Abstract
Cutaneous horns (cornu cutaneum) are uncommon lesions consisting of keratotic material resembling that of an animal horn. It is a conical- or cylindrical-shaped excessive hyperkeratosis of variable size ranging from few millimeters to several centimeters with a variable in size and shape, such as cylindrical, conical, pointed, transversely or longitudinally corrugated, or curved like a ram's horn. The lesions typically occur in sun-exposed areas, particularly the face, ear, nose, forearms and dorsum of hands. Even though 60% of the cutaneous horns are benign in nature, the possibility of skin cancer should always be kept in mind. The clinical diagnosis includes various benign and malignant lesions at its base. Lesions associated with cutaneous horn are keratosis, sebaceous molluscum, verruca, trichilemmal, Bowen's disease, epidermoid carcinoma, malignant melanoma and basal cell carcinoma. Herewith, we report a case of cutaneous horn on the upper lip vermillion masking the underlying malignancy at its base.
Keywords: Base of the lesion, cutaneous horn, verrucous carcinoma
INTRODUCTION
Cutaneous horns (cornu cutaneum) are uncommon lesions consisting of keratotic material resembling that of an animal horn. Cutaneous horn may arise from a wide range of the epidermal lesions, which may be benign, premalignant or malignant. Cutaneous horn is a clinical diagnosis that refers to a conical projection above the surface of the skin. The lesions typically occur in sun-exposed areas, particularly the face, ear, nose, forearms and dorsum of hands. Even though 60% of the cutaneous horns are benign, the possibility of skin cancer should always be kept in mind. Cutaneous horns can be variable in size and shape, such as cylindrical, conical, pointed, transversely or longitudinally corrugated, or curved like a ram's horn.[1]
The term “cutaneous horn” does not indicate any specific pathological diagnosis. Microscopically, it shows dense compaction of cohesive keratinized material with its base exhibiting various histological entities including benign, premalignant or malignant lesions. Therefore, for appropriate histopathological diagnosis, such a lesion should undergo biopsy at the base of the horn, and for smaller lesions, excision should be considered.[2]
This is a case report of cutaneous horn of upper lip vermillion with verrucous carcinoma at its base.
CASE REPORT
A59-year-old male reported with a chief complaint of a growth on the left side of upper lip. The lesion had been present for the last 6 months with gradual increase in size. Previously, the patient had undergone surgical excision of the lesion twice in the same area from an outside clinic only to notice it regrow again. He had the habit of smoking cigarettes for the past 25 years, around 20 cigarettes per day. The patient also gave a history of anemia for the past 1 month and was taking folic acid medication regularly. No other signs and symptoms were present.
On close clinical examination, an exophytic growth was seen on the left corner of upper lip. The growth was about 1.5 cm in length and was brown. On palpation, the growth was firm to hard in consistency and was slightly tender. Intraoral examination revealed a grayish-white patch on the left commissural mucosa and the dorsum of tongue measuring about 3 cm × 1 cm in dimension. Both the white patches were nontender and nonscrapable in nature. Hard tissue examination revealed several missing teeth (15, 16, 17, 25, 26, 27 and 46) and Grade II mobility with respect to teeth (11, 21, 22, 23, 31, 41, 42 and 47). Generalized gingival recession and attrition were also seen in Figure 1.
Figure 1.

Clinical presentation of cutaneous horn on upper lip vermillion
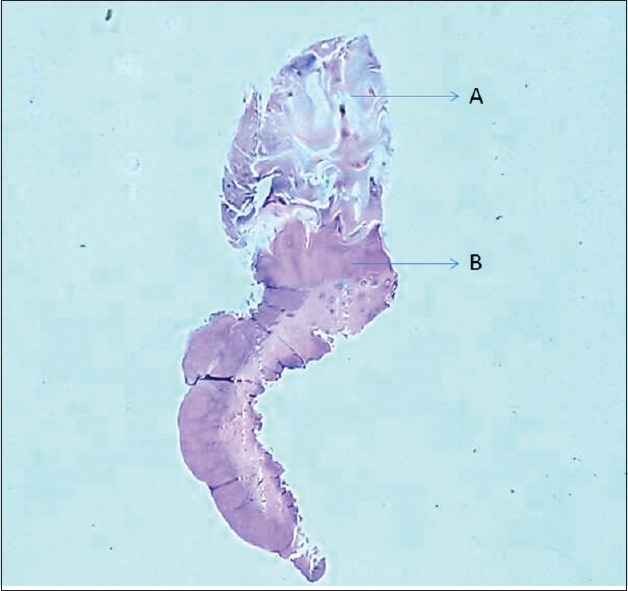
Excision of the lesion on the lip along with its adjacent grayish-white patch was done using CO2 laser. Satisfactory healing was observed after a week. The gross specimen received measured about 28 mm × 7 mm × 4 mm. One end of the specimen was soft in consistency, and the other end was firm which represents the horn [Figure 2].
Figure 2.

Gross specimen A. Cutaneous horn with base - cut surface B. Excised tissue from adjacent area
The histological sections revealed hyperkeratotic stratified squamous epithelium with underlying connective tissue. The epithelium exhibited acanthosis, spongiosis, hyperkeratosis and broad rete pegs with pushing margins along with parakeratinized keratin plugging. The underlying connective tissue exhibited mild inflammatory cell infiltration, areas of hemorrhage and muscle fibers bundles in cross sections [Figure 3]. The superficial layer of epithelium in one area showed exuberant keratinization in concentric layers forming a cutaneous horn [Figure 4]. The final diagnosis was given as cutaneous horn with underlying verrucous carcinoma. Histopathologic sections from the tissue adjacent to the cutaneous horn showed features of mild-to-moderate dysplasia.
Figure 3.
Stereo microscopic view of the lesion A. horn with compaction of keratin B. verrucous carcinoma at the base
Figure 4.
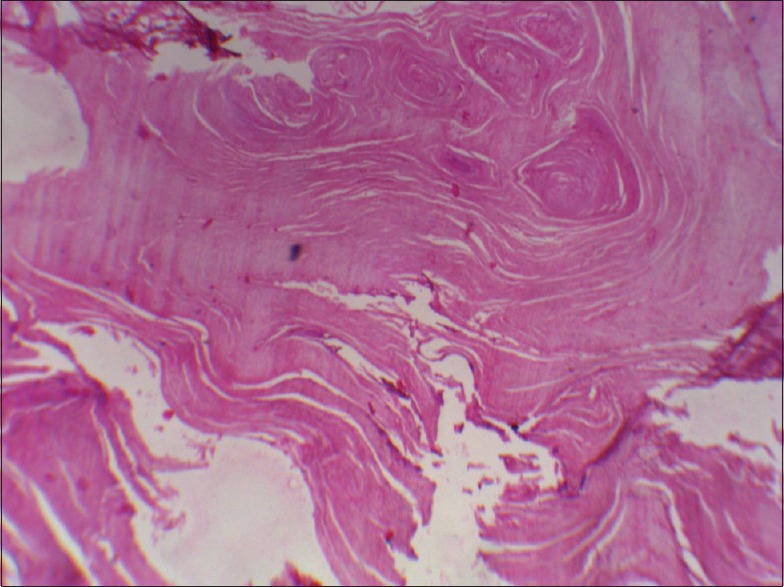
Magnified view of horn showing compact concentric layers of cohesive keratinized material
DISCUSSION
Cutaneous horn is a circumscribed, conical- or cylindrical-shaped excessive hyperkeratosis of variable size ranging from few millimeters to several centimeters. Cutaneous horns, although grossly similar to horns in animals, the former is histologically quite different from animal horn. The animal horns are composed of superficial hyperkeratotic epidermis, dermis and centrally positioned bone. No such axially positioned well-formed bone is observed even in the gigantic human horns. On the other hand, no cystic structures lined by trichilemmal-type epithelium are seen in any of the true animal horns.[3] Histologically, the cutaneous horn shows an abundance of compact keratin protruding from the epidermis. Basal layer of epidermis in cutaneous horn may be derived from a plethora of epidermal lesions, which range from benign to malignant epidermal proliferations.[4]
Cutaneous horn is a clinical diagnosis and includes various benign and malignant lesions at its base.[2] Lesions associated with cutaneous horn include keratosis, sebaceous molluscum, verruca, trichilemma, Bowen's disease, epidermoid carcinoma, malignant melanoma and basal cell carcinoma.[5] Cutaneous horn is most commonly encountered in Caucasians. It is relatively rare in Asians and even rarer in Africans. The possible explanation for this racial predilection may be the presence of more amount melanin pigmentation in the skin of Asians and Africans, which performs a protective role against ultraviolet rays-induced damage to epidermal cells. Long-term sun exposure and immunodeficiency have also been implicated in causation of this lesion.[4]
A sex predilection has not been shown in the literature; however, the possibility of harboring malignancy at the base of the lesion is increased in men when compared with age-matched women.[6,7] Cutaneous horn occurs mainly in individuals who are above 50 years of age, in both sexes, probably due to a major actinic and neoplastic degeneration occurring in elderly people.[8] Studies describe that the average age of patients with premalignant and malignant lesions is around 6 years more than that of the patients with benign alterations; and therefore, the chances of finding a malignant substratum on the base of a cutaneous horn would increase proportionally with age.[9]
The earliest well-documented case of cornu cutaneum from London in 1588 is of Mrs. Margaret Gryffith, an elderly Welsh woman. A showman had advertised it in a pamphlet. However, earliest observations on cutaneous horns in humans were described by the London surgeon Everard Home in 1791.[10] The largest study of 643 cutaneous horns was reported by Yu et al.[8] According to them, 39% of cutaneous horns were derived from malignant or premalignant epidermal lesions, and 61% from benign lesions. Other two studies on cutaneous horn showed 23%–37% of these to be associated with actinic keratosis or Bowen's disease and another 16%–20% with malignant lesions.[8,11,12]
Among the 222 lesions examined by Mantese et al., 92 cutaneous horns(41.44%) presented benign histopathologic alterations on their bases being the most frequent: viral wart (29; 31.52%), keratic acanthoma (24; 26.09%), keratosis seborrhoeic (20; 21.74%), benign epithelial hyperplasia (6; 6.52%), trichilemmoma (3; 3.26%) and others (10; 10.87%). A total of 114 lesions (51.35%) were premalignant and 16 (7.21%) malignant.[12]
Cutaneous horns are more frequently located on the head and upper limbs, which are the areas frequently exposed to higher actinic damage. Lesions on the trunk and lower limbs are also observed but in smaller scale in the available literature. Some studies showed that benign lesions are most frequently found in areas less exposed to the sun, like the lower limbs. On the other hand, areas more exposed to the sun such as nose, dorsum of the hands, scalp, forearm and arm have twice more chances of presenting premalignant or malignant lesions on the base of the cutaneous horn when compared to any other part of the body.[10] Other series showed that the body areas where it is mostly common observed that is the upper regions of the face and cartilaginous portion of the ear are more commonly associated with malignancy.[11]
In our case, verrucous carcinoma was found at the base of the lesion. Verrucous carcinoma is a distinct variant of differentiated squamous cell carcinoma with low-grade malignancy, slow growth and no metastatic potential. It occurs in elderly patient around 60–70 years of age. It is first described by Ackerman, hence termed as “Ackerman's tumour.” Since it is closely associated with snuff and chewing tobacco it is also termed “snuff dipper's cancer.” The term verrucous is used because of its fine finger-like surface projections.[13] Common sites of verrucous carcinoma are buccal mucosa, gingiva, alveolar ridge, palate and floor of the mouth. Verrucous carcinoma affecting the lips is rare which is seen in this present case.[14]
Verrucous carcinoma is considered as a warty variant of squamous cell carcinoma characterized by a predominantly exophytic overgrowth of well-differentiated keratinizing epithelium having minimal atypia and with locally destructive pushing margins at its interface with underlying connective tissue. Even though the lesion may be very extensive, the basement membrane will often appear intact. Hence, sometimes because of these histological features the diagnosis of Verrucous carcinoma is understated.[15]
Likewise, in the present case, the intraoral lesion did not show any finger-like projections and the extraoral lesion was present on the vermillion border which showed the presence of cutaneous horn. Hence, the diagnosis was difficult.
Similarly, Kumar et al. reported a case of giant cutaneous horn of left oral commissure along with carcinoma left buccal mucosa.[16] Under general anesthesia and nasotracheal intubation, the patient underwent wide local excision of the buccal mucosa growth taking 1 cm margin along with excision of the conical cutaneous lesion with supraomohyoid neck dissection of the left cervical nodes. Primary closure of the defect was done in 3 layers. Postoperative period was uneventful, and the patient was discharged on postoperative day 5. Histopathological examination of the surgical specimen showed features consistent with verrucous carcinoma of buccal mucosa with hyperkeratosis of underlying the horn.[16] A similar case was also reported by Gupta et al.[17]
On review of the literature, nine cases in the past have been reported to have cutaneous horn over the lip, and three of these had an associated squamous cell carcinoma at its base. The important issue is not the horn itself which is dead keratin, but rather the underlying condition, which may be benign or a malignant lesion. Hence, from treatment aspect cutaneous horn should be carefully excised and sent for evaluation. It is important to remove adjacent tissue with full thickness of cutaneous horn as the underlying lesion is present beneath the cutaneous horn.[1,2,3,4,5,6,7,8,9,10]
As was observed in the present case, excision limiting only to the horn would lead to recurrence and also delay in definitive treatment of the underlying pathology.
CONCLUSION
Cutaneous horns are predominantly benign lesions; however, the possibility of nearly one-third of them harboring malignant or premalignant skin lesions should be borne in mind. Full-thickness excision with margin should be the treatment of choice to enable detailed pathological examination of the underlying tissue, thereby unmasking the underlying lesion.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Pyne J, Sapkota D, Wong JC. Cutaneous horns: Clues to invasive squamous cell carcinoma being present in the horn base. Dermatol Pract Concept. 2013;3:3–7. doi: 10.5826/dpc.0302a02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cristobal MC, Urbina F, Espinoza A. Cutaneous horn malignant melanoma. Dermatol Surg. 2007;33:997–9. doi: 10.1111/j.1524-4725.2007.33208.x. [DOI] [PubMed] [Google Scholar]
- 3.Michal M, Bisceglia M, Di Mattia A, Requena L, Fanburg-Smith JC, Mukensnabl P, et al. Gigantic cutaneous horns of the scalp: Lesions with a gross similarity to the horns of animals: A report of four cases. Am J Surg Pathol. 2002;26:789–94. doi: 10.1097/00000478-200206000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Sidram V, Chndrakumar P, Varun M, Raghavendra B. A rare case of cutaneous horn of scalp with squamous cell carcinoma in an elderly male: A case report. Int J Adv Case Rep. 2014;1:107–9. [Google Scholar]
- 5.Bondeson J. Everard home, john hunter, and cutaneous horns: A historical review. Am J Dermatopathol. 2001;23:362–9. doi: 10.1097/00000372-200108000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Akan M, Yildirim S, Avci G, Aköz T. Xeroderma pigmentosum with a giant cutaneous horn. Ann Plast Surg. 2001;46:665–6. doi: 10.1097/00000637-200106000-00029. [DOI] [PubMed] [Google Scholar]
- 7.Kneitz H, Motschenbacher S, Wobser M, Goebeler M. Photoletter to the editor: Giant cutaneous horn associated with squamous cell carcinoma. J Dermatol Case Rep. 2015;9:27–8. doi: 10.3315/jdcr.2015.1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yu RC, Pryce DW, Macfarlane AW, Stewart TW. A histopathological study of 643 cutaneous horns. Br J Dermatol. 1991;124:449–52. doi: 10.1111/j.1365-2133.1991.tb00624.x. [DOI] [PubMed] [Google Scholar]
- 9.Copcu E, Sivrioglu N, Culhaci N. Cutaneous horns: Are these lesions as innocent as they seem to be? World J Surg Oncol. 2004;2:18. doi: 10.1186/1477-7819-2-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Castillo D, Zerpa O, Loyo N, López C, Oliver M. Histopathology of the Horn Cutaneous: Retrospective Study of 77 Cases. Derm Venez. 2002;40:65–9. [Google Scholar]
- 11.Markie RM. Epidermal skin tumours. In: Champion RH, Burton JL, Ebling FJ, editors. Rook/Wilkinson/Ebling Textbook of Dermatology. 5th ed. Oxford: Blackwell Scientific Publications; 2004. pp. 1477–81. [Google Scholar]
- 12.Mantese SA, Diogo PM, Rocha A, Berbert AL, Ferreira AK, Ferreira TC, et al. Cutaneous horn: A retrospective histopathological study of 222 cases. An Bras Dermatol. 2010;85:157–63. doi: 10.1590/s0365-05962010000200005. [DOI] [PubMed] [Google Scholar]
- 13.McCoy JM, Waldron CA. Verrucous carcinoma of the oral cavity: A review of 49 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1981;52:623–9. doi: 10.1016/0030-4220(81)90081-5. [DOI] [PubMed] [Google Scholar]
- 14.Cleydon RJ, Jordan JE. Verrucous carcinoma of ackerman: A distinctive clinicopathologic entity; report of 2 cases. J Oral Surg. 1978;36:564–7. [PubMed] [Google Scholar]
- 15.Rajendran R. Shafer's Textbook of Oral Pathology. India: Elsevier; 2009. [Google Scholar]
- 16.Kumar S, Bijalwan P, Saini SK. Carcinoma buccal mucosa underlying a giant cutaneous horn: A case report and review of the literature. Case Rep Oncol Med 2014. 2014 doi: 10.1155/2014/518372. 518372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gupta R, Lavania P, Bansal VK, Agarwal N, Singh A. Cutaneous horn developing over a verrucous carcinoma: A rare entity with an unusual presentation. Int Surg J. 2016;3:988–90. [Google Scholar]


