Abstract
This study compares reports from 2 next-generation sequencing tests to determine the level of concordance between platforms.
The growing use of next generation-sequencing to identify cancer-associated alterations as well as the increasing number of targeted drugs holds promise for better matching patients with cancer with effective therapies. The FoundationOne (F1; Foundation Medicine) test sequences clinical tumor samples to characterize the exons of 315 cancer-associated genes and introns from 28 genes involved in rearrangements. The Guardant360 (G360; Guardant Health) test uses cell-free circulating DNA from blood to sequence 70 genes. Both the F1 and G360 tests have high specificities (>99%) and somewhat lower sensitivities. However, little is known about how different next-generation sequencing tests compare when used in the same patients with cancer. We compared reports from F1 and G360 testing in 9 patients from a community oncology practice to determine the level of concordance between the platforms.
Methods
This study was approved by the University of Washington Institutional Review Board. Patients consented to the study, titled “A Tumor Crowd Modeling Platform for Patients with Cancer,” via an online patient information statement. Nine patients (mean [SD] age, 61 [19] years; 2 men and 7 women) underwent both F1 and G360 testing from April 14, 2015, to January 30, 2016. Patient reports from results of F1 tumor and G360 circulating tumor DNA testing were examined to generate a list of all genomic alterations detected by either assay and to assess concordance between reports. Reports from results of F1 and G360 testing were also assessed to compare recommended drugs. Recommended clinical trials from the reports were not compared owing to the wide variation in the criteria used to select trials. We limited comparisons to alterations identifiable by both F1 and G360 testing, and resolved uncertainties by contacting representatives of Foundation Medicine and Guardant Health, respectively. Statistical analysis used Fisher exact test and nonparametric Mann-Whitney inference testing.
Results
The Table displays the clinical characteristics of the patients and reported alterations and drugs. One patient had no identified genetic alteration using either platform. The remaining 8 patients had 45 alterations, only 10 (22%) of which were concordant between the platforms. For 2 of these remaining 8 patients, there was no concordance among the described alterations. For these 8 patients, a total of 36 drugs were mentioned. However, only 9 drugs (25%) were recommended for the same patients by both platforms, and in 5 patients, there was no overlap between the drugs recommended by the F1 test and those recommended by the G360 test. Concordance among drugs improved to 8 of 13 (62%) when reported mutations were also concordant.
Table. Clinical Characteristics, Numbers of Genetic Alterations and Drugs Mentioned in F1 and G360 Reports, and Concordance Between Reports From F1 and G360 Testing.
| Patient Characteristic | All Mutations Reported by at Least 1 Platform (n = 112) |
Mutations Detectable by Both Platforms (n = 45) |
Drugs Recommended by at Least 1 Platform (n = 36) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient No./Sex | Tumor Type | Stage | Time Difference, mo | F1 or G360, No. | Both, No. (%) | F1, No. | Both, No. (%) |
F1, No. | G360, No. | F1 or G360, No. | F1 and G360, No. (%) |
F1, No. | G360, No. |
| 1/F | Breast cancer | IV | 0.5 | 13 | 7 (54) | 6 | 1/7 (14) | 1 | 5 | 2 | 0 | 2 | 0 |
| 2/F | Pancreatic cancer | IV | 1 | 16 | 4 (25) | 12 | 1/4 (25) | 3 | 0 | 2 | 0 | 2 | 0 |
| 3/F | Breast cancer | IV | 15 | 8 | 5 (63) | 3 | 0 | 2 | 3 | 2 | 0 | 0 | 2 |
| 4/F | Thymic carcinoma | I | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 5/F | Breast cancer | IV | 0 | 9 | 5 (56) | 4 | 2/5 (40) | 1 | 2 | 7 | 4/7 (57) | 2 | 1 |
| 6/F | Breast cancer | IV | 0.5 | 19 | 4 (21) | 15 | 0 | 2 | 2 | 3 | 0 | 2 | 1 |
| 7/M | Lung cancer | IV | 1 | 18 | 7 (39) | 11 | 1/7 (14) | 1 | 5 | 11 | 1/11 (9) | 1 | 9a |
| 8/M | Salivary gland cancer | IV | 2.5 | 10 | 2 (20) | 8 | 2 (100) | 0 | 0 | 2 | 0 | 2 | 0 |
| 9/F | Breast cancer | III | 0 | 19 | 11 (58) | 8 | 3/11 (27) | 3 | 5 | 7 | 4/7 (57) | 0 | 3 |
| Total | 112 | 45 (40) | 67b | 10/45 (22) | 13 | 22 | 36 | 9/36 (25) | 11 | 16 | |||
Abbreviations: F1, FoundationOne; G360, Guardant360.
A recommendation of other KIT proto-oncogene receptor tyrosine kinase inhibitors was counted as a single drug.
The 67 alterations detectable owing to technical differences only by F1 testing were excluded from the analysis to avoid an exaggerated portrayal of discordance.
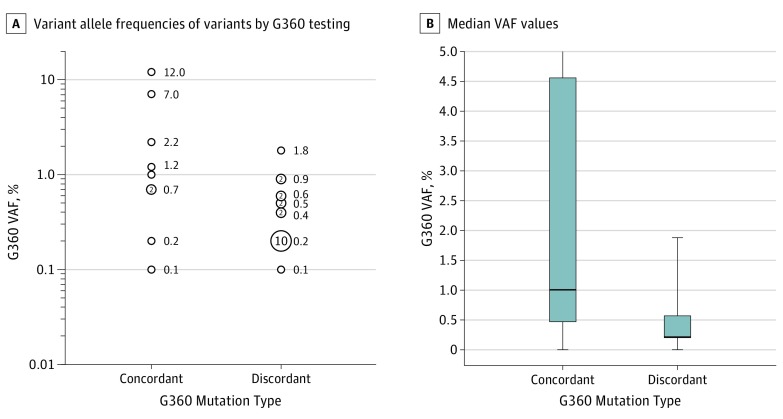
We expected that relatively high-frequency alterations identified by G360 testing would be more likely captured in tumor tissues examined by F1 testing. Consistent with this expectation, discordant alterations in results of G360 testing were more likely to have variant allele frequencies less than 1% (19 of 20 mutations, with 2 mutations without reported variant allele frequencies), compared with concordant G360 alterations (4 of 9 mutations, with 1 mutation without reported variant allele frequencies; P = .005) (Figure, A) and the distribution of variant allele frequencies was lower relative to concordant alterations (P = .02) (Figure, B). However, concordance among alterations improved only slightly (to 5 of 18 [28%]) when comparisons were limited to variant allele frequencies of 1% or more.
Figure. Association Between Variant Allele Frequencies (VAFs) of Variants Identified by G360 and Concordance With F1 Testing.
A, Distributions of VAFs for variants identified by G360 testing that are concordant (n = 10) or discordant (n = 22) with F1 results. Numbers of mutations are depicted by the size of the circles. Circles without numbers denote single mutations. Among variants identified by G360, discordance with F1 results is significantly more likely at VAFs of less than 1% (P = .005; Fisher exact test, 2-sided). When limiting variants identified by G360 to those with VAFs of 1% or more, 5 of 10 concordant mutations remain, whereas only 1 of the 22 discordant mutations remain. For 3 G360 mutations, VAFs were not provided in patient reports for 3 mutations and are, therefore, not displayed; of these, 2 mutations were discordant and 1 mutation was concordant with F1 results. B, Box plots display the median VAFs (black horizontal lines indicate the 50th percentile), interquartile range (box plots indicate the 25th-75th percentile), and minimum and maximum VAF values (whiskers). The maximum VAF for concordant mutations fell outside the displayed range, at 12%. Discordant mutations have a significantly lower median VAF relative to concordant mutations (P = .02; Mann-Whitney test for a nonparametric comparison). Median VAFs for concordant and discordant G360 mutations are 1.0% and 0.2%, respectively. Mean VAFs for concordant and discordant G360 mutations are 2.8% and 0.4%, respectively.
Discussion
Our findings indicate that the output from genetic testing can differ markedly depending on which genetic test is applied. Since both the F1 and the G360 tests are performed in thousands of patients with cancer each year, these findings are clinically relevant.
A major cause of discordance beyond that described here is that F1 testing detects a much broader range of aberrations than that accommodated by G360 testing. However, we excluded the alterations that are unique to F1 testing from our analysis; therefore, the discordance we describe comes from other causes. Differences in timing between the 2 tests may cause discordance; however, 7 of the 8 patients with alterations underwent both tests within a 2½-month period. Tumor heterogeneity and differences in the processes used to determine whether a variant is reported are also likely contributors to discordance.
Although reports from G360 testing frequently include relatively low-frequency variants, many alterations are likely present in only a small fraction of tumor cells, as supported by our finding that discordance between F1 and G360 testing declines after restricting comparisons to variants found via G360 testing present at frequencies of greater than 1%.
Although these results are preliminary, significant discordance also has been noted between reports comparing tissue-based next-generation sequencing tests and, in a recent report, between results from F1 and G360 testing. Our findings indicate that in-depth comparisons of next-generation sequencing tests across larger numbers of patients with cancer are needed to improve concordance and clinical utility.
References
- 1.Frampton GM, Fichtenholtz A, Otto GA, et al. . Development and validation of a clinical cancer genomic profiling test based on massively parallel DNA sequencing. Nat Biotechnol. 2013;31(11):1023-1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lanman RB, Mortimer SA, Zill OA, et al. . Analytical and clinical validation of a digital sequencing panel for quantitative, highly accurate evaluation of cell-free circulating tumor DNA. PLoS One. 2015;10(10):e0140712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gerlinger M, Rowan AJ, Horswell S, et al. . Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. N Engl J Med. 2012;366(10):883-892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weiss GJ, Hoff BR, Whitehead RP, et al. . Evaluation and comparison of two commercially available targeted next-generation sequencing platforms to assist oncology decision making. Onco Targets Ther. 2015;8:959-967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Squillace RM, Frampton GM, Stephens PJ, Ross JS, Miller VA. Comparing two assays for clinical genomic profiling: the devil is in the data. Onco Targets Ther. 2015;8:2237-2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chae YK, Davis AA, Carneiro BA, et al. . Concordance between genomic alterations assessed by next-generation sequencing in tumor tissue or circulating cell-free DNA [published online August 30, 2016]. Oncotarget. doi: 10.18632/oncotarget.11692 [DOI] [PMC free article] [PubMed] [Google Scholar]