Abstract
Both microscopic and endoscopic transsphenoidal surgery are effective approaches for nonfunctioning pituitary adenomas. The issue on the comparison of their efficacy and safety remains inconsistent. A thorough search of the literatures (PubMed, EMBASE, MEDLINE) were performed up to March 2017. Studies reporting outcomes of microscopic or endoscopic transsphenoidal surgery on nonfunctioning pituitary adenomas were included. A meta‐analysis was performed focusing on the early stage and long term outcomes. The final search yielded 19 eligible studies enrolling 3847 patients, 389 of them underwent microscopic approach and 3458 of them with endoscopic approach. As to the early stage outcomes, the rate of gross tumor resection was significantly higher in the endoscopic group than that in microscopic group (73% versus 60%, P < 0.001). Meanwhile, endoscopic approach showed priority over microscopy on postoperative hypopituitarism (63% versus 65%, P < 0.001) and CSF leakage (3% versus 7%, P < 0.001). For the long term outcomes, the rate of visual improvement was significant higher in the endoscopic group than that in microscopic group (77% versus 50%, P < 0.001). However, there was no significant difference between the groups regarding the rate of permanent diabetic insipidus and meningitis. The endoscopic approach may be associated with higher rate of gross tumor movement and lower risk of postoperatively complications for treating nonfunctioning pituitary adenoma, when compared with microscopic approach. However, the confidence was shorted due to limited high quality evidence (largely randomized and controlled studies).
Keywords: meta‐analysis, nonfunctioning pituitary adenoma, endoscopic, microscopic, transsphenoidal
Introduction
Non‐functioning pituitary adenoma (NFPA) is the most common phenotype of pituitary adenomas with considerable morbidity because of hypopituitarism and mass effect 1. In contrast to the prolactin and growth hormone‐secreting pituitary adenomas, none of effective drugs are available for NFPA, and transsphenoidal surgical resection remains the first‐line treatment 1. However, total resection of these lesions is challengeable because of the involvement of cavernous sinus. Moreover, the tumour‐associated hypopituitarism is another serious issue needed to be addressed, as the post‐operative hypopituitarism has been shown to contribute to an overall excess mortality in women 2. Therefore, surgical resection is significantly vital for the prognosis of patients with NFPA, to increase the rate of gross total resection (GTR) and eliminate the frequency of post‐operative hypopituitarism are the two most important issues needed to be addressed 1.
The microscopic transsphenoidal approach has long been taken as a standard procedure to manage NFPA, which has been challenged by the popular of endoscopic approach 3. With improved visualization, endoscopic approach provides a wider and superior picture of the parasellar and suprasellar compartments, which may gain access to improve the rate of GTR, protection of normal pituitary tissue, and thus reduce post‐operative complications 3. Previous studies have systemically reviewed the outcome of endoscopic and microscopic approach among either all the subtypes of pituitary adenomas 4, 5 or growth hormone‐secreting pituitary adenomas 6. As we mentioned before, NFPA is a unique entity, where cavernous compartments are more commonly involved and surgical resection plays a much more crucial role. However, whether endoscopic approach demonstrates priority over microscopic approach in treating NFPA remains inconsistent 7. We thus performed a meta‐analysis focusing on the outcome and complications of microscopic and endoscopic transsphenoidal resection of NFPA.
Materials and methods
Literature search strategy
A systematic search of PubMed, EMBASE, MEDLINE and references of all the retained studies were reviewed for any related articles ranging from the January 2000 to March 2017. The following searching terms were used to extract all the relative articles, non‐functioning, pituitary, neoplasm, adenoma, endoscopic, endoscopy, microscopic, transsphenoidal and surgery.
Inclusion and exclusion criteria
Studies were included if they matched the following criteria, (i) A comparison article between endoscopic and microscopic approach for non‐functioning pituitary adenoma. (ii) Retrospective studies or single‐armed studies observing the outcome of either endoscopic or microscopic approach. (iii) Studies consisted of no less than 10 samples. (iv) Duplicated reports of the same population or increased lengths of follow‐up, only the most complete studies were included. Studies were excluded if they had any of the following characteristics, (i) Endoscopic‐assisted comparison studies. (ii) Studies lack information of the efficacy and complications following operation. (iii) Studies published in other languages except English.
Outcome interests and statistics analysis
The early stage (GTR, CSF leak, hypopituitarism and meningitis) and long‐term outcomes (visual improvement and permanent diabetic insipidus (DI)) after the resection of NFPA were systemic evaluated.
Chi‐square test and I 2 were used to evaluate the heterogeneity among the studies towards each index. A random effect model or fixed effect model was applied for meta‐analysis with (P < 0.05, I 2 > 50%) or without heterogeneity (P > 0.05, I 2 < 50%), respectively. The comparison of the outcome between the endoscopic and microscopic approaches was tested using SPSS 19.0 (Chicago, IL, USA), P < 0.05 was considered as significant difference. Systematic analysis was conducted with the software, Review Manager 4.2 (Revman, The Cochrane Collaboration, Oxford, UK).
Results
A total of 824 articles were initially included, 745 of them were removed as a result of unrelated content or not published in English. Then, the left 79 articles went through full‐text reviewing. Eventually, 19 studies were included in the final analysis, enrolling 389 patients underwent microscopic transsphenoidal resection and 3458 patients with endoscopic approach. Four of which directly compared endoscopic and microscopic approaches 7, 8, 9, 10, while the other 15 articles are single‐armed studies 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, reporting purely endoscopic or microscopic transsphenoidal surgery on NFPA 11, 12, 13, 14, 15, 16, 17, 18, 20, 21, 22, 23. The proportion of gender, the presence of pre‐operatively hypopituitarism, visual deficiency and invasive tumours were significant different between the two groups (Table 1).
Table 1.
Patient and tumour features in studies on endoscopic/microscopic approach for non‐functioning pituitary adenomas
| Number of endoscopic/microscopic studies | Number of endoscopic/microscopic patients | Endoscopic pooled proportion (95%CI) | I 2% (P value for heterogeneity) | Microscopic pooled proportion (95%CI) | I 2% (P value for heterogeneity) | P value for difference | |
|---|---|---|---|---|---|---|---|
| Patient characteristics | |||||||
| Age | 11/5 | 1381/389 | 57.73 (51.35–56.10) | 0 (0.972) | 56.22 (54.07–58.37) | 0 (0.971) | 0.580 |
| Males% | 19/5 | 3458/389 | 57 (54–60) | 62.8 (<0.001) | 63 (58–68) | 17.1 (0.305) | 0.024 |
| Presenting symptoms | |||||||
| Hypopituitarism% | 8/3 | 892/269 | 48 (28–68) | 97.9 (<0.001) | 23 (9–37) | 86.5 (0.001) | <0.001 |
| Pre‐operative visual deficit% | 13/2 | 2200/226 | 57 (49–65) | 92.7 (<0.001) | 67.4 (0.080) | 44 (33–56) | <0.001 |
| Tumour characteristics | |||||||
| Macroadenoma% | 7/2 | 1030/167 | 86 (76–95) | 77.5 (0.012) | 63 (53–73) | 0 (<0.001) | <0.001 |
| Superasellae invasion% | 4/1 | 967/144 | 53 (6–100) | 99.5 (<0.001) | 11 | NA | <0.001 |
| Intrasellae/Clinvus invasion% | 3/1 | 476/144 | 55 (−20–131) | 99.5 (<0.001) | 12 | NA | <0.001 |
| Knosp score 0–2% | 10/4 | 2216/354 | 45 (36–55) | 94.9 (<0.001) | 45 (29–60) | 89.4 (<0.001) | 0.979 |
| Knosp score 3–4% | 10/4 | 2216/354 | 55 (45–64) | 94.9 (<0.001) | 55 (40–71) | 89.4 (<0.001) | 0.979 |
| Maximum tumour diameter (mm) | 9/2 | 1576/226 | 27.15 (16.35–37.95) | 0 (0.971) | 27.65 (10.50–44.80) | 0 (0.868) | 0.548 |
For the earl‐stage outcome, the rate of GTR was significantly higher in the endoscopic group than that in the microscopic group (P < 0.001; Fig. 1A). The rate of hypopituitarism (Fig. 1B) and CSF leak (Fig. 1C) in endoscopic group were less likely present than that in the microscopic group (P < 0.001). As to the long‐term outcome, patients endoscopically treated had a significantly higher rate of visual improvement than those treated with microscopy (P < 0.001; Fig. 1D). The rate of post‐operative permanent DI was comparable in the two groups.
Figure 1.
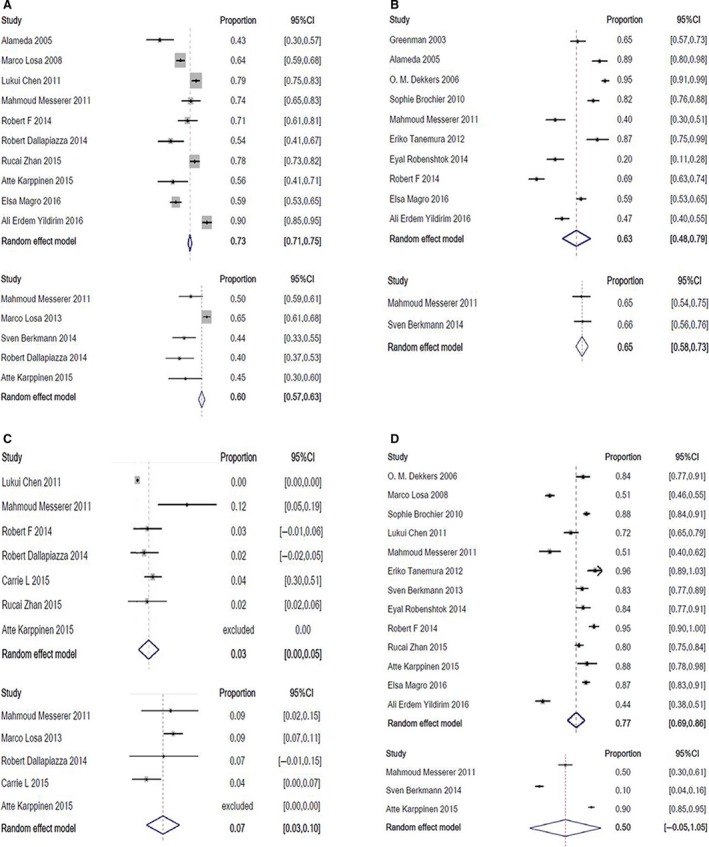
Pooled proportion of GTR (A), hypopituitarism (B), CSF leak (C) and postoperative visual improvement (D) of endoscopic (upper) and microscopic (lower) transsphenoidal resection of non‐functioning pituitary adenomas.
Discussion
The merits and disadvantages of endoscopic and microscopic transsphenoidal pituitary adenoma resection have been evaluated in several previous studies 4, 5, 6. However, the comparison of endoscopic and microscopic transsphenoidal resection specifically on NFPA has never been systematically performed before. In this study, the pooled data showed that patients with NFPA endoscopically treated tended to have higher rate of GTR and visual improvement, as well as lower percentage of post‐operative hypopituitarism and CSF leak.
Similarly, in the meta‐analysis performed by Gao et al., the rate of GTR was higher in the endoscopic group than that in the microscopic group, as well as less frequency perforation in patients underwent endoscopic surgery 4. In consistence, Li et al. concluded that endoscopic transsphenoidal surgery was associated with higher incidence of GTR 5. A major prognostic factor for the resection outcome and recurrence of a pituitary adenoma is its parasellar extension, particularly into the space of the cavernous sinus. With the panoramic visualization, endoscopy provides a wider and superior pathway to the area of parasellar and suprasellar compartments, which may gain access to improve the rate of GTR, protection of normal pituitary tissue and thus reduce postoperative complications 5.
Benefit from the progress of reconstructive techniques, the incidence of post‐operative CSF leak obviously decreased 24. In addition, endoscopy appeared to be more sensitive to identify CSF leak intra‐operatively and perform reconstruction of sellae 6. This may help to explain the lower rate of postoperatively CSF leak in endoscopic group in this study.
Still, we should note that our systematic review and meta‐analysis still have some limitations in need of further investigation. First, significant heterogeneity was noted in the majority of the studies in baseline information of patients (Table 1). Second, a large number of related studies were excluded from this studies, as they enrolled all subtypes of pituitary adenomas, where the particular data on NFPA were not available. Apart from this, the significant weakness of this study was lack of evidence of grade II and III. Thus, more randomized trials with large‐scale cohort of patients are warranted to help determine the efficacy of microscopic and endoscopic transsphenoidal surgery in treating NFPA.
Conflict of interest
The authors declare that they have no conflict of interest.
Acknowledgements
This work is supported by the Special Funds for the Cultivation of Guangdong College Students Scientific and Technological Innovation (Climbing Programme Special Funds, 2017), and the Medical Scientific Research Foundation of Guangdong Province (A2017188).
Contributor Information
Jian Wang, Email: wangjian2@sysucc.org.cn.
Xiao‐Bing Jiang, Email: jiangxiaob1@sysucc.org.cn.
References
- 1. Aghi MK, Chen CC, Fleseriu M, et al Congress of neurological surgeons systematic review and evidence‐based guidelines on the management of patients with nonfunctioning pituitary adenomas: executive summary. Neurosurgery. 2016; 79: 521–3. [DOI] [PubMed] [Google Scholar]
- 2. Olsson DS, Nilsson AG, Bryngelsson IL, et al Excess mortality in women and young adults with nonfunctioning pituitary adenoma: a Swedish nationwide study. J Clin Endocrinol Metab. 2015; 100: 2651–8. [DOI] [PubMed] [Google Scholar]
- 3. Zaidi HA, Awad AW, Bohl MA, et al Comparison of outcomes between a less experienced surgeon using a fully endoscopic technique and a very experienced surgeon using a microscopic transsphenoidal technique for pituitary adenoma. J Neurosurg. 2016; 124: 596–604. [DOI] [PubMed] [Google Scholar]
- 4. Gao Y, Zhong C, Wang Y, et al Endoscopic versus microscopic transsphenoidal pituitary adenoma surgery: a meta‐analysis. World J Surg Oncol. 2014; 12: 94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Li A, Liu W, Cao P, et al Endoscopic versus microscopic transsphenoidal surgery in the treatment of pituitary adenoma: a systematic review and meta‐analysis. World Neurosurg. 2017; 101: 236–46. [DOI] [PubMed] [Google Scholar]
- 6. Phan K, Xu J, Reddy R, et al Endoscopic endonasal versus microsurgical transsphenoidal approach for growth hormone‐secreting pituitary adenomas‐systematic review and meta‐analysis. World Neurosurg. 2017; 97: 398–406. [DOI] [PubMed] [Google Scholar]
- 7. Dallapiazza R, Bond AE, Grober Y, et al Retrospective analysis of a concurrent series of microscopic versus endoscopic transsphenoidal surgeries for Knosp Grades 0‐2 nonfunctioning pituitary macroadenomas at a single institution. J Neurosurg. 2014; 121: 511–7. [DOI] [PubMed] [Google Scholar]
- 8. Pledger CL, Elzoghby MA, Oldfield EH, et al Prospective comparison of sinonasal outcomes after microscopic sublabial or endoscopic endonasal transsphenoidal surgery for nonfunctioning pituitary adenomas. J Neurosurg. 2016; 125: 323–33. [DOI] [PubMed] [Google Scholar]
- 9. Karppinen A, Kivipelto L, Vehkavaara S, et al Transition from microscopic to endoscopic transsphenoidal surgery for nonfunctional pituitary adenomas. World Neurosurg. 2015; 84: 48–57. [DOI] [PubMed] [Google Scholar]
- 10. Messerer M, De Battista JC, Raverot G, et al Evidence of improved surgical outcome following endoscopy for nonfunctioning pituitary adenoma removal. Neurosurg Focus. 2011; 30: E11. [DOI] [PubMed] [Google Scholar]
- 11. Greenman Y, Ouaknine G, Veshchev I, et al Postoperative surveillance of clinically nonfunctioning pituitary macroadenomas: markers of tumour quiescence and regrowth. Clin Endocrinol (Oxf). 2003; 58: 763–9. [DOI] [PubMed] [Google Scholar]
- 12. Dekkers OM, Pereira AM, Roelfsema F, et al Observation alone after transsphenoidal surgery for nonfunctioning pituitary macroadenoma. J Clin Endocrinol Metab. 2006; 91: 1796–801. [DOI] [PubMed] [Google Scholar]
- 13. Brochier S, Galland F, Kujas M, et al Factors predicting relapse of nonfunctioning pituitary macroadenomas after neurosurgery: a study of 142 patients. Eur J Endocrinol. 2010; 163: 193–200. [DOI] [PubMed] [Google Scholar]
- 14. Chen L, White WL, Spetzler RF, et al A prospective study of nonfunctioning pituitary adenomas: presentation, management, and clinical outcome. J Neuro Oncol. 2011; 102: 129–38. [DOI] [PubMed] [Google Scholar]
- 15. Tanemura E, Nagatani T, Aimi Y, et al Quality of life in nonfunctioning pituitary macroadenoma patients before and after surgical treatment. Acta Neurochir. 2012; 154: 1895–902. [DOI] [PubMed] [Google Scholar]
- 16. Losa M, Donofrio CA, Barzaghi R, et al Presentation and surgical results of incidentally discovered nonfunctioning pituitary adenomas: evidence for a better outcome independently of other patients' characteristics. Eur J Endocrinol. 2013; 169: 735–42. [DOI] [PubMed] [Google Scholar]
- 17. Berkmann S, Schlaffer S, Buchfelder M. Tumor shrinkage after transsphenoidal surgery for nonfunctioning pituitary adenoma. J Neurosurg. 2013; 119: 1447–52. [DOI] [PubMed] [Google Scholar]
- 18. Robenshtok E, Benbassat C, Hirsch D, et al Clinical course and outcome of nonfunctioning pituitary adenomas in the elderly compared with younger age groups. Endocr Pract. 2014; 20: 159–64. [DOI] [PubMed] [Google Scholar]
- 19. Berkmann S, Schlaffer S, Nimsky C, et al Follow‐up and long‐term outcome of nonfunctioning pituitary adenoma operated by transsphenoidal surgery with intraoperative high‐field magnetic resonance imaging. Acta Neurochir. 2014; 156: 2233–43. [DOI] [PubMed] [Google Scholar]
- 20. Yildirim AE, Sahinoglu M, Ekici I, et al Nonfunctioning pituitary adenomas are really clinically nonfunctioning? clinical and endocrinological symptoms and outcomes with endoscopic endonasal treatment. World Neurosurg. 2016; 85: 185–92. [DOI] [PubMed] [Google Scholar]
- 21. Alameda C, Lucas T, Pineda E, et al Experience in management of 51 non‐functioning pituitary adenomas: indications for post‐operative radiotherapy. J Endocrinol Invest. 2005; 28: 18–22. [DOI] [PubMed] [Google Scholar]
- 22. Magro E, Graillon T, Lassave J, et al Complications related to the endoscopic endonasal transsphenoidal approach for nonfunctioning pituitary macroadenomas in 300 consecutive patients. World Neurosurg. 2016; 89: 442–53. [DOI] [PubMed] [Google Scholar]
- 23. Zhan R, Ma Z, Wang D, et al Pure endoscopic endonasal transsphenoidal approach for nonfunctioning pituitary adenomas in the elderly: surgical outcomes and complications in 158 patients. World Neurosurg. 2015; 84: 1572–8. [DOI] [PubMed] [Google Scholar]
- 24. Sigler AC, D'Anza B, Lobo BC, et al Endoscopic skull base reconstruction: an evolution of materials and methods. Otolaryngol Clin North Am. 2017; 50: 643–53. [DOI] [PubMed] [Google Scholar]


