Abstract
Purpose: To examine the features and types of health information provided in Chinese diabetes mobile applications (apps) for patients' self-management. Materials and Methods: Through multiple rounds of screening, we identified a total of 95 relevant iOS (Apple, Cupertino, CA) and Android™ (Google, Mountain View, CA) apps and examined each app's features and health information types based on each app's description in the app stores. We used a 15-feature algorithm to evaluate the apps' abilities for supporting diabetic patients' self-management, based on U.S. national standards for diabetes self-management. We also adapted the health information wants framework to analyze the types of information that the apps provided for diabetic patients. Results: Diabetes education was the most common feature, provided by 75% of the apps. Blood glucose checking was enabled by 65% of the apps. Diet management, insulin checking, and physical activity monitoring were enabled by 53%, 49%, and 44% of the apps, respectively. Only a small percentage of the apps enabled psychosocial support (29%) or tracking of blood pressure (14%), cholesterol (14%), or body mass index (11%). None of the apps provided all seven types of information posited by the health information wants framework. Only a small percentage of the apps provided information about psychosocial support (29%), healthcare providers (24%), or healthcare facilities (24%). Information about complementary and alternative medicine was the least likely type of information provided in the apps, with only 7% of the apps providing this type of information. Conclusions: Our findings have important implications for improving the quality of Chinese diabetes mobile apps to facilitate patients' self-management.
Key words: : e-health, mobile health, telehealth, technology
Introduction
China has about one-third of the global incidence of diabetes,1 and its diabetes-related economic burden ($38 billion in 2013) is increasing.2,3 Yet Chinese patients and their families typically do not receive sufficient information about diabetes from healthcare providers,4–6 and so the majority of Chinese diabetic patients lack information necessary for self-care.7 This can lead to severe health consequences and a sense of powerlessness regarding treatment and self-management.8–11
Effective self-management of diabetes12,13 can be supported by mobile health (m-health) applications (apps), enabling patients to communicate with healthcare providers regarding glucose levels, weight, and diet control.14–17 The quality of m-health tools is problematic, however; few apps offer all of the features considered necessary for effective diabetes management,18 and despite the high prevalence of diabetes and adoption rate of mobile phones in China,19,20 knowledge about the quality of diabetes-related Chinese mobile apps is lacking. Here we explore the features and types of health information that Chinese diabetes mobile apps provide, and we suggest recommendations for their further development.
Materials and Methods
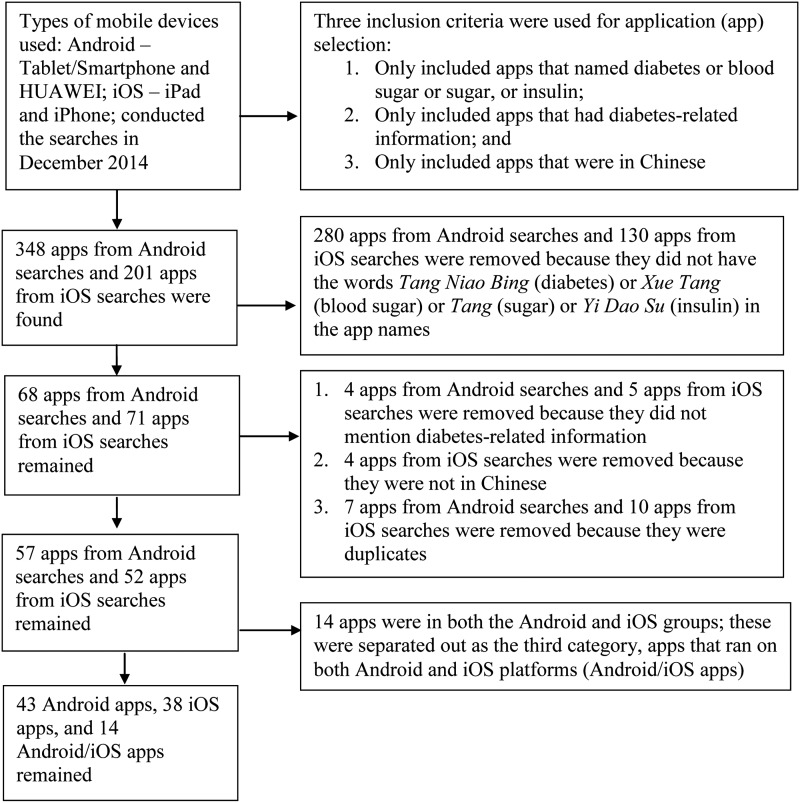
In December 2014, we selected Android™ (Google, Mountain View, CA) and iOS (Apple, Cupertino, CA) apps through multiple rounds of screening (Fig. 1). We then coded each app's features according to the app's description in the app stores. We defined “features” as functions that support diabetic patients' self-management. Five main features were adapted from a previous study21; additional features were based on the U.S. national standards for diabetes care.22 The final list of 15 features comprised general diabetes education, diet management, weight management, blood glucose monitoring, physical activity/exercise monitoring, communication with healthcare providers, insulin management (dosage calculation, self-injection), oral diabetes medication management, blood pressure (BP) monitoring, communication with family, communication with peer patients with similar conditions, disease-related alerts/reminders, calorie count, body mass index monitoring, and cholesterol monitoring.
Fig. 1.
Application (app) selection process.
To analyze the types of health information provided in the apps, we adapted the health information wants (HIW) framework,23–25 which defines seven types of health information that patients desire in medical encounters: information about diagnosis; treatment; laboratory tests; self-care; complementary and alternative medicine (CAM); psychosocial aspects; and healthcare providers (Table 1). Each app was independently coded by at least two authors. The authors' agreement rates for the iOS and the Android apps were 97% and 98%, respectively. Apps that ran on both Android and iOS platforms were coded by three authors, with an agreement rate of 0.942 (Krippendorff's alpha). Differences were resolved through all authors' discussion.
Table 1.
Seven Types of Health Information
| TYPE OF INFORMATION | DESCRIPTION | SUBGROUP EXPLANATION | EXAMPLE ITEM (USING DIABETES AS AN EXAMPLE) |
|---|---|---|---|
| Treatment | Information about the rationale, mechanism, and implications of a conventional method used to control a health condition | 1. Rationale: why treatment is needed; why a specific treatment is needed 2. Mechanism: how a treatment works 3. Implications of a conventional method: why a conventional method is needed to control diabetes |
1. Information explaining how a medication may help treat diabetes 2. Information about the specific drug(s) prescribed 3. Information about changing medications |
| Health condition specific | Information about the description, process and prognosis, and implications of a health condition | 1. Definition: what is a specific health condition (e.g., diabetes); what different types does this health condition include (e.g., types of diabetes; differences between type 1 and type 2 diabetes) 2. Process/prognosis/causes: how the health condition progresses and what the complications are; what are the causes for this health condition |
1. Information about the type of diabetes 2. Information about how severe my diabetes is 3. Information explaining why further referral is necessary |
| Laboratory test | Information about the rationale, process, and interpretations associated with laboratory tests or medical exams to diagnose or monitor a health condition | 1. Rationale: why a specific lab test is needed 2. Process: how to do a specific laboratory test (e.g., blood drawing or urine collection or something else; fasting or not) 3. Interpretations: what does a laboratory test result mean |
1. Information about the benefits and risks of different laboratory tests 2. Information about the procedures of laboratory tests 3. Information about interpretations of the results of laboratory tests |
| Self-care | Information about (a) the rationale and procedure of my own physical and dietary actions needed to maintain health, prevent disease, or control a health condition, (b) potential impact of the health condition on my work and daily life, and (c) signs and signals indicating when I should seek professional care | 1. Rational and procedure of physical and dietary action: why do I need to take an action to be healthy; what do I do to be healthy 2. Impact on work/daily life: how the health condition may affect my work and daily life 3. Signs/signals for when I need to seek help from a healthcare provider: when should I contact a healthcare provider |
1. Information about how diabetes may affect my work 2. Information about how diabetes may affect my personal life (e.g., sexual activity, smoking, alcohol use, hobbies) 3. Information about how to care for a diabetes-related wound or incision at home |
| CAM | Information about possible complementary or alternative treatments for a health condition | What CAM options are available; what are the benefits and risks of using of CAM | 1. Information about the benefits and risks of using CAM versus in combination with standard medicine 2. Information about when to get CAM 3. Information about where to get CAM |
| Psychosocial | Information about how to obtain assistance in dealing with feelings and family and social concerns resulting from a health condition | 1. Family: how to involve the family 2. Peers: how to get support from others who have the same condition 3. Social concerns: how society may perceive/react to someone with the health condition |
1. Information about support groups where I can talk with other people with diabetes 2. Information about how the treatment may affect feelings about myself 3. Information about how to involve my family in dealing with feelings about diabetes |
| Healthcare provider | Information about the credentials, experiences, and reputations of medical professionals and facilities, including the types and quality of services they provide | 1. Credentials/experiences/reputations of medical professionals (e.g., physicians, nurses, pharmacists) 2. Credentials/experiences/reputations of medical facilities (e.g., clinics, hospitals) |
1. Information about the credentials, experiences, or reputations of a particular medical facility 2. Information about the credentials, experiences, or reputations of a particular medical specialist |
CAM, complementary and alternative medicine.
Results
The final sample numbered 95 apps: 43 for Android, 38 for iOS, and 14 that ran on both Android and iOS. All Android apps were free. Five of the iOS apps required a fee that ranged from $0.99 to $1.99 for downloading. All apps were released during 2011–2014, with 2014 seeing the highest number for both Android and iOS. The features and types of health information provided by the apps are summarized in Table 2.
Table 2.
Year When Each Application (App) Was Released, Features, and Types of Health Information Provided by Chinese Diabetes Apps
| ANDROID | IOS | ANDROID/IOS | TOTAL | |
|---|---|---|---|---|
| Year app was released | ||||
| 2011 | 4 (9) | 6 (16) | 4 (29) | 14 (15) |
| 2012 | 5 (12) | 5 (13) | 0 (0) | 10 (11) |
| 2013 | 5 (12) | 10 (26) | 0 (0) | 15 (16) |
| 2014 | 29 (67) | 17(45) | 10 (71) | 56 (59) |
| Features | ||||
| Education | 31 (72) | 30 (79) | 10 (71) | 71 (75) |
| Diet management | 24 (56) | 22 (58) | 4 (29) | 50 (53) |
| Blood glucose | 23 (53) | 31 (82) | 8 (57) | 62 (65) |
| Insulin | 21 (49) | 23 (61) | 3 (21) | 47 (49) |
| Physical activity | 20 (47) | 18 (47) | 4 (29) | 42 (44) |
| Calorie count | 16 (37) | 13 (34) | 4 (29) | 33 (35) |
| Oral diabetes medications | 14 (33) | 13 (34) | 3 (21) | 30 (32) |
| Communication | 12 (28) | 17 (45) | 6 (43) | 35 (37) |
| Weight | 12 (28) | 13 (34) | 4 (29) | 29 (31) |
| Family | 10 (23) | 10 (26) | 3 (21) | 23 (24) |
| Disease-related alerts or reminds | 9 (21) | 14 (37) | 6 (43) | 29 (31) |
| Cholesterol information/medications | 9 (21) | 3 (8) | 1 (7) | 13 (14) |
| Blood pressure | 7 (16) | 4 (11) | 2 (14) | 13 (14) |
| Peer | 6 (14) | 4 (11) | 3 (21) | 13 (14) |
| BMI | 5 (12) | 4 (11) | 1 (7) | 10 (11) |
| Type of health information | ||||
| Treatment | 35 (81) | 26 (68) | 13 (93) | 74 (78) |
| Health condition specific | 34 (79) | 20 (53) | 7 (50) | 61 (64) |
| Self-care | 34 (79) | 32 (84) | 10 (71) | 76 (80) |
| Psychosocial | 14 (33) | 11 (29) | 3 (21) | 28 (29) |
| Laboratory test | 11 (26) | 2 (5) | 2 (14) | 15 (16) |
| Healthcare provider | 9 (21) | 12 (32) | 2 (14) | 23 (24) |
| CAM | 3 (7) | 4 (11) | 0 (0) | 7 (7) |
Data are n (%).
BMI, body mass index; CAM, complementary and alternative medicine.
Seven (7%) of the apps had none of the 15 features, 44 (46%) had 1–5, 39 (41%) had 6–10, and only 5 (5%) had more than 10 (Table 3).
Table 3.
Number of Features Provided in Each Chinese Diabetic Application
| NUMBER OF FEATURES | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TYPE OF APPLICATION | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 |
| Android | 3 | 1 | 7 | 8 | 2 | 4 | 2 | 3 | 4 | 3 | 4 | 1 | 0 | 1 | 0 | 0 |
| iOS | 3 | 2 | 5 | 3 | 3 | 1 | 4 | 4 | 1 | 3 | 6 | 3 | 0 | 0 | 0 | 0 |
| Android/iOS | 1 | 2 | 0 | 3 | 3 | 0 | 1 | 1 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 7 | 5 | 12 | 14 | 8 | 5 | 7 | 8 | 7 | 7 | 10 | 4 | 0 | 1 | 0 | 0 |
Six (6%) of the apps provided none of the seven types of health information defined by the HIW framework, 49 (52%) provided one to three types of information, and 40 (42%) provided four to six. No app provided all seven types (Table 4).
Table 4.
Numbers of Types of Health Information Provided in Each Chinese Diabetes Application
| NUMBER OF TYPES OF HEALTH INFORMATION | ||||||||
|---|---|---|---|---|---|---|---|---|
| TYPE OF APPLICATION | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| Android | 1 | 3 | 10 | 6 | 18 | 3 | 2 | 0 |
| iOS | 5 | 4 | 6 | 9 | 10 | 4 | 0 | 0 |
| Android/iOS | 0 | 3 | 3 | 5 | 2 | 1 | 0 | 0 |
| Total | 6 | 10 | 19 | 20 | 30 | 8 | 2 | 0 |
Discussion
General patient education was the most common feature among the apps, followed by monitoring of blood glucose, diet/food/nutrition, insulin, and exercise/physical exercise. These are also the most common features in U.S. diabetes apps,12,26 supporting the generalizability of our findings. However, few apps included more than 12 of the 15 self-management features, and seven of the apps had none, suggesting that few of the apps could provide a comprehensive set of tools for diabetes self-management.13,21,27
Psychosocial support, disease-related alerts/reminders, and information about BP, cholesterol, and body mass index were featured in only a small percentage of the apps, suggesting that there is much room for improvement in the development of Chinese diabetes mobile apps. Evidence suggests that information about laboratory tests, CAM, healthcare providers, and psychosocial support are all important to patients.23–25 Information about psychosocial support, for example, affects patients' well-being,12,26,28 and psychosocial interventions can improve patients' diabetes self-management.1,3,8,29 Not providing information about the psychosocial aspects of diabetes self-management is a missed opportunity that should be addressed. The majority of the apps also did not provide information about healthcare providers or facilities, so those apps could not facilitate decisions about sources of treatment. In addition, CAM has been recommended as a supplement to standard treatments in chronic disease prevention and health promotion,30 but CAM information was least likely to be provided in the apps.
Shared decision-making is at the core of self-management and patient-centered care. It requires that patients be actively involved in their own care and decision-making and that healthcare providers provide services based on patients' personalized needs and preferences.31–34 Because the majority of the selected Chinese apps did not provide many of the features and types of information essential for diabetes self-management, we recommend the following for future mobile app development, diabetes research, and practice:
1. Diabetes apps should integrate more features that facilitate diabetes self-management.
2. M-health apps should provide a diverse range of types of health information, especially about laboratory tests, CAM, and healthcare providers.
3. Healthcare providers should examine the features and types of health information provided in apps so that they can recommend appropriate apps to patients.
A major limitation of this study is that we adapted the U.S. national standards for diabetes self-management to develop our list of features, and we used the U.S.-originated HIW framework to develop a list of the types of health information that patients might want. Although these algorithms formed a solid, justifiable foundation for our analyses, they do reflect a U.S. context and might not accurately reflect the environment and challenges that Chinese diabetic patients face. Some evidence suggests that there are differences in diabetic care and self-management practice between China and the United States.5,35 Future research should examine the cultural aspects of diabetes self-management.
Acknowledgments
Editorial support with manuscript development was provided by the Cain Center for Nursing Research and the Center for Transdisciplinary Collaborative Research in Self-Management Science (grant P30, NR015335) at the University of Texas at Austin School of Nursing.
Disclosure Statement
No competing financial interests exist.
References
- 1.Li X, Zhan Y, Wang Q, et al. . A sneak peak of the 2015 report on the market of type 2 diabetes mellitus diagnosis and treatment in China. Ann Transl Med 2015;3:120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hu H, Sawhney M, Shi L, et al. . A systematic review of the direct economic burden of type 2 diabetes in China. Diabetes Ther 2015;6:7–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.International Diabetes Federation. IDF diabetes atlas, sixth edition. 2014. Available at www.idf.org/sites/default/files/Atlas-poster-2014_EN.pdf (last accessed December8, 2015)
- 4.Tang WK, Ungvari GS, Chan GWL. Patients' and their relatives' knowledge of, experience with, attitude toward, and satisfaction with electroconvulsive therapy in Hong Kong, China. J ECT 2002;18:207–212 [DOI] [PubMed] [Google Scholar]
- 5.Hua W, Cao S, Cui J, Maberley D, Matsubara J. Analysis of reasons for noncompliance with laser treatment in patients of diabetic retinopathy. Can J Ophthalmol 2013;48:88–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xie B, Su Z, Liu Y, Wang M, Zhang M. Health information wanted and obtained from doctors/nurses: A comparison of Chinese cancer patients and family caregivers. Support Care Cancer 2015;23:2873–2880 [DOI] [PubMed] [Google Scholar]
- 7.Zhou Y, Liao L, Sun M, He G. Self-care practices of Chinese individuals with diabetes. Exp Ther Med 2013;5:1137–1142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van Vugt M, de Wit M, Cleijne WHJJ, Snoek FJ. Use of behavioral change techniques in web-based self-management programs for type 2 diabetes patients: Systematic review. J Med Internet Res 2013;15:e279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nathan DM. Long-term complications of diabetes mellitus. N Engl J Med 1993;328:1676–1685 [DOI] [PubMed] [Google Scholar]
- 10.Hassan A, Meo SA, Usmani AM, Shaikh TJ. Diabetes during Ramadan—PRE-approach model: Presentation, risk stratification, education. Eur Rev Med Pharmacol Sci 2014;18:1798–1805 [PubMed] [Google Scholar]
- 11.Camerini L, Schulz PJ, Nakamoto K. Differential effects of health knowledge and health empowerment over patients' self-management and health outcomes: A cross-sectional evaluation. Patient Educ Couns 2012;89:337–344 [DOI] [PubMed] [Google Scholar]
- 12.El-Gayar O, Timsina P, Nawar N, Eid W. Mobile applications for diabetes self-management: Status and potential. J Diabetes Sci Technol 2013;7:247–262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arnhold M, Quade M, Kirch W. Mobile applications for diabetics: A systematic review and expert-based usability evaluation considering the special requirements of diabetes patients age 50 years or older. J Med Internet Res 2014;16:e104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sultan S, Mohan P. Self-regulated learning in a mobile health initiative for diabetic patients. 2012 IEEE 12th International Conference on Advanced Learning Technologies (ICALT) Rome: IEEE, 2012;706–707 [Google Scholar]
- 15.Lyles CR, Harris LT, Le T, et al. . Qualitative evaluation of a mobile phone and web-based collaborative care intervention for patients with type 2 diabetes. Diabetes Technol Ther 2011;13:563–569 [DOI] [PubMed] [Google Scholar]
- 16.Wildevuur SE, Simonse LW. Information and communication technology–enabled person-centered care for the “big five” chronic conditions: Scoping review. J Med Internet Res 2015;17:e77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goh G, Tan NC, Malhotra R, et al. . Short-term trajectories of use of a caloric-monitoring mobile phone app among patients with type 2 diabetes mellitus in a primary care setting. J Med Internet Res 2015;17:e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boulos MNK, Brewer AC, Karimkhani C, Buller DB, Dellavalle RP. Mobile medical and health apps: State of the art, concerns, regulatory control and certification. Online J Public Health Inform 2014;5:e229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pew Research Center Global Attitudes Project. Global digital communication: Texting, social networking popular worldwide. 2011. Available at www.pewglobal.org/files/2011/12/Pew-Global-Attitudes-Technology-Report-FINAL-December-20-2011.pdf (last accessed December8, 2015)
- 20.Mobithinking. Global mobile statistics 2014 part A: Mobile subscribers; handset market share; mobile operators. 2014. Available at https://mobiforge.com/research-analysis/global-mobile-statistics-2014-part-a-mobile-subscribers-handset-market-share-mobile-operators (last accessed December8, 2015)
- 21.Chomutare T, Fernandez-Luque L, Årsand E, Hartvigsen G. Features of mobile diabetes applications: Review of the literature and analysis of current applications compared against evidence-based guidelines. J Med Internet Res 2011;13:e65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.American Diabetes Association. Standards of medical care in diabetes—2015. Diabetes Care 2015;38(Suppl 1):S1–S93 [PubMed] [Google Scholar]
- 23.Xie B, Wang M, Feldman R, Zhou L. Exploring older and younger adults' preferences for health information and participation in decision making using the Health Information Wants Questionnaire (HIWQ). Health Expect 2014;17:795–808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xie B. Older adults' health information wants in the internet age: Implications for patient-provider relationships. J Health Commun 2009;14:510–524 [DOI] [PubMed] [Google Scholar]
- 25.Xie B, Wang M, Feldman R. Preferences for health information and decision-making: development of the Health Information Wants (HIW) questionnaire. Proceedings of iConference New York: ACM, 2011;273–280 [Google Scholar]
- 26.Ristau RA, Yang J, White JR. Evaluation and evolution of diabetes mobile applications: Key factors for health care professionals seeking to guide patients. Diabetes Spectrum 2013;26:211–215 [Google Scholar]
- 27.Arnhold M, Quade M, Kirch W. Mobile applications for diabetics: A systematic review and expert-based usability evaluation considering the special requirements of diabetes patients age 50 years or older. J Med Internet Res 2014;16:e104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cotter AP, Durant N, Agne AA, Cherrington AL. Internet interventions to support lifestyle modification for diabetes management: A systematic review of the evidence. J Diabetes Complications 2014;28:243–251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Silver MP. Patient perspectives on online health information and communication with doctors: A qualitative study of patients 50 years old and over. J Med Internet Res 2015;17:e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hawk C, Ndetan H, Evans MW., Jr Potential role of complementary and alternative health care providers in chronic disease prevention and health promotion: An analysis of National Health Interview Survey data. Prev Med 2012;54:18–22 [DOI] [PubMed] [Google Scholar]
- 31.Anderson RM, Funnell MM. Using the empowerment approach to help patients change behavior. In: Anderson BJ, Rubin RR, eds. Practical psychology for diabetes clinicians, 2nd ed. Alexandria, VA: American Diabetes Association, 2002:3–12 [Google Scholar]
- 32.Aujoulat I, D'Hoore W, Deccache A. Patient empowerment in theory and practice: Polysemy or cacophony? Patient Educ Couns 2007;66:13–20 [DOI] [PubMed] [Google Scholar]
- 33.Epstein RM, Street RL., Jr The values and value of patient-centered care. Ann Fam Med 2011;9:100–103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bravo P, Edwards A, Barr PJ, et al. . Conceptualising patient empowerment: A mixed methods study. BMC Health Serv Res 2015;15:252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zeng B, Sun W, Gary RA, Li C, Liu T. Towards a conceptual model of diabetes self-management among Chinese immigrants in the United States. Int J Environ Res Public Health 2014;11:6727–6742 [DOI] [PMC free article] [PubMed] [Google Scholar]