Abstract
Introduction: The alteration in serum lipid profile; increase in total cholesterol (TC), triacylglycerol (TAG), and low-density lipoprotein cholesterol (LDL-C); and reduction in high-density lipoprotein cholesterol (HDL-C) are key factors in cardiovascular disease progression. The high prevalence and severity of cardiovascular diseases require new screening tools for better evaluation. Atherogenic index (AI) (LDL-C/HDL-C) and coronary risk index (CRI) (TC/HDL-C) can be strong markers for predicting the risk of atherosclerosis and coronary heart disease and disclose the presence of LDL or TAG in the serum of related patients. To implement this strategy, the AIs and CRIs in our population were assessed. In this study, a total of 5207 subjects were recruited and AIs and CRIs were calculated for all of them. According to our data, age, body mass index, sex, as well as CRI and AI had affirmative correlation with TC, LDL-C, TAG, systolic blood pressure, and diastolic blood pressure. By increasing these factors, AIs and CRIs were augmented. Moreover, in situations where all atherogenic parameters are normal, these parameters may be the alternative screening tool.
Keywords: Atherogenic index, cardiovascular disease, lipid profile, coronary risk index
Introduction
Noncommunicable diseases (NCDs), such as cardiovascular diseases (CVDs), diabetes, cancers, and chronic respiratory diseases, are typically found in developed countries due to the predominantly sedentary lifestyle and cause 63% or more deaths in the world. By increasing the risk factors, CVD is one of the most prominent NCDs and it is the cause of one-third of deaths worldwide.1 The increased cardiovascular risk in the world population could have several causes including dyslipidemia, diabetes mellitus, hypertension (HTN), higher body mass index (BMI), higher waist to hip ratio, or impaired physical fitness.2 Among these, the plasma lipid profile is the major risk factor and predictor for CVD, acute myocardial infarction, and stroke.3
Previous studies indicated that total cholesterol (TC) is a risk factor for carotid atherosclerosis and has been associated with high-serum triglyceride (TG) and low-serum high-density lipoprotein cholesterol (HDL-C) concentrations.4 The importance of low-density lipoprotein (LDL) cholesterol in the development of atherosclerosis has long been recognized, and LDL-C remains the primary target of the therapy for the prevention of coronary heart disease (CHD). Nevertheless, increasing research attention over the past decade has been devoted to the heterogeneity of LDL-C particles and the atherogenicity of lipids and lipoproteins other than LDL-C.5 On that basis, atherogenic dyslipidemia, defined as high LDL-C/HDL-C ratio and high TAG, is associated with high cardiovascular risk.6 For better evaluation and to predict the risk of CVD, many clinical studies have attempted to introduce another marker of atherogenic dyslipidemia such as atherogenic index (AI) and coronary risk index (CRI).7
It is known that a large number of cardiovascular risk factors are modifiable, and so far, efforts have been put in this direction but much more is needed. For this purpose, it is necessary to know how these different risk factors affect each other. Within this context and to clarify the role and contribution of the lipid atherogenic risk that could help predict CVD risk, the correlation between AI, as a major risk factor of CVD, and other important factors such as BMI, HTN, waist circumference, and lipid status were assessed.
Methods
A total of 5207 subjects (2499 men and 2708 women), aged between 15 and 70 years, were asked to complete a checklist of study variables and patients’ blood sample results including sex (male, female), age (<30, 31-40, 41-50, >50), waist circumference (obese >90 cm for both sexes), fasting blood glucose (mg/dL), cholesterol (mg/dL), TG (mg/dL), HDL (mg/dL), and LDL (mg/dL) after obtaining informed consent. The protocol for the study was approved by the Research and Ethics Committee of Birjand University of Medical Sciences. The anthropometric measurements were determined by weighting scale and measuring tape. Based on the values of BMI, participants were classified as underweight (BMI < 18.5 kg/m2), normal (BMI: 18.5-24.9 kg/m2), overweight (BMI: 25-29.9 kg/m2), and obese (BMI ≥ 30 kg/m2). After completing the checklist, fasting blood samples were collected and sent to the lab. Serum was separated and stored in a freezer at −20°C until testing.7 Atherogenic index (AI = LDL-C/HDL-C) and CRI (CRI = TC/HDL-C) were calculated for all subjects. Plasma lipid abnormality was based on the expert panel of the National Cholesterol Education Program (NCEP) cutoff values.8 This study was approved by the research ethics committee of the university (Ethics Code 1392-09-22) and adhered to the Declaration of Helsinki.
The test results and medical recommendations were given to the patients and after surveying the information and ensuring that they were correctly entered into the IBM SPSS software (version 22), descriptive information was presented using mean and standard error and then data were analyzed by independent sample t test, 1-way analysis of variance method and Pearson correlation. A P value of less than .05 was considered significant.
Results
This study assessed the correlation between AI, as a major risk factor of CVD, and other important factors such as BMI, HTN, waist circumference, and lipid status. A total of 5207 subjects aged between 15 and 70 years were asked to complete a checklist of study variables and patients’ blood sample results.
Table 1 shows the general characteristics of the population study. From a total of 5207 participants, 2708 (52%) were women, most of them (1636 participants, 31.4%) were more than 50 years old, 1656 (31.8%) were overweight, and 881 (16.9%) were obese. In addition, 366 participants (7.0%) were in the habit of taking tobacco. Table 2 shows the mean and standard error of BMI, lipid profile, and AIs among the age groups. Based on the results, there were no significant differences in BMI values between age groups. Although TC, LDL-C, TG, CRI, and AI increase by age (P < .001), subjects less than 30 years had a higher mean of HDL-C (40.10) compared with subjects aged above 50 years (P < .001).
Table1.
General characteristics of the study.
| Variables | Frequency | % |
|---|---|---|
| Sex | ||
| Male | 2499 | 48 |
| Female | 2708 | 52 |
| Total | 5207 | 100 |
| Age groups, y | ||
| <30 | 1398 | 26.8 |
| 31–40 | 1172 | 22.5 |
| 41–50 | 1001 | 19.2 |
| >50 | 1636 | 31.4 |
| Total | 5207 | 100 |
| BMI groups, kg/m2 | ||
| <18.5 | 450 | 8.6 |
| 18.5–24.9 | 1897 | 36.4 |
| 25–29.9 | 1656 | 31.8 |
| >30 | 881 | 16.9 |
| Total | 4884 | 93.8 |
| Tobacco intake | ||
| Yes | 366 | 7.0 |
| No | 4776 | 91.7 |
Abbreviation: BMI, body mass index.
Table 2.
Comparison of BMI, lipid profile, and atherogenic indices among the age groups.
| Variables | Age groups, y | |||
|---|---|---|---|---|
| <30 | 31-40 | 41-50 | >50 | |
| BMI | 24.14 (0.75) | 27.37 (2.18) | 33.55 (5.39) | 28.69 (1.67) |
| Total cholesterol | 170.19 (0.89)b,c,d | 186.16 (1.01)a,c,d | 193.42 (1.09)a,b,d | 201.46 (0.97)a,b,c |
| LDL-C | 108.89 (0.85)b,c,d | 120.17 (0.97)a,c,d | 124.37 (1.06)a,b,d | 131.27 (0.88)a,b,c |
| HDL-C | 40.10 (0.23)d | 39.56 (0.24) | 39.30 (0.26) | 39.33 (0.19)a |
| Triglyceride | 126.25 (1.85)b,c,d | 145.77 (2.29)a,c,d | 164.89 (2.83)a,b | 170.53 (2.41)a,b |
| CRI | 4.38 (0.03)b,c,d | 4.86 (0.03)a,c,d | 5.08 (0.03)a,b,d | 5.26 (0.03)a,b,c |
| AI | 2.79 (0.02)b,c,d | 3.12 (0.03)a,c,d | 3.25 (0.03)a,b,d | 3.41 (0.02)a,b,c |
Abbreviations: AI, atherogenic index; BMI, body mass index; CRI, coronary risk index; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein.
Significant difference with first group.
Significant difference with second group.
Significant difference with third group.
Significant difference with last group.
Table 3 shows a comparison of lipid profile and AIs among the BMI categories. Based on the results, TC, CRI, and AI increased by age (P < .001). Moreover, the mean LDL-C was significantly different in BMI categories and increased with age except in overweight and obese subjects. Also, the mean HDL-C in the underweight and normal groups was statistically different from the overweight and obese groups (P < .001). The HDL-C mean was more in underweight and normal subjects than the 2 other groups. The same results were observed for TG. In addition, overweight and obese subjects had a significant difference in means and it also increased by age (P < .001).
Table 3.
Comparison of lipid profile and atherogenic indices among the BMI groups.
| Variables | BMI groups, kg/m2 | |||
|---|---|---|---|---|
| <18.5 (n = 450) | 18.5-24.9 (n = 1897) | 25-29.9 (n = 1656) | ≥30 (n = 881) | |
| Total cholesterol | 175.07 (1.65)b,c,d | 182.33 (0.82)a,c,d | 193.21 (0.88)a,b,d | 197.39 (1.24)a,b,c |
| LDL-C | 111.92 (1.46)b,c,d | 118.92 (0.76)a,c,d | 123.90 (0.81)a,b | 127.09 (1.19)a,b |
| HDL-C | 40.82 (0.38)c,d | 40.38 (0.19)c,d | 38.95 (0.19)a,b | 38.42 (0.26)a,b |
| Triglyceride | 123.94 (3.36)c,d | 133.06 (1.62)c,d | 166.80 (2.23)a,b,d | 178.62 (3.00)a,b,c |
| CRI | 4.40 (0.05)b,c,d | 4.65 (0.02)a,c,d | 5.11 (0.03)a,b,d | 5.30 (0.04)a,b,c |
| AI | 2.81 (0.04)b,c,d | 3.03 (0.02)a,c,d | 3.26 (0.02)a,b,d | 3.39 (0.03)a,b,c |
Abbreviations: AI, atherogenic index; BMI, body mass index; CRI, coronary risk index; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein.
Significant difference with first group.
Significant difference with second group.
Significant difference with third group.
Significant difference with last group.
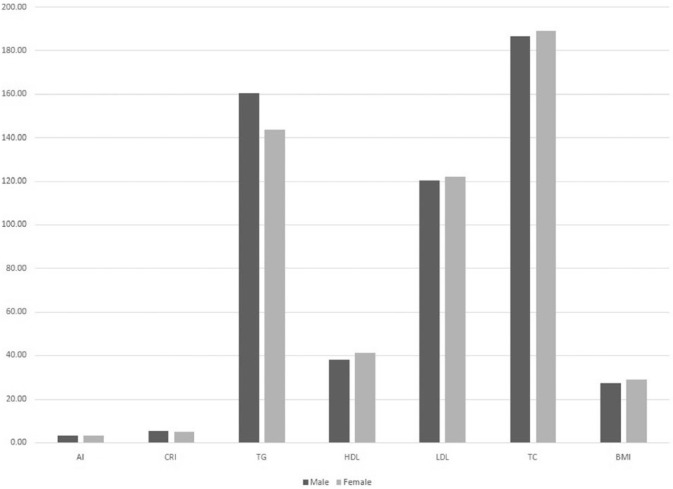
The results of the comparison of lipid profiles by sex (Figure 1) showed that the mean values of TC (P = .012) and HDL-C (P < .001) were more in women than men (189.19, 41.17 in women and 186.91, 37.88 in men). Moreover, the results indicated that the mean values of TG (P < .001), CRI (P < .001), and AI (P < .001) were more in men than women (160.72, 5.08, and 3.26 in men; 143.93, 4.74, and 3.05 in women). In addition, LDL and BMI levels showed no significant difference by sex.
Figure 1.
Comparison of BMI, lipid profile, and atherogenic indices related to sex. AI indicates atherogenic index; BMI, body mass index; CRI, coronary risk index; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; TC, total cholesterol; TG, triglyceride.
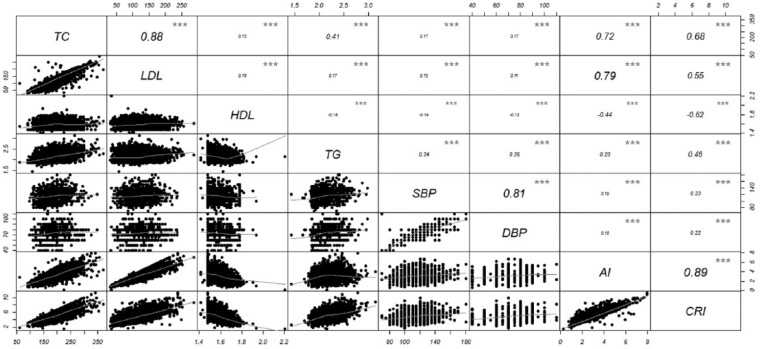
Figure 2 shows the correlation between lipid profile and AIs in a correlation matrix figure (vertical axis and horizontal axis are variables mentioned in the diameter). The CRI has a positive and significant relationship with TC, LDL-C, systolic blood pressure (SBP), diastolic blood pressure (DBP), and TG. In other words, CRI increases with increasing TC, LDL-C, or TAG values (P < .001). In addition, the relationship between CRI and HDL-C was significantly negative. Thus, CRI increases with a decrease in HDL-C and vice versa (P < .001). Another index, AI, has a direct relationship with TC, LDL-C, SBP, DBP, and TAG; it means that AI increases with increasing TC, LDL-C, or TAG values (P < .001). The relationship between AI and HDL-C was significantly negative and AI increases with decrease in HDL-C and vice versa (P < .001).
Figure 2.
Correlation between lipid profile and atherogenic indices. AI indicates atherogenic index; CRI, coronary risk index; DBP, diastolic blood pressure; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; SBP, systolic blood pressure; TC, total cholesterol; TG, triglyceride.
***Statistically significant at α = .001
Discussion
The alteration in the serum levels of the lipid profile; increase in TC, TG, and LDL-C; and decrease in HDL-C are major factors for the development of CVDs.9,10 Atherogenic index (LDL-C/HDL-C) and CRI (TC/HDL-C) as a strong marker to predict the risk of atherosclerosis and CHD and noninvasive parameters reveal the presence of LDL or TAG in the serum of related patients. Recently, it has been demonstrated that investigators provide considerable predictors.10–13 Furthermore, in conditions where other atherogenic risk parameters seem normal, AI and CRI may be the alternative diagnostic choices. In this study, it appears that there is a correlation between aging, BMI, sex, and CVDs; therefore, an estimate was made of the cross-sectional association between AI and other risk factors of CVD among 5207 candidate individuals in Birjand, east of Iran.
The results showed that 31.4% of candidate individuals are more than 50 years old and by aging the TC, LDL-C, TAG, CRI, and AI increased and were statistically significant.
The BMI reached the highest level in individuals aged between 41 and 50 years. Total cholesterol, LDL-C, TAG, CRI, and AI increased with increasing BMI. By comparing the lipid profile with AI in related subjects, TC, CRI, and AI increased (P < .001) among the candidates. Furthermore, HDL-C and TAG were statistically significant in this population; although TAG was seen more in obese and overweight individuals and vice versa for HDL-C (P < .001).
Overall, the women had more BMI than the men. By comparing the lipid profile with sex, the mean values of TC and HDL-C were higher in women, whereas the mean values of TAG, CRI, and AI were more in men. These findings were statistically significant.
According to our data, CRI and AI had affirmative correlation with TC, LDL-C, TAG, SBP, and DBP. By increasing these factors, these 2 indices were augmented.
According to previous studies, all these parameters are important risk factors for CVD.
A concordance was observed between increased AI and the significant increase in the value of, LDL-C, TC, and TAG, as well as SBP and DBP. This result is similar to the results of Karen et al.14,15
In accordance with our study, in a sample of Turkish population, the high AI of the plasma reflected obesity and hyperinsulinemia in men. It independently predicts CHD and type 2 diabetes in men and in women, high blood pressure, and metabolic syndrome. Therefore, high AI of plasma (AIP) is a powerful risk factor for coronary artery disease in both Turkish men and women.16
In line with this study, Pallavi et al assessed the AI and lipid profile in obese and nonobese women. They showed that in middle-aged women, the significant increase in AI was linked with increasing BMI (P < .05).17
In agreement with our data, Jobert et al reported that AIP may not be an independent factor affecting the risk of CVD among Cameroonian postmenopausal women. Results from this study showed that AIP and the risk of CVD were significantly correlated with each other; however, this correlation was weak (r = .369).18
Moreover, Nwagha and Igwe19 showed the massive contributions of TAG to cardiovascular risk. In fact, high levels of TAG have been linked with an increased incidence of CHD.20 Furthermore, the results indicated that AIP has a statistically marked difference (P = .001) between patients and healthy people. It revealed their positive association with severity of CHD.
Furthermore, Hadaegh et al9 reported that among Iranian men, the TAG/HDL-C ratio has disclosed a considerable adjusted (multivariable) risk ratio of 1.75 which was similar to the observation of Onat et al.16 They demonstrated that among women with myocardial ischemia, the TAG/HDL-C ratio was monitored to be an independent predictor of cardiovascular incidents and of mortality in multi-adjusted models.21
Niroumand et al22 stated that male participants were dominant in the increased-risk AIP category; hence, they were at a higher risk of developing CHD. This finding agrees with the study of Khazaál.23
It has been reported that AIP plays a predictive role for atherosclerosis24,25 and can be used as an available index of the highest sensitivity for assessing cardiovascular risk factors and for predicting acute coronary events.26 Moreover, in situations where all atherogenic parameters are normal, AIP may be the alternative screening tool.23
Conclusions
The result of this study can be applied to return the bleak prognosis of CVD and also can help policymakers to implement a population strategy in association with a high-risk group strategy for CVD prevention and reduce the burden of CVD in future decades.
In this study, risk factors such as alcohol consumption, physical activity, and diet were not considered, in the event that this information enables us to have a more accurate evaluation. Considering common and uncommon risk factors together promoted the prognosis and prevention of metabolic disorders.
Acknowledgments
The authors express their thanks to Birjand Cardiovascular Diseases Research Center, Vali-Asr Hospital Clinical Research Database, and also Hepatitis Research Center, Birjand University of Medical Sciences, Birjand, Iran. They would like to thank all individuals who helped kindly in this investigation as well.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: TK and MZ contributed to the conception or design of the work. MHa, MH, and MM contributed to the acquisition, analysis, or interpretation of data. TK and MH contributed to drafting the work or revising it critically for important intellectual content. The manuscript has been read and approved by all the authors and each author believes that the manuscript represents honest work.
References
- 1. Kazemi T, Sharifzadeh GR, Zarban A, et al. Risk factors for premature myocardial infarction: a matched case-control study. J Res Health Sci. 2011;11:77–82. [PubMed] [Google Scholar]
- 2. Kazemi T, Sharifzadeh G, Zarban A, Fesharakinia A. Comparison of components of metabolic syndrome in premature myocardial infarction in an Iranian population: a case control study. Int J Prev Med. 2013;4:110–114. [PMC free article] [PubMed] [Google Scholar]
- 3. Dehghani Firoozabadi M, Kazemi T, Sharifzadeh G, Dadbeh S, Dehghan P. Stroke in Birjand, Iran: a hospital-based study of acute stroke. Iran Red Crescent Med J. 2013;15:264–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Landray M, Sagar G, Muskin J, Murray S, Holder R, Lip G. Association of atherogenic low-density lipoprotein subfractions with carotid atherosclerosis. Quar J Med. 1998;91:345–351. [DOI] [PubMed] [Google Scholar]
- 5. Carmena R, Duriez P, Fruchart JC. Atherogenic lipoprotein particles in atherosclerosis. Circulation. 2004;109:III-2-III-7. [DOI] [PubMed] [Google Scholar]
- 6. Manninen V, Tenkanen L, Koskinen P, et al. Joint effects of serum triglyceride and LDL cholesterol and HDL cholesterol concentrations on coronary heart disease risk in the Helsinki Heart Study: implications for treatment. Circulation. 1992;85:37–45. [DOI] [PubMed] [Google Scholar]
- 7. Ebrahimzadeh A, Azarkar Z, Ziaee M, Sharifzadeh G, Bijari B. Prevalence and risk factors of hepatitis c infection (HCV) in Birjand, Iran, 2014. Int J Infect. 2016;3:e34102. [Google Scholar]
- 8. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 9. Hadaegh F, Khalili D, Ghasemi A, Tohidi M, Sheikholeslami F, Azizi F. Triglyceride/HDL-cholesterol ratio is an independent predictor for coronary heart disease in a population of Iranian men. Nutr Metab Cardiovasc Dis. 2009;19:401–408. [DOI] [PubMed] [Google Scholar]
- 10. Conkbayir C, Burak A, Ökçün EB. Lipid variables related to the extent and severity of coronary artery disease in non-diabetic Turkish Cypriots. Iran J Public Health. 2015;44:1196. [PMC free article] [PubMed] [Google Scholar]
- 11. Barzi F1, Patel A, Woodward M, et al. ; Collaboration APCS. A comparison of lipid variables as predictors of cardiovascular disease in the Asia Pacific region. Ann Epidemiol. 2005;15:405–413. [DOI] [PubMed] [Google Scholar]
- 12. Gaziano JM, Hennekens CH, O’Donnell CJ, Breslow JL, Buring JE. Fasting triglycerides, high-density lipoprotein, and risk of myocardial infarction. Circulation. 1997;96:2520–2525. [DOI] [PubMed] [Google Scholar]
- 13. Bampi ABA, Rochitte CE, Favarato D, Lemos PA, Da Luz PL. Comparison of non-invasive methods for the detection of coronary atherosclerosis. Clinics (Sao Paulo). 2009;64:675–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kearns K, Dee A, Fitzgerald AP, Doherty E, Perry IJ. Chronic disease burden associated with overweight and obesity in Ireland: the effects of a small BMI reduction at population level. BMC Public Health. 2014;14:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jiang Y, Chen Y, Manuel D, Morrison H, Mao Y. Quantifying the impact of obesity category on major chronic diseases in Canada. Sci World J. 2007;7:1211–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Onat A, Can G, Kaya H, Hergenç G. Atherogenic index of plasma (log10 triglyceride/high-density lipoprotein-cholesterol) predicts high blood pressure, diabetes, and vascular events. J Clin Lipidol. 2010;4:89–98. [DOI] [PubMed] [Google Scholar]
- 17. Kanthe PS, Patil BS, Bagali S, Deshpande A, Shaikh GB, Aithala M. Atherogenic index as a predictor of cardiovascular risk among women with different grades of obesity. Int J Collab Res Int Med Public Health. 2012;4:1767–1774. [Google Scholar]
- 18. Nansseu JRN, Moor VJA, Nouaga MED, Zing-Awona B, Tchanana G, Ketcha A. Atherogenic index of plasma and risk of cardiovascular disease among Cameroonian postmenopausal women. Lipids Health Dis. 2016;15:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nwagha UI, Igwe J. Atherogenic index of plasma: a significant indicator for the onset of atherosclerosis during menopause in hypertensive females of South East Nigeria. J College Med. 2006;10:67–71. [Google Scholar]
- 20. Hokanson JE, Austin MA. Plasma triglyceride level is a risk factor for cardiovascular disease independent of high-density lipoprotein cholesterol level: a metaanalysis of population-based prospective studies. J Cardiovasc Risk. 1996;3:213–219. [PubMed] [Google Scholar]
- 21. Bittner V, Johnson BD, Zineh I, et al. The triglyceride/high-density lipoprotein cholesterol ratio predicts all-cause mortality in women with suspected myocardial ischemia: a report from the women’s ischemia syndrome evaluation (WISE). Am Heart J. 2009;157:548–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Niroumand S, Khajedaluee M, Khadem-Rezaiyan M, et al. Atherogenic index of plasma (AIP): a marker of cardiovascular disease. Med J Islamic Republic Iran. 2015;29:240. [PMC free article] [PubMed] [Google Scholar]
- 23. Khazaál MS. Atherogenic index of plasma (AIP) as a parameter in predicting cardiovascular risk in males compared to the conventional dyslipidemic indices (cholesterol ratios). Karbala J Med. 2013;6:1506–1511. [Google Scholar]
- 24. Njajou OT, Kanaya AM, Holvoet P, et al. Association between oxidized LDL, obesity and type 2 diabetes in a population-based cohort, the health, aging and body composition study. Diabetes Metab Res Rev. 2009;25:733–739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Daniels L, Laughlin G, Sarno M. Lp-PLA2 is an independent predictor of incident coronary heart disease in appparently healthy older population. J Am Col Cardiol. 2008;51:913–919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dobiásová M, Urbanová Z, Samánek M. Relations between particle size of HDL and LDL lipoproteins and cholesterol esterification rate. Physiol Res. 2005;54:159–165. [PubMed] [Google Scholar]