Abstract
Purpose of Review
This review aims to describe the nonreconstructive options for treating ulnar collateral ligament (UCL) injuries ranging from nonoperative measures, including physical therapy and biologic injections, to ligament repair with and without augmentation.
Recent Findings
Nonoperative options for UCL injuries include guided physical therapy and biologic augmentation with platelet-rich plasma (PRP). In some patients, repair of the UCL has shown promising return to sport rates by using modern suture and suture anchor techniques. Proximal avulsion injuries have shown the best results after repair. Currently, there is growing interest in augmentation of UCL repair with an internal brace.
Summary
The treatment of UCL injuries involves complex decision making. UCL reconstruction remains the gold standard for attritional injuries and complete tears, which occur commonly in professional athletes. However, nonreconstructive options have shown promising results for simple avulsion or partial thickness UCL injuries. Future research comparing reconstructive versus nonreconstructive options is necessary.
Keywords: Ulnar collateral ligament, Repair, Augmentation, Platelet-rich plasma
Introduction
The anterior bundle of medial ulnar collateral ligament (UCL) is the primary restraint to valgus stress at the elbow (Fig. 1). Injury to the UCL was first described in javelin throwers in 1946 [1]. UCL injuries are common in overhead throwing athletes, leading to elbow instability, pain, and loss of control and stamina [2]. This ligament is under significant strain during high velocity pitching, most notably between 20 and 120 degrees of flexion [3] during the late cocking and early acceleration phases of throwing [4–6]. Despite attempts at injury prevention, UCL injury rates continue to climb in throwers of all levels [7, 8, 9•, 10•]. Prior to the initial description of UCL reconstruction in 1986 by Jobe et al., UCL injuries were commonly career ending [11]. Since that time, the technique has been refined and overhead athletes now experience return to sport rates (RTS) ranging from 80 to 94% [12–14]. Although outcomes are favorable, UCL reconstruction generally requires a 12- to 16-month recovery period, and a number of complications have been described such as fracture, inadequate healing, and nerve injury [15].
Fig. 1.
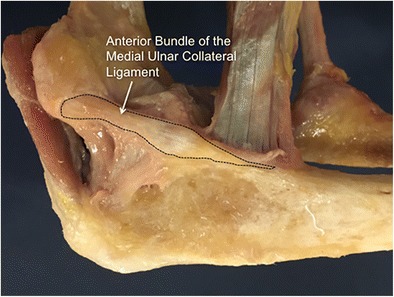
Cadaveric model demonstrating the anterior bundle of the medial ulnar collateral ligament. This ligament serves as the primary restraint to valgus stress across the ulnohumeral joint
Professional throwing athletes commonly have a complete, attritional UCL injury that requires reconstruction. However, younger recreational athletes commonly injure the UCL at either the proximal origin or the distal insertion, and these injuries may be more amendable to less invasive treatments [16]. Despite this, UCL reconstruction procedures increased nearly twofold from 2002 to 2011, with a 9.1% per year increase in patients 15 to 19 years of age [9•]. This significant increase correlates to common misconceptions of UCL reconstruction as over 50% of high school athletes and nearly 40% of high school parents believe that this procedure should be performed on players without elbow injury to enhance performance [17]. Additionally, over 20% of players and 40% of parents believed return to sport would occur in less than 9 months [17].
For selected overhead throwing athletes with UCL injuries, treatment options other than reconstruction have the potential to return them to sport in less time. Current nonreconstructive treatment options for UCL injuries range from nonoperative strategies, such as focused physical therapy and orthobiologic injections (platelet rich plasma [PRP]), to surgical treatments such as ligament repair with and without augmentation.
Patient Factors
The gold standard treatment for professional and elite throwers with full-thickness, attritional midsubstance UCL tears remains reconstruction (Fig. 2). However, for many athletes, nonreconstructive management should be considered.
Fig. 2.
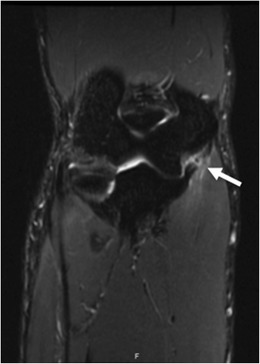
Complete, mid-substance tear of the ulnar collateral ligament in a professional baseball player. This injury was not amenable to nonreconstruction options and a reconstruction with palmaris autograft was performed. After 12 months, he made a full return to pitching in Major League Baseball
When discussing possible nonreconstructive management, the following should be considered: patient age, injury acuity, tissue quality, level of competition, desired timing for return to sport, and concomitant injuries. First-line treatment for nearly all patients with incomplete UCL tears (Fig. 3) is nonoperative management with early initiation of rehabilitation with possible adjunctive biologic treatments. This treatment strategy should also be considered for adolescent patients in order to avoid surgery during skeletal growth. Similarly, this is a common strategy used for high school or college athletes who will soon complete competitive play [18]. Ultimately, these patients would benefit from abstaining from the lengthy rehabilitation process associated with UCL reconstruction.
Fig. 3.
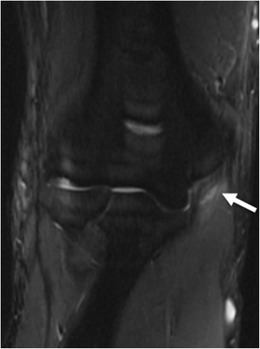
Partial, high-grade ulnar collateral ligament injury in a professional baseball pitcher. He was treated with platelet rich plasma injection, rest and physical therapy. After 8 weeks, he made a full return to pitching in Major League Baseball
Operative intervention should be considered in elite athletes who sustain a partial tear or those who sustain a complete avulsion tear (Fig. 4). In these cases, operative repair with or without augmentation should be considered, as recent results have been favorable with newer techniques [16, 19].
Fig. 4.
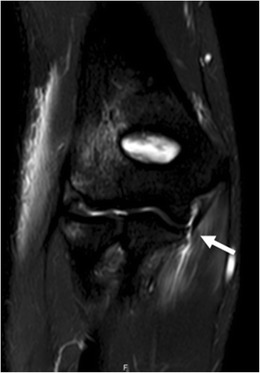
Acute distal ulnar collateral ligament avulsion in a 17-year-old female gymnast. This patient was a junior in high school and was not planning on continuing with gymnastics beyond the high school level. She was treated with an acute repair and was able to return to gymnastics at 6 months and complete her senior season
Nonoperative Management
Physical Therapy
Historically, nonoperative management for UCL injuries in the throwing athlete has shown inferior outcomes when compared to the results following reconstruction. In 2001, Rettig et al. reported on 31 patients treated nonoperatively after UCL injury, including 20 pitchers, 9 infielders, and 2 javelin throwers. Their protocol included rest for 8 to 12 weeks while immobilized in a brace or splint until the patient was pain free. The athlete then began strengthening and throwing over the next 6 weeks. This protocol provided a 42% return to sport (RTS) rate at a mean follow-up of approximately 2 years [20].
However, more recent reports have shown more promise with nonoperative management, particularly in quarterbacks. Dodson et al. reviewed 10 National Football League quarterbacks with UCL injuries and found a 90% RTS rate after less than 4 weeks [21]. Similarly, Bushnell et al. reported an 80% RTS for NFL throwers after 2 weeks of nonoperative management after grade III UCL injuries [22].
While these results were promising for football throwers, the stresses over the UCL for baseball pitchers and positional players are more significant, with average peak torque reaching 64 Newton-meters during the acceleration phase [23]. Despite this, contemporary reports have demonstrated more encouraging results for these athletes compared to prior studies. Ford et al. studied 35 UCL injuries treated nonoperatively in professional baseball players, including 24 pitchers. UCL injuries were evaluated and graded via magnetic resonance imaging (MRI). This cohort consisted of four patients with an intact ligament with edema (grade I), eight patients with an acute partial tear (grade IIA), and 23 patients with chronic healed partial UCL injuries (grade IIB). Therapies focused on rotator cuff and periscapular strengthening with throwing beginning when asymptomatic. High RTS rates were reported with nonoperative treatment, with a RTS rate of 71% for pitchers and 94% for positional players [24].
Frangiamore et al. recently reported outcomes following UCL injury in 32 professional baseball pitchers. These injuries were evaluated via MRI for location, chronicity, and grade of UCL tear. High-grade UCL injuries (> 50% tear) were present in 14 patients, low grade (< 50% tear) in 18 patients, and distal tears in 13 patients. Athletes were treated with rest and ROM exercises for the first week, with graduated rotator cuff and forearm strengthening and plyometric exercises for 6 weeks after injury. At 6 weeks, a progressive throwing program was initiated until asymptomatic. This protocol resulted in a 66% (21/32 athletes) RTS at previous competitive level. Failures were found to be 12.4 times more likely with distal UCL tears. Additionally, UCL tears comprising > 50% of the ligament failed nonoperative management in 73% of professional throwers [25].
Biologic Injections
The use of biologic adjuncts is an area of increasing interest and promise for the treatment of many orthopedic injuries, and the UCL is no exception. One such therapy that has been proposed is platelet-rich plasma (PRP), which is an autologous blood product composed of an ultrafiltrate autologous whole blood with platelet concentrations generally 2.5 to 8.0 times higher than baseline [26]. Injections with PRP result in a multiple fold increase in the number of growth factors present such as platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF), and insulin-like growth factor (IFG). These growth factors help to recruit cells to stimulate angiogenesis and endothelial cell growth to increase blood flow, allowing the initiation of an accelerated healing cascade [26, 27].
While clinical results have been variable, PRP has been associated with improvement in elbow epicondylitis [28], Achilles tendon injuries [26], muscle strains [29], rotator cuff injuries [30], and medial collateral ligament tears of the knee [31]. Mishra et al. reported some of the most promising results regarding PRP therapy for lateral epicondylitis. This double-blinded, prospective randomized control trial evaluated pain relief after PRP injections at 12 and 24 weeks. While there were no statistical differences at 12 weeks, the pain improvement rate was significantly better in the PRP group compared to controls at 24 weeks. Residual pain was noted after 24 weeks in 54% of controls versus only 29% of patients receiving PRP [28].
The clinical use of PRP for treating UCL injuries was recently evaluated in 34 throwing athletes. In this study, all patients were diagnosed with partial thickness UCL tears on MRI and all failed 2 months of nonoperative management after attempting to return to competitive play. These athletes all received a single PRP injection performed under ultrasound guidance into the site of injury of the UCL followed by a guided physical therapy protocol. This protocol resulted in an 88% RTS at an average of 12 weeks. Additionally, medial humeral-ulnar joint space gapping with valgus stress decreased by 9 mm at final follow-up after PRP injection [32].
Similarly, Dines et al. reported results in 44 competitive baseball throwers with MRI evidence of either partial thickness UCL tears (n = 29 patients) or diffuse signal changes (n = 15 patients) [13]. All athletes had previously failed a comprehensive conservative treatment strategy that included rest, activity modification, use of anti-inflammatory medications, and physical therapy. After PRP injections, 73% of athletes reported favorable outcomes, and 67% of professional throwers were able to return to pre-injury level of competition. Notably, of the 29 patients with partial tears, 22 were proximal tears and 7 were distal tears. Distal tears resulted in a poor outcome in 100% of athletes, similar to the findings reported by Frangiamore who showed a 12.4 times greater chance of failure with nonoperative management with distal UCL tears [25]. Additionally, all 15 patients with diffuse changes reported favorable outcomes [13].
While these studies have shown promising results, there has been little data regarding standardization of the PRP injections. Injection schedules are greatly varied throughout the literature, ranging from a single injection to three injections in the recovery period. Additionally, the preparations of the PRP vary greatly in concentration of platelet concentrations, and there is a lack of data supporting any particular concentration in the literature. These areas require additional investigation.
Finally, the use of mesenchymal stem cells (MSCs) has recently become an area of interest as a biologic treatment option. These cells have the potential to differentiate into targeted mesenchymal lineages. Results have demonstrated regenerative properties in patients with avascular necrosis [33], nonunion [34], and after meniscectomy operation [35]. While these results are encouraging, there are no clinical studies investigating the use of MSCs with UCL injuries at this time making this an area for future research.
Operative Management
Ligament Repair
Reconstruction of the ulnar collateral ligament remains the gold standard for the majority UCL injuries. However, primary ligament repair could be considered for acute avulsion injuries or in younger athletes reluctant to undertake the year-long recovery after UCL reconstruction. Additionally, many collegiate and high school athletes who will not advance to the next level of competition may be candidates for UCL repair if the timetable for rehabilitation following reconstruction would outlast their expected career length.
Historically, UCL repair resulted in inferior results compared to reconstruction. Cain et al. reported results of 733 patients who underwent UCL reconstruction and 10 patients who underwent UCL repair. Return to sport rates were higher in athletes treated with reconstruction (83%) versus those treated with repair (70%) [12]. Similarly, in 2000, Azar et al. reported 63% RTS after UCL repair versus 79% after reconstruction [36].
Results after UCL repair have been more favorable in recent studies (Fig. 5). In 2006, Argo et al. reported outcomes in 19 female athletes after UCL repair. This cohort included 14 throwing athletes. UCL repair was performed either by ligament plication, suture repair using transosseous drill holes, or suture repair with bone anchors. Favorable results were achieved in all patients with 16 reporting excellent results and 3 athletes reporting good results. All patients returned to their previous level of competition after UCL repair at an average of 2.5 months postoperatively [37]. Similarly, Savoie et al. reported outcomes after UCL repair in 60 patients in 2008. This cohort was composed of 85% throwers, including high school and collegiate athletes. All patients in this report had sustained either proximal or distal UCL tears, likely due to younger patients sustaining acute injuries versus attritional injuries noted in professional athletes. The authors performed a suture repair using bone anchors, and 97% of athletes were able to a return to play rate at the same or higher level by 6 months after repair [16]. Importantly, athletes commonly required a brace when throwing after repair, which has the potential to limit athletic performance and may not be tolerated in many competitive athletes. These more favorable results have been attributed to improved surgical technique as well as suture and suture anchor technology. Suture anchors have become a cornerstone of rotator cuff repairs [38], distal biceps repairs [39], ankle ligament repairs [40], and hand collateral ligament repairs [41]. New technologies have allowed suture anchors to be osteoconductive resulting in improved bone stock, which potentially diminishes complications associated with transosseous fixation [42]. Additionally, newer suture materials have improved load sharing capabilities and increased contact area resulting in both biomechanical and clinical benefits [43].
Fig. 5.
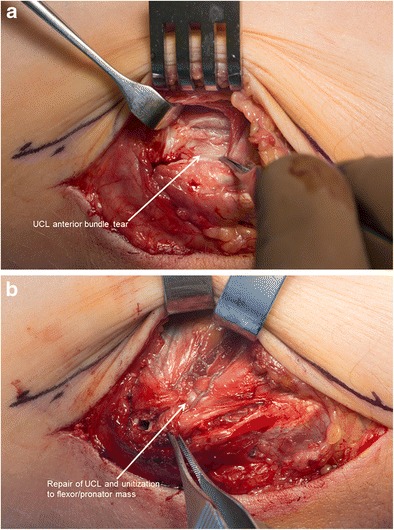
a Intraoperative photo reveals tear UCL anterior bundle and split in the flexor/pronator mass. b The UCL tear has been repaired and unitized to flexor/pronator mass using a nonabsorbable suture in a Krakow fashion
Harnessing these technologic advancements in anchor and suture material, Dugas et al. have recently described a technique for UCL repair that the supplemented by an internal brace composed of suture material (Fig. 6) [44]. The authors used a biomechanical study to compare this technique to the modified Jobe technique for UCL reconstruction in a cadaveric model. Gap formation under valgus load was less for the UCL repair augmented with spanning internal brace when compared to the UCL reconstruction group with no difference noted in ultimate failure strength. All failures occurred through the cadaveric bone, with no anchor failures or pull out, and no suture tears [45]. This technique could provide a bone preserving solution and more rapid and reliable recovery for UCL avulsion injuries, though in vivo studies are necessary to determine clinical utility. Based on their recommendations, current candidates for this procedure include younger athletes with UCL end avulsion injuries or partial UCL tears [44]. Although further investigations in a clinical population are warranted, this technique has the potential to allowing appropriately indicated throwers an opportunity to RTS faster than if they were to undergo reconstruction.
Fig. 6.
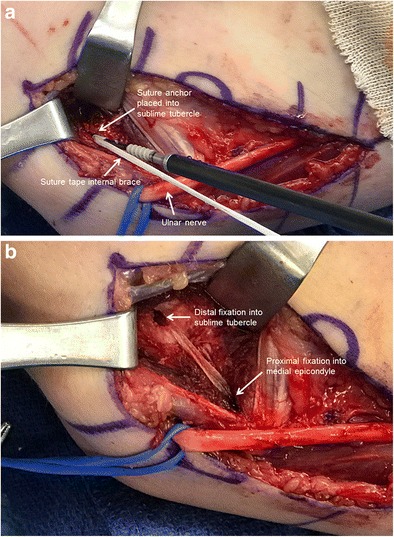
a Intraoperative image demonstrating insertion of internal brace composed of suture material using a suture anchor. b Final internal brace augmentation. The UCL repair lies under the internal brace augmentation
Revision
As the number of UCL reconstruction procedures continues to grow, the number of revisions has correspondingly continued to grow with an overall revision rate of 15% [46•]. Revision UCL reconstruction results have been less favorable than primary UCL reconstruction with lower RTS rates, decreased performance, and shorter career lengths [47•, 48]. However, there has been very little data reported on revision surgery after UCL repair. Savoie et al. reported on two patients who underwent UCL reconstruction after a failed UCL repair. Both patients were able to return to previous level of competitive play, and no complications were reported [16]. Theoretically, depending on the technique utilized, revision after UCL repair should be less technically challenging compared to revision following reconstruction. This is primary due to the fact that repair requires less soft tissue dissection and bone removal, which should lead to decreased scarring and more robust bone stock for the revision surgery if bone tunnels were not created [49].
Conclusions
Ulnar collateral ligament injuries are most commonly treated with reconstruction, especially in elite throwing athletes who sustain midsubstance, distal, complete, or diffuse ligament injury. However, the 12- to 16-month recovery after reconstruction could potentially be reduced in some patients after UCL injury if they are candidates for nonreconstructive options. Ideal criteria for consideration of these nonreconstruction strategies include acute tears, humeral sided injuries, young age, lower demand, and shorter athletic career expectancy. Both directed physical therapy and biologic injections have provided encouraging results with high return to sport rates in appropriately selected patients. UCL repair with suture tape augmentation may hold promise moving forward; however, additional clinical studies are needed. These nonreconstruction options have the advantages of a more rapid recovery time, decreased soft tissue injury, and improved bone preservation compared to modern reconstruction techniques. When considering nonreconstruction options for UCL injuries, it also is critical that timing be considered. If patients spend a significant amount of time pursing these options but ultimately require a UCL reconstruction, they could miss two or more years of athletic activity. Accordingly, treatment strategies must be individualized. While these techniques have all demonstrated encouraging results, further long-term clinical investigations and head-to-head comparisons with reconstruction are still necessary.
Compliance with Ethical Standards
Conflict of Interest
Joshua Dines reports a grant and personal fees from Arthrex, personal fees from CONMED Linvatec and Trice, and royalties from Linvatec and Wolters Kluwer Health. All other authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Injuries in Overhead Athletes
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Waris W. Elbow injuries of javelin-throwers. Acta Chir Scand. 1946;93(6):563–575. [PubMed] [Google Scholar]
- 2.Cain EL, Dugas JR, Wolf RS, Andrews JR. Elbow injuries in throwing athletes: a current concepts review. Am J Sports Med. 2003;31(4):621–635. doi: 10.1177/03635465030310042601. [DOI] [PubMed] [Google Scholar]
- 3.Freehill MT, Safran MR. Diagnosis and management of ulnar collateral ligament injuries in throwers. Curr Sports Med Rep. 2011;10(5):271–278. doi: 10.1249/JSR.0b013e31822d4000. [DOI] [PubMed] [Google Scholar]
- 4.Bruce JR, Andrews JR. Ulnar collateral ligament injuries in the throwing athlete. J Am Acad Orthop Surg. 2014;22(5):315–325. doi: 10.5435/JAAOS-22-05-315. [DOI] [PubMed] [Google Scholar]
- 5.Dodson CC, Altchek DW. Ulnar collateral ligament reconstruction revisited: the procedure I use and why. Sports Health. 2012;4(5):433–437. doi: 10.1177/1941738112454649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones KJ, Osbahr DC, Schrumpf MA, Dines JS, Altchek DW. Ulnar collateral ligament reconstruction in throwing athletes: a review of current concepts. AAOS exhibit selection. J Bone Joint Surg Am. 2012;94(8):e49–1-12. doi: 10.2106/JBJS.K.01034. [DOI] [PubMed] [Google Scholar]
- 7.Conte SA, Fleisig GS, Dines JS, Wilk KE, Aune KT, Patterson-Flynn N, ElAttrache N. Prevalence of ulnar collateral ligament surgery in professional baseball players. Am J Sports Med. 2015;43(7):1764–1769. doi: 10.1177/0363546515580792. [DOI] [PubMed] [Google Scholar]
- 8.Conte S, Camp CL, Dines JS. Injury trends in Major League Baseball over 18 seasons: 1998-2015. Am J Orthop (Belle Mead NJ) 2016;45(3):116–123. [PubMed] [Google Scholar]
- 9.Erickson BJ, Nwachukwu BU, Rosas S, Schairer WW, FM MC, Bach BR, et al. Trends in medial ulnar collateral ligament reconstruction in the United States: a retrospective review of a large private-payer database from 2007 to 2011. Am J Sports Med. 2015;43(7):1770–1774. doi: 10.1177/0363546515580304. [DOI] [PubMed] [Google Scholar]
- 10.Hodgins JL, Vitale M, Arons RR, Ahmad CS. Epidemiology of medial ulnar collateral ligament reconstruction: a 10-year study in New York state. Am J Sports Med. 2016;44(3):729–734. doi: 10.1177/0363546515622407. [DOI] [PubMed] [Google Scholar]
- 11.Jobe FW, Stark H, Lombardo SJ. Reconstruction of the ulnar collateral ligament in athletes. J Bone Joint Surg Am. 1986;68(8):1158–1163. doi: 10.2106/00004623-198668080-00004. [DOI] [PubMed] [Google Scholar]
- 12.Cain EL, Andrews JR, Dugas JR, Wilk KE, McMichael CS, Walter JC, et al. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: results in 743 athletes with minimum 2-year follow-up. Am J Sports Med. 2010;38(12):2426–2434. doi: 10.1177/0363546510378100. [DOI] [PubMed] [Google Scholar]
- 13.Dines JS, ElAttrache NS, Conway JE, Smith W, Ahmad CS. Clinical outcomes of the DANE TJ technique to treat ulnar collateral ligament insufficiency of the elbow. Am J Sports Med. 2007;35(12):2039–2044. doi: 10.1177/0363546507305802. [DOI] [PubMed] [Google Scholar]
- 14.Erickson BJ, Bach BR, Cohen MS, Bush-Joseph CA, Cole BJ, Verma NN, et al. Ulnar collateral ligament reconstruction: the rush experience. Orthop J Sports Med. 2016;4(1):2325967115626876. doi: 10.1177/2325967115626876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Watson JN, McQueen P, Hutchinson MR. A systematic review of ulnar collateral ligament reconstruction techniques. Am J Sports Med. 2014;42(10):2510–2516. doi: 10.1177/0363546513509051. [DOI] [PubMed] [Google Scholar]
- 16.Savoie FH, Trenhaile SW, Roberts J, Field LD, Ramsey JR. Primary repair of ulnar collateral ligament injuries of the elbow in young athletes: a case series of injuries to the proximal and distal ends of the ligament. Am J Sports Med. 2008;36(6):1066–1072. doi: 10.1177/0363546508315201. [DOI] [PubMed] [Google Scholar]
- 17.Ahmad CS, Grantham WJ, Greiwe RM. Public perceptions of Tommy John surgery. Phys Sportsmed. 2012;40(2):64–72. doi: 10.3810/psm.2012.05.1966. [DOI] [PubMed] [Google Scholar]
- 18.Rebolledo BJ, Dugas JR, Bedi A, Ciccotti MG, Altchek DW, Dines JS. Avoiding Tommy John surgery. Am J Sports Med. 2017;45(13):3143–3148. doi: 10.1177/0363546517692548. [DOI] [PubMed] [Google Scholar]
- 19.Kenter K, Behr CT, Warren RF, O’Brien SJ, Barnes R. Acute elbow injuries in the National Football League. J Shoulder Elb Surg. 2000;9(1):1–5. doi: 10.1016/S1058-2746(00)80023-3. [DOI] [PubMed] [Google Scholar]
- 20.Rettig AC, Sherrill C, Snead DS, Mendler JC, Mieling P. Nonoperative treatment of ulnar collateral ligament injuries in throwing athletes. Am J Sports Med. 2001;29(1):15–17. doi: 10.1177/03635465010290010601. [DOI] [PubMed] [Google Scholar]
- 21.Dodson CC, Slenker N, Cohen SB, Ciccotti MG, DeLuca P. Ulnar collateral ligament injuries of the elbow in professional football quarterbacks. J Shoulder Elb Surg. 2010;19(8):1276–1280. doi: 10.1016/j.jse.2010.05.028. [DOI] [PubMed] [Google Scholar]
- 22.Bushnell BD, Bitting SS, Crain JM, Boublik M, Schlegel TF. Treatment of magnetic resonance imaging-documented isolated grade III lateral collateral ligament injuries in National Football League athletes. Am J Sports Med. 2010;38(1):86–91. doi: 10.1177/0363546509344075. [DOI] [PubMed] [Google Scholar]
- 23.Fleisig GS, Andrews JR, Dillman CJ, Escamilla RF. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23(2):233–239. doi: 10.1177/036354659502300218. [DOI] [PubMed] [Google Scholar]
- 24.Ford GM, Genuario J, Kinkartz J, Githens T, Noonan T. Return-to-play outcomes in professional baseball players after medial ulnar collateral ligament injuries: comparison of operative versus nonoperative treatment based on magnetic resonance imaging findings. Am J Sports Med. 2016;44(3):723–728. doi: 10.1177/0363546515621756. [DOI] [PubMed] [Google Scholar]
- 25.Frangiamore SJ, Lynch TS, Vaughn MD, Soloff L, Forney M, Styron JF, Schickendantz MS. Magnetic resonance imaging predictors of failure in the nonoperative management of ulnar collateral ligament injuries in professional baseball pitchers. Am J Sports Med. 2017;45(8):1783–1789. doi: 10.1177/0363546517699832. [DOI] [PubMed] [Google Scholar]
- 26.Hall MP, Band PA, Meislin RJ, Jazrawi LM, Cardone DA. Platelet-rich plasma: current concepts and application in sports medicine. J Am Acad Orthop Surg. 2009;17(10):602–608. doi: 10.5435/00124635-200910000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Lopez-Vidriero E, Goulding KA, Simon DA, Sanchez M, Johnson DH. The use of platelet-rich plasma in arthroscopy and sports medicine: optimizing the healing environment. Arthroscopy. 2010;26(2):269–278. doi: 10.1016/j.arthro.2009.11.015. [DOI] [PubMed] [Google Scholar]
- 28.Mishra A, Woodall J, Vieira A. Treatment of tendon and muscle using platelet-rich plasma. Clin Sports Med. 2009;28(1):113–125. doi: 10.1016/j.csm.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 29.Hammond JW, Hinton RY, Curl LA, Muriel JM, Lovering RM. Use of autologous platelet-rich plasma to treat muscle strain injuries. Am J Sports Med. 2009;37(6):1135–1142. doi: 10.1177/0363546508330974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Randelli P, Arrigoni P, Ragone V, Aliprandi A, Cabitza P. Platelet rich plasma in arthroscopic rotator cuff repair: a prospective RCT study, 2-year follow-up. J Shoulder Elb Surg. 2011;20(4):518–528. doi: 10.1016/j.jse.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 31.Foster TE, Puskas BL, Mandelbaum BR, Gerhardt MB, Rodeo SA. Platelet-rich plasma: from basic science to clinical applications. Am J Sports Med. 2009;37(11):2259–2272. doi: 10.1177/0363546509349921. [DOI] [PubMed] [Google Scholar]
- 32.Podesta L, Crow SA, Volkmer D, Bert T, Yocum LA. Treatment of partial ulnar collateral ligament tears in the elbow with platelet-rich plasma. Am J Sports Med. 2013;41(7):1689–1694. doi: 10.1177/0363546513487979. [DOI] [PubMed] [Google Scholar]
- 33.Wyles CC, Houdek MT, Crespo-Diaz RJ, Norambuena GA, Stalboerger PG, Terzic A, Behfar A, Sierra RJ. Adipose-derived mesenchymal stem cells are phenotypically superior for regeneration in the setting of osteonecrosis of the femoral head. Clin Orthop Relat Res. 2015;473(10):3080–3090. doi: 10.1007/s11999-015-4385-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hernigou P, Poignard A, Beaujean F, Rouard H. Percutaneous autologous bone-marrow grafting for nonunions. Influence of the number and concentration of progenitor cells. J Bone Joint Surg Am. 2005;87(7):1430–1437. doi: 10.2106/JBJS.D.02215. [DOI] [PubMed] [Google Scholar]
- 35.Vangsness CT, Farr J, Boyd J, Dellaero DT, Mills CR, LeRoux-Williams M. Adult human mesenchymal stem cells delivered via intra-articular injection to the knee following partial medial meniscectomy: a randomized, double-blind, controlled study. J Bone Joint Surg Am. 2014;96(2):90–98. doi: 10.2106/JBJS.M.00058. [DOI] [PubMed] [Google Scholar]
- 36.Azar FM, Andrews JR, Wilk KE, Groh D. Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am J Sports Med. 2000;28(1):16–23. doi: 10.1177/03635465000280011401. [DOI] [PubMed] [Google Scholar]
- 37.Argo D, Trenhaile SW, Savoie FH, Field LD. Operative treatment of ulnar collateral ligament insufficiency of the elbow in female athletes. Am J Sports Med. 2006;34(3):431–437. doi: 10.1177/0363546505281240. [DOI] [PubMed] [Google Scholar]
- 38.Tashjian RZ, Kolz CW, Suter T, Henninger HB. Biomechanics of polyhydroxyalkanoate mesh-augmented single-row rotator cuff repairs. Am J Orthop (Belle Mead NJ) 2016;45(7):E527–EE33. [PubMed] [Google Scholar]
- 39.Maciel RA, Costa PS, Figueiredo EA, Belangero PS, Pochini AC, Ejnisman B. Acute distal biceps ruptures: single incision repair by use of suture anchors. Rev Bras Ortop. 2017;52(2):148–153. doi: 10.1016/j.rbo.2016.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Acevedo JI, Ortiz C, Golano P, Nery C. ArthroBroström lateral ankle stabilization technique: an anatomic study. Am J Sports Med. 2015;43(10):2564–2571. doi: 10.1177/0363546515597464. [DOI] [PubMed] [Google Scholar]
- 41.Gil JA, Chambers A, Shah KN, Crisco JJ, Got C, Akelman E. A biomechanical evaluation of a 2-suture anchor repair technique for thumb metacarpophalangeal joint ulnar collateral ligament injuries. Hand (N Y). 2017 1558944717725380. 10.1177/1558944717725380. [DOI] [PMC free article] [PubMed]
- 42.Barber FA, Dockery WD, Cowden CH. The degradation outcome of biocomposite suture anchors made from poly L-lactide-co-glycolide and β-tricalcium phosphate. Arthroscopy. 2013;29(11):1834–1839. doi: 10.1016/j.arthro.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 43.Barber FA, Herbert MA, Schroeder FA, Aziz-Jacobo J, Mays MM, Rapley JH. Biomechanical advantages of triple-loaded suture anchors compared with double-row rotator cuff repairs. Arthroscopy. 2010;26(3):316–323. doi: 10.1016/j.arthro.2009.07.019. [DOI] [PubMed] [Google Scholar]
- 44.Dugas JR. Ulnar collateral ligament repair: an old idea with a new wrinkle. Am J Orthop (Belle Mead NJ) 2016;45(3):124–127. [PubMed] [Google Scholar]
- 45.Dugas JR, Walters BL, Beason DP, Fleisig GS, Chronister JE. Biomechanical comparison of ulnar collateral ligament repair with internal bracing versus modified Jobe reconstruction. Am J Sports Med. 2016;44(3):735–741. doi: 10.1177/0363546515620390. [DOI] [PubMed] [Google Scholar]
- 46.Wilson AT, Pidgeon TS, Morrell NT, DaSilva MF. Trends in revision elbow ulnar collateral ligament reconstruction in professional baseball pitchers. J Hand Surg Am. 2015;40(11):2249–2254. doi: 10.1016/j.jhsa.2015.07.024. [DOI] [PubMed] [Google Scholar]
- 47.Marshall NE, Keller RA, Lynch JR, Bey MJ, Moutzouros V. Pitching performance and longevity after revision ulnar collateral ligament reconstruction in Major League Baseball pitchers. Am J Sports Med. 2015;43(5):1051–1056. doi: 10.1177/0363546515579636. [DOI] [PubMed] [Google Scholar]
- 48.Liu JN, Garcia GH, Conte S, ElAttrache N, Altchek DW, Dines JS. Outcomes in revision Tommy John surgery in Major League Baseball pitchers. J Shoulder Elb Surg. 2016;25(1):90–97. doi: 10.1016/j.jse.2015.08.040. [DOI] [PubMed] [Google Scholar]
- 49.Erickson BJ, Bach BR, Verma NN, Bush-Joseph CA, Romeo AA. Treatment of ulnar collateral ligament tears of the elbow: is repair a viable option? Orthop J Sports Med. 2017;5(1):2325967116682211. doi: 10.1177/2325967116682211. [DOI] [PMC free article] [PubMed] [Google Scholar]


