Abstract
Background:
The optimal postoperative rehabilitation protocol following repair of complete proximal hamstring tendon ruptures is the subject of ongoing investigation, with a need for more standardized regimens and evidence-based modalities.
Purpose:
To assess the variability across proximal hamstring tendon repair rehabilitation protocols published online by United States (US) orthopaedic teaching programs.
Study Design:
Cross-sectional study.
Methods:
Online proximal hamstring physical therapy protocols from US academic orthopaedic programs were reviewed. A web-based search using the search term complete proximal hamstring repair rehabilitation protocol provided an additional 14 protocols. A comprehensive scoring rubric was developed after review of all protocols and was used to assess each protocol for both the presence of various rehabilitation components and the point at which those components were introduced.
Results:
Of 50 rehabilitation protocols identified, 35 satisfied inclusion criteria and were analyzed. Twenty-five protocols (71%) recommended immediate postoperative bracing: 12 (34%) prescribed knee bracing, 8 (23%) prescribed hip bracing, and 5 (14%) did not specify the type of brace recommended. Fourteen protocols (40%) advised immediate nonweightbearing with crutches, while 16 protocols (46%) permitted immediate toe-touch weightbearing. Advancement to full weightbearing was allowed at a mean of 7.1 weeks (range, 4-12 weeks). Most protocols (80%) recommended gentle knee and hip passive range of motion and active range of motion, starting at a mean 1.4 weeks (range, 0-3 weeks) and 4.0 weeks (range, 0-6 weeks), respectively. However, only 6 protocols (17%) provided specific time points to initiate full hip and knee range of motion: a mean 8.0 weeks (range, 4-12 weeks) and 7.8 weeks (range, 0-12 weeks), respectively. Considerable variability was noted in the inclusion and timing of strengthening, stretching, proprioception, and cardiovascular exercises. Fifteen protocols (43%) required completion of specific return-to-sport criteria before resuming training.
Conclusion:
Marked variability is found in both the composition and timing of rehabilitation components across the various complete proximal hamstring repair rehabilitation protocols published online. This finding mirrors the variability of proposed rehabilitation protocols in the professional literature and represents an opportunity to improve patient care.
Keywords: hamstring, tendon rupture, tendon repair, physical therapy, rehabilitation
Complete proximal hamstring tendon ruptures are relatively uncommon injuries resulting from abrupt hyperflexion of the hip during knee extension.2 While most hamstring injuries are strains occurring at the myotendinous junction,17 proximal tendon ruptures account for nearly 12% of all hamstring injuries; they can be further characterized as complete or incomplete and with or without retraction of the tendinous insertion.21 Whereas strains can be successfully managed nonoperatively,11 recent studies have supported early operative repair of complete tendon ruptures. Harris et al16 systematically reviewed 18 studies, which included 286 operative and 14 nonoperative cases, and found improved clinical outcomes following operative repair. Specifically, operative repair resulted in a higher rate of return to preinjury level of sport and improved strength and endurance compared with nonoperative management. Van der Made et al34 performed a meta-analysis of 13 studies that included 387 total operative cases with magnetic resonance imaging or ultrasonography-confirmed proximal hamstring tendon ruptures; this meta-analysis showed improved patient satisfaction after operative repair. Most recently, a prospective case series of 96 operative cases also found benefit for surgical intervention, as evidenced by significantly better patient-reported outcomes when compared with conservative measures across all tendon avulsions regardless of time to surgery, degree of injury, or presence of tendon retraction.4
Despite the growing support for operative management of complete proximal hamstring tendon rupture, optimal guidelines for rehabilitation are not well established. This stands in contrast to numerous studies detailing physical therapy protocols for conservative management of hamstring strains and tears.31,36 Presently, physical therapy protocols are primarily based on rupture chronicity, the surgeon’s input regarding strength and tension of the repair, and the physical therapist’s assessment of tissue healing.8 Without a validated standard-of-care protocol, wide variability exists across the professional literature with regard to key elements of rehabilitation, including early postoperative protection, phases of rehabilitation, incorporation of hamstring stretching, and criteria for return to activity and sport.1,15
In this observational study, we evaluated a series of online rehabilitation protocols for the management of operatively treated complete proximal hamstring ruptures. Our primary objective was to better characterize protocol variability with regard to the inclusion and timing of key physical therapy components.
Methods
Using a method similar to that proposed by Makhni et al,24 we conducted a general web-based search in May 2017 of publicly available physical therapy protocols from the websites of United States academic orthopaedic surgery programs participating in the Electronic Residency Application Service (ERAS). ERAS is an online, centralized application service used in the residency application process. Academically driven protocols were preferentially selected in order to limit the degree of bias and variability obtained through online search engines. However, as only 21 academic protocols were identified, an additional 14 protocols were identified in May 2017 via a general web-based query (www.google.com) by use of the search term complete proximal hamstring repair rehabilitation protocol. This was performed to increase the sample size to a total of 35 protocols; however, these additional 14 protocols are also the most accessible protocols for patients. Supplemental protocols for pediatric patients, nonproximal hamstring repairs, or repairs following incomplete tears were not chosen for review. Furthermore, those protocols lacking sufficient detail, such as specific time points for the initiation of protocol components, were excluded from review.
A custom rubric was created, with scoring sections for the following rehabilitation protocol components: postoperative adjunctive therapies including bracing and cryotherapy, weightbearing status, range of motion (ROM) limitations, strengthening, stretching, proprioception exercises, and return to basic and athletic activities (Table 1). Each protocol was reviewed and appropriately scored based on the presence of the aforementioned rehabilitation protocol components. Data on the timing of specific interventions, as well as markers for therapy progression, were recorded and documented.
TABLE 1.
Proximal Hamstring Repair Rehabilitation Rubric Categories
| Postoperative adjunctive therapies | Brace type and use, brace lock limits, cryotherapy, neuromuscular electric stimulation |
| Range of motion and weightbearing | Knee and hip flexion/extension goals, weightbearing parameters |
| Strengthening | Passive range of motion, active range of motion, quadriceps sets, ankle pumps, mini-squats, hamstring sets, hip abduction/adduction, double-leg bridge, step-up/down, abdominal isometrics, resisted hamstring curls, double-leg physioball curls, lunges, single-leg physioball curls, single-leg bridge |
| Stretching | Hamstring stretch, hip flexion/adduction stretch, quadriceps stretch, calf stretch |
| Proprioception | Weight shifting, single-leg balance, impact control exercises, balance board, advanced proprioception |
| Return to basic activity | Upper body exercises, normal gait training, stationary bike, aquatic exercises, elliptical, stair climber, swimming, slow walking, jogging, running, sprinting |
| Return to athletic activity | Plyometrics, multiplane activity, agility, sports-specific drills, return to training, return to competition |
Results
Thirty-five rehabilitation protocols for proximal hamstring repair were collected and included for review. Of the 155 ERAS-affiliated academic orthopaedic programs, 21 programs (14%) provided publicly available physical therapy protocols. The remaining 14 protocols were the first protocols identified by a general web-based search.
Postoperative Adjunctive Therapy
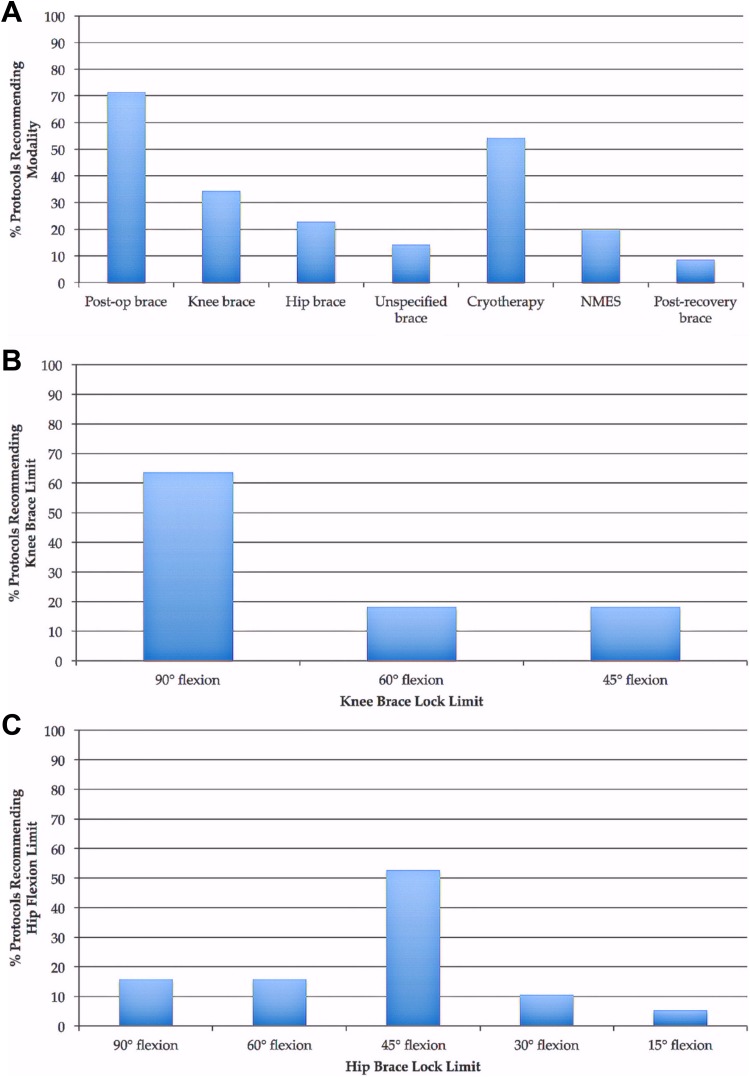
Three types of postoperative adjunct therapies were assessed (Figure 1A): bracing, cryotherapy, and neuromuscular electric stimulation (NMES). Most protocols (71%) advised immediate postoperative bracing: 34% recommended knee braces, while 23% recommended hip braces. The remaining 5 protocols (14%) recommended postoperative bracing but did not specify the type of brace to be used. For knee orthoses, bracing was recommended with the knee locked at 90° of flexion postoperatively by most protocols (64%) (Figure 1B). Alternatively, 53% of protocols recommending hip orthoses, advised limiting hip flexion to 45° (Figure 1C). The mean time points for discontinuing knee and hip orthoses were 5.5 weeks (range, 4-6 weeks) and 6.0 weeks (range, 4-8 weeks), respectively. Only 3 protocols reported guidelines for transitioning to any form of secondary or postrecovery functional brace. Approximately half of the protocols (19/35, 54%) recommended cryotherapy, and 7 protocols (20%) recommended commencement of NMES within the first postoperative week (Figure 1A).
Figure 1.
(A) Postoperative variability in adjunctive therapy utilization between physical therapy rehabilitation protocols. More than 70% of protocols recommended some form of immediate postoperative brace; 34% recommended knee braces, while 23% recommended hip braces. While cryotherapy was recommended to decrease swelling and pain in just over 50% of protocols, few protocols advocated for the use of neuromuscular electric stimulation (NMES) or postrecovery functional bracing. (B) Of those protocols recommending postoperative knee bracing, the most common knee flexion lock limit was 90° of flexion. (C) Of those protocols recommending postoperative hip bracing, the most common hip flexion lock limit was 45° of flexion.
Weightbearing and Range of Motion
With regard to immediate postoperative weightbearing, nonweightbearing and toe-touch weightbearing with crutches were nearly equally represented across studied protocols at 40% and 46%, respectively. Five protocols (14%) recommended partial weightbearing at varying percentages of body weight immediately postoperatively. The timeline for return to full weightbearing was reported at a mean of 7.1 (range, 4-12) weeks.
ROM milestones were rarely reported; when they were noted, they showed considerable variability in both the inclusion and timing of ROM goals. Only 6 protocols (17%) provided specific time points for achieving full hip and knee ROM, at means of 8.0 weeks (range, 4-12 weeks) and 7.8 weeks (range, 0-12 weeks), respectively.
Strengthening
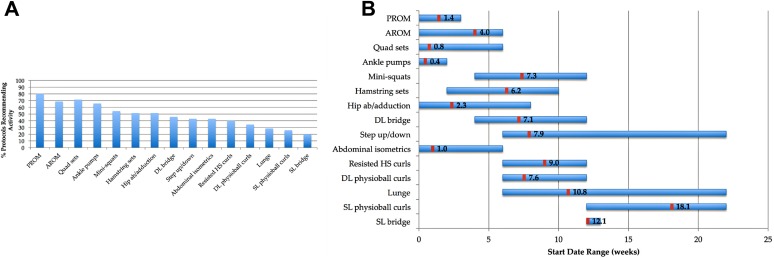
Fifteen strengthening exercises were examined in this investigation (see Table 1). Seven of the 15 exercises appeared in greater than 50% of protocols, with passive range of motion (PROM) of the knee and hip being the most commonly (28/35, 80%) recommended activity (Figure 2A). Wide variation was apparent with regard to when exercises were initiated (Figure 2B). Step-ups/downs and lunges were found to have the most variability in terms of recommended start times; in both, the range for earliest start date covered 16 weeks.
Figure 2.
(A) Strengthening exercises. Significant variation was found with regard to types of exercises included in rehabilitation protocols. (B) Significant variation was also found with regard to recommended start times. The numbered line within each range represents the mean of the data set. AROM, active range of motion; DL, double leg; HS, hamstring; PROM, passive range of motion; Quad, quadriceps; SL, single leg.
Stretching and Proprioception
Forty-six percent of protocols recommended starting hamstring stretches at a mean of 10.1 weeks (range, 6-17 weeks) postoperatively. Hip flexion/adduction, quadriceps, and calf stretches were rarely recommended, included in 4 or fewer protocols.
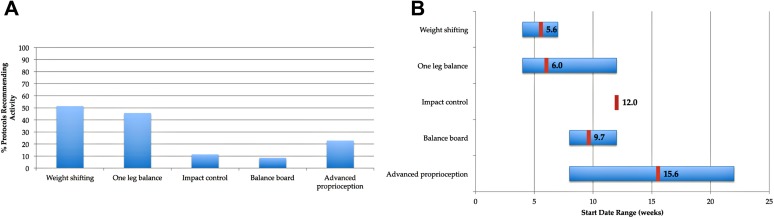
Five different proprioceptive exercises were selected for review (see Table 1). The most frequently recommended exercise was weight shifting, included by 51% of protocols (Figure 3A). As with strengthening exercises, a significant degree of variability was found with regard to earliest start dates (Figure 3B). This was particularly evident for unspecified “advanced proprioceptive” exercises, recommended at a mean of 15.6 weeks (range, 8-22 weeks).
Figure 3.
(A) Proprioception exercises. Significant variation was found with regard to the inclusion of certain exercises. Nearly 25% of rehabilitation protocols recommended late-stage proprioceptive activities but did not specify exercises, represented in the chart as advanced proprioception. (B) Exercise start dates were marked by substantial variation. The numbered line within each range represents the mean of the data set.
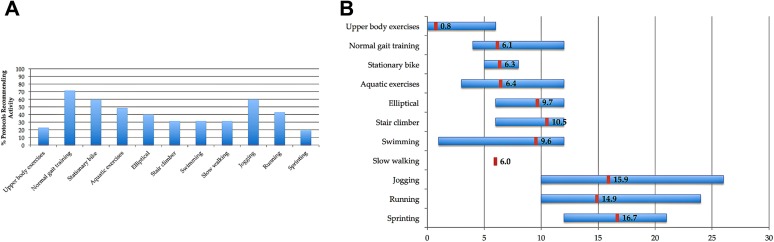
Return to Basic Activity
Eleven activities were included in the rubric to assess return to basic activity (see Table 1). Normal gait training was the most frequently recommended, reported by 71% of protocols (Figure 4A). Stationary biking and jogging were also common, both mentioned by 60% of protocols. Upper body exercises or circuits were the earliest activities, initiated at a mean start time of approximately 5 days. Start dates for jogging, running, and sprinting were highly variable (Figure 4B).
Figure 4.
(A) Return to basic activity and (B) start dates. The numbered line within each range represents the mean of the data set.
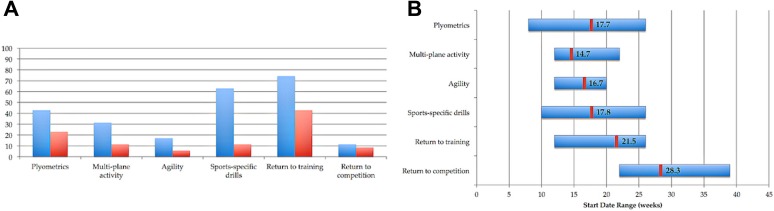
Return to Athletic Activity
Return to athletic activity was assessed by 4 metrics: sports-specific drills, plyometrics, multiplane activities, and agility exercises (Figure 5A). Across these activities, less than 25% of protocols were well described in terms of specific exercises and drills to be performed (Figure 5A). Again, considerable variability with regard to earliest start dates was noted across rehabilitation protocols (Figure 5B).
Figure 5.
(A) Return to athletic activity, where the blue bars represent the percentage of protocols recommending the activity and the red bars represent the percentage of protocols in which the activity is well-defined. (B) Return to athletic activity start dates. Protocols rarely provided clear instructions for athletic activities or established criteria-based progression for return to training. The numbered line within each range represents the mean of the data set.
Twenty-six protocols (75%) specifically reported return to training as a goal for proximal hamstring repair rehabilitation, at a mean of 21.5 weeks (range, 12-26 weeks). Fifteen protocols (43%) provided explicit criteria for this progression, of which 14 (40%) utilized isokinetic hamstring strength testing. Only 3 protocols explicitly recommended hop testing as an assessment tool for return to training. Return to competition was mentioned by 4 protocols, at a mean of 28.3 weeks (range, 22-39 weeks) postoperatively (Figure 5B).
Discussion
Recent studies have confirmed the longstanding belief that early operative management of complete proximal hamstring tendon rupture leads to superior clinical and patient-reported outcomes.4,5,8,10,16,30,34 However, amid the effort to accrue more high-quality prospective outcome studies, the importance of the postoperative rehabilitation process has been noticeably overlooked despite the possibility that it promotes earlier return to sport and prevents reinjury.1,15 In this study, we highlight that a minority of orthopaedic teaching programs publish proximal hamstring physical therapy protocols online; furthermore, available protocols are marked by disparities in both the inclusion of specific physical therapy modalities and the timelines of rehabilitation milestones. The wide variability in fundamental physical therapy components observed across online academic protocols is mirrored in the scientific literature.‡ Thus, there is a need for rehabilitation-centered investigations with aims of establishing a validated rehabilitation protocol and, ultimately, standardizing physical therapy programs to improve patient care.1,15,18
In 2009, Hamersly and Schrader15 reviewed 7 studies that had published postoperative rehabilitation regimens for complete proximal hamstring tendon tears, and their review noted the paucity and variability of scientific literature on the topic. Askling et al1 later reviewed the available literature for treatment of acute, total proximal hamstring tendon ruptures and arrived at the same conclusion regarding postoperative management: The studies were sparse and the proposed protocols varied widely. Notably, of all the studies included in both reviews, only one had established an objective of proposing a detailed rehabilitation protocol.18 Both of these groups of authors subsequently proposed rehabilitation guidelines, but considerable variability remained between basic components such as immobilization and early weightbearing status.1,15 Given this level of discrepancy, a baseline assessment of variability across key physical therapy components in the professional literature, as well as online, is warranted.
Weightbearing Limitations
Weightbearing status is one of the most important aspects of early rehabilitation. Restrictions on weightbearing status after complete proximal hamstring tendon repair are important to prevent hamstring activation and muscle lengthening.1,15 In our study, immediate nonweightbearing and toe-touch weightbearing were represented nearly equally across protocols, at 40% and 46%, respectively. Fewer protocols (14%) permitted initial partial weightbearing. Progression to full weightbearing was reported at a mean of 7.1 weeks (range, 4-12 weeks).
These findings are congruent with the available scientific literature. Several studies recommended immediate nonweightbearing periods lasting between 4 and 8 weeks,9,15,20,25 while others permitted immediate toe-touch weightbearing for periods between 2 and 6 weeks.1,7,12,13,30 Fewer research protocols have proposed immediate partial weightbearing with crutches23,35; of those doing so, full weightbearing was achieved by 6 weeks. Of note, in a case study of a patient with a chronic repair requiring an Achilles tendon allograft, immediate weightbearing as tolerated was permitted while using a Bledsoe hip spica knee brace.18 As an outlier to conservative management, Birmingham et al3 allowed immediate full weightbearing with the aid of crutches and a pelvic-thigh-hip spica orthosis in their case series of 9 acute and 14 chronic repairs.
Hip and Knee Immobilization
Immobilization of the hip, knee, or both hip and after complete proximal hamstring repairs remains a conundrum. While 71% of online protocols recommended immediate postoperative bracing, 34% recommended knee braces and 23% recommended hip braces. Of those protocols prescribing knee braces, 64% recommended locking the knee at 90° of flexion. Alternatively, for the protocols prescribing hip braces, 53% recommended limiting hip flexion to 45°. Several online protocols stated that the use of a brace was predicated on the discretion of the surgeon, the time of year, and the timing of surgery relative to the date of injury.
Within the professional literature, several notable studies recommend against postoperative bracing as long as the patient is capable of maintaining the leg in a neutral position.1,19,26,32 In reporting the outcomes of 72 acute and chronic complete proximal hamstring tears, Carmichael et al8 required only the chronic cases to use hinged knee braces with extension blocks at 90°. While several studies advocated the use of a hip brace,3,12,13 knee braces locked at 90° of flexion were also commonly recommended.20,35 Interestingly, although hip and knee orthoses, as well as hip-knee-ankle orthoses, have been used in the scientific literature,7,18,25 they were not mentioned in any of the online protocols reviewed in our study. Also, hamstring slings, in which a strap around the waist connects to the heel of the shoe to limit knee extension, have been recommended by 2 studies but were not mentioned in online protocols.15,29 Furthermore, two studies advised postoperative splinting. Lefevre et al,23 in their prospective case series of 34 patients undergoing operative repair of acute complete proximal hamstring rupture, immobilized the knee with a splint flexed at 30° for the first postoperative week. Afterward, the splint was replaced by a custom hinged knee brace that allowed free knee flexion but limited extension at 30°. Chakravarthy et al10 used a thermoplastic splint to maintain the knee at 90° of flexion during the first 2 postoperative weeks.
Hip and Knee Range of Motion
A short period of immobilization is thought to accelerate granulation tissue formation; however, establishing early ROM is critical to prevent muscle atrophy, promote muscle strengthening, resorb scar tissue, and reperfuse damaged tissue.10,22 Across online protocols, ROM milestones were vastly underreported, as only 6 protocols (17%) provided time points for achieving full hip and knee ROM. However, 80% of protocols recommended gentle PROM starting at a mean of 1.4 weeks (range, 0-3 weeks), and 69% of protocols recommended active range of motion (AROM) starting at a mean of 4.0 weeks (range, 0-6 weeks).
ROM milestones are also variable in the scientific literature. However, some of this variability can be explained by different recommendations for acute versus chronic ruptures. Brucker and Imhoff,7 in their case series of 6 acute and 2 chronic complete proximal hamstring avulsions, expected patients to achieve full ROM between 14 and 16 weeks. On the other hand, Marx et al25 described 2 patients with allograft repair for chronic ruptures who remained nonweightbearing for 8 weeks and began active knee extension and passive flexion at 12 weeks postsurgery. For those studies focusing exclusively on acute complete proximal hamstring tendon tears, PROM and AROM start dates mirrored those of our investigation, at 2 and 4 weeks, respectively.12,13,30 Interestingly, Chakravarthy et al10 described testing the amount of knee extension intraoperatively to determine a safe ROM arc for the promotion of early passive extension.
Hamstring Stretching
The role of hamstring stretching in complete proximal hamstring rupture rehabilitation is a contentious subject. In our study, nearly half of all protocols (46%) recommended initiating hamstring-specific exercises, at a mean of 10.1 weeks (range, 6-17 weeks). In the scientific literature, hamstring stretches are rarely recommended. Rather, several studies explicitly recommend against stretching.1,15,30 In their retrospective analysis of 41 patients undergoing repair for both acute and chronic complete proximal hamstring avulsions, Sarimo et al30 noted that any form of hamstring stretch was prohibited within the first 4 weeks after surgery. More recently, both Hamersly and Schrader15 and Sallay et al29 stated that hamstring stretches were avoided entirely given the risk of repair tissue elongation, or “creep,” and the tendency for the muscle to return to length through normal activities of daily living.
Return to Training
It is well described that neglected complete ruptures of the hamstring origin can result in significant functional impairment.10,34 However, a successful repair followed by a rigorous rehabilitation program should enable patients to return to preinjury levels of activity and sport.§ In 2015, Van der Made et al34 systematically reviewed 387 operative cases and concluded that after operative repair of acute and chronic proximal hamstring avulsion, 76% to 100% of patients returned to sports, 55% to 100% returned to preinjury activity level, and 88% to 100% were highly satisfied with their surgery. In the final stages of rehabilitation, patients demonstrate competence and confidence across a range of functional and athletic activities prior to return to sport. There is widespread support for the use of functional performance tests and isokinetic strength measurements in assessing readiness for return to training.12,14,15,20,29,32 In our study, while those protocols with well-defined criteria for return to training frequently used isokinetic hamstring testing (14/15, 93%), hopping tests were rarely recommended (3/15, 20%).
Protocol Standardization
Addressing the widespread variability of rehabilitation protocols found in both professional literature and online is an important next step for researchers and clinicians alike. Standardization of physical therapy protocols after several orthopaedic procedures has been shown to be of great benefit. In total joint replacement, increased standardization of clinical pathways led to improvements in both patient outcomes and resource utilization.6,22 Additionally, standardization has been shown to enhance interdisciplinary communication and increase patient and family engagement in care.33 Our investigation revealed considerable variability with regard to both the inclusion of specific physical therapy components and the timing of when these components are introduced postoperatively. Although specific timelines for therapy progression can be expected to vary between protocols, such wide discrepancies in basic adjunctive therapies, weightbearing status, and ROM milestones are indicative of a lack of evidence-based guidelines.12 Our observation that the majority of protocols rarely provided clear, patient-directed instructions or explicit criteria for progression throughout the recovery process further highlights the lack of consensus regarding best practices.
Study Limitations
This observational study has several limitations. First, although 155 total ERAS-affiliated orthopaedic programs were considered, only 21 programs provided protocols that met the eligibility criteria. From our initial searches, it was apparent that this number represents a small minority of available online rehabilitation protocols for complete proximal hamstring repair. Many individual physicians and practice groups provide rehabilitation protocols on personalized websites. As a result, the data pool was supplemented with non-ERAS-affiliated protocols that were readily and consistently available via a commonly used web-based search engine. In our attempt to better characterize the variability of rehabilitation protocols that are easily accessible to patients, the protocols were not stratified but rather were assessed as a single collective group. Notably, this method was used in a prior investigation evaluating quality and variability of anterior cruciate liagment rehabilitation and was selected in an effort to identify a series of comparable protocols while minimizing selection bias.24
Additionally, while the included rehabilitation protocols were limited to complete proximal hamstring tendon ruptures, the protocols themselves rarely specified rupture chronicity and operative technique. For example, it is reasonable to expect that operative management in the acute setting would involve primary repair1,3,28; however, depending on the level of tendon retraction, graft assistance could be necessary. Certainly, postoperative management could differ between acute versus chronic and primary versus graft-assisted repairs; these discrepancies are potential confounders that could influence the course of rehabilitation. Moreover, as Cohen and Bradley12 described in 2007, the patient populations most affected by this uncommon injury are elite-level athletes and middle-aged individuals. None of the online protocols reviewed in this investigation designated a specific target population with respect to the age and athletic status of patients. As with variation in operative technique, it would be expected that the postoperative recovery process would differ between these 2 demographics.
Last, our study is limited by potential barriers to the use of multimedia by the studied institutions. It is unrealistic to assume that all programs have a particular goal to increase the dissemination of publicly available information through online content. Our study merely sought to detect the presence or absence of said material but did not investigate whether the presence would be helpful to the community each institution serves. Despite the aforementioned limitations, given the overall trend toward the use of online content, our findings reveal a specific area for improving patient education and health care content access with regard to rehabilitation after operative management of complete proximal hamstring rupture.
Conclusion
In conclusion, this study demonstrates the marked variability in both the composition and timing of rehabilitation components across the few academic complete proximal hamstring repair rehabilitation protocols that are published online. This finding mirrors the variability of proposed rehabilitation protocols in the professional literature. Such variability, with the corresponding lack of outcome-based studies to establish guidelines, represents an opportunity for future research to increase access to more evidence-based, standardized health care content.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: C.S.A. receives royalties from Arthrex; receives research support from Arthrex, Major League Baseball, and Stryker; has stock/stock options in At Peak; and receives publishing royalties from Lead Player.
Ethical approval was not sought for the present study.
References
- 1. Askling CM, Koulouris G, Saartok T, Werner S, Best TM. Total proximal hamstring ruptures: clinical and MRI aspects including guidelines for postoperative rehabilitation. Knee Surg Sports Traumatol Arthrosc. 2013;21:515–533. [DOI] [PubMed] [Google Scholar]
- 2. Bencardino JT, Mellado JM. Hamstring injuries of the hip. Magn Reson Imaging Clin N Am. 2005;13:677–690. [DOI] [PubMed] [Google Scholar]
- 3. Birmingham P, Muller M, Wickiewicz T, Cavanaugh J, Rodeo S, Warren R. Functional outcome after repair of proximal hamstring avulsions. J Bone Joint Surg Am. 2011;93(19):1819–1826. [DOI] [PubMed] [Google Scholar]
- 4. Blakeney WG, Zilko SR, Edmonston SJ, Schupp NE, Annear PT. A prospective evaluation of proximal hamstring tendon avulsions: improved functional outcomes following surgical repair. Knee Surg Sports Traumatol Arthrosc. 2017;25(6):1943–1950. [DOI] [PubMed] [Google Scholar]
- 5. Blakeney WG, Zilko SR, Edmonston SJ, Schupp NE, Annear PT. Proximal hamstring tendon avulsion surgery: evaluation of the Perth Hamstring Assessment Tool. Knee Surg Sports Traumatol Arthrosc. 2017;25:1936–1942. [DOI] [PubMed] [Google Scholar]
- 6. Bozic KJ, Maselli J, Pekow PS, Lindenauer PK, Vail TP, Auerbach AD. The influence of procedure volumes and standardization of care on quality and efficiency in total joint replacement surgery. J Bone Joint Surg Am. 2010;92:2643–2652. [DOI] [PubMed] [Google Scholar]
- 7. Brucker PU, Imhoff AB. Functional assessment after acute and chronic complete ruptures of the proximal hamstring tendons. Knee Surg Sports Traumatol Arthrosc. 2005;13:411–418. [DOI] [PubMed] [Google Scholar]
- 8. Carmichael J, Packham I, Trikha SP, et al. Avulsion of the proximal hamstring origin: surgical technique. J Bone Joint Surg Am. 2009;91:249–256. [DOI] [PubMed] [Google Scholar]
- 9. Chahal J, Bush-Joseph CA, Chow A, et al. Clinical and magnetic resonance imaging outcomes after surgical repair of complete proximal hamstring ruptures: does the tendon heal? Am J Sports Med. 2012;40:2325–2330. [DOI] [PubMed] [Google Scholar]
- 10. Chakravarthy J, Ramisetty N, Pimpalnerkar A, et al. Surgical repair of complete proximal hamstring tendon ruptures in water skiers and bull riders: a report of four cases and review of the literature. Br J Sports Med. 2005;39:569–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Clanton TO, Coupe KJ. Hamstring strains in athletes: diagnosis and treatment. J Am Acad Orthop Surg. 1998;6:237–248. [DOI] [PubMed] [Google Scholar]
- 12. Cohen S, Bradley J. Acute proximal hamstring rupture. J Am Acad Orthop Surg. 2007;15:350–355. [DOI] [PubMed] [Google Scholar]
- 13. Cohen SB, Rangavajjula A, Vyas D, Bradley JP. Functional results and outcomes after repair of proximal hamstring avulsions. Am J Sports Med. 2012;40:2092–2098. [DOI] [PubMed] [Google Scholar]
- 14. Folsom GJ, Larson CM. Surgical treatment of acute versus chronic complete proximal hamstring ruptures: results of a new allograft technique for chronic reconstructions. Am J Sports Med. 2008;36:104–109. [DOI] [PubMed] [Google Scholar]
- 15. Hamersly SF, Schrader M. Postoperative rehabilitation of proximal hamstring tendon tears. Oper Tech Sports Med. 2009;17:219–224. [Google Scholar]
- 16. Harris JD, Griesser MJ, Best TM, Ellis TJ. Treatment of proximal hamstring ruptures—a systematic review. Int J Sports Med. 2011;32:490–495. [DOI] [PubMed] [Google Scholar]
- 17. Järvinen TAH, Järvinen TLN, Kääriäinen M, Kalimo H, Järvinen M. Muscle injuries: biology and treatment. Am J Sports Med. 2005;33:745–764. [DOI] [PubMed] [Google Scholar]
- 18. Kirkland A, Garrison C, Singleton S, Rodrigo J, Boettner F, Stuckey S. Surgical and therapeutic management of a complete proximal hamstring avulsion after a failed conservative approach. J Orthop Sports Phys Ther. 2008;38:754–760. [DOI] [PubMed] [Google Scholar]
- 19. Klingele KE, Sallay P. Surgical repair of complete proximal hamstring tendon rupture. Am J Sports Med. 2002;30:742–747. [DOI] [PubMed] [Google Scholar]
- 20. Konan S, Haddad F. Successful return to high level sports following early surgical repair of complete tears of the proximal hamstring tendons. Int Orthop. 2010;34:119–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Koulouris G, Connell D. Evaluation of the hamstring muscle complex following acute injury. Skeletal Radiol. 2003;32:582–589. [DOI] [PubMed] [Google Scholar]
- 22. Kujala UM, Orava S, Järvinen M. Hamstring injuries. Sports Med. 1997;23(6):397–404. [DOI] [PubMed] [Google Scholar]
- 23. Lefevre N, Bohu Y, Naouri JF, Klouche S, Herman S. Returning to sports after surgical repair of acute proximal hamstring ruptures. Knee Surg Sports Traumatol Arthrosc. 2013;21(3):534–539. [DOI] [PubMed] [Google Scholar]
- 24. Makhni EC, Crump EK, Steinhaus ME, et al. Quality and variability of online available physical therapy protocols from academic orthopaedic surgery programs for anterior cruciate ligament reconstruction. Arthroscopy. 2016;32:1612–1621. [DOI] [PubMed] [Google Scholar]
- 25. Marx RG, Fives G, Chu SK, et al. Allograft reconstruction for symptomatic chronic complete proximal hamstring tendon avulsion. Knee Surg Sports Traumatol Arthrosc. 2009;17:19–23. [DOI] [PubMed] [Google Scholar]
- 26. Mica L, Schwaller A, Stoupis C, Penka I, Vomela J, Vollenweider A. Avulsion of the hamstring muscle group: a follow-up of 6 adult non-athletes with early operative treatment: a brief report. World J Surg. 2009;33:1605–1610. [DOI] [PubMed] [Google Scholar]
- 27. Moatshe G, Chahla J, Vap AR, et al. Repair of proximal hamstring tears: a surgical technique. Arthrosc Tech. 2017;30:6(2):311–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rust DA, Giveans MR, Stone RM, Samuelson KM, Larson CM. Functional outcomes and return to sports after acute repair, chronic repair, and allograft reconstruction for proximal hamstring ruptures. Am J Sports Med. 2014;42:1377–1383. [DOI] [PubMed] [Google Scholar]
- 29. Sallay PI, Ballard G, Hamersly S, Schrader M. Subjective and functional outcomes following surgical repair of complete ruptures of the proximal hamstring complex. Orthopedics. 2008;31:1092. [PubMed] [Google Scholar]
- 30. Sarimo J, Lempainen L, Mattila K, Orava S. Complete proximal hamstring avulsions: a series of 41 patients with operative treatment. Am J Sports Med. 2008;36:1110–1115. [DOI] [PubMed] [Google Scholar]
- 31. Sherry MA, Best TM. A comparison of 2 rehabilitation programs in the treatment of acute hamstring strains. J Orthop Sports Phys Ther. 2004;34:116–125. [DOI] [PubMed] [Google Scholar]
- 32. Skaara HE, Moksnes H, Frihagen F, Stuge B. Self-reported and performance-based functional outcomes after surgical repair of proximal hamstring avulsions. Am J Sports Med. 2013;41:2577–2584. [DOI] [PubMed] [Google Scholar]
- 33. Van Citters AD, Fahlman C, Goldmann DA, et al. Developing a pathway for high-value, patient-centered total joint arthroplasty. Clin Orthop Relat Res. 2014;472:1619–1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Van der Made AD, Reurink G, Gouttebarge V, Tol JL, Kerkhoffs GM. Outcome after surgical repair of proximal hamstring avulsions: a systematic review. Am J Sports Med. 2015;43:2841–2851. [DOI] [PubMed] [Google Scholar]
- 35. Wood DG, Packham I, Trikha SP, Linklater J. Avulsion of the proximal hamstring origin. J Bone Join Surg Am. 2008;90:2365–2374. [DOI] [PubMed] [Google Scholar]
- 36. Worrell TW. Factors associated with hamstring injuries: an approach to treatment and preventative measures. Sports Med. 1994;17:338–345. [DOI] [PubMed] [Google Scholar]