Abstract
BACKGROUND
HIV-infected children with long-term nonprogressive disease (LTNPs) eventually convert to a progressive disease type, yet the extent to which these children experience the cognitive and emotional symptoms observed in typical progressive HIV (Progressors) is unknown.
METHODS
Eighty-eight LTNPs, 53 Progressors, and 323 healthy controls completed annual assessments of cognitive and emotional health as part of a prospective study. The two HIV-infected groups and the healthy controls were matched on age and sex distribution at enrollment. Plasma HIV RNA, T-cell counts/percentages, activated monocytes, perivascular monocytes, and markers of macrophage activation (sCD163 and sCD14) were compared by progression subtype. Cognitive and emotional outcomes were compared using cross-sectional linear regression analysis and longitudinal sensitivity models.
RESULTS
LTNPs exhibited the same cognitive phenotype and emotional dysregulation as Progressors, with worse outcomes in both groups compared to controls. Additionally, cognitive and emotional symptoms were evident before children reached the minimum age for LTNP designation (8 years). Baseline plasma HIV RNA, sCD163, activated monocytes, and perivascular monocytes were lower in LTNPs versus Progressors, with no difference in T-cell counts/percentages or sCD14 levels. Most LTNPs converted to a progressive disease subtype during the study, with similar cognitive and emotion profiles between these subgroups.
CONCLUSIONS
Pediatric LTNPs experience cognitive and emotional difficulties that mirror symptoms of progressive disease. The abnormalities are present at young ages and persist independent of plasma T-cell counts. The findings highlight the neurodevelopmental risk of pediatric HIV, even in those with early innate disease control.
INTRODUCTION
Nearly half of all children exposed to human immunodeficiency virus (HIV) in utero, during birth, or breast feeding, will develop viral infection and subsequent immunosuppression.1 In the absence of treatment, the mortality rate of pediatric HIV exceeds 50% within three years from birth.2–3 Most HIV-infected children who survive the early postnatal period develop persistent plasma viremia and CD4 T-cell depletion characteristic of progressive HIV disease. However, a subset of HIV-infected children display some degree of innate capacity to maintain CD4 T-cell counts > 350 cells/mm3 and plasma viral loads levels < 10,000 copies per ml without prior or current treatment.4–5 Phenotypically, these individuals are described as pediatric long-term nonprogressors (LTNPs).6
Compared to children with progressive disease (identified herein as Progressors), pediatric LTNPs are more likely to express the delta 32 mutation on the CCR5 gene,7 exhibit higher levels of anti-nef antibodies,8–9 lower levels of cytotoxic T-cells, lower levels of memory CD4+ T-cells, and a higher percentage of plasma-derived naïve CD4+ T-cells,4,10–11 all of which correspond to less intense disease activity compared to pediatric Progressors. However, elevated plasma levels of activated T helper cells and T cytotoxic cells have been reported in a well-characterized cohort of pediatric LTNPs.6 Additionally, longitudinal studies demonstrate that most LTNPs eventually convert to a progressive disease phenotype,12 raising concern that these children harbor an underlying vulnerability for HIV-related disease complications despite innate control over select disease mechanisms early in life.
Cognitive and emotional complications of HIV have long been recognized as important components of pediatric HIV. Pediatric Progressors exhibit impaired intellectual performance and poor academic achievement when compared to demographically similar HIV-uninfected peers.13–14 Below average performance in attention, executive function, learning, and memory is common in children with HIV infection,15–19 and the cognitive difficulties remain despite otherwise successful HIV treatment.20–22 Numerous studies also identify poor emotional health in this population.23–25 HIV-infected children face psychosocial pressures typical of youth, plus the challenge of managing a chronic illness characterized by high potential for stigma and social marginalization.
Limited information is available regarding the extent to which pediatric LTNPs experience the cognitive and emotional challenges typical of progressive HIV. Results from a cross-sectional investigation of 12 treatment-naïve children with CD4>25%, and WHO Stage 1 disease revealed worse executive function, processing speed, attention, and memory in the HIV-infected sample compared to demographically-similar healthy controls.26 Pediatric slow progressors also exhibited abnormalities on neuroimaging when compared to Progressors on ART.27 These preliminary outcomes, combined with the recognition that most pediatric LTNPs eventually convert to a progressive subtype, suggest that children with robust viral control may be vulnerable to poor cognitive and emotional outcomes.
No prospective studies have examined cognitive or emotional complications associated with LTNP disease progression or whether immunological markers of brain integrity correspond to cognitive and emotion phenotypes in this population. The present study addressed these gaps by leveraging the prospective design of the Pediatric Randomized Early vs. Deferred Initiation in Thailand study (PREDICT).28 Prior studies from PREDICT revealed no differences in AIDS-defining illnesses28 or cognitive outcomes29 among children who initiated ART early (i.e., CD4 15–24%) compared to children who initiated treatment consistent with treatment guidelines in practice at the time (CD4<15%). Based on the results of children with slow progressive disease and the observation of high conversion from LTNP to progressive disease type, we hypothesized that pediatric LTNPs would exhibit cognitive and emotional abnormalities that were similar to Progressors, and the severity of these symptoms would correspond to plasma-derived immune markers previously linked to HIV neuropathogenesis.
METHODS
Study Design
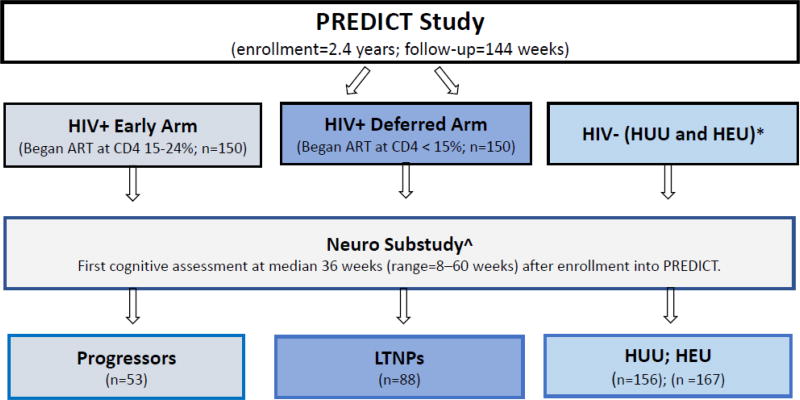
The PREDICT28 study (clinicaltrials.gov identification number NCT00234091) enrolled 300 HIV-infected, treatment-naïve children age 2–17 from Thailand and Cambodia. A neuro sub-study of PREDICT was initiated approximately one year after the start of the parent trial. Results reported in the present study were acquired in the neuro sub-study. The PREDICT trial and the neuro sub-study were approved by Institutional Review Boards from each participating agency. Informed consent was obtained from caregivers following a thorough explanation of the study procedures. Assent was obtained from children older than age 8 years of age.
Participants completed standardized assessments of cognition and emotional health on an annual basis. Since LTNP designation required a minimum age of 8 years, the PREDICT study enrolled and prospectively followed children up to 7 years prior to individual LTNP designation. Additionally, most of the participants elected to enroll in subsequent prospective studies after completing the PREDICT trial, and they were administered many of the same cognitive and emotional health outcome measures in the follow-up studies. We included results from children randomized to the deferred treatment arm of the PREDICT trial as well as the additional study visits to extend the follow-up period of the LTNP group (median: 5.7 years; IQR: 5.2–6.1). The study design (see Figure 1) provided the opportunity to address cognitive and emotional health in LTNPs from three clinically relevant perspectives. First, we employed a cross-sectional model to contrast cognitive, emotional, and immunological indices of LTNPs, Progressors, and healthy controls. Second, a prospective model examined all available time points, including annual assessments completed before children met the minimum age of 8 for LTNP classification. Third, we examined demographic, immune, viral, and cognitive/emotional indices in the minority of children who continued to meet LTNP designation over all follow-up periods (n=17) compared to LTNPs who converted to a progressive disease subtype (n=71).
Figure 1.
Long-term nonprogressors (LTNPs); HIV unexposed, uninfected (HUU); HIV exposed, uninfected (HEU). ^Median duration of follow-up: 5.8 (5.4–6.1 years. *Median duration of follow-up: 2.3 (2.0–2.9) years.
Participants
Pediatric LTNPs (n=88), Progressors (n=53), and two groups of HIV-uninfected healthy controls (n=323) were included in the present study. HIV-infected children were treatment-naïve at the time of study enrollment, and began treatment prior to experiencing sustained immunosuppression. HIV-uninfected children were recruited from regional health clinics with similar demographic characteristics of LTNPs and Progressors. The two healthy control groups included HIV exposed, but uninfected children (HEU, n=157) and HIV unexposed, uninfected children (HUU, n=166). Inclusion criteria were as follows: (1) HIV confirmed by positive antibody test for the HIV-infected children; (2) younger than 18 years of age; and (3) informed consent by legal guardians and assent by children older than 8 years of age. Exclusion criteria included: (1) previous or current brain infection; (2) neurological or psychiatric disorder known to affect brain integrity; (3) congenital abnormalities; (4) previous use of immunomodulators within four weeks of enrollment; (5) absolute neutrophil count < 750 cells/mL, hemoglobin < 7.5 g/dL; (6) platelet counts < 50,000 per mL; or (7) alanine aminotransferase > 4 times greater than average. LTNP designation was determined using previously established criteria6 (at least 8 years old, CD4 T-cell count > 350 cells/mm3, and no history of ART).
Neuropsychological Assessment
Participants completed age-appropriate neuropsychological tests selected for cultural relevance in Thailand and Cambodia. The tests were administered by study personnel in accordance with a rigorous training program and quality control system to ensure high fidelity to standardized administration and scoring procedures. Cognitive testing was completed in the child’s native language (Thai or Khmer) and occurred approximately one year after enrollment into the main PREDICT trial when the neuro sub-study was initiated. The neuropsychological battery included Children’s Color Trails Test 1 and 2 (Color Trails),29 Beery Visual Motor Integration (Beery VMI),30 and Purdue Pegboard.31 Raw scores served as dependent variables.
Children from Thailand were also administered the Thai version of the Wechsler Scale of Intelligence for Children – III (WISC-III).32 This version includes modifications to the Vocabulary, Comprehension, and Similarities subtests to ensure cultural relevancy for Thai children. Normative data from more than 3,000 Thai children without neurological/psychological histories revealed acceptable psychometric properties for the primary summary scales. Dependent measures from the WISC III included the Verbal Intelligence Quotient (VIQ), the Performance Intelligence Quotient (PIQ), and the Processing Speed Index Quotient (PSIQ). Performances on the WISC-III were converted to standardized scores. A Cambodian version of the test was not available for administration and therefore the intellectual measures were only administered to the Thai sample.
Emotion Measure
Emotion and behavioral dysregulation was measured using the Child Behavior Checklist (CBCL).33 The scale was translated into Thai and Khmer and back-translated into English to ensure accuracy. Caregivers completed the CBCL at each study visit. Raw scores were converted to standardized indices based on external norms. Three scales served as the primary variables of interest for this study, including the Internalizing (anxiety, depression, and somatic complaints), Externalizing (rule breaking and aggressive behavior), and the Total Problem scale (sum of scales). This approach is consistent with prior studies that reported CBCL outcomes from the parent PREDICT trial and other pediatric cohorts in Thailand.34–36
Laboratory Variables
Laboratory markers were collected at enrollment into the neuro-study (and before Progressors initiated treatment). Standard HIV disease variables included CD4 and CD8 T-cells (number and percent), CD8/CD4 T-cell ratio, and log transformed plasma HIV viral load. The frequencies of activated monocytes (CD14+/CD16+/HLA-DR+) and perivascular monocytes (CD14+/CD16+/CD163+) were defined by flow cytometry following procedures defined by the National Institute of Allergy and Infectious Diseases – Division of AIDS. A stand-alone ELISA assay quantified plasma levels of sCD14. sCD163 was quantified from plasma using the Macro163 kit (IQ Products and Trillium Diagnostics, Bangor, Maine, USA).
Statistical Analysis
Analyses were conducted with STATA 14.1 (Statacorp, College Station, TX, USA).37 Age differences between groups were compared using analysis of variance (ANOVA). Sex, household income/child living situation, and educational levels of participants and their caregivers were analyzed using Chi-square or Fisher’s exact tests. Preliminary analyses revealed significant group differences in age, sex, living situation, caregiver’s educational level, and household income (see Table 1); therefore, these variables were included as covariates in adjusted models. Country of origin was included as a covariate with the exception of analyses of WISC III measures since these were not administered to the Cambodian sample.
Table 1.
Demographic and HIV disease markers for all participants.
| Characteristic | Progressors (N=53) | LTNP (N=88) | P | HEU (N=157) | HUU (N=166) | P |
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Age at enrollment^ | 4.3 (2.5–5.8) | 8.2 (6.6– 9.7) | <0.001 | 6.8 (5.0–9.8) | 7.4 (5.3–9.8) | <0.001 |
| Age at first cognitive test^ | 5.0 (3.1–6.0) | 8.8 (7.1–10.4) | <0.001 | |||
| Sex, n (%) male | 23 (43.40) | 26 (29.55) | 0.094 | 69 (43.95) | 67 (40.36) | 0.151 |
| Thai: Cambodian (%) | 49:51 % | 68:32 % | 0.024 | 63:37 % | 67:33 % | 0.092 |
| Primary caregiver | 0.693 | <0.001 | ||||
| Parent | 36 (67.92) | 56 (63.64) | 146 (92.99) | 142 (85.54) | ||
| Relative | 10 (18.87) | 22 (25.00) | 6 (3.82) | 22 (13.25) | ||
| Other | 7 (13.21) | 10 (11.36) | 5 (3.18) | 2 (1.20) | ||
| Caregiver education, n (%) | 0.470 | <0.001 | ||||
| None | 9 (16.98) | 14 (15.91) | 18 (11.46) | 10 (6.02) | ||
| Elementary school | 19 (35.85) | 41 (46.59) | 79 (50.32) | 50 (30.12) | ||
| High school | 17 (32.08) | 23 (26.14) | 44 (28.03) | 60 (36.14) | ||
| Vocational School | 4 (7.55) | 2 (2.27) | 10 (6.37) | 24 (14.46) | ||
| Bachelor degree of higher | 4 (7.55) | 8 (9.09) | 1 (0.64) | 12 (7.23) | ||
| Unknown | 0 | 0 | 5 (3.18) | 10 (6.02) | ||
| Income, n (%) | 0.102 | <0.001 | ||||
| Average or above | 10 (18.87) | 31 (35.23) | 71 (45.22) | 110 (66.27) | ||
| Below average | 35 (66.04) | 44 (50.00) | 84 (53.50) | 56 (33.73) | ||
| Unknown | 8 (15.09) | 13 (14.77) | 2 (1.27) | 0 | ||
| HIV disease markers | ||||||
| CD4 cell count cells/mm3^ | 586 (344–769), (n=16) | 581 (435–797), (n=79) | 0.68 | |||
| CD4%^ | 20 (17–25) | 21 (18–23) | 0.96 | |||
| CD8 cell count cells/mm3^ | 1,193 (856–1,596), (n=16) | 1,222 (1,029–1,675), (n=78) | 0.61 | |||
| CD8%^ | 45 (40–51) | 47 (40–51) | 0.99 | |||
| CD4/CD8 cell ratio ^ | 0.44 (0.35 – 0.57) | 0.45 (0.35 – 0.55) | 0.79 | |||
| Log viral load (log10 copies/mL) | 5.0 (4.8–5.0) | 4.4 (4.0–4.8) | <0.001 | |||
| Serum soluble CD14 ng/mL^ | 6.2 (6.1–6.3), (n=41) | 6.2 (6.1–6.4), (n=66) | 0.82 | |||
| Serum soluble CD163ng/mL^ | 4,502 (3,118–5,191), (n=41) | 3,385 (2,559–4,144), (n=66) | 0.02 | |||
| (CD14+/CD16+/HLA-DR+) count, cells/uL)^ | 69.3 (36.0–127.2) (n=36) | 39.1 (17.8– 72.9) (n=36) | 0.03 | |||
| (CD14+/CD16+/HLA-DR+)%^ | 10.4 (6.6–16.1) (n=36) | 7.1(4.8–14.4) (n=36) | 0.17 | |||
| (CD14+/CD16+/CD163+) count, (cells/uL)^ | 41.5 (18.4– 84.2) (n=36) | 15.3 (7.5–39.5) (n=36) | 0.004 | |||
| (CD14+/CD16+/CD163+)%^ | 5.4(3.3– 8.9) (n=36) | 3.5 (1.8 –5.9)(n=36) | 0.02 | |||
All laboratory biomarkers were obtained at the baseline, enrollment visit into PREDICT.
Median (IQR)
Adjusted and unadjusted cross-sectional linear regression models compared cognitive performances and CBCL indices by disease progression subtype. Prospective data were examined using a longitudinal sensitivity analysis (generalized estimating equations; GEE), contrasting the LTNP group to each reference group (Progressors, HEUs, HUUs) and the Progressor group to the three reference groups. This analytic approach allowed comparisons between the HIV-infected children to each control group separately. Laboratory measures were compared using a Wilcoxon test or Kruskal Wallis test. Finally, cognitive, emotion, and laboratory data were compared between children who maintained LTNP designation (n=17) throughout all observation periods compared to children who converted to a progressive disease phenotype (n=71).
RESULTS
Collapsed across progression subtype, the HIV-infected sample included 49 males (35%) and 92 females (65%), and averaged 7.0 (3.0) years of age at baseline. Demographic and clinical characteristics are provided in Table 1. The majority of children in the Progressors group (44/53 = 83%) were on ART at the time of the cross-sectional analysis (median duration: 2.5 years (IQR 1.1–4.0)). First line treatment included zidovudine, lamivudine, and nevirapine. Children who experienced sensitivity to nevirapine were switched to efavirenz or lopinavir boosted with ritonavir. One individual in the Progressors group initiated ART after receiving a diagnosis of esophageal candidiasis one month after enrollment into PREDICT (CD4 =21.5%, viral load=100,000). No other AIDS-defining illnesses were observed.
Cross-Sectional Analyses of Cognitive Performances and CBCL Scales
Adjusted models revealed no differences in cognitive performance between LTNPs and Progressors. Performances on VIQ, PIQ, and PSIQ were similar between the two HIV-infected groups (all ps > 0.20). Additionally, LTNPs and Progressors performed similarly on the Beery VMI, Pegboard, Color Trails 1, and Color Trails 2 (ps > 0.35). When compared to both groups of healthy controls, LTNPs performed worse on VIQ, PIQ, PSIQ, and Color Trails 2 (ps < .05). LTNPs also performed worse than HUUs, but not HEUs, on Color Trails 1 (p < .05). Progressors performed worse than both groups of healthy controls on VIQ, PIQ, PSIQ, and Color Trails 2 (ps < .01), and worse than HUUs, but not HEUs, on Color Trails 1 and the Beery VMI (ps < .05).
On the CBCL, the adjusted analyses revealed similar scores between LTNPs and Progressors on the Internalizing, Externalizing, and Total Problem scales. (Table 2). When compared to both groups of healthy controls, caregivers reported that LTNPs exhibited more symptoms on the Internalizing and Externalizing scales (indicating worse outcomes; ps < .05). Caregivers of the Progressors reported that the children exhibited more symptoms than both groups of healthy controls on all three CBCL scales (ps < .05).
Table 2.
Cross sectional regression models comparing cognitive and emotion indices.
| Test and Group | Unadjusted | Adjusted^ | ||
|---|---|---|---|---|
| Coef (95% CI) | P | Coef (95% CI) | P | |
| VIQ | ||||
| Progressors | −1.09 (−7.06,4.88) | 0.72 | −0.50 (−7.40,6.40) | 0.89 |
| HEUs | 8.93(4.83,13.04) | <0.001 | 5.43 (0.90,9.96) | 0.02 |
| HUUs | 13.51(9.50,17.53) | <0.001 | 10.24 (5.72,14.77) | <0.001* |
| PIQ | ||||
| Progressors | −1.40 (−8.96,6.16) | 0.72 | −5.55 (−14.53,3.44) | 0.23 |
| HEUs | 11.97 (6.78,17.17) | <0.001 | 7.78 (1.89,13.67) | 0.01* |
| HUUs | 16.46 (11.37,21.56) | <0.001 | 11.94 (6.05,17.82) | <0.001* |
| PRIQ | ||||
| Progressors | −4.07 (−12.09,3.95) | 0.32 | −4.59 (−14.06,4.88) | 0.34 |
| HEUs | 12.49 (6.96,18.02) | <0.001 | 10.28 (4.06,16.50) | 0.001* |
| HUUs | 17.33 (11.93,22.74) | <0.001 | 14.15 (7.93,20.36) | <0.001* |
| Beery VMI | ||||
| Progressors | −3.99 (−9.19,1.21) | 0.13 | −2.60 (−8.03,2.84) | 0.35 |
| HEUs | 2.52 (−1.46,6.50) | 0.21 | 1.67 (−2.50,5.83) | 0.43 |
| HUUs | 5.75 (1.80,9.69) | 0.004 | 3.61 (−0.54,7.76) | 0.09* |
| Color Trails 1 | ||||
| Progressors | −2.90 (−8.90,3.11) | 0.34 | −3.03 (−9.53,3.47) | 0.36 |
| HEUs | 2.01 (−2.73,6.75) | 0.40 | −0.31 (−5.43,4.80) | 0.90 |
| HUUs | 10.27 (5.66,14.89) | <0.001 | 7.83 (2.83,12.83) | 0.002* |
| Color Trails 2 | ||||
| Progressors | −1.33 (−6.75,4.09) | 0.63 | −0.23 (−6.15,5.69) | 0.94 |
| HEUs | 8.49 (4.22,12.76) | <0.001 | 6.62 (1.95,11.28) | 0.006* |
| HUUs | 11.05 (6.89,15.21) | <0.001 | 8.56 (4.00,13.12) | <0.001* |
| Purdue Pegboard | ||||
| Progressors | −0.65 (−1.36,0.07) | 0.08 | −0.08 (−0.72,0.56) | 0.81 |
| HEUs | −0.77 (−1.33,−0.22) | 0.007 | −0.40 (−0.89,0.09) | 0.11 |
| HUUs | −0.74 (−1.29,−0.19) | 0.008 | −0.36 (−0.85,0.13) | 0.15 |
| CBCL Internalizing Problem Scale | ||||
| Progressors | −2.89 (−6.20,0.42) | 0.09 | −2.01 (−5.58,1.55) | 0.27 |
| HEUs | −4.03 (−6.56,−1.49) | 0.002 | −3.45 (−6.18,−0.72) | 0.01 |
| HUUs | −5.02 (−7.53,−2.52) | <0.001 | −4.07 (−6.78,−1.35) | 0.003 |
| CBCL Externalizing Problem Scale | ||||
| Progressors | −1.49 (−4.50,1.52) | 0.33 | −1.38 (−4.63,1.86) | 0.40 |
| HEUs | −3.29 (−5.60,−0.98) | 0.005 | −2.66 (−5.14,−0.18) | 0.04 |
| HUUs | −5.38 (−7.66,−3.09) | <0.001 | −4.27 (−6.74,−1.80) | 0.001 |
| CBCL Total Problem Scale | ||||
| Progressors | −2.53 (−5.84,0.78) | 0.13 | −1.94 (−5.50,1.63) | 0.29 |
| HEUs | −3.30 (−5.84,−0.77) | 0.01 | −2.55 (−5.28,0.18) | 0.07 |
| HUUs | −5.52 (−8.03,−3.01) | <0.001 | −4.33 (−7.05,−1.61) | 0.002 |
Results comparing long-term nonprogressors to children with progressive disease (Progressors), and children who were HIV-exposed but uninfected (HEU) and children who were not HIV-exposed (HUU).
Adjusted for age, sex, caregiver education and income, and ethnicity.
p<.05.
Longitudinal Analyses by Disease Progression Subtype
Results of the longitudinal sensitivity analyses were consistent with the cross-sectional outcomes. (Table 3). LTNPs and Progressors performed similarly on VIQ, PIQ, PSIQ, Beery VMI, Color Trails 1, and Color Trails 2 (all p values > 0.14). Pegboard performances were modestly lower among Progressors than LTNPs (p < .01). When compared to both groups of healthy controls, longitudinal analyses revealed worse performance by LTNPs and Progressors on VIQ (ps < 0.001), PIQ (ps < .01), PSIQ (ps < .001), and Beery VMI (ps < 0.001) compared to both control groups. LTNPs performed worse than HUUs, but not HEUs, on Color Trails 1 (p= 0.008) and Color Trails 2 (p=0.006). A similar pattern was evident when Progressors were compared to the control groups (ps < .01), with the addition of worse performance on Color Trails 1 among Progressors compared to HEUs and HUUs (ps < .05).
Table 3.
Longitudinal models comparing cognitive and emotion indices.
| Test and Group | Unadjusted | Adjusted^ | ||
|---|---|---|---|---|
| Coef (95% CI) | P | Coef (95% CI) | P | |
| VIQ | ||||
| Progressors | 1.18 (−4.05,6.42) | 0.66 | 2.00 (−4.28,8.28) | 0.53 |
| HEUs | 11.53 (7.87,15.19) | <0.001 | 8.05 (3.85,12.25) | <0.001 |
| HUUs | 17.06 (13.49,20.63) | <0.001 | 13.75 (9.58,17.92) | <0.001* |
| PIQ | ||||
| Progressors | −3.63 (−10.13,2.87) | 0.27 | −5.83 (−13.58,1.92) | 0.14 |
| HEUs | 9.24 (4.71,13.76) | <0.001 | 6.68 (1.51,11.85) | 0.011* |
| HUUs | 13.73 (9.32,18.15) | <0.001 | 10.86 (5.72,16.00) | <0.001* |
| PRIQ | ||||
| Progressors | −3.83 (−10.76,3.10) | 0.28 | −2.38 (−10.85,6.09) | 0.58 |
| HEUs | 11.45 (6.58,16.31) | <0.001 | 10.79 (5.10,16.47) | <0.001* |
| HUUs | 15.94 (11.21,20.68) | <0.001 | 14.34 (8.70,19.98) | <0.001* |
| Beery VMI | ||||
| Progressors | −1.71 (−5.81,2.39) | 0.41 | −0.77 (−4.94,3.41) | 0.72 |
| HEUs | 6.47 (3.23,9.71) | <0.001 | 5.89 (2.59,9.19) | <0.001* |
| HUUs | 9.32 (6.12,12.52) | <0.001 | 7.60 (4.33,10.86) | <0.001* |
| Color Trails 1 | ||||
| Progressors | −2.27 (−6.81,2.27) | 0.33 | −1.84 (−6.65,2.98) | 0.45 |
| HEUs | −0.81 (−4.42,2.80) | 0.66 | −1.67 (−5.49,2.15) | 0.39 |
| HUUs | 7.01 (3.52,10.51) | <0.001 | 5.08 (1.35,8.80) | 0.008* |
| Color Trails 2 | ||||
| Progressors | −1.94 (−6.26,2.38) | 0.38 | −1.85 (−6.65,2.94) | 0.45 |
| HEUs | 4.36 (0.94,7.79) | 0.01 | 3.61 (−0.18,7.40) | 0.06* |
| HUUs | 7.28 (3.97,10.60) | <0.001 | 5.19 (1.49,8.90) | 0.006* |
| Purdue Pegboard | ||||
| Progressors | −2.34 (−2.96,−1.71) | <0.001 | −2.22 (−2.91,−1.53) | <0.001 |
| HEUs | −1.79 (−2.29,−1.28) | <0.001 | −1.68 (−2.23,−1.13) | <0.001 |
| HUUs | −1.77 (−2.26,−1.27) | <0.001 | −1.79 (−2.33,−1.24) | <0.001 |
| CBCL Internalizing Problem Scale | ||||
| Progressors | 0.38(−1.87,2.64) | 0.74 | 1.38 (−0.92,3.69) | 0.24 |
| HEUs | −2.46(−4.30,−0.63) | 0.008 | −2.30 (−4.18,−0.42) | 0.02* |
| HUUs | −2.05(−3.86,−0.24) | 0.03 | −1.70 (−3.56,0.16) | 0.07* |
| CBCL Externalizing Problem Scale | ||||
| Progressors | 0.85 (−1.12,2.81) | 0.40 | 1.38 (−0.74,3.49) | 0.20 |
| HEUs | −2.45 (−4.06,−0.85) | 0.003 | −2.03 (−3.76,−0.31) | 0.02* |
| HUUs | −3.33 (−4.91,−1.75) | <0.001 | −2.68 (−4.38,−0.98) | 0.002* |
| CBCL Total Problem Scale | ||||
| Progressors | 0.79 (−1.49,3.08) | 0.50 | 1.80 (−0.57,4.17) | 0.14 |
| HEUs | −1.93 (−3.78,−0.07) | 0.04 | −1.36 (−3.29,0.56) | 0.17* |
| HUUs | −2.62 (−4.44,−0.79) | 0.005 | −1.84 (−3.74,0.07) | 0.06* |
Results comparing long-term nonprogressors to children with progressive disease (Progressors), and children who were HIV-exposed but uninfected (HEU) and children who were not HIV-exposed (HUU).
Adjusted for age, sex, caregiver education and income, and ethnicity.
p<.05.
On the CBCL, longitudinal analyses revealed similar index scores between LTNPs and Progressors on all three scales (ps > .05). Compared to healthy controls, caregivers reported that LTNPs exhibited more symptoms on the Externalizing scale and Internalizing scale than HEUs (ps < .05). Internalizing, Externalizing, and Total Problem scores were higher in Progressors than both groups of healthy controls (ps < .05).
Disease Progression Subtypes and Baseline Laboratory Markers
Of the 88 individuals in the LTNP group, 44 (50%) met the LTNP criteria at the time of enrollment. The remainder of the LTNP sample (n=44) met criteria when the children reached age 8. The median time from baseline to LTNP classification was 6 weeks (IQR 0 – 79), and the median time from baseline to determination of progressive disease was 72 weeks (IQR 59 – 120). At baseline, LTNPs had lower median log10 plasma HIV RNA, lower sCD163 concentrations, lower counts of activated monocytes, and lower counts and frequencies of perivascular monocytes than Progressors (all ps < .05) (Table 1). By contrast, sCD14 plasma levels and total counts and percentages of CD4 and CD8 T-cells and CD4/CD8 ratios did not differ between LTNPs and Progressors (all ps > .6).
Exploratory correlational analyses revealed associations between laboratory indices and cognitive performance/CBCL scales at the cross-sectional visit when LTNP status was ascertained. Among LTNPs, lower sCD163 levels correlated with higher PSIQ scores (r = −.30), and lower perivascular monocyte percentage correlated with higher VIQ scores (r = −.55) and PIQ scores (r = −.50). Higher CD8 percent among LTNPs correlated modestly with better performance on the Pegboard test (r = .29). On the CBCL, higher CD8 percent correlated modestly with more severe problems on the Internalizing scale (r = .28). Among Progressors, higher perivascular monocyte cell counts correlated with higher PIQ scores (r = .54), better performances on Color Trails 2 (r = .40), and higher (worse) scores on the CBCL Externalizing scale (r = .47). Finally, higher CD8 counts correlated inversely with performance on the Pegboard (r = −.30). (Supplemental Figure 1).
Extended Follow-Up of LTNPs
Seventy-one of the 88 LTNPs converted to a progressive disease type over the follow-up period (median 5.7 years). The 17 children who continued to meet LTNP criteria had higher baseline CD4 T-cell counts and percentages than children who converted to a progressive subtype. (Supplemental Table 1). Plasma HIV RNA levels did not differ between converters and nonconverters, and there were no differences at baseline in sCD14, sCD163, or activated monocyte and perivascular monocyte concentrations between converters and nonconverters. Individuals that maintained the LTNP designation exhibited the same cognitive test performances as Progressors. The one exception was performance on Color Trails 1, on which children who maintained LTNP status performed worse than converters (p=0.03). On the CBCL scales, adjusted analyses revealed higher scores (worse outcomes) on the Internalizing scale (p = 0.03) and the Total Problem scale (p = 0.02) among children who maintained LTNP status compared to converters. Children who maintained LTNP status were also identified by caregivers as experiencing more symptoms than converters on the Externalizing scale, but the difference was not significant (p = 0.07).
DISCUSSION
The present study reveals several important findings. First, pediatric LTNPs exhibit cognitive and emotional complications that are similar in nature and severity to the challenges experienced by children with progressive disease. Results from both cross-sectional and longitudinal sensitivity analyses revealed a similar phenotype of cognitive and emotional disruption relative to HIV-uninfected controls. Second, baseline levels of select viral and immune factors were preserved in LTNPs when compared to Progressors, while other markers did not differ between groups (i.e., sCD14 plasma levels, CD4 and CD8 T-cells counts/percentages and ratios). Third, nearly all LTNPs converted to a progressive disease subtype over the course of the study, yet LTNPs who maintained viral control without treatment exhibited the same pattern of cognitive difficulties and some evidence of worse emotional health compared to children who converted to progressive disease.
The observation of cognitive symptoms among HIV-infected, treatment-naïve children with functionally intact CD4 T-cell counts is consistent with preliminary work conducted in South Africa26–27 and Uganda.38 When compared to HUUs and HEUs, the two HIV-infected groups in the current study performed worse on intellectual measures, and tests of psychomotor speed, executive function, and visuomotor integration. These findings remained after adjustments for potential confounds and were observed in both cross-sectional and longitudinal analyses. The cognitive phenotype resembles the profile of typical pediatric HIV.13–19 It remains unknown if earlier treatment would lead to better long-term outcomes in pediatric LTNPs. Results from the CHER study revealed better cognitive outcomes when ART is initiated ART within the first 6 months of life,39 which coincides with the main results of the PREDICT study. Collectively, the data suggest that the critical window of treatment initiation is very early, at least in terms of cognitive outcomes. Whether long-term complications of HIV can be fully arrested in perinatally infected children requires further study.
Our study also identified higher rates of emotional and behavioral dysregulation in LTNPs and Progressors compared to healthy controls. Results from the adjusted analyses revealed no differences between the LTNPs and Progressors on scales sensitive to depression, withdrawal, agitation, or disobedience. It is important to note that the CBCL was completed by caregivers and the results may not fully reflect the burden perceived by the children themselves. Nevertheless, the observation that LTNPs are described by caregivers as burdened by symptoms of emotional and behavioral dysregulation indicates that while LTNP designation corresponds to some immunologically advantages, these children are not free of emotional and behavioral complications.
Baseline laboratory results revealed lower plasma HIV RNA (median log10), sCD163 levels, and frequencies of activated monocytes, and perivascular monocytes in LTNPs compared to Progressors. (Table 1). By contrast, sCD14 plasma levels and total counts and percentages of CD4 and CD8 T-cells and CD4/CD8 ratios were similar between the two HIV-infected groups. The observation that sCD163 and CD14+/CD16+/CD163+ were lower in LTNPs than Progressors is intriguing, as both immune markers correspond to cognitive performance in HIV-positive adults.40–44 Correlation analyses focused on LTNPs revealed inverse associations between the PSIQ and PIQ with sCD163 levels, and an inverse association between VIQ and frequencies of perivascular monocytes. The functional relevance of these immune activation makers requires further examination since the correlational analyses conducted in this study were exploratory and associations were evident in both groups of HIV-infected children.
At the longest follow-up visit, all but 17 of the 88 LTNPs converted to progressive disease, and while those who maintained LTNP status had higher CD4 T-cell counts and lower plasma HIV RNA levels, the cognitive and emotional symptoms were nearly identical to children who converted to a progressive subtype. The primary exception being worse performance on one test of fine motor speed and worse emotional health among the group with sustained LTNP status. Interestingly, children who sustained LTNP status were rated by caregivers as having more severe difficulties on the CBCL compared to converters. Whether differences in clinical contact among Progressors translated into fewer perceived emotional and behavioral problems requires further study.
The observation that pediatric LTNPs convert to a progressive subtype differs from the long-term outcome of HIV-infected adults with innate viral control. The difference in disease progression may be due to the absence of protective human leukocyte antigen (HLA) class I alleles (e.g., HLA-B*27) in pediatric LTNPs.45–46 Posthoc analyses of our data revealed a low frequency of HLA-B*27 heterozygosity in Progressors (7.5%) and LTNPs (9.2%), with no difference in risk allele frequencies between groups. Similarly, heterozygosity of HLA-B*57 was uncommon in our samples of Progressors (1.9%) and LTNPs (3.5%), again with no difference in the frequency of the risk allele. Recent work by Muenhchoff et. al.12 suggests that the pace of disease progression in pediatric HIV is likely determined by immune activation rather than the severity of viral replication. Our data provide ancillary support for this perspective, as we observed high sCD14 levels in children years before they met the minimum age criteria for LTNP.
Limitations of the study merit consideration. The main PREDICT trial enrolled children as young as 12 months of age, and the baseline assessments for cognition, emotional/behavioral function, and entry labs occurred several years before some children met LTNP criteria. Additionally, we applied US norms for a subset of outcome measures given the lack of available local data, and this may have artificially compressed the standardized scores for the Thai and Cambodian children. However, the impact would be minimal as such compression would have applied to all four groups and would be expected to remain consistent over time. Further, the observation of worse cognitive performance in LTNPs and the Progressors compared to the two control groups indicates that the normative approach was sufficient to reveal significant group-level differences. Finally, it is important to note that the two healthy control groups differed from each other and the HIV-infected groups on several socioeconomic variables. Comparisons of outcomes to the HEUs who most closely matched the demographic profiles of the two HIV-infected groups revealed a similar pattern of results to both the full group design and the longitudinal sensitivity analyses, which together provide a strong basis of support for the main study findings.
The present study offered the unique opportunity to model cognitive and emotional health in LTNPs using data acquired prior to the minimum age for LTNP status. Outcomes revealed that cognitive and emotional abnormalities of typical pediatric HIV emerged early in life among LTNPs, were independent of disease progression subtype, and remained persistent over time. The findings emphasize that significant and prolonged immunosuppression is not mandatory for poor cognitive and emotional outcomes in pediatric HIV. Even when CD4 T cell counts are maintained, perinatally infected children experience the same cognitive and emotion/behavioral symptoms of children who meet current classification of progressive disease. Additional studies are needed to identify central drivers of disease progression during the dynamic phases of neurodevelopment in pediatric HIV and opportunities to maximize resilience in this vulnerable population.
Supplementary Material
Acknowledgments
The PREDICT study was sponsored by the National Institute of Allergy and Infectious Disease (NIAID), Grant number U19 AI053741, Clinicaltrial.gov identification number NCT00234091. The follow-up study of PREDICT (Resilience) is funded by the National Institute of Mental Health (5R01MH102151). Antiretroviral drugs for PREDICT were provided by ViiV Healthcare (AZT, 3TC), Boehringer Ingelheim (NVP), Merck (EFV), Abbott (RTV) and Roche (NFV). The neuroimaging and neurodevelopment work were supported by R01MH089722 (Valcour). The PREDICT and Resilience Study Groups
HIV Netherlands Australia Thailand (HIV-NAT) Research Collaboration, Thai Red Cross AIDS Research Center, Bangkok, Thailand; Kiat Ruxrungtham, Jintanat Ananworanich, Thanyawee Puthanakit, Chitsanu Pancharoen, Torsak Bunupuradah, Stephen Kerr, Theshinee Chuenyam, Sasiwimol Ubolyam, Apicha Mahanontharit, Tulathip Suwanlerk, Jintana Intasan, Thidarat Jupimai, Primwichaya Intakan, Tawan Hirunyanulux, Praneet Pinklow, Kanchana Pruksakaew, Oratai Butterworth, Nitiya Chomchey, Chulalak Sriheara, Anuntaya Uanithirat, Sunate Posyauattanakul, Thipsiri Prungsin, Pitch Boonrak, Waraporn Sakornjun, Tanakorn Apornpong, Jiratchaya Sophonphan, Ormrudee Ritim, Nuchapong Noumtong, Noppong Hirunwadee,, Chowalit Phadungphon, Wanchai Thongsee, Orathai Chaiya, Augchara Suwannawat, Threepol Sattong, Niti Wongthai, Kesdao Nantapisan, Umpaporn Methanggool, Narumon Suebsri, Taksin Panpuy, Chayapa Phasomsap, Boonjit Deeaium, Pattiya Jootakarn.
Bamrasnaradura Infectious Diseases Institute, Nonthaburi, Thailand; Jurai Wongsawat, Rujanee Sunthornkachit, Visal Moolasart, Natawan Siripongpreeda, Supeda Thongyen, Piyawadee Chathaisong, Vilaiwan Prommool, Duangmanee Suwannamass, Simakan Waradejwinyoo, Nareopak Boonyarittipat, Thaniya Chiewcharn, Sirirat Likanonsakul, Chatiya Athichathana, Boonchuay Eampokalap, Wattana Sanchiem.
Srinagarind Hospital, Khon Kaen University, Khon Kaen, Thailand; Srinagarind Hospital, Khon Kaen University, Khon Kaen, Thailand; Pope Kosalaraksa, Pagakrong Lumbiganon, Chulapan Engchanil, Piangjit Tharnprisan, Chanasda Sopharak, Viraphong Lulitanond, Samrit Khahmahpahte, Ratthanant Kaewmart, Prajuab Chaimanee, Mathurot Sala, Thaniita Udompanit, Ratchadaporn Wisai, Somjai Rattanamanee, Yingrit Chantarasuk, Sompong Sarvok, Yotsombat Changtrakun, Soontorn Kunhasura, Sudthanom Kamollert.
Queen Savang Vadhana Memorial Hospital, Chonburi, Thailand; Wicharn Luesomboon, Dr. Pairuch Eiamapichart, Dr. Tanate Jadwattanakul, Isara Limpetngam, Daovadee Naraporn, Pornpen Mathajittiphun, Chatchadha Sirimaskul, Woranun Klaihong, Pipat Sittisak, Tippawan Wongwian, Kansiri Charoenthammachoke, Pornchai Yodpo.
Nakornping Hospital, Chiang Mai, Thailand; Suparat Kanjanavanit, Maneerat Ananthanavanich, Penpak Sornchai, Thida Namwong, Duangrat Chutima, Suchitra Tangmankhongworakun, Pacharaporn Yingyong, Juree Kasinrerk, Montanee Raksasang, Pimporn Kongdong, Siripim Khampangkome, Suphanphilat Thong-Ngao, Sangwan Paengta, Kasinee Junsom, Ruttana Khuankaew M, Parichat Moolsombat, Duanpen Khuttiwung, Chanannat Chanrin.
Chiangrai Regional Hospital, ChiangRai, Thailand; Rawiwan Hansudewechakul, Yaowalak Jariyapongpaiboon, Chulapong Chanta, Areerat Khonponoi, Chaniporn Yodsuwan, Warunee Srisuk, Pojjavitt Ussawawuthipong, Yupawan Thaweesombat, Polawat Tongsuk, Chaiporn Kumluang, Ruengrit Jinasen, Noodchanee Maneerat, Kajorndej Surapanichadul, Pornpinit Donkaew.
National Pediatric Hospital, Phnom Penh, Cambodia; Saphonn Vonthanak, Ung Vibol, Sam Sophan, Pich Boren, Kea Chettra, Lim Phary, Toun Roeun, Tieng Sunly, Mom Chandara, Chuop Sokheng, Khin Sokoeun, Tuey Sotharin.
Social Health Clinic, Phnom Penh, Cambodia; Saphonn Vonthanak, Ung Vibol, Vannary Bun, Somanythd Chhay Meng,. Kea Chettra, Sam Phan, Wuddhika In vong, Khuon Dyna.
Prapokklao Hospital, Chantaburi, Thailand; Chaiwat Ngampiyaskul, Naowarat Srisawat, Wanna Chamjamrat, Sayamol Wattanayothin, Pornphan Prasertphan, Tanyamon Wongcheeree, Pisut Greetanukroh, Chataporn Imubumroong, Pathanee Teirsonsern.
Research Institute for Health Sciences, Chiang Mai University, Chiang Mai, Thailand; Virat Sirisanthana, Linda Aurpibul, Pannee Visrutaratna, Siriporn Taphey, Tawalchaya Cholecharoentanan, Nongyow Wongnum, Chintana Khamrong, Rassamee Kaewvichit, Kittipong Rungroengthanakit.
Chiang Mai University: Kulvadee Thongpibul
Conflicts of Interest and Sources Funding
Dr. Jintanat Ananworanich has received honoraria from ViIV Healthcare and Merck
Dr. Victor Valcour has received honoraria from ViIV Healthcare
For the remaining authors none were declared
The PREDICT study was sponsored by the National Institute of Allergy and Infectious Disease (NIAID), Grant number U19 AI053741, Clinicaltrial.gov identification number NCT00234091. The follow-up study of PREDICT (Resilience) was funded by the National Institute of Mental Health (5R01MH102151). Antiretroviral drugs for PREDICT were provided by ViIV Healthcare (AZT, 3TC), Boehringer Ingelheim (NVP), Merck (EFV), Abbott (RTV) and Roche (NFV). The neurodevelopment was supported by R01MH089722 (Valcour).
References
- 1.Barnhart HX, Caldwell MB, Thomas P, Mascola L, Ortiz I, Hsu HW, Schulte J, Parrott R, Maldonado Y, Byers R. Pediatric Spectrum of Disease Clinical Consortium. Natural history of human immunodeficiency virus disease in perinatally infected children: an analysis from the Pediatric Spectrum of Disease Project. Pediatrics. 1996 May 1;97(5):710–6. [PubMed] [Google Scholar]
- 2.Blanche S, Newell ML, Mayaux MJ, Dunn DT, Teglas JP, Rouzioux C, Peckham CS. Morbidity and mortality in European children vertically infected by HIV-1: the French Pediatric HIV Infection Study Group and European Collaborative Study. JAIDS Journal of Acquired Immune Deficiency Syndromes. 1997 Apr 15;14(5):442–50. doi: 10.1097/00042560-199704150-00008. [DOI] [PubMed] [Google Scholar]
- 3.Newell ML, Coovadia H, Cortina-Borja M, Rollins N, Gaillard P, Dabis F. Mortality of infected and uninfected infants born to HIV-infected mothers in Africa: a pooled analysis. The Lancet. 2004 Oct 8;364(9441):1236–43. doi: 10.1016/S0140-6736(04)17140-7. [DOI] [PubMed] [Google Scholar]
- 4.Poropatich K, Sullivan DJ., Jr Human immunodeficiency virus type 1 long-term non-progressors: the viral, genetic and immunological basis for disease non-progression. Journal of General Virology. 2011 Feb 1;92(2):247–68. doi: 10.1099/vir.0.027102-0. [DOI] [PubMed] [Google Scholar]
- 5.Warszawski J, Lechenadec J, Faye A, Dollfus C, Firtion G, Meyer L, Douard D, Monpoux F, Tricoire J, Benmebarek Y, Rouzioux C. Long-term nonprogression of HIV infection in children: evaluation of the ANRS prospective French Pediatric Cohort. Clinical Infectious Diseases. 2007 Sep 15;45(6):785–94. doi: 10.1086/521165. [DOI] [PubMed] [Google Scholar]
- 6.Ananworanich J, Apornpong T, Kosalaraksa P, Jaimulwong T, Hansudewechakul R, Pancharoen C, Bunupuradah T, Chandara M, Puthanakit T, Ngampiyasakul C, Wongsawat J. Characteristics of lymphocyte subsets in HIV-infected, long-term nonprogressor, and healthy Asian children through 12 years of age. Journal of Allergy and Clinical Immunology. 2010 Dec 31;126(6):1294–301. doi: 10.1016/j.jaci.2010.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Romiti ML, Colognesi C, Cancrini C, Mas A, Berrino M, Salvatori F, Orlandi P, Jansson M, Palomba E, Plebani A, Bertran JM. Prognostic value of a CCR5 defective allele in pediatric HIV-1 infection. Molecular Medicine. 2000 Jan;6(1):28. [PMC free article] [PubMed] [Google Scholar]
- 8.Corró G, Rocco CA, De Candia C, Catano G, Turk G, Mangano A, Aulicino PC, Bologna R, Sen L. Genetic and functional analysis of HIV type 1 nef gene derived from long-term nonprogressor children: association of attenuated variants with slow progression to pediatric AIDS. AIDS research and Human Retroviruses. 2012 Dec 1;28(12):1617–26. doi: 10.1089/AID.2012.0020. [DOI] [PubMed] [Google Scholar]
- 9.Corró G, Crudeli CM, Rocco CA, Marino SA, Sen L. High levels of anti-Nef antibodies may prevent AIDS disease progression in vertically HIV-1-infected infants. Journal of the International AIDS Society. 2014;17(1) doi: 10.7448/IAS.17.1.18790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harrer T, Harrer E, Kalams SA, Barbosa P, Trocha A, Johnson RP, Elbeik T, Feinberg MB, Buchbinder SP, Walker BD. Cytotoxic T lymphocytes in asymptomatic long-term nonprogressing HIV-1 infection. Breadth and specificity of the response and relation to in vivo viral quasispecies in a person with prolonged infection and low viral load. The Journal of Immunology. 1996 Apr 1;156(7):2616–23. [PubMed] [Google Scholar]
- 11.Paul ME, Mao C, Charurat M, Serchuck L, Foca M, Hayani K, Handelsman EL, Diaz C, McIntosh K, Shearer WT. Predictors of immunologic long-term nonprogression in HIV-infected children: implications for initiating therapy. Journal of Allergy and Clinical Immunology. 2005 Apr 30;115(4):848–55. doi: 10.1016/j.jaci.2004.11.054. [DOI] [PubMed] [Google Scholar]
- 12.Muenchhoff M, Adland E, Karimanzira O, Crowther C, Pace M, Csala A, Leitman E, Moonsamy A, McGregor C, Hurst J, Groll A. Nonprogressing HIV-infected children share fundamental immunological features of nonpathogenic SIV infection. Science Translational Medicine. 2016 Sep 28;8(358):358ra125-. doi: 10.1126/scitranslmed.aag1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wachsler-Felder JL, Golden CJ. Neuropsychological consequences of HIV in children: a review of current literature. Clinical psychology review. 2002 Apr 30;22(3):441–62. doi: 10.1016/s0272-7358(01)00108-8. [DOI] [PubMed] [Google Scholar]
- 14.Blanchette N, Smith ML, King S, Fernandes-Penney A, Read S. Cognitive development in school-age children with vertically transmitted HIV infection. Developmental neuropsychology. 2002 Jun 1;21(3):223–41. doi: 10.1207/S15326942DN2103_1. [DOI] [PubMed] [Google Scholar]
- 15.Nozyce ML, Lee SS, Wiznia A, Nachman S, Mofenson LM, Smith ME, Yogev R, McIntosh K, Stanley K, Pelton S. A behavioral and cognitive profile of clinically stable HIV-infected children. Pediatrics. 2006 Mar 1;117(3):763–70. doi: 10.1542/peds.2005-0451. [DOI] [PubMed] [Google Scholar]
- 16.Jeremy RJ, Kim S, Nozyce M, Nachman S, McIntosh K, Pelton SI, Yogev R, Wiznia A, Johnson GM, Krogstad P, Stanley K. Neuropsychological functioning and viral load in stable antiretroviral therapy-experienced HIV-infected children. Pediatrics. 2005 Feb 1;115(2):380–7. doi: 10.1542/peds.2004-1108. [DOI] [PubMed] [Google Scholar]
- 17.Shanbhag MC, Rutstein RM, Zaoutis T, Zhao H, Chao D, Radcliffe J. Neurocognitive functioning in pediatric human immunodeficiency virus infection: effects of combined therapy. Archives of Pediatrics & Adolescent Medicine. 2005 Jul 1;159(7):651–6. doi: 10.1001/archpedi.159.7.651. [DOI] [PubMed] [Google Scholar]
- 18.Blanchette N, Lou M, Fernandes-Penney A, King S, Read S. Cognitive and motor development in children with vertically transmitted HIV infection. Brain and Cognition. 2001 Jul 31;46(1):50–3. doi: 10.1016/s0278-2626(01)80032-4. [DOI] [PubMed] [Google Scholar]
- 19.Bagenda D, Nassali A, Kalyesubula I, Sherman B, Drotar D, Boivin MJ, Olness K. Health, neurologic, and cognitive status of HIV-infected, long-surviving, and antiretroviral-naive Ugandan children. Pediatrics. 2006 Mar 1;117(3):729–40. doi: 10.1542/peds.2004-2699. [DOI] [PubMed] [Google Scholar]
- 20.Smith R, Malee K, Leighty R, Brouwers P, Mellins C, Hittelman J, Chase C, Blasini I. Effects of perinatal HIV infection and associated risk factors on cognitive development among young children. Pediatrics. 2006 Mar 1;117(3):851–62. doi: 10.1542/peds.2005-0804. [DOI] [PubMed] [Google Scholar]
- 21.Linn K, Fay A, Meddles K, Isbell S, Lin PN, Thair C, Heaps J, Paul R, Mar SS. HIV-related cognitive impairment of orphans in Myanmar with vertically transmitted HIV taking antiretroviral therapy. Pediatric Neurology. 2015 Dec 31;53(6):485–90. doi: 10.1016/j.pediatrneurol.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 22.Martin SC, Wolters PL, Toledo-Tamula MA, Zeichner SL, Hazra R, Civitello L. Cognitive functioning in school-aged children with vertically acquired HIV infection being treated with highly active antiretroviral therapy (HAART) Developmental Neuropsychology. 2006 Oct 1;30(2):633–57. doi: 10.1207/s15326942dn3002_1. [DOI] [PubMed] [Google Scholar]
- 23.Mellins CA, Levenson RL, Zawadzki R, Kairam R, Wetson M. Effects of pediatric HIV infection and prenatal drug exposure on mental and psychomotor development. Journal of Pediatric Psychology. 1994 Oct 1;19(5):617–28. doi: 10.1093/jpepsy/19.5.617. [DOI] [PubMed] [Google Scholar]
- 24.Malee KM, Tassiopoulos K, Huo Y, Siberry G, Williams PL, Hazra R, Smith RA, Allison SM, Garvie PA, Kammerer B, Kapetanovic S. Mental health functioning among children and adolescents with perinatal HIV infection and perinatal HIV exposure. AIDS Care. 2011 Dec 1;23(12):1533–44. doi: 10.1080/09540121.2011.575120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mellins CA, Smith R, O’Driscoll P, Magder LS, Brouwers P, Chase C, Blasini I, Hittleman J, Llorente A, Matzen E. High rates of behavioral problems in perinatally HIV-infected children are not linked to HIV disease. Pediatrics. 2003 Feb 1;111(2):384–93. doi: 10.1542/peds.111.2.384. [DOI] [PubMed] [Google Scholar]
- 26.Hoare J, Fouche JP, Spottiswoode B, Donald K, Philipps N, Bezuidenhout H, Mulligan C, Webster V, Oduro C, Schrieff L, Paul R. A diffusion tensor imaging and neurocognitive study of HIV-positive children who are HAART-naïve “slow progressors”. Journal of Neurovirology. 2012 Jun 1;18(3):205–12. doi: 10.1007/s13365-012-0099-9. [DOI] [PubMed] [Google Scholar]
- 27.Hoare J, Fouche JP, Phillips N, Joska JA, Paul R, Donald KA, Thomas KG, Stein DJ. White matter micro-structural changes in ART-naive and ART-treated children and adolescents infected with HIV in South Africa. Aids. 2015 Sep 10;29(14):1793–801. doi: 10.1097/QAD.0000000000000766. [DOI] [PubMed] [Google Scholar]
- 28.Puthanakit T, Saphonn V, Ananworanich J, Kosalaraksa P, Hansudewechakul R, Vibol U, Kerr SJ, Kanjanavanit S, Ngampiyaskul C, Wongsawat J, Luesomboon W. Early versus deferred antiretroviral therapy for children older than 1 year infected with HIV (PREDICT): a multicentre, randomised, open-label trial. The Lancet Infectious Diseases. 2012 Dec 31;12(12):933–41. doi: 10.1016/S1473-3099(12)70242-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Llorente AM, Williams J, Satz P, D’Elia LF. Children’s color trails test (CCTT) Odessa, Florida: Psychological Assessment Resources; 2003. [Google Scholar]
- 30.Beery KE. Visual-motor integration: Monograph. Modern Curriculum Press; 1967. [Google Scholar]
- 31.Tiffin J. Purdue pegboard examiner manual. Science Research Associates; 1968. [Google Scholar]
- 32.Channarong P, Watanasopon J, Veachvirool C. Development of Intelligence Test WISC-III Thai edition. Bangkok; Thailand: 2003. [Google Scholar]
- 33.Auchenbach TM, Rescorla LA. Manual for the ASEBA School-Age forms and Profiles. Burlington VT: University of Vermont Research Center for Children, Youth and Families; 2001. [Google Scholar]
- 34.Ananworanich J, Jupimai T, Mekmullica J, Sosothikul D, Pancharoen C. Behavioral and emotional problems in Thai children with HIV infection compared to children with and without other chronic diseases. Journal of the International Association of Physicians in AIDS Care (JIAPAC) 2008 Jan 1;7(1):52–3. doi: 10.1177/1545109707305173. [DOI] [PubMed] [Google Scholar]
- 35.Kerr SJ, Puthanakit T, Vibol U, Aurpibul L, Vonthanak S, Kosalaraksa P, Kanjanavanit S, Hansudewechakul R, Wongsawat J, Luesomboon W, Ratanadilok K. Neurodevelopmental outcomes in HIV-exposed-uninfected children versus those not exposed to HIV. AIDS care. 2014 Nov 2;26(11):1327–35. doi: 10.1080/09540121.2014.920949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Louw KA, Ipser J, Phillips N, Hoare J. Correlates of emotional and behavioural problems in children with perinatally acquired HIV in Cape Town, South Africa. AIDS care. 2016 Jul 2;28(7):842–50. doi: 10.1080/09540121.2016.1140892. [DOI] [PubMed] [Google Scholar]
- 37.Statacorp. College Station, TX, USA: [Google Scholar]
- 38.Ruel TD, Boivin MJ, Boal HE, Bangirana P, Charlebois E, Havlir DV, Rosenthal PJ, Dorsey G, Achan J, Akello C, Kamya MR. Neurocognitive and motor deficits in HIV-infected Ugandan children with high CD4 cell counts. Clinical Infectious Diseases. 2012 Apr 1;54(7):1001–9. doi: 10.1093/cid/cir1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Laughton B, Cornell M, Grove D, Kidd M, Springer PE, Dobbels PE, Cotton MF. Early antiretroviral therapy improves neurodevelopmental outcomes in infants. AIDS. 2012;26(13):1685–1690. doi: 10.1097/QAD.0b013e328355d0ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Burdo TH, Weiffenbach A, Woods SP, Letendre S, Ellis RJ, Williams KC. Elevated sCD163 in plasma but not cerebrospinal fluid is a marker of neurocognitive impairment in HIV infection. AIDS (London, England) 2013 Jun 1;27(9) doi: 10.1097/QAD.0b013e32836010bd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Williams K, Burdo TH. Monocyte mobilization, activation markers, and unique macrophage populations in the brain: observations from SIV infected monkeys are informative with regard to pathogenic mechanisms of HIV infection in humans. Journal of Neuroimmune Pharmacology. 2012 Jun 1;7(2):363–71. doi: 10.1007/s11481-011-9330-3. sc163. [DOI] [PubMed] [Google Scholar]
- 42.Valcour VG, Ananworanich J, Agsalda M, Sailasuta N, Chalermchai T, Schuetz A, Shikuma C, Liang CY, Jirajariyavej S, Sithinamsuwan P, Tipsuk S. HIV DNA reservoir increases risk for cognitive disorders in cART-naive patients. PloS One. 2013 Jul 31;8(7):e70164. doi: 10.1371/journal.pone.0070164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ananworanich J, Kerr SJ, Jaimulwong T, Vibol U, Hansudewechakul R, Kosalaraksa P, Ngampiyaskul C, Kanjanavanit S, Wongsawat J, Luesomboon W, Apornpong T. Soluble CD163 and monocyte populations in response to antiretroviral therapy and in relationship with neuropsychological testing among HIV-infected children. Journal of Virus Eradication. 2015;1(3):196. doi: 10.1016/S2055-6640(20)30501-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Royal W, III, Cherner M, Burdo TH, Umlauf A, Letendre SL, Jumare J, Abimiku AL, Alabi P, Alkali N, Bwala S, Okwuasaba K. Associations between cognition, gender and monocyte activation among HIV infected individuals in Nigeria. PloS One. 2016 Feb 1;11(2):e0147182. doi: 10.1371/journal.pone.0147182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pereyra F, Addo MM, Kaufmann DE, Liu Y, Miura T, Rathod A, Baker B, Trocha A, Rosenberg R, Mackey E, Ueda P. Genetic and immunologic heterogeneity among persons who control HIV infection in the absence of therapy. Journal of Infectious Diseases. 2008 Feb 15;197(4):563–71. doi: 10.1086/526786. [DOI] [PubMed] [Google Scholar]
- 46.Adland E, Paioni P, Thobakgale C, Laker L, Mori L, Muenchhoff M, Csala A, Clapson M, Flynn J, Novelli V, Hurst J. Discordant impact of HLA on viral replicative capacity and disease progression in pediatric and adult HIV infection. PLoS Pathog. 2015 Jun 15;11(6):e1004954. doi: 10.1371/journal.ppat.1004954. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.