Abstract
Background:
Reconstruction of the anterior cruciate ligament (ACL) in the skeletally immature patient is frequently performed in hopes of preventing new or additional chondral damage and meniscal injuries. Patients within a few years of skeletal maturity are more at risk for ACL injuries than prepubescent patients, about whom several physeal-sparing techniques have been described. Reconstruction techniques in the former higher risk group need to be better understood.
Purpose:
To review a series of adolescent patients with ACL injuries surgically treated with the hybrid physeal-sparing technique.
Study Design:
Case series; Level of evidence, 4.
Methods:
Surgical logs of ACL reconstructions (ACLRs) performed at a single pediatric/adolescent sports medicine center over a 6-year period were reviewed. Patients with open physes who had undergone ACLR with a femoral physeal-sparing tunnel and transphyseal tibial tunnel were identified. Their demographics, operative reports, rehabilitative course, time to return to play, outcome scores, and postoperative radiographs were collected and analyzed.
Results:
Twenty-three patients with a mean chronological age and bone age of 13.0 and 13.6 years, respectively, were identified. Examination and subjective outcome scores were obtained at a mean of 19 months and overall demonstrated positive results, with a mean Pediatric International Knee Documentation Committee (Pedi-IKDC) score of 96.0 and a mean Anterior Cruciate Ligament–Return to Sport after Injury (ACL-RSI) score of 89.1. Full-length mechanical axis films obtained at a mean 21 months postoperatively demonstrated no leg-length discrepancies or angular deformities in 21 of 23 patients. Two patients had an identified growth disturbance in the form of femoral and tibial growth acceleration on the ACL-reconstructed limb.
Conclusion:
The femoral physeal-sparing with transphyseal tibial drilling “hybrid” technique in skeletally maturing patients appears to have a high rate of success with low morbidity. However, the possibility of physeal abnormalities does exist, which demonstrates the importance of a close postoperative follow-up and evaluation until skeletal maturity is achieved. ACLR in skeletally immature patients is performed on an increasingly regular basis. Establishing the best and safest technique to do so is therefore important.
Keywords: skeletally immature, anterior cruciate ligament reconstruction, physeal sparing
While once considered rare, anterior cruciate ligament (ACL) ruptures are now increasingly diagnosed in skeletally immature athletes.28,32,44 Nonoperative treatment until skeletal maturity with reduction or avoidance of sport participation with external bracing during physical activity to help maintain knee stability is possible.7,30 However, long-term follow-up of this treatment method has demonstrated that an ACL-deficient knee in a skeletally immature patient increases the risk for meniscal and chondral damage, instability, and ultimately decreased ability to return to higher level sports.∥
ACL injuries in skeletally immature athletes are more commonly being diagnosed, especially in high school–aged student-athletes.12,27 Along with the increase in ACL tear rates, the rates of ACL reconstruction (ACLR) are also increasing, creating a concern as well as a true incidence of complications associated with growth disturbances.9 Currently, several different surgical technique options exist for ACLR in a skeletally immature patient population, including anatomic and nonanatomic physeal-sparing techniques. The use of the femoral and tibial transphyseal technique has also been described in this group. Nonanatomic physeal-sparing techniques have been developed to minimize any damage to the femoral or tibial physis.4,14,21,26,31 While the nonanatomic technique may be appropriate for very young prepubescent athletes, the transphyseal and physeal-sparing techniques offer the advantage of anatomic reconstruction. The specific technique that is best for the group of athletes at highest risk of ACL injuries, those within 2 to 3 years of skeletal maturity, has yet to be established. Some authors have recommended a transphyseal technique in this particular age group.37 However, adverse outcomes, specifically lower limb growth disturbances and angular deformities, have been reported with the use of this technique.15,16,19,20 Other authors have recommended physeal-sparing techniques to avoid these growth disturbances, although long-term studies regarding return-to-play and complication rates are few.17,20
There is a potential risk of growth disturbances with all of these techniques. Theoretically, the physeal-sparing techniques have a lower risk of injuries, but they are technically demanding, especially tibial physeal-sparing techniques. The creation of all-epiphyseal tunnels is constrained by the size of the epiphysis as well as the angle necessary to keep the tunnels away from the physes. Often, in drilling these tunnels, even in the best of circumstances, the tunnels’ entrance into the joint is an acute angle, creating the potential for increased graft stress at that point. Furthermore, while the graft itself may be epiphyseal, its location, especially on the tibia, may need to be in the metaphysis of the tibia. This places a “tension band” across the anteromedial tibial physis, increasing the risk of physeal angular growth disturbances.
For these reasons, a hybrid physeal-sparing technique for ACLR in skeletally immature patients has been developed. This technique is intended to provide anatomic reconstruction, minimizing the risk of growth disturbances while being less technically demanding and more reproducible. This technique uses a physeal-sparing tunnel in the lateral femoral epiphysis and a vertical transphyseal tunnel in the tibia. To the best of our knowledge, there are no studies currently in the literature that evaluate the outcomes and risk of this technique in young adolescents nearing skeletal maturity. Therefore, the purpose of this study was to retrospectively review a series of adolescent patients with ACL injuries surgically treated with the hybrid physeal-sparing technique at a single institution over a 6-year period. The primary aim was to evaluate for the presence of growth disturbances. The secondary aim was to subjectively evaluate clinical measures of knee function and athletic confidence.
Methods
Patients
Institutional review board approval was obtained for this study. A review of surgical records at our institution identified 436 patients who were ≤17 years of age at the time of their ACLR surgery between 2010 and 2016. Of these patients, 83 were identified as having open or closing tibial and femoral physes before surgical intervention. A further review of operative notes identified 38 patients treated with the hybrid physeal-sparing technique, of whom 23 patients were ≥1 year removed from their surgery and were included in this study.
Operative Technique
We prefer to perform a hybrid ACLR procedure using a femoral physeal-sparing retrograde drilling technique with a transtibial transphyseal technique for young athletes with a bone age of approximately 12 years, with at least 2 years of growth remaining as determined by a posteroanterior radiograph of the left hand.
Full diagnostic arthroscopic surgery was performed first in a standard fashion. If meniscal or chondral abnormalities were found, then their treatment was carried out before ACLR. Once the ACL tear was confirmed arthroscopically and associated abnormalities were treated, ACL remnants are debrided, and notchplasty was performed as necessary. Soft tissue grafts were used universally for physeal-sparing ACLR techniques, with a quadrupled gracilis-semitendinosus autograft being most commonly utilized. The pediatric ACL femoral guide (Arthrex) was directed to the center of the ACL femoral footprint, and fluoroscopy was used to confirm that the tunnel was positioned completely within the epiphysis. The femoral tunnel was drilled in a retrograde fashion a minimum of 20 mm in length and a suture placed for graft passage later.
A standard ACL guide was used for drilling the tibial tunnel in the center of the ACL tibial footprint. For this technique, the angle of the guide was increased to approximately 70° and the drilling starting point through the anteromedial incision used for hamstring harvest. Utilizing the tibial guide with this high angle reduced the cross-sectional area of the physis disturbed by the drill/tunnel by producing a vertically oriented tunnel through a more central portion of the tibial physis.
After graft passage, an adjustable loop cortical suspension device was used for fixation on the femoral side, and tibial fixation was performed using an interference screw, metaphyseal plate and screw (Double Spiked Plate; Smith & Nephew), cortical button, or staple. Tibial fixation was completed with the knee in near full extension. Fluoroscopy was used to help measure the distance from the physis to the anteromedial aperture. This was useful in determining if a minimum amount of space was available for interference screw fixation without violation of the physis. If the distance was too small, or by surgeon preference, distal fixation was completed with a cortical button, screw and post, or staple (Figure 1). Cycling the knee multiple times before tensioning the tibial side to reduce any creep in the loop systems was routinely performed.
Figure 1.
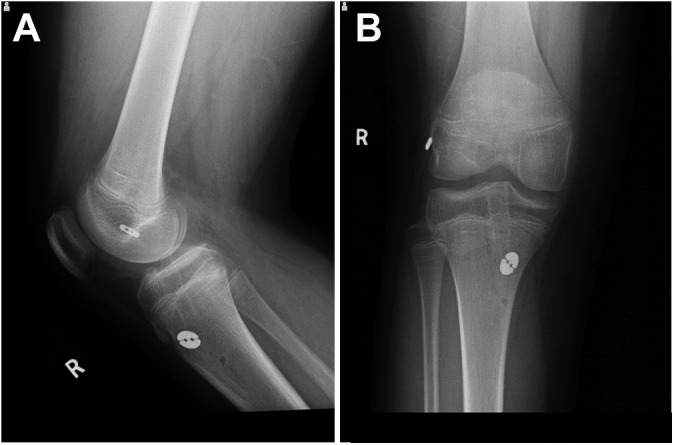
Imaging of a 14-year-old male patient 10 months after anterior cruciate ligament reconstruction of the right knee with a hybrid physeal-sparing technique. Postoperative (A) lateral and (B) anteroposterior radiographs depict a physeal-sparing tunnel in the lateral femoral epiphysis and a vertical transphyseal tunnel in the tibia. The hamstring autograft has a 14-mm round attachable button system (Arthrex) for tibial fixation and a TightRope RT adjustable loop button (Arthrex) for femoral fixation.
Postoperative Care and Return-to-Play Assessments
Postoperative rehabilitation included an emphasis on early range of motion. Once good quadriceps control was established, crutches and bracing were discontinued. Advancing to running was generally delayed until around 3 months and only if the patient demonstrated adequate quadriceps strength as demonstrated by a less than 30% deficit on isometric strength testing. Plyometrics and hop test training began in months 3 to 6. Patients had to demonstrate competency before the formal return-to-play assessment. All patients underwent a comprehensive return-to-play assessment that included clinical parameters (no pain, no swelling, symmetric range of motion), subjective outcomes including the Pediatric International Documentation Committee (Pedi-IKDC) score and Anterior Cruciate Ligament–Return to Sport after Injury (ACL-RSI) score, symmetric quadriceps and hamstring strength (<10% deficit on isometric and isokinetic strength testing), and multiple hop testing (as evaluated by a sports-trained physical therapist with an assessment of distance, symmetry, and form). Return-to-play assessments were conducted no earlier than 6 months postoperatively. Timing of physician clearance was obtained from clinical notes.
Radiographic Assessment
The postoperative radiographic evaluation during follow-up clinical appointments included a bilateral standing radiographic assessment for leg-length discrepancies. These images were used for the surveillance of growth disturbances in the postoperative period. Leg length was measured from the iliac crest to the tibial plafond. The measurement of angular deformities was also determined on the standing radiograph. The measurements obtained were the mechanical axis deviation (MAD), mechanical lateral distal femoral angle (MLDFA), and medial proximal tibial angle (MPTA). The MAD was measured in millimeters as the distance from the center of the knee joint between the femoral condyles and the mechanical axis line drawn from the center of the femoral head to the center of the talar dome. The MLDFA was measured as the angle between a line drawn from the center of the femoral head to the center of the knee joint between the femoral condyles and a transverse line tangential to the most distal points of the femoral condyles. The MPTA was measured as the angle between a transverse line tangential to the tibial plateau and a longitudinal line connecting the center of the proximal tibial plateau to the center of the talar dome. The MAD was used to determine if the knee was in varus or valgus alignment. A decreased MLDFA represents distal femoral valgus, and a decreased MPTA represents proximal tibial varus. A growth disturbance was defined as ≥1 cm of leg-length discrepancy and a statistically significant change in the MAD, MPTA, or MLDFA as compared with the nonsurgical limb. Measurements were conducted by all authors.
Subjective Outcomes
Subjective outcomes of knee function were evaluated with the Pedi-IKDC questionnaire.23 Athletic confidence was evaluated with the ACL-RSI questionnaire.43 Each questionnaire was completed by the patient or an accompanying adult postoperatively at each follow-up office visit.
Statistical Analysis
Statistical analyses were conducted using SAS (version 9.3; SAS Institute). Descriptive analysis was performed on patient demographics, return-to-play timing, and subjective outcome scores. Angular deformity measurements were not normally distributed; therefore, the nonparametric form of the t test, the Mann-Whitney U test, was used to compare differences between the surgical limb and nonsurgical limb. Statistical significance was set to .05.
Results
Patients
Twenty-three patients were included in this review (6 female, 17 male), with a mean chronological age at the time of surgery of 13.0 ± 1.4 years and a mean skeletal age of 13.6 ± 1.1 years. The mean hamstring autograft size was 7.8 mm in diameter (range, 6-9 mm). A hamstring autograft was used exclusively in this study, although a soft tissue quadriceps tendon autograft may also be an option. Nineteen patients reported that they were competitive athletes, participating in soccer, basketball, football, baseball, and skiing. Four patients reported that they were recreationally active and did not participate in competitive athletics before their ACL injury.
Surgical and Radiographic Outcomes
A radiographic evaluation to assess for growth disturbances was completed at a mean of 21 months (range, 10-57 months) after surgery, with all but 6 patients achieving skeletal maturity. At the time of the evaluation, there were 21 patients (91.3%) with equal leg lengths bilaterally (discrepancies <1.0 cm) and 2 patients (8.7%) with a leg-length discrepancy; 1 patient had a 2.2-cm (10-year-old male) discrepancy, and 1 patient had a 1.2-cm (14-year-old female) discrepancy, with both patients having growth acceleration on the ACL-reconstructed limb. With regard to angular deformities, no patients had a statistically significant difference when compared with the contralateral limb (P < .05) after analysis (Table 1).
TABLE 1.
Measurements of Angular Deformitya
| Age, y | Mechanical Lateral Distal Femoral Angle, deg | Medial Proximal Tibial Angle, deg | Mechanical Axis Deviation, mm | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Patient | Sex | Chronological | Bone | Surgical | Nonsurgical | Surgical | Nonsurgical | Surgical | Nonsurgical |
| 1 | M | 9.7 | — | 85 | 86 | 86 | 86 | 0 | –1 |
| 2b | M | 10.3 | 12.0 | 86 | 87 | 87 | 89 | 2 | 2 |
| 3 | M | 11.1 | — | 88 | 90 | 90 | 87 | 1 | –1 |
| 4 | M | 12.0 | 12.5 | 86 | 88 | 89 | 87 | 1 | –1 |
| 5 | F | 12.2 | 13.5 | 83 | 85 | 88 | 86 | 1 | 1 |
| 6 | M | 12.3 | 12.5 | 85 | 87 | 87 | 88 | 0 | 1 |
| 7 | M | 12.3 | — | 88 | 87 | 87 | 89 | 1 | 0 |
| 8 | F | 12.3 | 12.0 | 85 | 85 | 80 | 83 | –1 | –1 |
| 9 | M | 12.4 | 13.0 | 81 | 86 | 87 | 84 | 2 | –1 |
| 10 | M | 12.8 | 12.5 | 83 | 84 | 88 | 88 | 1 | 2 |
| 11 | M | 13.1 | 14.0 | 85 | 87 | 90 | 85 | 1 | –2 |
| 12 | M | 13.2 | 15.0 | 88 | 87 | 89 | 89 | 0 | 1 |
| 13 | M | 13.3 | 14.0 | 86 | 86 | 82 | 84 | –2 | –1 |
| 14 | M | 13.5 | 13.0 | 93 | 92 | 94 | 92 | 2 | 4 |
| 15 | M | 13.5 | 14.0 | 85 | 86 | 84 | 85 | –1 | –1 |
| 16 | F | 13.7 | 15.0 | 88 | 87 | 88 | 88 | 0 | 0 |
| 17 | F | 14.1 | — | 85 | 86 | 83 | 83 | –1 | –1 |
| 18c | M | 14.4 | 14.0 | 86 | 83 | 88 | 86 | 10 | 10 |
| 19 | M | 14.4 | 15.0 | 84 | 86 | 79 | 80 | –2 | –3 |
| 20 | M | 14.6 | 12.5 | 83 | 83 | 87 | 84 | 2 | 0 |
| 21d | F | 14.7 | — | 87 | 87 | 89 | 94 | 1 | 2 |
| 22 | M | 14.8 | 16.0 | 86 | 87 | 88 | 89 | 1 | 1 |
| 23 | F | 15.0 | 13.0 | 87 | 88 | 87 | 87 | 0 | 1 |
| Median | 86 | 87 | 87 | 87 | 1 | 0 | |||
| Range | 81 to 93 | 83 to 92 | 79 to 94 | 80 to 94 | –2 to 10 | –3 to 10 | |||
| P value | .177 | .562 | .453 | ||||||
aNegative values denote varus positioning. F, female; M, male.
bPatient had a 2.2-cm leg-length difference (operative > nonoperative).
cPatient demonstrated bilateral physiological valgus.
dPatient had a 1.2-cm leg-length difference (operative > nonoperative).
The patient with a leg-length discrepancy of 2.2 cm was identified as having an overgrowth of both the femur and tibia of the operative leg, requiring operative intervention with pangenicular temporary epiphysiodesis. The other patient developed a leg-length discrepancy of 1.2 cm that was also an overgrowth of both the femur and tibia of the operative leg and is being observed at this time.
In addition to the patient treated with epiphysiodesis, 4 patients underwent subsequent surgical procedures after their hybrid physeal-sparing ACLR surgery. These findings are summarized in Table 2.
TABLE 2.
Subsequent Surgery After Hybrid Physeal-Sparing ACL Reconstructiona
| Patient | Second Surgery | Time From Hybrid Procedure, y | Age and Sex (During Second Surgery) |
|---|---|---|---|
| 2 | Ipsilateral epiphysiodesis | 4.0 | 14 y, male |
| 10 | Contralateral ACL reconstruction | 2.5 | 15 y, male |
| 15 | Ipsilateral medical meniscus repair | 1.5 | 14 y, male |
| 16 | Contralateral ACL reconstruction | 3.0 | 16 y, female |
| 21 | Contralateral ACL reconstruction | 2.0 | 16 y, female |
aACL, anterior cruciate ligament.
Subjective Outcomes and Return to Play
Subjective outcomes were obtained at a mean of 19 months (range, 6-57 months) after surgery. Overall, patients demonstrated favorable outcomes on both the Pedi-IKDC, with a mean score of 96.0 ± 3.5 (range, 89.1-100.0), and the ACL-RSI, with a mean score of 89.1 ± 12.9 (range, 53.0-100.0). Return-to-play data were available for 19 patients, of which the mean clearance to resume unrestricted athletics occurred 8 months (range, 6-14 months) after surgery.
Discussion
Controversy remains with respect to the appropriate operative treatment of ACL injuries in skeletally immature patients. Despite the development of several different techniques, discussion continues as to which method poses the least risk to the patient while providing optimal outcomes. The results of this study suggest that the hybrid physeal-sparing technique, during early follow-up, allows for anatomic reconstruction while minimizing the risk of growth disturbances in skeletally immature patients. This technique also produces satisfactory subjective outcomes in the majority of young patients and allows them to return to an active lifestyle.
While the highest rates of ACL injuries occur in patients between the ages of 15 to 17 years, the next highest rate occurs in athletes between 12 and 14 years of age.37 These patients are at particularly higher risk of growth disturbances, as they typically have 2 to 3 years or more of growth remaining. Based on their review of the literature, Kocher et al21 have recommended physeal-sparing ACLR in this age group. Several series have shown that transphyseal ACLR using soft tissue grafts, usually a hamstring autograft, in postpubescent adolescents is safe with no angular deformities or leg-length discrepancies.6,24,36 These authors, however, realizing the need to respect the open physes, often recommend modifications of the adult transphyseal reconstruction technique. One of those modifications is the drilling of vertically oriented tunnels to reduce the risk of both leg-length discrepancies and angular deformities. Unfortunately, these modified tunnel orientations typically create a more vertical femoral tunnel that is nonanatomic.
Regarding the use of an anatomic femoral tunnel in this population, independent drilling through a low anteromedial portal creates an oblique femoral tunnel through the distal femoral physis. This oblique angle increases the risk of physeal injuries and possibly injuries to the perichondral ring.1,40 A recent study by Cruz et al10 found increased physeal disruption when independent tunnel drilling was employed compared with a transtibial technique in skeletally immature patients. Additionally, despite its history of good to excellent results, more recent data have called into question the safety of transphyseal drilling for patients 2 to 3 years away from achieving skeletal maturity. In a recent study by Fauno et al,15 24% of patients who underwent transphyseal ACLR experienced either a compensated growth disturbance or leg-length discrepancy of ≥10 mm. Several other studies and reviews have reported premature physeal closure, angular deformities, and leg-length discrepancies with transphyseal ACLR.9,34,45 Transphyseal drilling has demonstrated a substantial risk to the physis in several animal studies as well, causing both leg-length discrepancies and angular deformities.18,39 Some authors have suggested that an anatomic physeal-sparing technique may not offer a significant advantage over a transphyseal approach with respect to avoiding growth disturbances. One systematic review found no statistical difference in the incidence of leg-length discrepancies and angular deformities when comparing a transphyseal and physeal-sparing cohort.34 A separate review found that in 4 reported cases of tibial angular deformities, a physeal-sparing technique was used in all 4 cases.9 Other concerns regarding physeal-sparing techniques have been raised as well. A recent magnetic resonance imaging study of the epiphyseal space available in the tibia has revealed that the “safe” area available may only be 19 to 21 mm.11 This poses a significant challenge to the surgeon to create an all-epiphyseal tunnel that will be of adequate length while avoiding oblique drilling of the physis. Similar difficulties have not been described in the literature for drilling of an all-epiphyseal femoral tunnel.
Several nonanatomic techniques have also been described that are excellent options for treating prepubescent athletes with ACL injuries. Kocher et al21 have described a nonanatomic, combined intra-articular, extra-articular technique that has displayed satisfactory results in patients with a mean age of 10.3 years. This technique produced good results with a low revision rate. Similarly, the Anderson4 and Lawrence et al26 all-epiphyseal techniques are outstanding options for athletes of this age group with ACL-deficient knees. While these procedures have uniformly produced good to excellent results with a low revision rate, their utility in patients 2 to 3 years from skeletal maturity has not been described.
When considering the available data on the risk of growth disturbances in ACLR of the skeletally immature patient, our approach is to preserve the femoral physis while drilling a vertically oriented transphyseal tibial tunnel. This technique will ideally avoid any damage to the femoral physis while minimizing the risk of injuries to the tibial physis and ultimately the consequence of a growth disturbance. This technique will also provide reconstruction using the anatomic footprints of the native ACL. While not identical to our technique, other forms of the “hybrid” technique for ACLR have been published previously. Lipscomb and Anderson28 reported on 24 skeletally immature patients with a mean age of 13 years who underwent hybrid ACLR using a hamstring autograft similar to our technique but with the addition of extra-articular reconstruction. Only 1 patient had a leg-length discrepancy, and 83% of all athletes returned to play (including the athlete who underwent epiphysiodesis). Another study of 8 patients with a mean age of 13.5 years who had undergone reconstruction with a fascia lata or Achilles allograft with an “over-the-top” femoral fixation device had 87.5% good to excellent results with no occurrence of growth disturbances at a mean follow-up of 58 months.5 A separate report of 5 patients was also published by Lo et al29 in patients with a mean age of 12.9 years who were treated with a hybrid reconstruction technique with “over-the-top” femoral placement of a soft tissue autograft and transtibial drilling. There were no cases of a leg-length discrepancy at a mean follow-up of 7.4 years.
As of 2016, there were 39 pediatric patients reported who developed a growth disturbance after ACLR.9 The rates of growth disturbances that have been described range from 0% to 24% depending on the technique used.13,15,20,21,45 In our review of 23 patients with a minimum of 1-year follow-up, the hybrid physeal-sparing technique resulted in 2 cases of growth disturbance, or an 8.3% rate. This growth disturbance was an acceleration of femoral and tibial growth that was ultimately correctable with an additional surgical procedure. There were no documented cases of statistically significant angular deformities.
This study has several strengths. This is a unique description of a hybrid femoral physeal-sparing technique for ACLR in skeletally immature athletes. The satisfactory results at initial follow-up provide surgeons with a viable option for treating adolescent patients with 2 to 3 years of growth remaining. This study also addresses return to play as it pertains to patients who underwent ACLR using the hybrid femoral physeal-sparing technique. This will aid clinicians in counseling patients regarding postoperative expectations about future athletic endeavors. This study also highlights the importance of close radiographic monitoring of skeletally immature patients in the postoperative period after ACLR. Regardless of the technique, a growth disturbance may occur, and early intervention is key for treating a patient with an iatrogenic leg-length discrepancy or angular deformity. It is suggested that patients be observed clinically and radiographically until skeletal maturity to assess for any potential growth abnormality including a leg-length discrepancy or angular deformity. The sooner any potential growth issue is identified, the sooner potential growth modulation treatment options can be provided if the growth abnormality is felt to be potentially clinically significant.
This study is not without its limitations. Objective clinical data, including range of motion and stability, were not available for all patients included in the study. Preoperative mechanical axis films were not routinely collected on all patients; therefore, the true leg length and limb alignment before surgical intervention are not known for this cohort. All patients obtained their mechanical axis films using the same radiographic protocol at the physicians’ office; however, we were unable to control for the possibility that patients may have had their knees in varying degrees of flexion while taking the radiograph. This may have resulted in an apparent valgus presentation on the mechanical axis films. Finally, the mean radiographic follow-up for this small cohort was 21 months after surgery. Additional long-term follow-up is needed for a comprehensive understanding of the benefits as well as limitations of this technique.
Conclusion
The femoral physeal-sparing with transphyseal tibial drilling “hybrid” technique in skeletally immature athletes appears to have a high rate of success with low morbidity. When compared with existing options for ACLR in patients with open physes, this method poses a minimal risk of growth disturbances while also providing high subjective knee scores and the ability to successfully return to an active athletic lifestyle. Although it is a viable option, the possibility of physeal abnormalities does exist, which demonstrates the importance of a close postoperative follow-up and evaluation until skeletal maturity is achieved in this at-risk patient population.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: M.D.M. has received grant funding from the Pediatric Orthopaedic Society of North America, has received publishing royalties from Elsevier Inc, and receives research support from Vericel Corp and AlloSource Inc as a member of the Research in OsteoChondritis of the Knee (ROCK) group. C.W.N. has received unrestricted educational grants as a member of the ROCK group from Vericel Corp and AlloSource Inc.
Ethical approval for this study was obtained from the Connecticut Children’s Medical Center (No. 14-109).
References
- 1. Abebe ES, Moorman CT, 3rd, Dziedzic TS, et al. Femoral tunnel placement during anterior cruciate ligament reconstruction: an in vivo imaging analysis comparing transtibial and 2-incision tibial tunnel-independent techniques. Am J Sports Med. 2009;37(10):1904–1911. [DOI] [PubMed] [Google Scholar]
- 2. Aichroth PM, Patel DV, Zorrilla P. The natural history and treatment of rupture of the anterior cruciate ligament in children and adolescents: a prospective review. J Bone Joint Surg Br. 2002;84(1):38–41. [DOI] [PubMed] [Google Scholar]
- 3. Al-Hadithy N, Dodds AL, Akhtar KS, Gupte CM. Current concepts of the management of anterior cruciate ligament injuries in children. Bone Joint J. 2013;95-B(11):1562–1569. [DOI] [PubMed] [Google Scholar]
- 4. Anderson AF. Transepiphyseal replacement of the anterior cruciate ligament in skeletally immature patients: a preliminary report. J Bone Joint Surg Am. 2003;85-A(7):1255–1263. [DOI] [PubMed] [Google Scholar]
- 5. Andrews M, Noyes FR, Barber-Westin SD. Anterior cruciate ligament allograft reconstruction in the skeletally immature athlete. Am J Sports Med. 1994;22(1):48–54. [DOI] [PubMed] [Google Scholar]
- 6. Aronowitz ER, Ganley TJ, Goode JR, Gregg JR, Meyer JS. Anterior cruciate ligament reconstruction in adolescents with open physes. Am J Sports Med. 2000;28(2):168–175. [DOI] [PubMed] [Google Scholar]
- 7. Buckley SL, Barrack RL, Alexander AH. The natural history of conservatively treated partial anterior cruciate ligament tears. Am J Sports Med. 1989;17(2):221–225. [DOI] [PubMed] [Google Scholar]
- 8. Cassard X, Cavaignac E, Maubisson L, Bowen M. Anterior cruciate ligament reconstruction in children with a quadrupled semitendinosus graft: preliminary results with minimum 2 years of follow-up. J Pediatr Orthop. 2014;34(1):70–77. [DOI] [PubMed] [Google Scholar]
- 9. Collins MJ, Arns TA, Leroux T, et al. Growth abnormalities following anterior cruciate ligament reconstruction in the skeletally immature patient: a systematic review. Arthroscopy. 2016;32(8):1714–1723. [DOI] [PubMed] [Google Scholar]
- 10. Cruz AI, Jr, Lakomkin N, Fabricant PD, Lawrence JT. Transphyseal ACL reconstruction in skeletally immature patients: does independent femoral tunnel drilling place the physis at greater risk compared with transtibial drilling? Orthop J Sports Med. 2016;4(6):23259 67116650432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Davis DL, Almardawi R, Mitchell JW. Analysis of the tibial epiphysis in the skeletally immature knee using magnetic resonance imaging: an update of anatomic parameters pertinent to physeal-sparing anterior cruciate ligament reconstruction. Orthop J Sports Med. 2016;4(6):23259 67116655313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dodwell ER, Lamont LE, Green DW, Pan TJ, Marx RG, Lyman S. 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med. 2014;42(3):675–680. [DOI] [PubMed] [Google Scholar]
- 13. Domzalski M, Karauda A, Grzegorzewski A, Lebiedzinski R, Zabierek S, Synder M. Anterior cruciate ligament reconstruction using the transphyseal technique in prepubescent athletes: midterm, prospective evaluation of results. Arthroscopy. 2016;32(6):1141–1146. [DOI] [PubMed] [Google Scholar]
- 14. Fabricant PD, Kocher MS. Anterior cruciate ligament injuries in children and adolescents. Orthop Clin North Am. 2016;47(4):777–788. [DOI] [PubMed] [Google Scholar]
- 15. Fauno P, Romer L, Nielsen T, Lind M. The risk of transphyseal drilling in skeletally immature patients with anterior cruciate ligament injury. Orthop J Sports Med. 2016;4(9):2325967116664685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gausden EB, Calcei JG, Fabricant PD, Green DW. Surgical options for anterior cruciate ligament reconstruction in the young child. Curr Opin Pediatr. 2015;27(1):82–91. [DOI] [PubMed] [Google Scholar]
- 17. Graf BK, Lange RH, Fujisaki CK, Landry GL, Saluja RK. Anterior cruciate ligament tears in skeletally immature patients: meniscal pathology at presentation and after attempted conservative treatment. Arthroscopy. 1992;8(2):229–233. [DOI] [PubMed] [Google Scholar]
- 18. Guzzanti V, Falciglia F, Gigante A, Fabbriciani C. The effect of intra-articular ACL reconstruction on the growth plates of rabbits. J Bone Joint Surg Br. 1994;76(6):960–963. [PubMed] [Google Scholar]
- 19. Henry J, Chotel F, Chouteau J, Fessy MH, Berard J, Moyen B. Rupture of the anterior cruciate ligament in children: early reconstruction with open physes or delayed reconstruction to skeletal maturity? Knee Surg Sports Traumatol Arthrosc. 2009;17(7):748–755. [DOI] [PubMed] [Google Scholar]
- 20. Koch PP, Fucentese SF, Blatter SC. Complications after epiphyseal reconstruction of the anterior cruciate ligament in prepubescent children. Knee Surg Sports Traumatol Arthrosc. 2016;24(9):2736–2740. [DOI] [PubMed] [Google Scholar]
- 21. Kocher MS, Garg S, Micheli LJ. Physeal sparing reconstruction of the anterior cruciate ligament in skeletally immature prepubescent children and adolescents: surgical technique. J Bone Joint Surg Am. 2006;88(pt 2, suppl 1):283–293. [DOI] [PubMed] [Google Scholar]
- 22. Kocher MS, Saxon HS, Hovis WD, Hawkins RJ. Management and complications of anterior cruciate ligament injuries in skeletally immature patients: survey of the Herodicus Society and The ACL Study Group. J Pediatr Orthop. 2002;22(4):452–457. [PubMed] [Google Scholar]
- 23. Kocher MS, Smith JT, Iversen MD, et al. Reliability, validity, and responsiveness of a modified International Knee Documentation Committee Subjective Knee Form (Pedi-IKDC) in children with knee disorders. Am J Sports Med. 2011;39(5):933–939. [DOI] [PubMed] [Google Scholar]
- 24. Kocher MS, Smith JT, Zoric BJ, Lee B, Micheli LJ. Transphyseal anterior cruciate ligament reconstruction in skeletally immature pubescent adolescents. J Bone Joint Surg Am. 2007;89(12):2632–2639. [DOI] [PubMed] [Google Scholar]
- 25. Lawrence JT, Argawal N, Ganley TJ. Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: is there harm in delay of treatment? Am J Sports Med. 2011;39(12):2582–2587. [DOI] [PubMed] [Google Scholar]
- 26. Lawrence JT, Bowers AL, Belding J, Cody SR, Ganley TJ. All-epiphyseal anterior cruciate ligament reconstruction in skeletally immature patients. Clin Orthop Relat Res. 2010;468(7):1971–1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lind M, Menhert F, Pedersen AB. The first results from the Danish ACL reconstruction registry: epidemiologic and 2 year follow-up results from 5,818 knee ligament reconstructions. Knee Surg Sports Traumatol Arthrosc. 2009;17(2):117–124. [DOI] [PubMed] [Google Scholar]
- 28. Lipscomb AB, Anderson AF. Tears of the anterior cruciate ligament in adolescents. J Bone Joint Surg Am. 1986;68(1):19–28. [PubMed] [Google Scholar]
- 29. Lo IK, Kirkley A, Fowler PJ, Miniaci A. The outcome of operatively treated anterior cruciate ligament disruptions in the skeletally immature child. Arthroscopy. 1997;13(5):627–634. [DOI] [PubMed] [Google Scholar]
- 30. McCarroll JR, Rettig AC, Shelbourne KD. Anterior cruciate ligament injuries in the young athlete with open physes. Am J Sports Med. 1988;16(1):44–47. [DOI] [PubMed] [Google Scholar]
- 31. McCarthy MM, Graziano J, Green DW, Cordasco FA. All-epiphyseal, all-inside anterior cruciate ligament reconstruction technique for skeletally immature patients. Arthrosc Tech. 2012;1(2):e231–e239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. McConkey MO, Bonasia DE, Amendola A. Pediatric anterior cruciate ligament reconstruction. Curr Rev Musculoskelet Med. 2011;4(2):37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Millett PJ, Willis AA, Warren RF. Associated injuries in pediatric and adolescent anterior cruciate ligament tears: does a delay in treatment increase the risk of meniscal tear? Arthroscopy. 2002;18(9):955–959. [DOI] [PubMed] [Google Scholar]
- 34. Pierce TP, Issa K, Festa A, Scillia AJ, McInerney VK. Pediatric anterior cruciate ligament reconstruction: a systematic review of transphyseal versus physeal-sparing techniques. Am J Sports Med. 2017;45(2):488–494. [DOI] [PubMed] [Google Scholar]
- 35. Ramski DE, Kanj WW, Franklin CC, Baldwin KD, Ganley TJ. Anterior cruciate ligament tears in children and adolescents: a meta-analysis of nonoperative versus operative treatment. Am J Sports Med. 2014;42(11):2769–2776. [DOI] [PubMed] [Google Scholar]
- 36. Sankar WN, Carrigan RB, Gregg JR, Ganley TJ. Anterior cruciate ligament reconstruction in adolescents: a survivorship analysis. Am J Orthop (Belle Mead NJ). 2008;37(1):47–49. [PubMed] [Google Scholar]
- 37. Shea KG, Pfeiffer R, Wang JH, Curtin M, Apel PJ. Anterior cruciate ligament injury in pediatric and adolescent soccer players: an analysis of insurance data. J Pediatr Orthop. 2004;24(6):623–628. [DOI] [PubMed] [Google Scholar]
- 38. Smith TO, Davies L, Hing CB. Early versus delayed surgery for anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2010;18(3):304–311. [DOI] [PubMed] [Google Scholar]
- 39. Stadelmaier DM, Arnoczky SP, Dodds J, Ross H. The effect of drilling and soft tissue grafting across open growth plates: a histologic study. Am J Sports Med. 1995;23(4):431–435. [DOI] [PubMed] [Google Scholar]
- 40. Tompkins M, Milewski MD, Brockmeier SF, Gaskin CM, Hart JM, Miller MD. Anatomic femoral tunnel drilling in anterior cruciate ligament reconstruction: use of an accessory medial portal versus traditional transtibial drilling. Am J Sports Med. 2012;40(6):1313–1321. [DOI] [PubMed] [Google Scholar]
- 41. Vavken P, Murray MM. Treating anterior cruciate ligament tears in skeletally immature patients. Arthroscopy. 2011;27(5):704–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Vavken P, Tepolt FA, Kocher MS. Concurrent meniscal and chondral injuries in pediatric and adolescent patients undergoing ACL reconstruction. J Pediatr Orthop. 2018;38(2):105–109. [DOI] [PubMed] [Google Scholar]
- 43. Webster KE, Feller JA, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport. 2008;9(1):9–15. [DOI] [PubMed] [Google Scholar]
- 44. Werner BC, Yang S, Looney AM, Gwathmey FW., Jr Trends in pediatric and adolescent anterior cruciate ligament injury and reconstruction. J Pediatr Orthop. 2016;36(5):447–452. [DOI] [PubMed] [Google Scholar]
- 45. Yoo WJ, Kocher MS, Micheli LJ. Growth plate disturbance after transphyseal reconstruction of the anterior cruciate ligament in skeletally immature adolescent patients: an MR imaging study. J Pediatr Orthop. 2011;31(6):691–696. [DOI] [PubMed] [Google Scholar]


