Abstract
Background
Sleep problems are common but often neglected in older adults, particularly in the context of cancer. Underlying mechanisms are poorly understood and interventions frequently lack a clear scientific basis.
Objective
The objective of this report was to examine scientific content presented at an NIH-sponsored, U13 “Bedside to Bench” conference using a qualitative and iterative review procedure. Analysis of current scientific issues regarding sleep in older adults with cancer is needed to direct nurse scientists and clinicians toward research opportunities.
Methods
A multistep review procedure for the analysis/synthesis of knowledge gaps and research opportunities was undertaken by oncology nurse scientists in attendance.
Results
Conceptual problems in this area include the lack of standard sleep terminology and absence of an overarching conceptual model. Methodological problems are inconsistent sleep/napping measurement and complex operational challenges in designing comprehensive yet feasible studies in older adults. Knowledge gaps in basic and clinical science relate to cellular and molecular mechanisms that underlie sleep and circadian rhythm disturbances, contribution of sleep to adverse outcomes, and impact of disturbed sleep during hospitalization and the transition from hospital to home.
Conclusions
Focused and interdisciplinary research that advances conceptual and operational understanding of biological and behavioral determinants of sleep health in the aging cancer population can lead to more effective, safe, and targeted interventions for those with cancer-related sleep-circadian disturbances.
Problem and Significance
Sleep disturbance is increasingly being recognized as a geriatric syndrome. Geriatric syndromes refer to common health conditions in older adults that do not fall into discrete disease categories (eg, delirium, frailty).1 Aging and sleep are both complex phenomena requiring multidisciplinary approaches to research and treatment.2 Older adults are a high risk for the coexistence of multiple chronic diseases.3 Competing medical priorities contribute to suboptimal diagnosis and treatment of sleep problems in older adults. Underlying mechanisms are poorly understood and sleep interventions have not been systematically tested in older adults. Disruptions in sleep and circadian rhythms lead to many adverse health outcomes; in turn, common diseases of older adults cause sleep disturbances.
To address knowledge gaps and research opportunities, the National Institute on Aging (NIA) and the American Geriatrics Society (AGS) co-sponsored a U13 Conference Series, entitled Sleep, Circadian Rhythms, and Aging: New Avenues for Improving Brain Health, Physical Health, and Functioning (George Kuchel, PI) on October 4–6, 2015, with additional support provided by unrestricted educational grants from the American Academy of Sleep Medicine, Pfizer, and Philips-Respironics. The specific aims of the conference were to focus attention on high-quality research in the area of geriatric sleep and to facilitate the development of a cadre of diverse and productive geriatric sleep researchers. Identified knowledge gaps and research opportunities would then be disseminated to geriatric and other high-impact specialties.
The conference planning committee, speakers, moderators, and participants represented a wide range of basic and translational sleep researchers from diverse disciplines, such as nursing, medicine, neuroscience, epidemiology, and geriatrics. Conference participants were selected through a competitive application process. Over the 3-day period, sleep and aging experts shared state-of-the-art research related to brain health, physical health, and functioning specific to aging, sleep, and circadian rhythms. Conference planners incorporated time to network, seek consultation from sleep and aging groups, and form writing groups. The authors of this report, oncology nurse scientists with backgrounds in sleep research, were selected to attend this bench-to-bedside conference. These nurse scientists formed a writing group to synthesize information from the conference into this current report for the benefit of researchers and clinicians in the oncology, nursing, and sleep medicine communities. Although the conference was directed primarily toward research, the eventual translation of effective sleep interventions into clinical practice will require substantial input from clinicians; thus, early integration of research and clinical practice is paramount. This report provides a brief overview of the problems related to sleep along with a synthesis of the knowledge gaps and research opportunities identified in conference presentations, particularly gaps and opportunities that are relevant to older adults with cancer.
Sleep in Older Adults
Advancing age is associated with sleep pattern changes and is superimposed on cancer treatments and psychosocial co-morbidities that add to sleep difficulties and disability4. Poor sleep is linked to depression, pain, dementia, sleep-disordered breathing, and other common geriatric problems, including bidirectional relationships with urinary incontinence and delirium5. Most cancers are inherently diseases of older adults, and understanding the unique contribution of aging to poor sleep in those with cancer and their caregivers is a unique opportunity for nurse scientists and clinicians specializing in oncology and gerontology.
Although impaired sleep is a public health issue, healthcare providers have been slow to acknowledge the substantial negative impact of poor sleep in the general population, much less older adults6. Similarly, sleep researchers have only recently begun to examine sleep-circadian characteristics, disorders, and pathophysiology in older adults. In light of recent advances in sleep and circadian biology, questions arise such as: 1) What is normal sleep in the aging adult and how might this apply to sleep-circadian health in older cancer survivors?, 2) can sleep interventions improve physical and cognitive functioning during cancer treatment?, 3) what are the major barriers and opportunities for sleep research?, and 4) what high priority, geriatric research problems need to be addressed in the next 5 years to advance sleep research? These questions are consistent with the pre-conference priorities identified by conference attendees (Table 1). Our objective was to consider these questions in light of the scientific content presented at an NIH-sponsored, U13 “Bedside to Bench” conference using a qualitative and iterative review procedure.
Table 1.
Pre-conference Sleep and Aging Research Priorities
| Pre-conference Priorities |
|---|
| 1. What are the mechanisms by which sleep affects normal aging, are they reversible, and, if so, when? |
| 2. What are the mechanisms by which sleep effects diseases typically co-morbid with aging, are they reversible and if so when? |
| 3. What is “normal” sleep across the older adult life span? |
| 4. Does the “need” to sleep change with age? |
| 5. Is the impact of habitual sleep duration on health a function of age? |
| 6. Do the mechanisms by which sleep disorders impact health vary by age? |
| 7. What are the best methods to improve sleep, do they also improve other measures of health, and what are the healthcare utilization and cost savings? |
| 8. What are the roles of sleep, hypnotics, nocturia, delirium, and institutionalization relative to function, falls, and cognitive impairment, and what are the implications for prevention? What are the healthcare utilization and cost savings? Are any of the above modified by sex, race, ethnicity, or socioeconomic status? |
Methods
Synthesis of Conference Information
To integrate the conference highlights from the perspectives of sleep and aging with cancer, our writing group developed a multistep, iterative review procedure for the initial analysis and subsequent synthesis of the conference content. Members of the group developed the review procedure, discussed themes and patterns, and reached consensus during six months of regularly scheduled 1-hour teleconferences (approximately 2 per month). First, we independently reviewed all conference slides publicly available on the AGS website,7 focusing on the knowledge gaps and research opportunities outlined by each speaker. The “sample” consisted of the 23 conference presentations with scientific content. Three brief presentations with general information about the conference were excluded due to lack of research-related subject matter. Table 2 outlines the conference topics and speakers that were included in the sample. Three main types of scientific issues emerged from our independent review of the conference slides during our initial discussions: 1) conceptual, 2) methodological, and 3) physiological. Because of the broad nature of the proposed physiological questions, this category was further subdivided into issues in basic or clinical (applied) science. For the purpose of this report, basic science refers to research done in a laboratory focused on understanding mechanisms (eg, cellular, genetic) that underlie diseases; clinical science is research using humans to evaluate biomedical or health-related outcomes.8 Next, we assigned each knowledge gap and research opportunity in the conference slides to one type of issue (conceptual, methodological, basic or clinical research; Figure). Lastly, we reached consensus through 10 1-hour group discussions about important and relevant gaps and opportunities in the context of cancer. It is within these categories (conceptual, methodological, and physiological) that we describe the knowledge gaps and set an agenda for research opportunities in sleep and aging that are germane to oncology practice and research.
Table 2.
U13 Presentation Topics (Speakers)
| Presentation Topics (Speakers) | |
|---|---|
| 1. | Aging, Blood Pressure, and Cardiovascular Disease Event Risk (Michael Smolensky) |
| 2. | Assessing Functional Status and Quality of Life in Older Adults (Cathy Alessi) |
| 3. | Chronic Sleep Loss and Neuro-degeneration (Sigrid Veasey) |
| 4. | Glymphatic System, Sleep & other states of unconsciousness (Helene Benveniste) |
| 5. | Insomnia and aging: Risks for brain health and new treatment approaches (Daniel Buysse) |
| 6. | Insufficient Sleep and CNS Inflammation (Mark Opp) |
| 7. | Long Sleep Duration is Associated with an Increased Risk for Adverse Outcomes in Older |
| 8. | Adults (R. Nisha Aurora) |
| 9. | Sleep and Chronic Pain (Michael Smith) |
| 10. | Sleep and Circadian Rhythms in Neurodegenerative Disorders (Erik Musiek) |
| 11. | Sleep and Falls (Katie Stone) |
| 12. | Sleep and Hospitalization: Effect on Outcomes (Vineet Arora) |
| 13. | Sleep Apnea in Older Adults (Barbara Phillips) |
| 14. | Sleep Disturbance as a Geriatric Syndrome (Cathy Alessi) |
| 15. | Sleep Duration is NOT a risk factor for increased mortality in the elderly (Daniel O’Hearn) |
| 16. | Sleep, Circadian Rhythms and Aging: New Avenues for Improving Brain Health, Physical |
| 17. | Sleep, Circadian Rhythms and Metabolism (Kenneth Wright) |
| 18. | Sleep, Circadian Rhythms, and Aging: New Avenues for Improving Brain Health, Physical |
| 19. | Health and Functioning. (Kathy Richardson) |
| 20. | Sleep, Circadian Rhythms, and Aging: Translational Perspective (Phyllis Zee) |
| 21. | Sleep, Circadian Rhythms, Cognitive Function (Rebecca Spencer) |
| 22. | Sleepiness, Napping, and Health Risk in the Elderly (Anne Newman) |
| 23. | Treating Sleep as a Geriatric Syndrome: Nocturia (Donald Bliwise) |
American Geriatric Society
National Institute on Aging
Conference overview/goals rather than sleep content.
Figure.
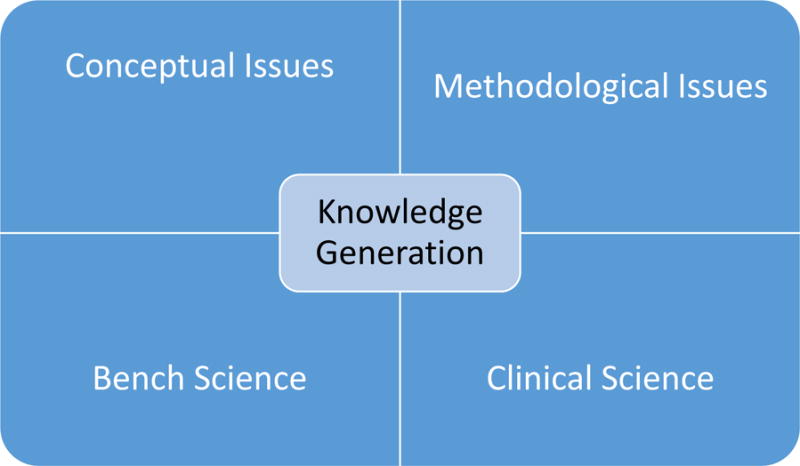
Model of Research Opportunities in Older Adults with Sleep Disorders and Cancer
Results
Conceptual Issues
Conference presenters outlined several conceptual issues surrounding sleep in the aging population. Three main knowledge gaps emerged: 1) lack of standard definitions of key words to describe the complexity of insufficient sleep in older adults, 2) poor delineation of the relationships among the complex variables related to insufficient or poor quality sleep, and 3) absence of a comprehensive conceptual model for sleep.
Lack of Standard Terminology
A major contributing factor to knowledge gaps is the absence of clear and consistent terminology, which is especially problematic in the cancer literature.9 A recent review of cancer studies found that at least 36 different terms were used interchangeably as primary or secondary descriptors of sleep (eg, sleep duration, efficacy, insomnia). It is reasonable to use different terms for distinct aspects of sleep (eg, sleep duration, sleep efficiency); however, accepted formal classification systems that use common terms, such as DSM-IV or ICSD-3, are available but used inconsistently. Terminology gaps noted by conference presenters included an overarching lack of clear definitions for common sleep conditions in aging, such as a clear clinical definition of obstructive sleep apnea in older populations. It is also unclear if definitions for sleep conditions in the aging population translate to other chronic comorbid conditions and are the same across the aging trajectory. Specific recommendations from conference presenters included defining sleep using consistent language across the aging trajectory, clear recommendations on diagnostic terminology to describe sleep in research and practice, and defining adequate sleep duration through clear and consistent measurements. Although these messages were presented in the scope of the aging population, it is also pertinent to clarify these definitions within the scope of the cancer population. Providing clarity can lead to a better conceptual model of these variables and help redefine effective interventions for practice.
Unclear Delineation of the Relationships
Challenges with creating an accepted model or framework include the complexity of sleep, bidirectional relationships between predictive or contributing factors and outcomes, and unclear mediator/moderator relationships. Unclear relationships span all aspects of the sleep-wake cycle (eg, impact of napping on nighttime sleep) and related health outcomes. There are research opportunities within cancer to map a well-defined conceptual model that would lead to a better understanding of the directional and bi-directional influences of factors related to insufficient sleep and to negative physiological, psychological, and behavioral health outcomes. Specifically, cancer researchers have the opportunity to delineate the concepts of sleepiness, fatigue, tiredness, fatigability, and impact of napping through testing their interrelationships and determining their respective impacts on nighttime sleep. In addition, current models need to include the relationships between and impact of metabolic disorders relative to circadian rhythms.
Absence of an Overarching Conceptual Model
Sleep research in general lacks conceptual congruency across the many disciplines that study sleep. There currently is no mutually agreed-upon, overarching conceptual framework or model to guide the many disciplines involved in sleep research, such as geriatrics, neurology, pulmonology, nursing, and psychology. In the cancer literature, several models are used to describe factors related to insufficient sleep, suggesting conceptual incongruity.10 In addition, the sleep models and frameworks cited in the cancer literature have ranged from mathematical models to symptom management models, with little to no consistency across studies.10 This lack of a consistent conceptual model creates particular difficulty when trying to compare research findings across sleep studies involving people with cancer or when trying to link theory with research and clinical practice. Seminal reviews in the cancer nursing literature have delineated many of these conceptual issues and made recommendations for conceptual clarity through using diagnostic terminology in research.11–13 However, the cancer literature does not indicate that these recommendations have been translated, posing the challenge of better translating knowledge of how to diagnose and treat sleep issues during the cancer trajectory into practice. Despite recommendations to improve conceptual clarity, inconsistencies and conceptual overlap persist in the cancer literature. Important next steps should focus on developing a comprehensive biobehavioral model of sleep. Nurse scientists with expertise in sleep are well-positioned to lead this work. A comprehensive model would require the careful integration of current evidence with extant models of sleep, aging, and disease management. Essential components may include physiological and behavioral sleep factors, consequences of impaired sleep over the lifespan, and potential interventions including timing and dosage.
Methodological issues
Methodological issues associated with sleep research in older patients described at the conference fall into three broad categories: 1) measurement of sleep and napping; 2) expanding the breadth and depth of sleep research; and 3) the complexity of operationally defining relationships among sleep and other biopsychosocial variables (Table 3). Although discussing all of the methodological and measurement considerations is beyond the scope of this paper, highlighting the main knowledge gaps and research opportunities helps to ensure that the most meaningful sleep research is conducted in the older cancer patients. Operationalizing sleep and/or sleep disturbances in older cancer patients is one of the most salient methodological decisions facing researchers in the area. Although much progress in sleep research has been made, questions persist regarding how to best assess sleep along with the frequency and duration of assessments under a wide range of research circumstances.
Table 3.
Conceptual, Methodological, Basic Science, and Clinical Science Issues
| Scientific Issues, Gaps and Opportunities | Examples |
|---|---|
| Conceptual | |
| Lack of standard definitions/descriptors of sleep concepts, “normal” sleep, and sleep disorders in aging adults | Use of generic sleep terms and inconsistent use of formal sleep disorder classification systems in practice and research Vague parameters of “adequate” sleep duration and sleep quality in older adults Lack of evidence to support the use of the same diagnostic criteria of sleep disorders (eg, sleep apnea) in older vs. younger adults |
| Absence of scientifically established commonalities and relationships among key sleep concepts, and influence of these factors on health and functioning | Conceptual overlap in sleepiness, fatigue, tiredness, fatigability; and insufficiently explained impact of daytime napping on these sleep-related variables Uncertain impact of nighttime sleep on daytime symptoms and functioning Complexity of sleep as a geriatric syndrome make it difficult to conceptualize underlying pathophysiologic mechanisms. |
| Inability of current conceptual models to capture the unique aspects of sleep in older adults, particularly in comorbid conditions | Traditional disease models fail to take into account the complexity of sleep disturbances across the lifespan. Bidirectional relationships between metabolic disorders and sleep/circadian rhythms are poorly delineated in older adults. |
| Methodological Issues | |
| Inadequate, standardized measurement of sleep and napping | Standardized interpretation and use of common sleep measures and technological advancements is needed. |
| Limited breadth and depth of sleep research | Individual, environmental, and treatment-related processes, such as multiple co-morbidities and age-related changes, need to be addressed. |
| Difficulty operationalizing complex relationships among sleep and other biopsychosocial variables | Lack of an integrated, interdisciplinary framework to guide and focus future research that captures relevant biopsychosocial variables |
| Basic Science | |
| Gaps in knowledge | Physiological degeneration of circadian systems and sleep circuitry Cellular and molecular basis of sleep loss/disruption and circadian dysregulation relative to cancer and brain health Underlying mechanism(s) of sleep/circadian disruption, fragmented sleep, and “sundowning” in older adults with and without acute and chronic illness (ie, cancer) |
| Interdisciplinary Research Opportunities | Develop animal models to study sleep/circadian dysregulation. Investigate perivascular neurons, gliovascular interactions, and intramural vascular signaling change in glymphatic pathway functioning in normal aging. Unravel the contribution of sleep/circadian dysregulation on other neurodegenerative pathways and neural function. Describe relationships of sleep loss/disturbance to metabolic dysregulation and inflammatory markers over the lifespan and in those with cancer. Identify and validate sleep-circadian biomarkers; understand how aging may modify their expression in health, disease, and age-related sleep disorders. |
| Clinical Science | |
| Gaps in knowledge | Uncertain contribution of sleep and circadian rhythm optimization to reducing the risk of cancer, modifying tumor activity, and preventing adverse outcomes Limited understanding of the clinical effects of sleep disorders, inadequate sleep duration/quality on relevant health outcomes in older adults with cancer (eg, brain health and physical functioning) Unknown influence of sleep disorders/deprivation on cancer or hospital-related common adverse events in older adults (eg, delirium, falls, infections) |
| Interdisciplinary Research Opportunities | Design high quality, disease-specific clinical trials to test interventions to improve sleep-circadian health as a target for disease prevention and disease modification. Test the feasibility and impact of routine screening/timely treatment of common sleep disorders in older hospitalized adults. Develop and implement programs to enhance the sleep environment and symptom management in the hospital and home for older adults with cancer. |
Measurement of Sleep and Napping
Cancer nurse researchers have used a variety of approaches to assess sleep in people with cancer, commonly including patient-completed questionnaires, sleep diaries, polysomnography (PSG), and wrist actigraphy. Patient-completed questionnaires and sleep diaries are relatively inexpensive and easy to implement in clinical research. The findings from these self-report instruments, however, may or may not be consistent with objective assessments of sleep. In-laboratory PSG, the gold standard for sleep assessment, provides the most comprehensive assessment of sleep and sleep problems via simultaneous monitoring of various body functions such as eye movements, skeletal muscle activation, and heart rhythm. Recent data suggest that unattended, portable home PSG may be an acceptable alternative to monitored, in-laboratory testing.14 Wrist actigraphy offers a reasonable alternative for objective assessment of sleep, particularly in clinical field studies that require multiple days of sleep data. Like PSG, this approach requires the use of specialized equipment and software. The associated costs may be lower than for PSG but are higher than subjective measures. Unlike PSG, the retrieved data from actigraphy does not include information from multiple body systems, and thus the assessment is not as comprehensive. Future research opportunities stem from knowledge gaps related to lack of standardization for measuring sleep. Technological advancements, such as home-based PSG, may improve the quantity and quality of the sleep data.
Expanding Sleep Research
Expanding the breadth and depth of sleep research in people with cancer is important for facilitating our understanding of this complex phenomenon and promoting sleep science. Many of the conference presenters envisioned sleep as a geriatric syndrome like frailty and delirium. Classifying sleep disturbances as a geriatric syndrome advances our knowledge of sleep as a multifactorial process. At the same time, this introduces complexity into conducting sleep research. In older people with cancer, sleep disturbances are associated with numerous individual, environmental, and treatment-related processes, such as multiple co-morbidities and age-related changes. The potential negative health outcomes associated with sleep disturbances, such as cognitive impairment, are complex and intertwined. The research implications for categorizing sleep disturbances as a geriatric syndrome, particularly in people with cancer, need to be further clarified. For example, what are the defining characteristics of sleep disturbances as a geriatric syndrome? From a methodological perspective, will classifying sleep disturbances as a geriatric syndrome require a wide range of biopsychosocial data to adequately measure the syndrome?
Complex Interactions among Sleep and Biopsychosocial Variables
The complexity of relationships among sleep and other biopsychosocial variables creates multiple avenues for future research and, at the same time, may lead to a perceived inability to capture all relevant data in any given research proposal. As noted in the conceptual section above, lack of an overarching framework across disciplines to guide sleep research complicates generation of discipline-specific and discipline-nonspecific knowledge related to sleep and associated biopsychosocial variables. The challenge for cancer nursing researchers examining sleep disturbances will be to avoid focusing the research too narrowly or broadly. Narrowly focused sleep studies limit relevance and generalizability. Conversely, studies that are too broad in scope result in diluted and less meaningful findings, particularly if an all-inclusive approach that approximates data mining is used.
Physiologic: Basic Science Issues
Although age-related sleep changes have been well-described, cellular and molecular mechanisms that underlie sleep and circadian rhythm disturbances in older adults are poorly understood. The 24-hour sleep-wake cycle influences the regulation of the immune-inflammatory response,15 and interactions among the central nervous, endocrine, and immune systems,16 yet precise mechanisms in humans are elusive, particularly in older adults. Conference presenters proposed several knowledge gaps and research opportunities designed for laboratory and animal research. Proposals included research to determine the effects of obstructive sleep apnea (OSA)-related intermittent hypoxemia on the aging brain, as well as unravelling the degeneration of circadian systems (suprachiasmatic nucleus, peripheral oscillators) and sleep circuitry. Other suggestions to move sleep science forward include: 1) developing animal models to explain the origins of phenomena such as “sundowning”; 2) identifying biological mechanisms of sleep-related inflammatory and metabolic responses; and 3) determining the relative value of biomarkers to quantify sleep and brain function.
The underlying mechanisms and complex interrelationships between declining physical and mental health and sleep quality in older individuals are poorly understood. Illnesses such as cancer can precipitate sleep disruption, although the reverse may also be true. Prolonged sleep loss may hasten aging and neurodegenerative processes in the brain and heighten sensitivity to metabolic stress. Recognizing these complex relationships can provide avenues for investigation of critical importance to older adults. Presenters focused on several research opportunities respectively relating to: 1) identifying mechanisms underlying sleep-brain health; 2) distinguishing pathogenic degeneration of sleep from other neurodegenerative pathways and general neural function; 3) understanding the role of sleep in glymphatic, perivascular brain circulation for removal of extracellular proteins and metabolic waste (eg, amyloid B, a peptide associated with Alzheimer’s disease): and 4) characterizing relationships between age-related sleep loss/disturbance and metabolic dysregulation and inflammatory markers (eg, IL-6, TNFα, c-reactive protein). Finally, conference presenters posited the need to determine the most sensitive biological and circadian measures of sleep improvement attributable to pharmacological and non-pharmacological interventions.
Physiologic: Clinical Science Issues
The knowledge gaps and research opportunities related to sleep and aging in people with cancer fall into three broad categories: 1) benefits of sleep to prevent adverse outcomes; 2) adverse effects of poor sleep on health outcomes; and 3) impact of disturbed sleep during hospitalization and the transition from hospital to home. According to conference presenters, new scientific discoveries elucidate the benefits of sleep and suggest that sufficient sleep enhances memory by consolidating memories and stimulating circuits to remodel and erase spurious memories.17 Animal and human studies have revealed that after intensive working memory training slow wave activity (SWA) is increased in a small left frontoparietal cluster as measured by high-density EEG recordings. This increase reflects synaptic plasticity in children and young adults.18 Though much progress has been made, many knowledge gaps related to sleep and its impact on brain and physical health remain. For example, what is the role of napping in promoting brain health and cognitive functioning? What is the role of sleep in neural plasticity and/or neurodegenerative disorders? Future research may involve mapping of sleep SWA in older adults with working memory deficiencies.
The adverse effects of poor sleep on health outcomes has been the focus of extensive research, which has led to improvements in our understanding of the importance of sleep. Sleep disruption and circadian misalignments contribute to cardio-metabolic and brain disorders common with aging. Sleep-disordered breathing has been associated with the development of cardiovascular, cerebrovascular, and metabolic disease; REM sleep behavior has been implicated in Parkinson’s disease; and new evidence supports the occurrence of sleep and circadian rhythm abnormalities in the pathogenesis of Alzheimer’s Disease.19 Although not discussed at the conference, sleep disorders and circadian rhythm abnormalities have been implicated in cancer and cancer treatment.20 In light of these relationships, conference presenters asserted that interventions for improving sleep-circadian health can be viewed as new targets for disease prevention and disease modification. Examples of knowledge gaps as they pertain to people with cancer include: What are the clinical implications of sleep-disordered breathing and its treatment relative to cancer and cancer prevention? Is there a therapeutic role for sleep and circadian rhythm optimization in reducing the risk of cancer, modifying cancer activity, and improving cancer treatment outcomes?
Finally, people with cancer frequently spend time in the hospital for cancer treatment and/or the side effects of cancer treatment. Hospitalized older adults are at risk for sleep disorders. One presenter reported that 2 out of every 5 general medical inpatients in an academic medical center were at high risk for obstructive sleep apnea.21 These high-risk patients slept 5 hours per night, had 70% sleep efficiency, as well as poor sleep quality, and were relatively more likely to receive sleep medication while hospitalized. Hospitalized patients with undiagnosed sleep apnea are at risk for respiratory failure from inappropriate prescribing of sedatives. Routinely screening older hospitalized adults for sleep disorders may lead to reductions in preventable adverse events and to improved health. Hospitalization, though necessary, is a time of acute vulnerability for the older adult, who is at risk for delirium, hyperglycemia, falls, and sleep loss. One conference presenter reported that patients sleep 2 hours per night less in the hospital than in their home.22,23 Patient-reported in-hospital sleep disruptions that led to poor quality sleep have included pain, vital signs, tests, and noise. Knowledge gaps relate to the effects of prompt screening for sleep apnea on health outcomes in hospitalized older adults; influence of better pain management and a corrected hospital environment on sleep and circadian rhythms; and the impact of improved sleep and circadian rhythms on hospital-acquired conditions. Targeting improved symptom management and enhancing the sleep environment in the hospitalized older adult may lead to better health outcomes.
Recommendations
We propose an agenda for change through several recommendations to address the conceptual, methodological, and physiological issues facing scientists conducting sleep research related to aging, particularly in individuals with cancer. The planners of the U13 conference met the goals of raising awareness of research in geriatric sleep and facilitating the development of geriatric sleep researchers. Yet, to address the conceptual, methodological, and physiological issues raised in this paper, we recommend additional interdisciplinary forums to: 1) standardize sleep terminology and measurements, 2) create a comprehensive conceptual model, and 3) determine key priorities for physiological and behavioral geriatric sleep research funding, with an emphasis on comorbid conditions (e.g., cancer).
Defining sleep terminology and delineating the complex interactions between and among key sleep-related concepts across the aging and cancer trajectory are the first steps to advancing the field. Precision of sleep terms will contribute to improved communication between and among scientists and clinicians. An overarching conceptual model is needed to facilitate the integration of research findings across sleep studies and to link theory with research and oncology clinical practice. Standard methods to assess sleep, sleep disturbances, and napping can move the science forward across and within disciplines. Standard sleep assessments also will provide needed consistency across settings and providers, and in so doing can facilitate the documentation and monitoring of sleep disorders. Although objective methods to assess sleep are relatively well accepted, multiple instruments to subjectively assess sleep are used, which may lead to conflicting results even within the same cancer population. The choice of sleep instrument should be driven by the research question and availability of resources to conduct the research. The most comprehensive sleep assessment should be conducted within the confines of available resources in both research and clinical practice. Consistently assessing sleep along with frequent co-occurring symptoms, such as fatigue and pain, would further promote our understanding of complex symptom interactions and the effects on brain and physical health in older people with cancer.
Studies designed to understand the pathophysiologic complexity and multifactorial nature of sleep disturbance in older adults are needed, particularly in those with multimorbidity. Effective prevention and treatment of sleep disturbances in older adults depend on teasing out these mechanisms. Future research will need to identify vulnerability factors that put older individuals at risk of sleep-circadian disturbances, including testing promising biomarkers. Hospitalized and sleep-impaired older adult patients are vulnerable to iatrogenic complications, suggesting the vital need to recognize and reduce contributing factors in sleep disturbances. The most effective strategies to implement screening for sleep apnea, minimize cancer-related pain and other symptoms, and reduce the risk for delirium need to be tested in hospitalized older adults. To improve uptake of evidence-based sleep screening and management, clinicians will need to partner with researchers in the design and conduct of implementation research. Finally, national resources for funding in age-related sleep research will need to be developed.
Conclusions
Sleep is a fundamental biological imperative. Older adults are at increased risk for insufficient sleep and sleep-circadian disorders because of changes in the environment, unhealthy behaviors, and disease.24 Poor sleep ultimately can lead to problematic medical, neurologic, and psychiatric conditions.25 Experts at the conference highlighted recent findings indicating that sleep has an essential role in the expression and development of disease, suggesting an agenda for research in older adults with cancer. As such, interventions to improve sleep and circadian health have the transformative potential to maximize healthy aging, particularly in vulnerable older adults with cancer. Additional research is needed to address and prioritize conceptual, methodological, and physiological issues in the aging cancer population. Nurse scientists and multidisciplinary clinicians need to be fully engaged in these research efforts. The ultimate goal is to develop better understanding of concepts, measurement, and biological aspects of sleep in this population. Better understanding can lead to effective, safe, and targeted interventions for older adults with cancer-related sleep-circadian disturbances that can be translated into clinical practice.
Implications for Practice.
Research that addresses current conceptual, methodological, and physiological issues can lead to more effective, safe, and targeted care for older adults with cancer-related sleep-circadian disturbances.
Acknowledgments
U13 Conference Series supported by National Institute on Aging and American Geriatric Society. Additional support provided by unrestricted educational grants from the American Academy of Sleep Medicine, Pfizer, and Philips-Respironics.
Footnotes
Declaration of Conflicting Interests: Dr. Otte received a travel stipend from Indiana University to attend the U13 conference. The other authors have no funding or conflicts of interest to disclose.
References
- 1.Inouye SK, Studenski S, Tinetti ME, Kuchel GA. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc. 2007;55(5):780–791. doi: 10.1111/j.1532-5415.2007.01156.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ong JC, Crisostomo MI. The more the merrier? Working towards multidisciplinary management of obstructive sleep apnea and comorbid insomnia. J Clin Psychol. 2013;69(10):1066–1077. doi: 10.1002/jclp.21958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marengoni A, Angleman S, Melis R, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. 2011;10(4):430–439. doi: 10.1016/j.arr.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 4.Fleming L, Randell K, Harvey CJ, Espie CA. Does cognitive behaviour therapy for insomnia reduce clinical levels of fatigue, anxiety and depression in cancer patients? Psychooncology. 2014;23(6):679–684. doi: 10.1002/pon.3468. [DOI] [PubMed] [Google Scholar]
- 5.Zdanys KF, Steffens DC. Sleep Disturbances in the Elderly. Psychiatr Clin North Am. 2015;38(4):723–741. doi: 10.1016/j.psc.2015.07.010. [DOI] [PubMed] [Google Scholar]
- 6.Barnes CM, Drake CL. Prioritizing Sleep Health: Public Health Policy Recommendations. Perspect Psychol Sci. 2015;10(6):733–737. doi: 10.1177/1745691615598509. [DOI] [PubMed] [Google Scholar]
- 7.Society AG. U13 Conference Presentations. 2015 http://www.americangeriatrics.org/health_care_professionals/research_conferences/sleep_conference/. Accessed August 23, 2016.
- 8.American, Cancer, Society. ACS Cancer Glossary. http://www.cancer.org/cancer/cancerglossary/index. Accessed August 23, 2016.
- 9.Otte JL, Carpenter JS, Manchanda S, et al. Systematic review of sleep disorders in cancer patients: can the prevalence of sleep disorders be ascertained? Cancer medicine. 2015;4(2):183–200. doi: 10.1002/cam4.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Otte JL, Carpenter JS. Theories, models, and frameworks related to sleep-wake disturbances in the context of cancer. Cancer Nurs. 2009;32(2):90–104. doi: 10.1097/01.NCC.0000339261.06442.7d. quiz 105–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berger AM, Parker KP, Young-McCaughan S, et al. Sleep wake disturbances in people with cancer and their caregivers: state of the science. Oncol Nurs Forum. 2005;32(6):E98–126. doi: 10.1188/05.ONF.E98-E126. [DOI] [PubMed] [Google Scholar]
- 12.Clark J, Cunningham M, McMillan S, Vena C, Parker K. Sleep-wake disturbances in people with cancer part II: evaluating the evidence for clinical decision making. Oncol Nurs Forum. 2004;31(4):747–771. doi: 10.1188/04.ONF.747-771. [DOI] [PubMed] [Google Scholar]
- 13.Vena C, Parker K, Cunningham M, Clark J, McMillan S. Sleep-wake disturbances in people with cancer part I: an overview of sleep, sleep regulation, and effects of disease and treatment. Oncol Nurs Forum. 2004;31(4):735–746. doi: 10.1188/04.ONF.735-746. [DOI] [PubMed] [Google Scholar]
- 14.Bruyneel M, Ninane V. Unattended home-based polysomnography for sleep disordered breathing: current concepts and perspectives. Sleep Med Rev. 2014;18(4):341–347. doi: 10.1016/j.smrv.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 15.Besedovsky L, Lange T, Born J. Sleep and immune function. Pflugers Arch. 2012;463(1):121–137. doi: 10.1007/s00424-011-1044-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reis ES, Lange T, Köhl G, et al. Sleep and circadian rhythm regulate circulating complement factors and immunoregulatory properties of C5a. Brain Behav Immun. 2011;25(7):1416–1426. doi: 10.1016/j.bbi.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 17.Westermann J, Lange T, Textor J, Born J. System consolidation during sleep – a common principle underlying psychological and immunological memory formation. Trends Neurosci. 2015;38(10):585–597. doi: 10.1016/j.tins.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 18.Pugin F, Metz AJ, Wolf M, Achermann P, Jenni OG, Huber R. Local increase of sleep slow wave activity after three weeks of working memory training in children and adolescents. Sleep. 2015;38(4):607–614. doi: 10.5665/sleep.4580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pushpanathan ME, Loftus AM, Thomas MG, Gasson N, Bucks RS. The relationship between sleep and cognition in Parkinson’s disease: A meta-analysis. Sleep Med Rev. 2016;26:21–32. doi: 10.1016/j.smrv.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 20.Zhang XB, Peng LH, Lyu Z, Jiang XT, Du YP. Obstructive sleep apnoea and the incidence and mortality of cancer: a meta-analysis. Eur J Cancer Care. doi: 10.1111/ecc.12427. http://onlinelibrary.wiley.com/doi/10.1111/ecc.12427/abstract. Accessed August 23, 2016. [DOI] [PubMed]
- 21.Shear TC, Balachandran JS, Mokhlesi B, et al. Risk of sleep apnea in hospitalized older patients. J Clin Sleep Med. 2014;10(10):1061–1066. doi: 10.5664/jcsm.4098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yoder JC, Staisiunas PG, Meltzer DO, Knutson KL, Arora VM. Noise and sleep among adult medical inpatients: far from a quiet night. Arch Intern Med. 2012;172(1):68–70. doi: 10.1001/archinternmed.2011.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adachi M, Staisiunas PG, Knutson KL, Beveridge C, Meltzer DO, Arora VM. Perceived control and sleep in hospitalized older adults: a sound hypothesis? J Hosp Med. 2013;8(4):184–190. doi: 10.1002/jhm.2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smagula SF, Stone KL, Fabio A, Cauley JA. Risk factors for sleep disturbances in older adults: Evidence from prospective studies. Sleep Med Rev. 2016;25:21–30. doi: 10.1016/j.smrv.2015.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ancoli-Israel S. Sleep and its disorders in aging populations. Sleep Med. 2009;10(Suppl 1):S7–11. doi: 10.1016/j.sleep.2009.07.004. [DOI] [PubMed] [Google Scholar]


