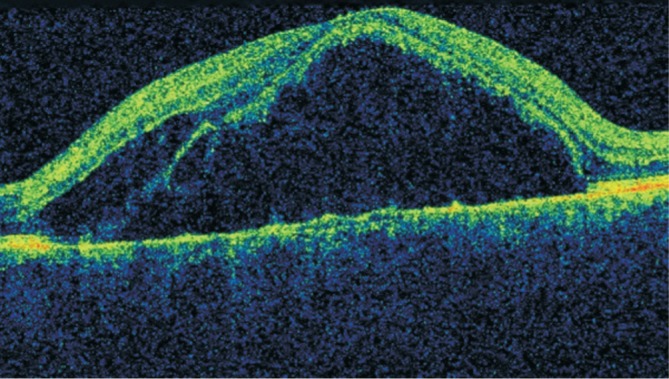
Figure 2. Resolution of macula oedema following treatment with intravitreal triamcinolone.
Two patients did not achieve resolution of the SRF after a single PDT session and decided against any more treatment. One patient has persistent SRF with BCVA 0.3 logMAR and the other patient has a last recorded visual acuity of -0.12 logMAR BCVA.
Comparing the two groups of patients; those who achieved resolution of the SRF at final follow up had a mean final BCVA of 0.18 logMAR (range -0.12-0.6, SD=0.25), those who had persistent SRF had a mean final BCVA of 0.46 (range -0.12 -0.84, SD=0.39). Analysing the anatomical characteristics of the OCT scans significant changes were seen. In 7/13 patients multiple hyper reflective foci were noted pre-treatment in the subretinal space, in all of these patients these foci were found to resolve post-treatment. Whilst we did not have access to enhanced depth imaging OCT, it was observed that there was thickening of the underlying choroid in 4 of the patients pre-treatment. Two of these patients were noted to have an improvement in their choroidal thickening post-treatment. Post-treatment even after resolution of SRF, 9 patients were noted to have focal disruption in their ellipsoid zone. Their mean final BCVA was 0.36 (range -0.12-0.84, SD=0.32) compared to the 4 patients who were found to have an intact ellipsoid zone with a mean final BCVA of 0.12 (range -0.12-0.6, SD=0.33).
DISCUSSION
Our study provides further confirmation that half-fluence PDT can be used to successfully treat chronic CSCR. It shows that half-fluence PDT can have a significant effect on improvement of a patient's visual acuity, in resolving SRF and reducing central retinal thickness and macula cube volume. Whilst the sample is not large enough to allow statistical analysis we show that patients that were found to have focal disruption of their ellipsoid zone following treatment had a worse mean final BCVA than those patients with an intact ellipsoid zone.
There has been several other small cohort studies that have also tried to elucidate the efficacy and safety of different PDT protocols[7]–[22]. A variety of methods have been tried including; standard dose standard fluence, half dose standard fluence or standard dose half fluence as in this study. Thus far no study has identified whether a particular protocol is superior to another in terms of safety or final visual or anatomical outcomes. None of the studies referenced found any deleterious effects of altering the PDT protocol. Those that compared to standard dose protocols did not show any significant difference in visual or anatomical outcomes with half-dose or half-fluence protocols. One study, Nicoló et al[20] did find in their cohort that those treated with half-dose PDT had a more lasting resolution of SRF in their cohort treated with half-dose vs half fluence. They experienced a statistically significant increase in the rate of recurrence of SRF in their cohort treated with half-fluence compared to half-dose. Other studies comparing half-dose directly to half-fluence have not found a similar trend[7],[21]. Ideally a large prospective randomised control trial comparing the various protocol's is needed to elucidate further whether one protocol is superior in terms of visual and anatomical outcomes, and safety profile.
One eye developed acute macula oedema 1d post-re-treatment which was similar to previous single case report by Mammo and Forooghian[22]. This was successfully treated with intravitreal triamcinolone with complete resolution of SRF at week 2. This has been well described in patients receiving full dose PDT for wet macular degeneration[23] but is rare with half dose PDT. The mechanism of this complication has been suggested to be inflammatory in nature due to the morphological similarities observed between this and Vogt-Koyanagi-Harada (VKH) syndrome[24].
The strengths of our study are that it includes long-term follow up of a cohort of patients who received half-fluence PDT. Patients were followed up for a significant period following treatment with PDT without identifying any long term ill effects. We also describe a case of acute exudative maculopathy which is a relatively rare occurrence, having only been reported once before following half-fluence PDT in the literature[22].
Our study is not without its limitations, it is a small number, retrospective analysis, is not randomised and lacks a control group. We recognise that a large, prospective study would useful to provide more robust evidence as to which PDT protocol is superior.
In summary, our study provides further confirmation that half-fluence PDT can be used to successfully treat chronic CSCR. It highlights acute exudative maculopathy as a rare but potential adverse effect. The strength of our study is that it includes long-term follow up of a cohort of patients who received half-fluence PDT.
Acknowledgments
Conflicts of Interest: Doyle J, None; Gupta B, None; Tahir I, None.
REFERENCES
- 1.Klein ML, Van Buskirk EM, Friedman E, Gragoudas E, Chandra S. Experience with nontreatment of central serous choroidopathy. Arch Ophthalmol. 1974;91(4):247–250. doi: 10.1001/archopht.1974.03900060257001. [DOI] [PubMed] [Google Scholar]
- 2.Framme C, Walter A, Gabler B, Roider J, Sachs HG, Gabel VP. Fundus autofluorescence in acute and chronic-recurrent central serous chorioretinopathy. Acta Ophthalmol Scand. 2005;83(2):161–167. doi: 10.1111/j.1600-0420.2005.00442.x. [DOI] [PubMed] [Google Scholar]
- 3.Yannuzzi LA. Central serous chorioretinopathy: a personal perspective. Am J Ophthalmol. 2010;149(3):361–363. doi: 10.1016/j.ajo.2009.11.017. [DOI] [PubMed] [Google Scholar]
- 4.Nicholson B, Noble J, Forooghian F, Meyerle C. Central serous chorioretinopathy: update on pathophysiology and treatment. Surv Ophthalmol. 2013;58(2):103–126. doi: 10.1016/j.survophthal.2012.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gemenetzi M, De Salvo G, Lotery AJ. Central serous chorioretinopathy: an update on pathogenesis and treatment. Eye (Lond) 2010;24(12):1743–1756. doi: 10.1038/eye.2010.130. [DOI] [PubMed] [Google Scholar]
- 6.Silva RM, Ruiz-Moreno JM, Gomez-Ulla F, Montero JA, Gregório T, Cachulo ML, Pires IA, Cunha-Vaz JG, Murta JN. Photodynamic therapy for chronic central serous chorioretinopathy: a 4-year follow-up study. Retina. 2013;33(2):309–315. doi: 10.1097/IAE.0b013e3182670fbe. [DOI] [PubMed] [Google Scholar]
- 7.Cheng CK, Chang CK, Peng CH. Comparison of photodynamic therapy using half-dose of verteporfin or half-fluence of laser light for the treatment of chronic central serous chorioretinopathy. Retina. 2017;37(2):325–333. doi: 10.1097/IAE.0000000000001138. [DOI] [PubMed] [Google Scholar]
- 8.Reibaldi M, Cardascia N, Longo A, Furino C, Avitabile T, Faro S, Sanfilippo M, Russo A, Uva MG, Munno F, Cannemi V, Zagari M, Boscia F. Standard-fluence versus low-fluence photodynamic therapy in chronic central serous chorioretinopathy: a nonrandomized clinical trial. Am J Ophthalmol. 2010;149(2):307–315. doi: 10.1016/j.ajo.2009.08.026. [DOI] [PubMed] [Google Scholar]
- 9.Rouvas A, Stavrakas P, Theodossiadis PG, Stamatiou P, Milia M, Giannakaki E, Datseris I. Long-term results of half-fluence photodynamic therapy for chronic central serous chorioretinopathy. Eur J Ophthalmol. 2012;22(3):417–422. doi: 10.5301/ejo.5000051. [DOI] [PubMed] [Google Scholar]
- 10.Smretschnig E, Ansari-Shahrezaei S, Hagen S, Glittenberg C, Krebs I, Binder S. Half-fluence photodynamic therapy in chronic central serous chorioretinopathy. Retina. 2013;33(2):316–323. doi: 10.1097/IAE.0b013e318280769c. [DOI] [PubMed] [Google Scholar]
- 11.Shin JY, Woo SJ, Yu HG, Park KH. Comparison of efficacy and safety between half-fluence and full-fluence photodynamic therapy for chronic central serous chorioretinopathy. Retina. 2011;31(1):119–126. doi: 10.1097/IAE.0b013e3181e378f2. [DOI] [PubMed] [Google Scholar]
- 12.Lim SH, Chang W, Sagong M. Efficacy of half-fluence photodynamic therapy depending on the degree of choroidal hyperpermeability in chronic central serous chorioretinopathy. Eye(Lond) 2013;27(3):353–362. doi: 10.1038/eye.2013.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al-Hinai A, Al-Abri M. Half-fluence photodynamic therapy to treat chronic central serous chorioretinopathy: a case series. Oman J Ophthalmol. 2011;4(2):63–66. doi: 10.4103/0974-620X.83655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Taban M, Boyer DS, Thomas EL, Taban M. Chronic central serous chorioretinopathy: photodynamic therapy. Am J Ophthalmol. 2004;137(6):1073–1080. doi: 10.1016/j.ajo.2004.01.043. [DOI] [PubMed] [Google Scholar]
- 15.Naseripour M, Falavarjani KG, Sedaghat A, Moghaddam AK, Nasserisina S, Alemzadeh SA. Half-dose photodynamic therapy for chronic central serous chorioretinopathy. J Ophthalmic Vis Res. 2016;11(1):66–69. doi: 10.4103/2008-322X.180706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Neves F, Costa J, Fonseca S, Silva L, Agrelos L. Half-dose photodynamic therapy for chronic central serous chorioretinopathy: efficacy and safety outcomes in real world. Photodiagnosis Photodyn Ther. 2016;14:173–177. doi: 10.1016/j.pdpdt.2016.04.012. [DOI] [PubMed] [Google Scholar]
- 17.Lai FH, Ng DS, Bakthavatsalam M, Chan VC, Young AL, Luk FO, Tsang CW, Brelén ME. A multicenter study on the long-term outcomes of half-dose photodynamic therapy in chronic central serous chorioretinopathy. Am J Ophthalmol. 2016;170:91–99. doi: 10.1016/j.ajo.2016.07.026. [DOI] [PubMed] [Google Scholar]
- 18.Fujita K, Imamura Y, Shinoda K, Matsumoto CS, Mizutani Y, Hashizume K, Mizota A, Yuzawa M. One-year outcomes with half-dose verteporfin photodynamic therapy for chronic central serous chorioretinopathy. Ophthalmology. 2015;122(3):555–561. doi: 10.1016/j.ophtha.2014.09.034. [DOI] [PubMed] [Google Scholar]
- 19.Lai TYY, Chan W, Li H, Lai RYK, Liu DTL, Lam DSC. Safety enhanced photodynamic therapy with half dose verteporfin for chronic central serous chorioretinopathy: a short term pilot study. Br J Ophthalmol. 2006;90(7):869–874. doi: 10.1136/bjo.2006.090282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nicoló M, Eandi CM, Alovisi C, Grignolo FM, Traverso CE, Musetti D, Cardillo Piccolino F. Half-fluence versus half-dose photodynamic therapy in chronic central serous chorioretinopathy. Am J Ophthalmol. 2014;157(5):1033–1037. doi: 10.1016/j.ajo.2014.01.022. [DOI] [PubMed] [Google Scholar]
- 21.Kim YK, Ryoo NK, Woo SJ, Park KH. Comparison of visual and anatomical outcomes of half-fluence and half-dose photodynamic therapy in eyes with chronic central serous chorioretinopathy. Graefes Arch Clin Exp Ophthalmol. 2015;253(12):2063–2073. doi: 10.1007/s00417-014-2926-6. [DOI] [PubMed] [Google Scholar]
- 22.Mammo Z, Forooghian F. Incidence of acute exudative maculopathy after reduced-fluence photodynamic therapy. Retin Cases Brief Rep. 2017;11(3):217–220. doi: 10.1097/ICB.0000000000000356. [DOI] [PubMed] [Google Scholar]
- 23.Michels S, Hansmann F, Geitzenauer W, Schmidt-Erfurth U. Influence of treatment parameters on selectivity of verteporfin therapy. Invest Ophthalmol Vis Sci. 2006;47(1):371–376. doi: 10.1167/iovs.05-0354. [DOI] [PubMed] [Google Scholar]
- 24.Lin D, Chen W, Zhang G, Huang H, Zhou Z, Cen L, Chen H. Comparison of the optical coherence tomographic characters between acute Vogt-Koyanagi Harada disease and acute central serous chorioretinopathy. BMC Ophthalmol. 2014;14:87. doi: 10.1186/1471-2415-14-87. [DOI] [PMC free article] [PubMed] [Google Scholar]


