Abstract
One of the four national HIV prevention goals is to incorporate combinations of effective, evidence-based approaches to prevent HIV infection. In fields of public health, techniques that alter environment and affect choice options are effective. Structural approaches may be effective in preventing HIV infection. Existing frameworks for structural interventions were lacking in breadth and/or depth. We conducted a systematic review and searched CDC’s HIV/AIDS Prevention Research Synthesis Project’s database for relevant interventions during 1988–2013. We used an iterative process to develop the taxonomy. We identified 213 structural interventions: Access (65%), Policy/Procedure (32%), Mass Media (29%), Physical Structure (27%), Capacity Building (24%), Community Mobilization (9%), and Social Determinants of Health (8%). Forty percent targeted high-risk populations (e.g., people who inject drugs [12%]). This paper describes a comprehensive, well-defined taxonomy of structural interventions with 7 categories and 20 subcategories. The taxonomy accommodated all interventions identified.
Keywords: structural interventions, HIV prevention, policy, social determinants of health, systematic review
Introduction
National HIV prevention goals [1] include the expansion of efforts to prevent HIV infection by using a combination of effective, evidence-based strategies. An updated, national goal [1] calls for adoption of structural approaches to reduce HIV infections and improve health outcomes in communities with high rates of infection as one of the steps to reducing HIV-related disparities and health inequities. Many public health outcomes are partly determined by individuals’ behaviors. Public health efforts to reduce the consequences of such behaviors often rely on appeals to individuals to change their behavior. However, other approaches have been developed and these strategies, one of which is referred to as “structural,” alter the environment in ways that facilitate or promote safer behaviors, or reduce risk in ways that do not rely on individual behavior change. Historically, major structural public health interventions have had large impacts.
Several HIV specialists have developed frameworks for classifying structural interventions for HIV prevention. However, they all consisted of a set of categories designed to be illustrative, rather than comprehensive. Sweat and Denison [2] proposed that behavior change interventions can produce change at any of four causal levels—individual, environmental, structural, and “superstructural”—and gave examples and change mechanisms for each. For example, superstructural interventions were defined as “macrosocial and political arrangements, resources, and power differences that result in unequal advantages.” Examples of such interventions might include “national and international social movements, revolution, land redistribution, war, and empowerment of disenfranchised populations.” Structural interventions were defined as “laws, policies, and standard operating procedures.”
Blankenship and colleagues [3] reviewed the literature available at the time and proposed nine categories of structural interventions based on contextual factors of availability, acceptability (e.g., campaigns shaming people committing unacceptable behavior, such as drug use), and accessibility. Similarly to the Sweat and Denison analysis, these authors gave examples of each at the individual, organizational, and environmental levels.
Sumartojo and colleagues [4], in the context of a special issue of AIDS resulting from a consultation organized by scientists (including the senior author of the current manuscript) at the Centers for Disease Control and Prevention (CDC), presented a table listing types of structural interventions (economic resources, policy supports, societal conditions, and organizational structures and functions) crossed with types of institutions (government, service organizations, private business, workforce organization, faith community, justice system, media, educational system, and the health care system) that could be a barrier or provide support. Again, these examples were not based on the extant literature, nor meant to be comprehensive.
In 2000, Cohen and Scribner [5] described four categories of structural interventions: Availability, Physical Structures, Social Structures, and Media Messages. In a later exposition by Blankenship and colleagues [6], structural interventions were categorized into four types: community mobilization, integration of HIV services, contingent funding, and economic and educational interventions; these four were largely mutually exclusive of the four specified by Cohen et al. [5]. Another such effort was undertaken by Tsai [7] who described structural interventions as existing along two dimensions: implementation intensity, and dependence of the effects on user agency. However, only a few examples were provided. Lastly, Kaufman and colleagues [8] noted stigma as an important factor that may influence HIV-related behavior. Other efforts at structural interventions to date have suffered the same issue of lacking comprehensiveness [9–13]. Moreover, a systematic process to categorize existing structural interventions was not attempted.
As we became immersed in the literature, we found the need for an all-inclusive framework to organize the different types of structural interventions. Therefore, we conducted a systematic review of the literature on structural interventions addressing HIV and developed a detailed and comprehensive taxonomy to enable categorization of every identified structural intervention. The purpose of this paper is to describe this new taxonomy in detail and to apply it to organize interventions identified through the systematic review.
Research Questions
This review addressed the following research questions.
What types of HIV prevention structural interventions are currently in the literature?
What are the outcomes of HIV prevention structural interventions?
Are there patterns in types of HIV prevention structural interventions? (Do certain types go together?)
What are the study designs of HIV prevention structural interventions?
Has the mix of HIV prevention structural interventions changed across time in terms of location, SI type, research design, and population groups?
Methods
Search Strategy
To identify structural interventions in HIV prevention, we used CDC’s Prevention Research Synthesis (PRS) Project’s cumulative database (PRS database) of citations relating to HIV, AIDS and STI prevention literature from 1988 to 2013. Citations in this database are coded for a variety of variables related to populations, settings, interventions and outcomes. At the time of this project in 2013, the database contained more a total of 62,000 unique citations that were coded according to topics, target populations and types of interventions. This database is updated annually with automated searches [14] designed and tailored to four research areas: (1) HIV, AIDS, or STI behavioral prevention; (2) linkage to, retention in, and re-engagement in HIV care; (3) HIV, AIDS, antiretroviral therapy (ART) treatment and adherence; and (4) systematic reviews on HIV and AIDS. The automated searches use six electronic bibliographic databases to retrieve relevant published literature: CAB Global Health (OVID), CINAHL (EBSCOhost), EMBASE (OVID), PsycINFO (OVID), MEDLINE (OVID), Sociological Abstracts (ProQuest) [15–18]. In addition, there is a supplemental manual search, which includes a quarterly hand search of 52 journals, requesting publications from experts in the field and reviewing other sources, such as electronic mail lists, clinical trial databases (e.g., Cochrane Library, CRISP database), conference proceedings, and references harvested from relevant HIV behavioral prevention research literature [14]. Full search strategy details of databases searched, MEDLINE search strategy, and a list of hand-searched journals are provided in the online Supplementary Materials A, B, and C, respectively (insert a link to online materials). Citations identified through automated and manual searches were downloaded and deduplicated in the PRS database before conducting title/abstract screening and full report coding.
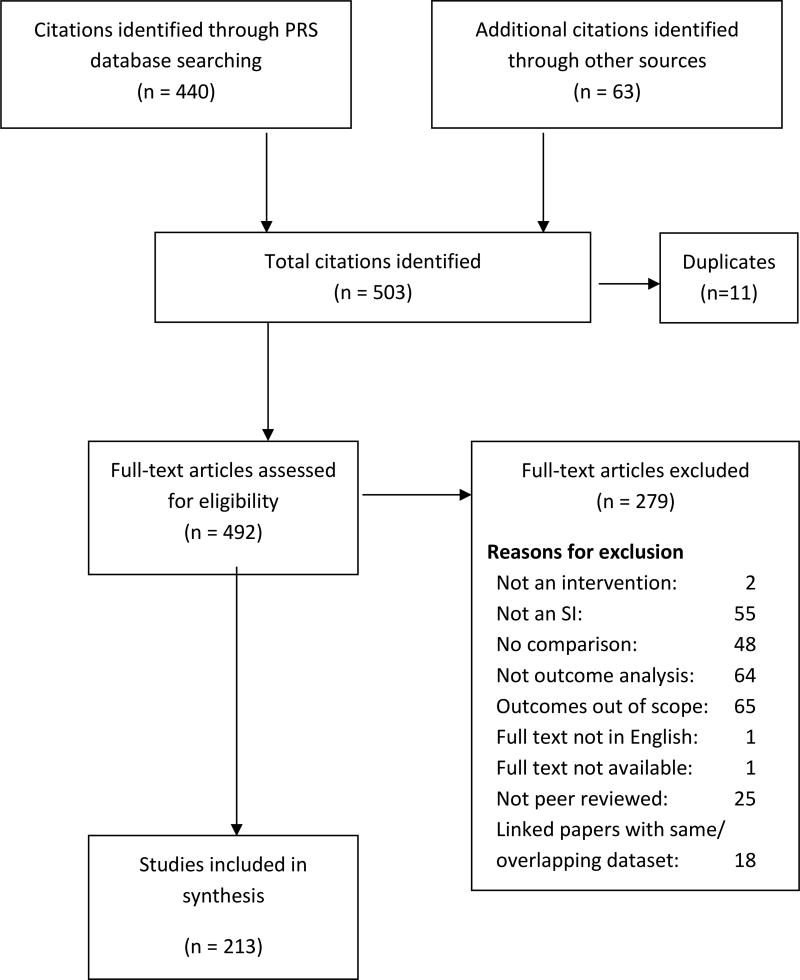
To obtain citations for this project specific to structural interventions, the PRS database was searched for citations published between 1988 and March 2013 that were coded as (1) “structural intervention,” yield = 135 citations; or (2) “policy intervention,” yield = 38 citations; or (3) “structural change mechanism,” yield = 100 citations. A second search was conducted after the taxonomy was developed and included terms that were not in the original search. These coded terms included (1) “capacity building,” yield = 33 citations, (2) “community mobilization,” yield = 37 citations, and (3) “social marketing/mass media,” yield = 97 citations. The total citation yield from the PRS database was 440 citations, last searched on May 3, 2017. In addition, authors hand-searched reference lists of related reports and systematic reviews and identified 63 more citations. Thus, 503 potential papers were identified (see Figure 1).
Fig. 1.
Flow chart showing number of papers identified, duplicates, reasons for exclusion, and total number of included studies.
Inclusion Criteria
To be included in this review, studies were required to meet the following criteria:
Evaluation of an intervention that included at least one structural component not controlled by the individual, affecting recipients’ behavior or other aspects of HIV risk
Reported data on at least one of the specified outcomes (see list below in Outcome Measures)
Published in English in a peer-reviewed journal
- Research design including a comparison condition, specifically:
-
◦RCTs, cluster RCTs
-
◦quasi-experimental, cluster quasi-experimental (defined here as comparison trials where treatment assignment is not random but also not self-selected)
-
◦time series (requiring two or more observations before and after the intervention)
-
◦prospective cohort studies
-
◦retrospective cohort studies
-
◦case-control studies
-
◦before/after comparisons (including comparisons against a baseline of zero)
-
◦
Exclusion Criteria
Interventions delivered at the community level unless there was an explicit structural component. Interventions were considered community level and not structural if the activity focused on individual participation or transactions, such as small group empowerment meetings or one-to-one conversations.
Exposure analysis (i.e., only comparing people reporting exposure versus no exposure to an intervention)
Variables Abstracted
The following variables were abstracted: first author name, year of publication, years and location of implementation, target population, type of structural intervention, study design, outcomes measured, and description of intervention.
Outcome Measures
Studies were eligible for this review if they reported results on at least one of the following outcome measures:
Sexual risk behaviors associated with HIV or STI infection (e.g., condomless sex, number of sex partners)
Injection drug use behaviors (e.g., uptake of sterile syringes, frequency of injection drug use)
HIV testing (e.g., number of people tested for HIV)
HIV infection
STI when used as a proxy for behavior change (i.e., excluding improved surveillance)
HIV stigma
ART prescriptions when an outcome of provider interventions
Adherence to HIV medication
Engagement in HIV primary medical care (including health care utilization, linkage to and retention in care)
We excluded certain outcomes that we considered more distal to HIV infection. The outcomes excluded, or that did not qualify a citation for the review, were:
Number of condoms distributed/taken
Attitudes other than stigma
Cognition including knowledge
Communication
Procedure
We developed a definition for structural interventions through an iterative procedure of literature review and workgroup discussion. In 2010–2011, a team of experts reviewed the first 87 citations and developed an initial definition and taxonomy. In 2012, two coders were added to the project and independently coded the 87 citations by using the categories developed in the first step. The categories and corresponding definitions were further refined. All citations were coded by pairs of independent coders. Discrepancies were resolved through discussion by all team members.
Statistical methods
Taxonomy categories and subcategories were analyzed using descriptive statistics and cross-tabulations. We used logistic regression to examine changes across time in the proportion of studies that featured various characteristics, specifically type of SI, location (high versus middle/low income economies), type of study population, and study design quality (stronger versus weaker designs). In each model the dependent variable was presence or absence of the characteristic of interest. The independent variable was year, so that the odds ratio (OR) represents the annual increase in odds that a study includes the characteristic of interest. For graphic presentation we grouped the 26-year review period into one group of 6 years followed by four groups of 5 years. SAS version 9.3 was used for the analyses.
Results
Structural Intervention Definition and Taxonomy Development
We defined structural interventions as:
An intervention that affects risk and/or behavioral choices by changing something that is external to the individual and not under his/her control.
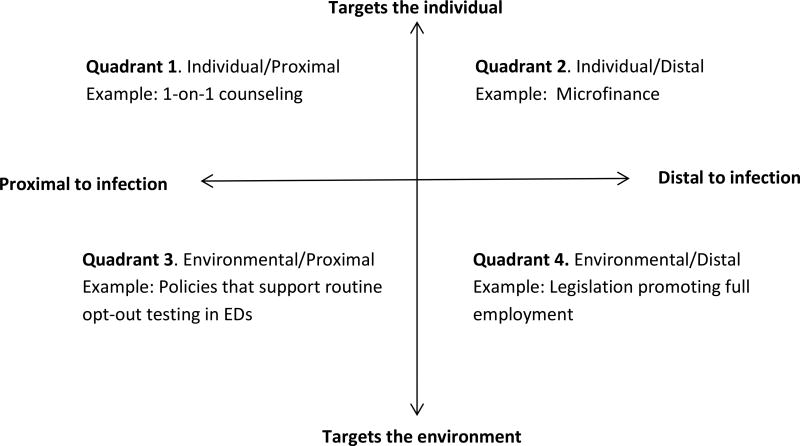
The definition is broad enough to include interventions that operate in two distinct ways along separate continua to reduce risk: intervention target and proximity to HIV infection. The first dimension refers to whether an intervention targets changes in individuals vs. environment. When the intervention alters the environment (e.g., storefront HIV testing centers) or uses strategies to alter the choice structure (e.g., routine opt-out HIV testing in clinical settings), these are outside the individual’s control. The second dimension refers to whether an intervention alters social determinants of the epidemic (e.g., microfinance interventions or reducing societal homophobia). We categorized all interventions along these two dimensions as illustrated in Figure 2. Interventions are considered structural if they meet one or both criteria of being distal to the infection (social determinants of health) or targeting the environment. Thus, structural interventions fall into three of the four quadrants.
Fig. 2.
Two dimensions and four quadrants useful in distinguishing structural interventions from other types of interventions. Interventions are considered structural if they are either target the environment and/or address determinants of health that are distal to HIV infection. Quadrant 1 is not considered to be structural.
Interventions in Quadrant 1 are typically focused on changing individual behavior, knowledge, and awareness and focused on proximal causes; these meet neither criterion, thus are considered not structural. Interventions in Quadrant 4 are considered structural as they meet both criteria (i.e., they target the environment rather than the individual and are focused on distal causes). Those in Quadrants 2 and 3 meet only one of the two criteria to affect change; however, these types of interventions were considered to be structural as well.
We next developed a taxonomy of structural interventions and refined definitions for each category in the taxonomy (Access, Policy/Procedure, Physical Structure, Capacity Building, Mass Media, Community Mobilization, and Social Determinants). Most of the categories had subcategories; all are defined below.
Taxonomy Definitions
Access
Provision of a health product or service or actions that make such products or services more readily available to the intended users. Access can be modified in ways that include, but are not limited to, physical changes. Examples include locating a storefront HIV testing site in a neighborhood or expanding its hours of operation. Condom distribution counts as access only if condoms are available widely and do not require enrollment into a program to procure. Subcategories of Access include HIV testing, Condoms, STI testing, Sterile injection equipment, HIV Health Care, and Drug treatment.
Policy/Procedure
Policy is formal guidance, principal, or rule adopted to bring about change. Procedure is the implementation of a policy and typically specifies a process. It is important to note that virtually all interventions require some policy or procedural change in order to be instantiated. Both are decided at an organizational or higher level that do require input at the individual level. Often, policy/procedure interventions are ones in which the change is the intervention itself.
Institutional policy/procedure: Policies enacted by a nonjudicial entity such as a clinic, school, or workplace that affect risk and/or behavioral choices (e.g., opt-out testing in an ER).
Governmental policy: For interventions in this category, there may not be legal consequences for infractions and they may be issued from a municipal, state, or national body (e.g., CDC guidelines on preexposure prophylaxis).
Legislation: Involves change in law that affect risk and/or behavioral choices (e.g., syringe access laws). Such changes have the authority of the polity behind them.
Mass Media
Widely disseminated interventions via a large-scale communication medium other than person-to-person.
Social marketing: The promotion of some positive social objective by employing marketing techniques used commercially; often disseminated via mass media (e.g., radio or TV spots delivering a crafted message). A requirement is that the information channel can be said to saturate the environment, so that exposure is largely outside the control of the individual (e.g., video shown to large waiting room; large posters displayed in multiple locations in a neighborhood). Small communication channels, such as letters, brochures, newsletters, and videos delivered to individuals or small groups, do not qualify as mass media.
Narrative interventions: Interventions focused on a storyline included in the media (e.g., soap operas, podcast serial dramas)
Physical structure
Any physical form that affects risk directly or the ease with which healthy behaviors can be performed (e.g., creating new clinics, integrating services in one location, building a road, using a mobile van to deliver services).
Integration of services: Services or products are brought together (i.e., co-located) for the sake of the convenience of the intended user and the efficiency of service provision. This is an important subset of physical structure interventions.
New physical structures: Development of structures that did not exist previously, at least in the present location (e.g. clinics, vans, doors on bathhouse rooms).
Service provided in nontraditional setting: Health services made available to people in a particular setting (e.g., homes, workplaces, prisons, schools) and the original service provided in the setting is not related to health or located in a health setting.
Capacity-building
Change that improves an agency’s ability to provide services or programs.
Provider/supervisor training: Training of health care or other staff to help them use more effective procedures with patients/clients.
Technology: Using tools to increase productivity.
Hiring staff/funding: Adding personnel to start interventions or increase productivity or securing monies to implement or enhance interventions.
Staff incentives: Providing inducements, either monetary or nonmonetary, to increase productivity.
Community Mobilization
A process of change involving multiple stakeholders within a community, including people who live in the community. A key criterion is that the community becomes involved through interaction with each other and the resulting change includes emergent properties, such as collective efficacy (e.g., sex workers who unite together to demand condom use from clients). A substantial amount of the change is generated by community members who play a role in developing and implementing the intervention.
Social Determinants of Health Interventions
Interventions addressing survival or acceptance and respect.
Survival: Interventions that address factors having to do with basic necessities, such as money, food, and shelter, rather than, or in addition to, addressing HIV-related risk behavior directly.
Acceptance and Respect: Interventions that address prejudice, discrimination, HIV stigma, or homophobia in the social environment of those whose health and/or health behaviors are affected by them. Interventions aimed at reducing internalized prejudice do not necessarily count as structural interventions because they may directly influence only the affected individuals.
The categories are mutually exclusive with the exception of the Access category. Often, interventions in other categories provided access to things by their very nature, such as condoms, HIV testing, or sterile syringes, and thus meet the definition of the Access category. On the other hand, interventions can also be classified in more than one category when they have multiple components, such as an intervention that includes community mobilization of sex workers in addition to a policy of 100% condom use. Most of the interventions in these categories fit into quadrants 3 or 4 in Figure 2. Only intervention in the social determinants of health category may fit into quadrant 2 or 4.
Characteristics of Structural Interventions and Categorization using the New Taxonomy
Sample of studies
From the 503 citations identified by the search, 213 intervention studies published between 1988 and 2013 met criteria and are therefore included in this review (Figure 1, Appendix Table I). The interventions were conducted between 1984 and 2010; more than half began in 2001 or later.
Type of Structural Intervention
The majority of interventions were categorized as Access (65%, n = 139) (Table I); the most common Access types were HIV testing (n = 52), condoms (n = 48), and STI testing and treatment (n = 34). The next largest category was Policy/Procedure (32%, n = 68) with 51 studies employing institutional policies/procedures and 18 employing governmental. Twenty-nine percent of the interventions were developed as Mass Media interventions (n = 62), most of which included social marketing campaigns (n = 56). Five of the social marketing studies also included narrative interventions while six were narrative interventions only.
Table I.
Type of Structural Intervention in HIV Prevention (k = 213)
| Type of Structural Intervention | Frequency | % |
|---|---|---|
| Access | 139 | 65% |
| HIV testing | 52 | |
| Condoms | 48 | |
| STI testing and treatment | 34 | |
| Sterile injection equipment | 21 | |
| HIV health care | 17 | |
| Drug treatment | 2 | |
| Policy/Procedure | 68 | 32% |
| Institutional | 51 | |
| Governmental | 18 | |
| Legislation | 0 | |
| Mass Media | 62 | 29% |
| Social marketing | 56 | |
| Narrative | 11 | |
| Physical Structure | 58 | 27% |
| Services provided in nontraditional setting | 23 | |
| Integration of services | 22 | |
| New physical structures | 20 | |
| Capacity Building | 51 | 24% |
| Provider/supervisor training | 42 | |
| Technology | 12 | |
| Hiring staff/funding | 1 | |
| Staff incentives | 0 | |
| Community Mobilization | 20 | 9% |
| Social Determinants of Health | 16 | 8% |
| Survival | 9 | |
| Acceptance and respect | 8 |
Note. Totals exceed 100% because of multiple response
HIV: Human Immunodeficiency virus; STI: Sexually transmitted infections
Twenty-seven percent of studies were categorized as a Physical Structure (n = 58), either by providing services in a nontraditional setting (n=23), integrating services (n = 22), or developing a new physical structure (n = 20). Twenty-four percent of the studies featured Capacity Building (n = 51), most frequently through provider or supervisor training (n = 42) or new technology (n = 12). Nine percent of studies were categorized as Community Mobilization (n = 20) and eight percent of studies were considered to be Social Determinants of Health (n = 16).
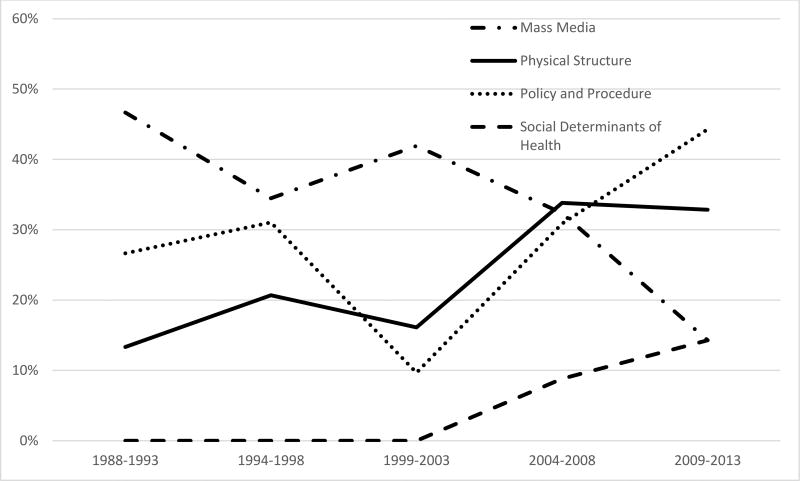
There was a significant increase across time in the proportion of studies that included three SI types (Figure 3). The proportion including Physical Structure increased from 13% in 1988–1993 to 33% in 2009–2013 (OR per year = 1.08, 95% CI 1.02, 1.14). The proportion including Policy and Procedure increased from 27% to 44% (OR = 1.06, 95% CI 1.01, 1.11). The proportion including Social Determinants of Health increased from 0% to 14% (OR = 1.24, 95% CI 1.06, 1.46). There was a significant decrease across time in the proportion of studies that included Mass Media from 47% to 14% (OR = 0.91, 95% CI 0.88, 0.97). There was no significant change across time in the proportion of studies that included Access, Capacity Building, or Community Mobilization.
Fig. 3.
Changes over time in proportion of studies by type of structural intervention 1998 – 2013.
Intervention location
The interventions were located in countries around the world (Table II). The largest proportion (49%, n = 104) of studies were conducted in the Americas, most of them in the United States (n = 84); within the United States, the largest numbers were from the West (n = 30), Southeast (n = 16) and Northeast (n = 15). Twenty-four percent of studies were conducted in Africa (n = 52), including nine from Tanzania, eight from South Africa, and six from Uganda. Seventeen percent of the studies were conducted in Asia (n = 36) including nine each from China, India, and Thailand. Eight percent were conducted in Europe (n = 18), including nine studies from the United Kingdom and two each from France, Italy, and the Netherlands. Three studies were from Australia. In analyses examining change over time, there was no significant change in the proportion of interventions conducted in high income economies versus middle/low economies (OR = 0.99, 95% CI 0.95, 1.04).
Table II.
Location of Intervention by Type of Structural Interventions in HIV Prevention (k = 213)
| Type of Structural Intervention | ||||||||
|---|---|---|---|---|---|---|---|---|
| Continent/Region | PP | MM | PS | CB | CM | SDH | A | TOTALa |
| Americas | 38 (37%) | 22 (21%) | 28 (27%) | 23 (22%) | 6 (6%) | 5 (5%) | 72 (69%) | 104 (49%) |
| United States | 32 | 18 | 22 | 21 | 4 | 3 | 56 | 84 |
| Latin America & Caribbean | 3 | 2 | 3 | 1 | 2 | 2 | 9 | 13 |
| Canada | 3 | 2 | 3 | 1 | 0 | 0 | 7 | 7 |
| Africab | 12 (23%) | 16 (31%) | 17 (33%) | 18 (35%) | 4 (8%) | 8 (15%) | 30(58%) | 52(24%) |
| East Africa | 4 | 5 | 7 | 8 | 1 | 1 | 12 | 20 |
| Southern Africa | 4 | 3 | 6 | 6 | 2 | 6 | 10 | 17 |
| Central Africa | 4 | 4 | 3 | 3 | 1 | 0 | 6 | 9 |
| West Africa | 0 | 4 | 1 | 1 | 0 | 1 | 2 | 6 |
| Asiab | 8 (22%) | 16 (44%) | 7 (19%) | 7 (19%) | 10 (28%) | 3 (8%) | 24 (67%) | 36 (17%) |
| Southeast Asia | 6 | 8 | 2 | 2 | 4 | 0 | 10 | 15 |
| East Asia | 2 | 4 | 2 | 3 | 1 | 1 | 7 | 11 |
| South Asia | 0 | 4 | 3 | 2 | 5 | 2 | 7 | 10 |
| Europec | 10 (56%) | 6 (33%) | 5 (28%) | 3 (17%) | 0 (0%) | 0 (0%) | 12 (67%) | 18 (8%) |
| Australia | 0 (0%) | 2 (67%) | 1 (33%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (33%) | 3 (1%) |
A: Access; CB: Capacity Building; CM: Community Mobilization; MM: Mass Media; PP: Policy/Procedure; PS: Physical structure; SDH: Social Determinants of Health
Percentages in far right column indicatethe proportion of 213 studies from each continent / region; all other percentages represent the proportion of interventions within each continent or region that include each structural type
5 multi-regional studies are included in the region with the most countries represented, e.g., a study in 4 countries in Southern Africa and 1 country in East Africa is included in the row for Southern Africa; if thelargest number of countries is a tie then the study is included with the country that has the largest population, e.g., a study in Zambia and Rwanda is included in the row for Central Africa
Includes Western and Eastern Europe
Target population
Table III summarizes the target populations across the interventions. Forty percent of the structural interventions focused on high-risk populations, including 32 studies targeting commercial sex workers, 26 studies targeting individuals who inject drugs (PWID), and 17 studies targeting men who have sex with men (MSM). Several studies focused on females (n = 47), persons living with HIV (n = 32), youth (n = 30), people residing in urban/inner city areas (n = 26), young adults (n = 20), HIV clinic patients (n = 16), blacks or African Americans (n = 12), and Hispanics/Latinos (n = 8).
Table III.
Target Population of Structural Interventions in HIV Prevention (k = 213)
| Population Type | Frequency | % |
|---|---|---|
| Sex | 64 | 30% |
| Female | 47 | |
| Male | 24 | |
| Age | 38 | 11% |
| Young adult (18–25 years) | 20 | |
| Youth (<18 years) | 30 | |
| Race/Ethnicity | 21 | 10% |
| Black or African American | 12 | |
| Hispanic/Latino | 8 | |
| People of color | 5 | |
| High-Risk Populations | 86 | 40% |
| Sex worker | 32 | |
| PWID | 26 | |
| MSM | 17 | |
| Sex partner, high riska | 10 | |
| Noninjection drug users | 4 | |
| Sexually active youth | 3 | |
| Unspecifiedb | 8 | |
| Populations | 69 | 32% |
| Low income | 11 | |
| Health service providers | 13 | |
| General population | 10 | |
| Hospital in-patients | 5 | |
| On ART/Treatment experienced | 4 | |
| Homeless | 4 | |
| Pregnantfemales | 4 | |
| Incarcerated | 4 | |
| Otherc | 20 | |
| Clinic Patients | 44 | 21% |
| HIV clinic | 16 | |
| Emergency department | 10 | |
| Primary care | 3 | |
| STI/genitourinary clinic | 6 | |
| Other clinicd | 12 | |
| Residence | 56 | 26% |
| Urban/inner city | 26 | |
| Rural | 19 | |
| High-risk area | 14 | |
| HIV Status | 39 | 18% |
| HIV positive | 32 | |
| HIV negative | 7 | |
| Not specified | 1 | 0.5% |
Note. Totals exceed 100% because of multiple response.
ART: Antiretroviral therapy; HIV: Human Immunodeficiency virus; STI: Sexually transmitted infections;
Includes sex partner of PWID, new or multiple sex partners, and high risk sex partner
Reported by author as people at high risk for HIV and/or STI but not specified
Includes heterosexuals, employees, mentally ill, transgender persons, parents, teachers, community leaders, and tuberculosis infected patients
Includes tuberculosis clinics, Veterans Affairs health clinics, antenatal clinics, traveler clinics, and health departments
Fewer studies targeted homeless persons (n = 4), non-injection drug users (n = 4), pregnant females (n = 4), incarcerated persons (n = 4), or sexually active youth (n = 3). Only one study focused on transgender persons. There was a significant increase over time in the proportion of interventions focusing on persons living with HIV, from 7% in 1988–1993 to 30% in 2009–2013 (OR = 1.17, 95% CI 1.06, 1.28), and a significant decrease in the proportion of interventions targeting PWID, from 53% to 7% (OR = 0.89, 95% CI 0.84, 0.95). There was no significant change across time in the proportion of studies focusing on commercial sex workers (OR = 0.97, 95% CI 0.91, 1.03) or MSM (OR = 1.00, 95% CI 0.92, 1.08).
Outcome
Sex behavior outcomes constituted the largest category of outcomes (50%, n = 106); condom use was the most frequent outcome in this category (n = 81) (Table IV). Testing or treatment outcomes were the next largest category (40%, n = 86); HIV testing (n = 60) was the most frequent type of testing/treatment, followed by retention in care (n = 13) and antiretroviral adherence (n = 11). Twenty-five percent of the interventions reported biologic outcomes (n = 53), which consisted predominantly of STI (n = 31) and HIV infection (n = 26). Other biologic outcomes included viral load/suppression, CD4 counts and AIDS mortality. There was a smaller proportion of drug injection behavior outcomes (13%, n = 28); among these, sharing of equipment or injection drug use were reported most frequently. There were only 5 studies with stigma outcomes (2%).
Table IV.
Type of Outcomes Reported in Structural Interventions in HIV Prevention (k = 213)
| Type of Outcomea | Frequency | % |
|---|---|---|
| Sex Behaviors | 106 | 50% |
| Condom use | 81 | |
| Multiple partners | 22 | |
| Unprotected sex | 19 | |
| Sex risk behaviors | 17 | |
| Abstinence/sex initiation | 8 | |
| Testing/Treatment | 86 | 40% |
| HIV testing | 60 | |
| Retention in care | 13 | |
| Antiretroviraladherence | 11 | |
| Engaged in care | 10 | |
| Linked to care | 9 | |
| Antiretroviral uptake | 8 | |
| HIV Diagnosis or serostatus awareness | 4 | |
| STI testingb | 3 | |
| Biologic | 53 | 25% |
| STI | 31 | |
| HIV infection | 26 | |
| Viral load/suppression | 9 | |
| CD4 counts | 9 | |
| AIDS mortality | 3 | |
| Injection DrugBehaviors | 28 | 13% |
| Sterile injection equipment | 28 | |
| Injection drug use | 12 | |
| Stigma | 5 | 2% |
Note. AIDS: Acquired immune deficiency syndrome; HIV: Human Immunodeficiency virus; PWID: People who inject drugs; STI: Sexually transmitted infections
Categorized for uniformity
Used when interpretable as a proxy for behavior
Type of Research Design
The majority of interventions was evaluated using before/after research design, either one group or cross-sectional (57%, n = 121), but other research designs of randomized controlled trials, quasi-experimental, and serial cross-sectional designs were also employed (Table V). There was no significant change over time in proportion of high-quality study designs (i.e., RCT, cluster RCT, quasi-experimental and cluster quasi-experimental) vs. low-quality study design (e.g., before/after designs or after-only designs) (OR = 1.01, 95% CI 0.96, 1.06).
Table V.
Type of Study Design Employed in Structural Interventions in HIV Prevention (k = 213)
| Type of Study Design | Frequency | % |
|---|---|---|
| Before/After, one group | 61 | 29% |
| Before/After, cross-sectional | 60 | 28% |
| Cluster RCT | 20 | 9% |
| Quasi-Experimental | 19 | 9% |
| Cluster Quasi-Experimental | 14 | 7% |
| Serial Cross-Sectional | 14 | 7% |
| RCT | 12 | 6% |
| Retrospective Cohort | 10 | 5% |
| Prospective Cohort | 8 | 4% |
| After Only, two groups | 7 | 3% |
| Time Series | 6 | 3% |
| Othera | 2 | 0.9% |
Note. Totals exceed 100 because of multiple response.
RCT: Randomized control trial
Other includes alternating comparison trial, after-only four group comparison
Discussion
Overall HIV incidence in the United States has remained stable despite increasing prevalence [19]. Several federal initiatives have been used to maintain or reduce new HIV diagnoses, the most recent of which is High Impact Prevention [20], a strategy to allocate resources on activities found to have a greater impact in HIV prevention. Moving forward, the national HIV prevention goals [1] emphasize structural interventions as a way to reduce new HIV infections, thus it is timely to have a comprehensive framework for structural interventions. In this study, we developed a taxonomy of structural interventions comprising 7 categories and 20 subcategories, and classified 213 structural interventions into the new taxonomy. The new taxonomy is parsed similarly to Cohen et al. [5] and Blankenship et al. [6], but is more comprehensive than either taken singly and also includes social determinants of health (survival and acceptance). Blankenship et al. [6] included “community mobilization” and “integration of services,” which are also part of our own taxonomy. “Contingent funding,” while being sparse in the literature at the time we conducted our review, would be an example of using Social Determinants of Health-Survival, as would “economic development programs.” The category of “educational interventions” has more to do with site of delivery than type of intervention per se, and therefore does not appear in our taxonomy.
In earlier work, Blankenship and colleagues [3] proposed “availability” and “accessibility” categories, which are similar to our access category. Sumartojo and colleagues [4] included “economic resources,” which is similar to our category of social determinants of health-survival; “policy supports” is similar to our policy/process; and both “societal conditions” and “organizational structures and functions” encompass more than a single category in our taxonomy. Tsai [7], on the other hand, gave a few examples but none of them overlap with our categories. In summary, our taxonomy encompassed every structural intervention identified from the systematic review in HIV prevention and was built to be inclusive and comprehensive of interventions beyond the systematic review. Each category and subcategory has detailed definitions that were tested and refined during an iterative process. Moreover, since this taxonomy is broad, it is useful in presenting a wide variety of options to consider when choosing strategies that will best address the specific needs of a community.
Access, Policy/Procedures, Mass Media, and Physical Structure were the most common structural interventions identified in the literature. By contrast, interventions addressing social determinants of health were rarely found in the HIV prevention and treatment literature. The largest proportion of the interventions were conducted in the United States but it is important to note that many of the interventions in low-middle–income countries were conducted by researchers from high-income countries. In general, the evaluation of the interventions consisted of before/after research designs and the rigor did not increase over time, possibly because it is often not feasible to randomly allocate structural interventions or study them in controlled situations.
While nearly 40% of the structural interventions focused on high-risk populations, interventions targeting MSM were relatively few compared to PWID and commercial sex workers.
Some structural interventions—namely, those addressing social determinants of health (both survival-related and tolerance/acceptance–related)—have the potential to influence multiple health conditions. Poverty, for example, is related to many health outcomes [21]. While conducting a microfinance intervention to address HIV risk alone may appear to be prohibitively expensive, a study assessing its effects on multiple health outcomes may demonstrate cost-effectiveness. Unfortunately, the disease-specific silos around which health promotion and illness prevention funding are organized make it difficult to conduct such studies. Thus, most interventions target intermediate structural factors associated with HIV and do not address fundamental contributors to health disparities, such as poverty, housing, and education. These contributors are termed frequently as “social determinants of health” and, for many health conditions, generally account for more variance in health than most factors and arguably more than individual behaviors [21]. Agencies that are capable of addressing these major structural determinants, such as US Departments of Housing and Urban Development (HUD), Labor (DOL) or Education (ED), do not necessarily focus on public health, but their programs are likely to have great impact on health outcomes. Evaluation of programmatic or policy interventions directed towards employment generation, school retention, or housing stability can be designed to examine effects on HIV and other health outcomes. It is often considered outside the reach of public health to intervene on these domains due to narrow organizational missions and vertical funding streams. However, with shrinking public health dollars, an HIV epidemic characterized by extreme disparities driven by social conditions, and the syndemic nature of infectious disease, chronic illness, substance abuse, and mental health, meaningful action-oriented collaborations that alter the fundamental causes of HIV and other health outcomes are needed urgently. Given the lack of integration between the health care system and other key non-health care systems, more of these collaborations from different arenas will be necessary.
It was a challenge to develop a definition for identifying that an intervention was truly structural and then create a taxonomy that was able to encompass all structural interventions identified in our review. Our definition of structural interventions necessitates that exposure to the intervention is outside of the control of the person affected. For example, small-group interventions are not considered structural, as people self-select into group interventions and are thus in control of the receipt of the intervention. The distinction is that of personal agency (i.e., individuals controlling their own actions). We did include interventions that required some personal agency, as in the case of individuals using syringe exchange programs, because the environment is changed in a way that is not under the control of the involved person. By contrast, an example that would be excluded is a community-level intervention with no structural components. Even though these interventions are delivered in community settings, most also feature significant one-on-one transactions (e.g., Popular Opinion Leader and Community PROMISE) or small group risk-reduction meetings (e.g., Voices/Voces) [22–24]. Thus, interventions with a large reach do not necessarily meet the criteria as structural interventions unless the intervention entails an environmental change. Lastly, small communication media, such as brochures or pamphlets, even if they have a large reach, do not translate to structural change unless they change the environment.
Limitations
Our taxonomy may not be broad enough to apply to structural interventions reported for other health conditions, such as poverty alleviation interventions that affect many outcomes, including outcomes associated with HIV risk. While we were highly inclusive in allowing less rigorously evaluated studies to be included, there are many interventions that are structural in nature that have not been evaluated. On the other hand, there may be some structural intervention evaluations not included in this study that report outcomes not directly related to HIV, but in theory could impact HIV risk. Lastly, we did not quantify the effectiveness of these interventions, nor did we assess in detail the quality of studies. Examining these dimensions in future studies will enhance the usefulness of the findings reported here.
Conclusions
To our knowledge, this is the first time a framework for structural interventions in HIV prevention has yielded a comprehensive, well-defined taxonomy of structural interventions. The taxonomy may move the field toward a more precise and shared language for discussing these types of interventions. It can be used to develop further generalizations about different types of interventions, as well as providing insight into the gaps in research in various categories within the taxonomy.
Supplementary Material
References
- 1.Office of National AIDS Policy. [cited November 9, 2015];National HIV/AIDS Strategy for the United States: Updated to 2020. 2015 Available from: https://www.aids.gov/federal-resources/national-hiv-aids-strategy/nhas-update.pdf.
- 2.Sweat MD, Denison JA. Reducing HIV incidence in developing countries with structural and environmental interventions. AIDS. 1995;9(Suppl A):S251–7. [PubMed] [Google Scholar]
- 3.Blankenship KM, Bray SJ, Merson MH. Structural interventions in public health. AIDS. 2000;14(Suppl 1):S11–21. doi: 10.1097/00002030-200006001-00003. [DOI] [PubMed] [Google Scholar]
- 4.Sumartojo E. Structural factors in HIV prevention: concepts, examples, and implications for research. AIDS. 2000;14(Suppl 1):S3–10. doi: 10.1097/00002030-200006001-00002. [DOI] [PubMed] [Google Scholar]
- 5.Cohen DA, Scribner R. An STD/HIV prevention intervention framework. AIDS Patient Care STDS. 2000;14(1):37–45. doi: 10.1089/108729100318118. [DOI] [PubMed] [Google Scholar]
- 6.Blankenship KM, Friedman SR, Dworkin S, Mantell JE. Structural interventions: concepts, challenges and opportunities for research. J Urban Health. 2006;83(1):59–72. doi: 10.1007/s11524-005-9007-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsai AC. A typology of structural approaches to HIV prevention: a commentary on Roberts and Matthews. Soc Sci Med. 2012;75(9):1562–7. doi: 10.1016/j.socscimed.2012.06.033. discussion 8–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaufman MR, Cornish F, Zimmerman RS, Johnson BT. Health behavior change models for HIV prevention and AIDS care: practical recommendations for a multi-level approach. J Acquir Immune Defic Syndr. 2014;66(Suppl 3):S250–8. doi: 10.1097/QAI.0000000000000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adimora AA, Auerbach JD. Structural interventions for HIV prevention in the United States. J Acquir Immune Defic Syndr. 2010;55(Suppl 2):S132–5. doi: 10.1097/QAI.0b013e3181fbcb38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Des Jarlais DC. Structural interventions to reduce HIV transmission among injecting drug users. AIDS. 2000;14(Suppl 1):S41–6. doi: 10.1097/00002030-200006001-00006. [DOI] [PubMed] [Google Scholar]
- 11.Gupta GR, Parkhurst JO, Ogden JA, Aggleton P, Mahal A. Structural approaches to HIV prevention. Lancet. 2008;372(9640):764–75. doi: 10.1016/S0140-6736(08)60887-9. [DOI] [PubMed] [Google Scholar]
- 12.Parker RG, Easton D, Klein CH. Structural barriers and facilitators in HIV prevention: a review of international research. AIDS. 2000;14(Suppl 1):S22–32. doi: 10.1097/00002030-200006001-00004. [DOI] [PubMed] [Google Scholar]
- 13.Parkhurst JO. HIV prevention, structural change and social values: the need for an explicit normative approach. J Int AIDS Soc. 2012;15(Suppl 1):1–10. doi: 10.7448/IAS.15.3.17367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DeLuca JB, Mullins MM, Lyles CM, Crepaz N, Kay K, Thadiparthi S. Developing a comprehensive search strategy for evidence based systematic reviews. Evid Based Libr Inf Pract. 2008;3(1):3–32. [Google Scholar]
- 15.PsycINFO [Internet] [cited November 9, 2015];Wolters Kluwer. 1988 Available from: http://www.ovid.com/site/
- 16.EMBASE [Internet] [cited November 9, 2015];Wolters Kluwer. 1988 Available from: http://www.ovid.com/site/?cmpid=Database%2520Landing:%2520RecomendMedicine%2520-%2520Embase.
- 17.MEDLINE [Internet] [cited November 9, 2015];Wolters Kluwer. 1988 Available from: http://gateway.ovid.com/autologin.html.
- 18.Sociological Abstracts [Internet] [cited November 9, 2015];ProQuest. 2012 Available from: http://www.proquest.com/products-services/socioabs-set-c.html.
- 19.Centers for Disease Control and Prevention. Diagnoses of HIV infection in the United States and dependent areas, 2013. HIV Surveillance Report. 2013;25:1–82. [Google Scholar]
- 20.Purcell DW, McCray E, Mermin J. The shift to high-impact HIV prevention by health departments in the United States. Public Health Rep. 2016;131(1):7–10. doi: 10.1177/003335491613100104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Frieden TR. A framework for public health action: the health impact pyramid. Am J Public Health. 2010;100(4):590–5. doi: 10.2105/AJPH.2009.185652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention (CDC) AIDS Community Demonstration Projects Research Group. Community-level HIV intervention in 5 cities: final outcome data from the CDC AIDS Community Demonstration Projects. Am J Public Health. 1999;89(3):336–45. doi: 10.2105/ajph.89.3.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kelly JA, Murphy DA, Sikkema KJ, McAuliffe TL, Roffman RA, Solomon LJ, et al. Randomised, controlled, community-level HIV-prevention intervention for sexual-risk behaviour among homosexual men in US cities. Community HIV Prevention Research Collaborative. Lancet. 1997;350(9090):1500–5. doi: 10.1016/s0140-6736(97)07439-4. [DOI] [PubMed] [Google Scholar]
- 24.Neumann MS, O'Donnell L, Doval AS, Schillinger J, Blank S, Ortiz-Rios E, et al. Effectiveness of the VOICES/VOCES sexually transmitted disease/human immunodeficiency virus prevention intervention when administered by health department staff: does it work in the "real world"? Sex Transm Dis. 2011;38(2):133–9. doi: 10.1097/OLQ.0b013e3181f0c051. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.