Abstract
Purpose of Review
To discuss the clinical significance of the most common hip and groin injuries in baseball players, as well as an algorithmic approach to diagnosis and treatment of these injuries.
Recent Findings
(a) Limitations in throwing velocity, pitch control, and bat swing speed may be secondary to decreased mobility and strength within the proximal kinetic chain, which must harness power from the lower extremities and core. (b) Approximately 5.5% of all baseball injuries per year involve the hip/groin and may lead to a significant amount of time spent on the disabled list.
Summary
Injuries involving the hip and groin are relatively common in baseball players. Our knowledge of the mechanics of overhead throwing continues to evolve, as does our understanding of the contribution of power from the lower extremities and core. It is paramount that the team physician be able to accurately diagnose and treat injuries involving the hip/groin, as they may lead to significant disability and inability to return to elite levels of play. This review focuses on hip- and groin-related injuries in the baseball player, including femoroacetabular impingement, core muscle injury, and osteitis pubis.
Keywords: Hip arthroscopy, Femoroacetabular impingement, FAI, Athletic pubalgia, Core muscle injury, Osteitis pubis
Introduction
The overhead throwing athlete must harness a complex transfer of energy which utilizes the entire kinetic chain, requiring muscle activation and sequencing through the lower extremities to the core and trunk to propagate the transfer of power to the upper extremity [1, 2]. With repetitive throwing, this transfer of power and subsequent dynamic overload to the upper extremity may cause injury in baseball players, often presenting with shoulder and elbow injuries [3, 4]. More recent focus on upstream kinetic chain mechanics has suggested that limited mobility, strength, or conditioning at any point within the kinetic chain can impact the athlete’s throwing performance [5•, 6–9]. Similarly, while batting, a player first leads with a step to transfer rotational power through the lower extremity into the core/trunk and lastly into the upper extremities, culminating in maximal swing velocity [10]. Thus, repetitive throwing or batting in an athlete with upstream kinetic chain deficits may lead to increased stress and dynamic overload of the pelvic girdle, consequently leading to injuries of the hip and groin. Posner et al. delineated an increasing incidence of injury among professional baseball players from 2002 to 2008, with approximately 43% of these injuries involving the lower extremity, spine, or core [11]. Coleman et al. further determined that approximately 5.5% of the 33,623 recorded injuries in the major (MLB) and minor (MiLB) leagues from 2011 to 2014 involved the hip or groin [12•]. With these injuries often demanding a significant amount of time spent on the disabled list, accurate diagnosis and effective injury prevention or treatment is of utmost importance.
Proper throwing mechanics require adequate trunk and core rotation to generate velocity and control. Intra- and extra-articular hip pathology can cause mechanical limitations and/or arthrogenic pain inhibition, which can limit the downstream kinetic chain and thus affect performance. The differential diagnosis for hip and groin pain in the athlete is vast, with common diagnoses found in Table 1. This review will present the clinical and radiographic approach to diagnosis and treatment for the most common hip and groin injuries in the baseball player, including femoroacetabular impingement (FAI), core muscle injury, and osteitis pubis.
Table 1.
Common intra- and extra-articular causes of hip/groin pain
| Intra-articular | Extra-articular | |
|---|---|---|
| Femoroacetabular impingement | Contusion | Greater trochanteric bursitis |
| Dysplasia | Adductor strain | Piriformis syndrome |
| Labral tear | Core muscle injury (Ath Pub) | Ischiofemoral impingement |
| Capsulitis | Iliopsoas strain | Nerve entrapment |
| Chondral damage | Gluteus max/med/min strain | Sacroiliac joint pathology |
| Loose body | IT band syndrome | Osteitis pubis |
| Capsular laxity | Lumbar-referred pain | Stress fracture |
Clinical Examination
Patients with hip and/or groin pain can be challenging to accurately diagnose. They often present with a myriad of vague clinical symptoms and there rarely is a pathognomonic finding. When faced with differentiating the diagnosis of an athlete’s hip/groin pain, it is often helpful to use the layered approach concept, described by Poultsides et al. [13]. This concept defines layer 1 as the osteochondral layer, which delineates the individual’s joint congruence and osteoarticular kinematics. Building upon this is layer 2, the inert layer, which includes the labrum, capsule, and ligamentous complex of the hip, all of which act as static stabilizers of the hip. Layer 3 is the contractile layer, including the 27 periarticular muscles functioning in dynamic stabilization of the hip. Lastly, layer 4 is the neuromechanical layer, which includes the thoracolumbosacral plexuses as well as the lumbopelvic structures, which function as a neuromuscular link to maintain functional control of the limb segment as it tasks within its environment.
As with any patient presenting with a chief complaint of hip/groin pain, a thorough history and physical examination should be performed. However, specific to baseball athletes, it is often helpful to evaluate the player’s throwing mechanics, fielding posture, and batting stance, as these may elucidate further contributory elements of information. A complete history should be investigated including any suggestion of slipped capital femoral epiphysis, Legg-Calvé-Perthes disease, developmental dysplasia of the hip, or remote trauma, as these may be contributory to an incongruence of the femoroacetabular articulation. It is important to delineate the timing, character, onset, precipitating factors, and associated findings of the injury presentation. Hip or groin pain can be secondary to acute trauma (stress reaction/fracture or tendon avulsion/tear), and these injuries are more likely to present with focal symptoms and associated muscle cramping or spasms. More commonly however, athletic groin pain presents insidiously, often secondary to the athlete’s increased physiologic demands exceeding their functional capabilities. Mechanical symptoms of clicking, catching, locking, or the sensation of subluxation/instability are suggestive of an intra-articular pathology. The location of intra-articular pain is classically demonstrated by the C-sign, when a patient will cup their hand around their anterior and lateral aspect of their hip, just proximal to their greater trochanter [14]. Radiating pain associated with concomitant neurologic symptoms is suggestive of a lumbosacral origin.
Complete physical examination of the athlete should be performed, with special focus on gait, posture, batting/pitching mechanics, range of motion, and strength of the spine, trunk/core, and lower extremities, as well as focused provocative maneuver testing. An examination similar to those described by Trofa et al. and Martin et al. is performed with the patient in five different positions [15, 16]. Li et al. recently demonstrated a correlation between reduced total hip rotation arc and lower extremity injuries about the hip, further determining a correlation with decreased internal rotation and in-season hip, hamstring, and groin injuries in MLB players [9]. Thorough strength testing should be performed and compared to the contralateral side, with a particular focus on lumbar/core, hip abduction, hip adduction, and hip flexion/extension. Too often is an athlete’s strength assumed to be normal given their level of competition, but in actuality they have objective weakness on examination of the periarticular musculature, given fatigue failure of their compensatory mechanism secondary to their pathologic injury. Specific provocative testing should include the anterior, lateral, and posterior impingement tests, FADIR (flexion, adduction, and internal rotation) and FABER (flexion, abduction, and external rotation), the Stinchfield test, the McCarthy test, the lateral compression symphysis test, and resisted hip abduction/adduction and combined with resisted crunch testing [15, 17, 18]. Palpation of bony prominences (anterior superior iliac spine, pubic symphysis, greater trochanter, ischial tuberosity) can elicit pain suggestive of pathology. A complete neurovascular examination should be performed of the core/trunk and lower extremities, as neuromuscular concomitant dysfunction and nerve entrapment pathologies (meralgia paresthetica, deep gluteal syndrome, etc.) are relatively common about the hip/groin [19, 20].
Femoroacetabular Impingement
First described in 2003, FAI is now recognized as the most common cause of dynamic intra-articular hip pain, resulting from abnormal pathologic engagement of the proximal femoral head-neck junction and the acetabular rim at terminal ranges of motion [21]. Traditionally described as either cam-type or pincer-type impingement, FAI is most commonly caused by a combination of the two pathologies [22]. Furthermore, our understanding of the contributions of subtle deformities of the proximal femur and acetabulum to dynamic impingement continues to evolve [23].
Cam-type deformity (Fig. 1) refers to an aspherical femoral head with loss of femoral head-neck offset, resulting in abutment of the femoral neck with the acetabular rim. This is an inclusion-type pathology, which can result in microtrauma of the chondrolabral junction and subsequent anterosuperior cartilage delamination with repetitive flexion, adduction, and internal rotation of the hip. The cam-type morphology of the proximal femur is relatively common in the asymptomatic general population, and even more common in the athletic population. Many hypotheses have been formed aiming to elucidate the origins of its development, and most recently, Siebenrock et al. have suggested an association between cam-type morphology development and high-intensity athletic activities during the critical growth phase of adolescence [24•]. Genetic and developmental factors may put the athletic population at increased risk for cam-type morphology and symptomatic femoroacetabular impingement.
Fig. 1.
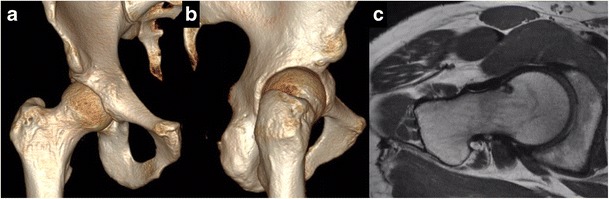
Predominant cam-type FAI of the right hip in 18-year-old pitcher with hip pain. (A) 3D CT scan with cam lesion located from 1:30–3:00, alpha angle of 64° and reduced femoral anteversion of 5°. (B) Reveals a Type-II AIIS. (C) Axial proton density MRI of the right hip reveals impingement cyst along anterior femoral head-neck junction at approximately 2:00
Pincer-type deformity (Fig. 2) results from acetabular-sided overcoverage, which results in focal linear contact between the rim and the proximal femur. This type of overcoverage may rarely be secondary to global acetabular retroversion, but it is more commonly caused by a focal anterosuperior retroversion. With flexion, adduction, and internal rotation of the femur, premature contact of the acetabular rim and femur occurs, resulting in impaction of the interposed labrum. This may result in premature degeneration and subsequent ossification of the labrum, further worsening the relative overcoverage. Continued impingement may lead to leverage of the femoral head-neck junction on the pincer-type rim, leading to increased shearing forces of the posteroinferior cartilage and a contrecoup pattern of injury [25].
Fig. 2.
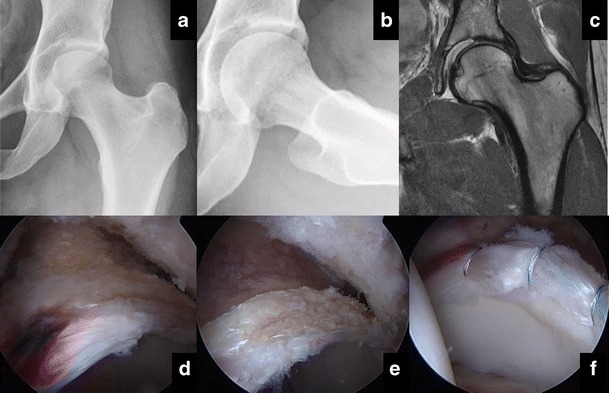
Predominant pincer-type FAI of the left hip in a 19-year-old catcher with hip pain. (A) AP and (B) Dunn-45° lateral XR revealing pincer deformity, negative Tӧnnis angle. (C) Anterosuperior labral tear with acetabular subchondral overload sclerosis but maintained cartilage. (D) Arthroscopic view of significant subspine and pincer deformities with hyperemic labrum and associated tear. (E) Acetabulum after pincer/subspine resection and (F) labral refixation
Extra-articular impingement between the anterior inferior iliac spine (AIIS) and the proximal femur is also a common concomitant pathology seen in patients with FAI [26]. Athletes are especially prone to development of AIIS subspine impingement secondary to avulsions or traction apophysitis of the direct head origin of the rectus femoris tendon [27]. Repetitive hip flexion during high-demand athletics requiring cutting, pivoting, sprinting, and kicking is theorized to result in hypertrophy of the AIIS, and thus a morphology consistent with potential pathologic impingement with the proximal femur during deep flexion activities.
Patients typically present with a history of “hip flexor tightness,” complaints of hip stiffness, reduced range of motion, and insidious anterior/lateral groin pain with prolonged sitting or deep-flexion activities. They may also note mechanical symptoms with associated sharp pain and/or relief from a palpable or audible snapping. Patients with FAI have restricted internal rotation (< 20°) when the hip is flexed to 90°. Provocative FADIR testing will be positive, and anterior impingement from deep flexion alone is suggestive of an ASIS subspine impingement component. Diagnostic imaging should include plain radiographs and 3-dimensional computed tomography scans to evaluate the bony anatomy and characterize the patient’s severity of impingement. An MRI should be obtained to evaluate the soft tissues about the hip, including the labrum and articular cartilage. Image-guided intra-articular injection can be used to differentiate intra- and extra-articular sources of hip/groin pain if necessary.
While femoroacetabular impingement is not unique to baseball players, it is the most common cause of diagnosed intra-articular hip/groin pain. Coleman et al. found that FAI was the cause of 47.6% MLB and MiLB players diagnosed with intra-articular hip/groin pain [12•]. Furthermore, its importance in contribution to extra-articular concomitant injuries cannot be overstated. Femoroacetabular impingement, whether cam- or pincer- or mixed-type morphology, causes a mechanical limitation to functional range of motion. When an elite-level athlete’s functional range of motion exceeds the physiologic range of motion limitations defined by their bony hip morphology, compensatory motion through the lumbar spine, sacroiliac joints, pubic symphysis, core/trunk, and peri-hip musculature can often accommodate to meet the athlete’s needs. However, these compensatory mechanisms put increased strain on each individual link within the kinetic chain, and often these functional demands exceed the physiologic limitation, thus leading to injury.
Non-operative treatment for FAI includes maximizing the mobility and strength of the adjacent segments within the kinetic chain to alleviate the limited range of motion within the hip. Oral or intra-articular medications can be used to facilitate pain relief and anti-inflammatory modalities to enable the athlete to improve strength deficits through physical therapy. Specifically, athletes can strengthen their lumbar and core musculature to increase their lumbar lordosis, thus functionally improving their acetabular anteversion in a standing position. If non-surgical treatment fails, operative management of FAI can be done with open or arthroscopic techniques. Advancements in both our understanding of the disease process and the surgical instrumentation have enabled surgeons to address most cases of FAI arthroscopically. Open surgical dislocation can be utilized to treat cases requiring articular cartilage transplantation, labral reconstruction, global rim resection (protrusio/profunda), or posterior extension of cam-type impingement. An arthroscopic approach is preferred to treat cam- and pincer-type impingement and repair labral pathology to facilitate a safe, timely return to sport (Fig. 3). Byrd et al. recently reported his mid-term results (average follow-up 45 months) of 41 intercollegiate or professional baseball players undergoing hip arthroscopy for treatment of FAI [28]. Ninety percent of these athletes returned to their previous level of competition at a mean of 4.3 months with no complications, but three players required revision hip arthroscopy. Similarly, Klingenstein et al. reported their results of 16 high-level baseball players undergoing arthroscopic treatment for FAI [29]. All 16 athletes were able to return to their previous level of competition at 12-month follow-up with no complications or revision surgery reported.
Fig. 3.
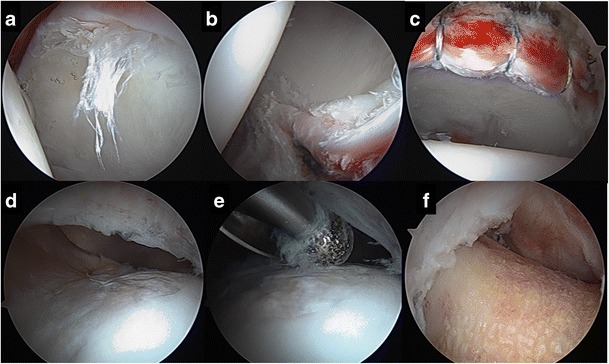
Arthroscopic images of 28-year-old pitcher with right hip pain and predominantly cam-type FAI with (A) significant anterosuperior chondral delamination and hyperemic labral injury. (B) Posterolateral contrecoup injury. (C) Stable hyperemic labrum after subspine decompression and labral refixation. (D) Anterosuperior cam lesion was resected (E) with a high-speed bur to restore the sphericity of the femoral head and concavity of the head-neck junction (F)
Core Muscle Injury
Historically termed “Gilmore’s groin,” this complex injury pattern involving the abdominal and pelvic musculature is more commonly referred to as “athletic pubalgia” or “sports hernia” [30]. However, confusion among the medical community and public alike has led to a more accurate and representative term, “core muscle injury” to describe this injury [31, 32]. Core muscle injury is hypothesized to result from an insult to the posterior inguinal wall secondary to rotational shear forces at the pubic symphyseal combined insertion of the rectus abdominis and adductor longus. Repetitive trunk hyperextension, hip hyperabduction, and core rotation can lead to weakening or tearing of the soft-tissue envelope. Patients often present with unilateral or bilateral lower abdominal pain that radiates to the groin and perineum when engaging the core or hip adductors. Referred pain secondary to inflammatory irritation or entrapment of the iliohypogastric, ilioinguinal, and genitofemoral nerves can occur. Classically, however, the athlete will have difficulty performing at their elite level secondary to this constellation of symptoms, but experience resolution of symptoms with inactivity. On physical examination, their symptoms can often be reproduced with resisted crunch testing (the player is supine with knees bent, performing resisted hip adduction, while performing a resisted partial sit-up). This maneuver maximally strains the combined insertion on the pubic symphysis and reproduction of symptoms is consistent with a positive diagnosis.
Advancement of dedicated non-contrast MRI protocols have enabled 68% sensitivity and 100% specificity for diagnosis of core muscle injury when compared to intra-operative findings [33]. Typically, the MRI will reveal a curvilinear cleft sign just along the medial pubic symphysis at the rectus abdominis-adductor longus aponeurosis (Fig. 4), suggestive of injury when combined with a consistent history and physical examination [31]. However, similar findings in asymptomatic athletes are relatively common and therefore should be interpreted within the context of the patient’s history and physical examination. For diagnostic and potentially therapeutic purpose, an image-guided injection of local anesthetic and corticosteroid can be performed; however, there is currently limited evidence for non-operative treatment with platelet-rich plasma [34].
Fig. 4.

Coronal (A) and axial (B) MRI in a 21-year-old infielder with hip/groin pain reveals hyperintensity at insertion of left rectus abdominus (white arrows) consistent with left core muscle injury. Normal signal found within contralateral muscle belly (green star)
Coleman et al. determined 1.8% of all hip and groin injuries categorized by the MiLB and MLB players from 2011 to 2014 which were consistent with core muscle injury [12•]. These injuries are first approached with rest, activity modification, and non-surgical treatment. This is followed by dedicated physical therapy focusing on core strengthening, trunk stabilization, postural training, batting/throwing mechanics, and graduated return to sport. If non-surgical management fails to return the athlete to the desired level of activity, surgical management may be considered. Meyers et al. has published the largest series of 8490 athletes treated surgically (6.2% baseball players) [35]. Over a 20-year span, they report 95% of athletes were able to return to sport at 3 months post-operatively. However, it is also important to note the high incidence of concomitant core muscle injury and femoroacetabular impingement. Hammoud et al. reported on 38 consecutive professional athletes (23.6% baseball players), of which 32% (12/38) underwent surgical intervention for core muscle injury alone [36•]. No patient was able to return to sport after this intervention alone, but all 12 patients were able to return to sport after combined core muscle surgery and hip arthroscopy to treat their FAI. This illustrates the importance of recognizing core muscle injury as a possible compensatory injury pattern secondary to FAI and its effects on limited hip range of motion.
Osteitis Pubis
The pubic symphysis is a non-synovial amphiarthrodial joint with an interposed fibrocartilaginous disk. This allows for minimal rotational and translational motion, the stability of which is conveyed by static ligamentous and dynamic musculotendinous components. Like any other joint in the body, increased motion or stress across the articulation can stimulate an inflammatory cascade. This can lead to subchondral bony edema, subchondral cyst formation, and, ultimately, articular erosions [37]. This is akin to a stress reaction of the pubic symphysis from overuse and commonly secondary to increased compensatory motion through the pubic symphysis secondary to limited motion elsewhere within the kinetic chain (lumbopelvis, sacroiliac joint, FAI). Diagnosis of chronic osteitis pubis can be made on radiograph alone, with mixed cystic and sclerotic changes and widening of the pubic symphysis. MRI can be used to diagnose earlier changes, which include periarticular bone marrow edema. Treatment is generally non-surgical with rest, anti-inflammatory medication, activity modification, and gradual return to physical therapy to improve core/trunk muscle dysfunction and improve adjacent segment mobility to decrease stress within the symphysis. If these measures fail, surgical management may include arthroscopic curettage with adductor tenodesis, but evidence is limited and no baseball-specific outcomes are available at the time of this review [38].
Conclusion
Hip and groin injuries are relatively common among baseball players at all levels of competition. A thorough understanding of femoroacetabular biomechanics and its interplay with adjacent segments within the kinetic chain is necessary to differentiate and successfully treat an athlete presenting with hip/groin pain. Often an elite player’s functional muscular envelope is able to overcome or accommodate for limitations to motion within the kinetic chain. However, over time, compensatory mechanisms can fail, resulting in injury as described above. Through a systematic and algorithmic approach, hip and groin injuries in the baseball player may be accurately diagnosed, prevented, and/or effectively treated.
Compliance with Ethical Standards
Conflict of Interest
Both authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Injuries in Overhead Athletes
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Kibler WB, Wilkes T, Sciascia A. Mechanics and pathomechanics in the overhead athlete. Clin Sports Med. 2013;32(4):637–651. doi: 10.1016/j.csm.2013.07.003. [DOI] [PubMed] [Google Scholar]
- 2.Mlynarek RA, Lee S, Bedi A. Shoulder injuries in the overhead throwing athlete. Hand Clin. 2017;33(1):19–34. doi: 10.1016/j.hcl.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 3.Zaremski JL, Wasser JG, Vincent HK. Mechanisms and treatments for shoulder injuries in overhead throwing athletes. Curr Sports Med Rep. 2017;16(3):179–188. doi: 10.1249/JSR.0000000000000361. [DOI] [PubMed] [Google Scholar]
- 4.Ciccotti MG, Pollack KM, Ciccotti MC, D'Angelo J, Ahmad CS, Altchek D, et al. Elbow injuries in professional baseball: epidemiological findings from the Major League Baseball Injury Surveillance System. Am J Sports Med. 2017;45(10):2319–2328. doi: 10.1177/0363546517706964. [DOI] [PubMed] [Google Scholar]
- 5.Chu SK, Jayabalan P, Kibler WB, Press J. The kinetic chain revisited: new concepts on throwing mechanics and injury. PM & R : the journal of injury, function, and rehabilitation. 2016;8(3 Suppl):S69–S77. doi: 10.1016/j.pmrj.2015.11.015. [DOI] [PubMed] [Google Scholar]
- 6.Kibler WB, Kuhn JE, Wilk K, Sciascia A, Moore S, Laudner K, Ellenbecker T, Thigpen C, Uhl T. The disabled throwing shoulder: spectrum of pathology-10-year update. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2013;29(1):141–161. doi: 10.1016/j.arthro.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 7.Wight J, Richards J, Hall S. Influence of pelvis rotation styles on baseball pitching mechanics. Sports Biomech. 2004;3(1):67–83. doi: 10.1080/14763140408522831. [DOI] [PubMed] [Google Scholar]
- 8.Robb AJ, Fleisig G, Wilk K, Macrina L, Bolt B, Pajaczkowski J. Passive ranges of motion of the hips and their relationship with pitching biomechanics and ball velocity in professional baseball pitchers. Am J Sports Med. 2010;38(12):2487–2493. doi: 10.1177/0363546510375535. [DOI] [PubMed] [Google Scholar]
- 9.Li X, Ma R, Zhou H, Thompson M, Dawson C, Nguyen J, Coleman S. Evaluation of hip internal and external rotation range of motion as an injury risk factor for hip, abdominal and groin injuries in professional baseball players. Orthop Rev (Pavia) 2015;7(4):6142. doi: 10.4081/or.2015.6142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Welch CM, Banks SA, Cook FF, Draovitch P. Hitting a baseball: a biomechanical description. The Journal of orthopaedic and sports physical therapy. 1995;22(5):193–201. doi: 10.2519/jospt.1995.22.5.193. [DOI] [PubMed] [Google Scholar]
- 11.Posner M, Cameron KL, Wolf JM, Belmont PJ, Jr, Owens BD. Epidemiology of Major League Baseball injuries. Am J Sports Med. 2011;39(8):1676–1680. doi: 10.1177/0363546511411700. [DOI] [PubMed] [Google Scholar]
- 12.Coleman SH, Mayer SW, Tyson JJ, Pollack KM, Curriero FC. The epidemiology of hip and groin injuries in professional baseball players. Am J Orthop. 2016;45(3):168–175. [PubMed] [Google Scholar]
- 13.Poultsides LA, Bedi A, Kelly BT. An algorithmic approach to mechanical hip pain. HSS J. 2012;8(3):213–224. doi: 10.1007/s11420-012-9304-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Byrd JW. Hip arthroscopy. The Journal of the American Academy of Orthopaedic Surgeons. 2006;14(7):433–444. doi: 10.5435/00124635-200607000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Trofa DP, Mayeux SE, Parisien RL, Ahmad CS, Lynch TS. Mastering the physical examination of the Athlete’s hip. Am J Orthop. 2017;46(1):10–16. [PubMed] [Google Scholar]
- 16.Martin HD, Palmer IJ. History and physical examination of the hip: the basics. Current reviews in musculoskeletal medicine. 2013;6(3):219–225. doi: 10.1007/s12178-013-9175-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Byrd JW. Evaluation of the hip: history and physical examination. N Am J Sports Phys Ther. 2007;2(4):231–240. [PMC free article] [PubMed] [Google Scholar]
- 18.Lynch TS, Bedi A, Larson CM. Athletic hip injuries. The Journal of the American Academy of Orthopaedic Surgeons. 2017;25(4):269–279. doi: 10.5435/JAAOS-D-16-00171. [DOI] [PubMed] [Google Scholar]
- 19.Hernando MF, Cerezal L, Perez-Carro L, Abascal F, Canga A. Deep gluteal syndrome: anatomy, imaging, and management of sciatic nerve entrapments in the subgluteal space. Skelet Radiol. 2015;44(7):919–934. doi: 10.1007/s00256-015-2124-6. [DOI] [PubMed] [Google Scholar]
- 20.Cheatham SW, Kolber MJ, Salamh PA. Meralgia paresthetica: a review of the literature. Int J Sports Phys Ther. 2013;8(6):883–893. [PMC free article] [PubMed] [Google Scholar]
- 21.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 22.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. The Journal of bone and joint surgery British volume. 2005;87(7):1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 23.Nepple JJ, Clohisy JC, Members ASG. Evolution of Femoroacetabular impingement treatment: the ANCHOR experience. Am J Orthop. 2017;46(1):28–34. [PubMed] [Google Scholar]
- 24.Siebenrock KA, Ferner F, Noble PC, Santore RF, Werlen S, Mamisch TC. The cam-type deformity of the proximal femur arises in childhood in response to vigorous sporting activity. Clin Orthop Relat Res. 2011;469(11):3229–3240. doi: 10.1007/s11999-011-1945-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ito K, Leunig M, Ganz R. Histopathologic features of the acetabular labrum in femoroacetabular impingement. Clin Orthop Relat Res. 2004;429:262–271. doi: 10.1097/01.blo.0000144861.11193.17. [DOI] [PubMed] [Google Scholar]
- 26.Hetsroni I, Larson CM, Dela Torre K, Zbeda RM, Magennis E, Kelly BT. Anterior inferior iliac spine deformity as an extra-articular source for hip impingement: a series of 10 patients treated with arthroscopic decompression. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2012;28(11):1644–1653. doi: 10.1016/j.arthro.2012.05.882. [DOI] [PubMed] [Google Scholar]
- 27.Ryan JM, Harris JD, Graham WC, Virk SS, Ellis TJ. Origin of the direct and reflected head of the rectus femoris: an anatomic study. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2014;30(7):796–802. doi: 10.1016/j.arthro.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 28.Byrd JW, Jones KS. Hip arthroscopy in high-level baseball players. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2015;31(8):1507–1510. doi: 10.1016/j.arthro.2015.03.002. [DOI] [PubMed] [Google Scholar]
- 29.Klingenstein GG, Martin R, Kivlan B, Kelly BT. Hip injuries in the overhead athlete. Clin Orthop Relat Res. 2012;470(6):1579–1585. doi: 10.1007/s11999-012-2245-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gilmore O. Gilmore’s Groin. Sports Med Soft Tissue Trauma. 1992;3(3).
- 31.Palisch A, Zoga AC, Meyers WC. Imaging of athletic pubalgia and core muscle injuries: clinical and therapeutic correlations. Clin Sports Med. 2013;32(3):427–447. doi: 10.1016/j.csm.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 32.Knapik DM, Gebhart JJ, Nho SJ, Tanenbaum JE, Voos JE, Salata MJ. Prevalence of surgical repair for athletic pubalgia and impact on performance in football athletes participating in the National Football League Combine. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2017;33(5):1044–1049. doi: 10.1016/j.arthro.2017.01.024. [DOI] [PubMed] [Google Scholar]
- 33.Zoga AC, Kavanagh EC, Omar IM, Morrison WB, Koulouris G, Lopez H, Chaabra A, Domesek J, Meyers WC. Athletic pubalgia and the “sports hernia”: MR imaging findings. Radiology. 2008;247(3):797–807. doi: 10.1148/radiol.2473070049. [DOI] [PubMed] [Google Scholar]
- 34.McCarthy E, Hegazi TM, Zoga AC, Morrison WB, Meyers WC, Poor AE, Nevalainen MT, Roedl JB. Ultrasound-guided interventions for core and hip injuries in athletes. Radiol Clin N Am. 2016;54(5):875–892. doi: 10.1016/j.rcl.2016.04.008. [DOI] [PubMed] [Google Scholar]
- 35.Meyers WC, McKechnie A, Philippon MJ, Horner MA, Zoga AC, Devon ON. Experience with “sports hernia” spanning two decades. Ann Surg. 2008;248(4):656–665. doi: 10.1097/SLA.0b013e318187a770. [DOI] [PubMed] [Google Scholar]
- 36.Hammoud S, Bedi A, Magennis E, Meyers WC, Kelly BT. High incidence of athletic pubalgia symptoms in professional athletes with symptomatic femoroacetabular impingement. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2012;28(10):1388–1395. doi: 10.1016/j.arthro.2012.02.024. [DOI] [PubMed] [Google Scholar]
- 37.Gaudino F, Spira D, Bangert Y, Ott H, Beomonte Zobel B, Kauczor HU, Weber MA. Osteitis pubis in professional football players: MRI findings and correlation with clinical outcome. Eur J Radiol. 2017;94:46–52. doi: 10.1016/j.ejrad.2017.07.009. [DOI] [PubMed] [Google Scholar]
- 38.Hopp SJ, Culemann U, Kelm J, Pohlemann T, Pizanis A. Osteitis pubis and adductor tendinopathy in athletes: a novel arthroscopic pubic symphysis curettage and adductor reattachment. Arch Orthop Trauma Surg. 2013;133(7):1003–1009. doi: 10.1007/s00402-013-1777-7. [DOI] [PubMed] [Google Scholar]


