Abstract
Background:
Youth baseball is extremely popular in the United States, but it has been associated with shoulder pain and injury. The incidence of shoulder abnormalities in this athletic population has yet to be defined.
Purpose:
To examine abnormalities noted on magnetic resonance imaging (MRI) in the shoulders of asymptomatic Little League baseball players and to correlate these findings with the players’ throwing history and physical examinations.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
A total of 23 Little League baseball players aged 10 to 12 years were recruited. All players underwent a comprehensive physical examination and responded to a questionnaire addressing their playing history and any arm or shoulder pain. Bilateral shoulder MRIs were performed and read in a blinded manner by 2 radiologists. Responses on the questionnaire and physical examination findings were compared between participants with and without positive MRI findings through use of chi-square test and analysis of variance.
Results:
The dominant arm was 8.5 times more likely to have an abnormality on MRI compared with the nondominant arm. In all, 12 players (52%) had 17 positive MRI findings in their throwing shoulder that were not present in their nondominant shoulder. These findings included edema or widening of the proximal humeral physis (n = 5), labral tear (n = 4), partial rotator thickness tear (n = 4), acromioclavicular joint abnormality (n = 2), subacromial bursitis (n = 1), and cystic change of the greater tuberosity (n = 1). Two primary risk factors were associated with an abnormal MRI: year-round play and single-sport athletes focusing solely on baseball (P < .05). Players with no risk factors, 1 risk factor, and both risk factors had a 25%, 71%, and 100% chance, respectively, of having an abnormal MRI. A majority of players (61%) had previously experienced shoulder pain, especially pitchers throwing curveballs and sliders (P < .05), but this was not associated with an abnormal MRI.
Conclusion:
Abnormalities seen on MRI involving the shoulder are common in Little League baseball players, especially those who are single-sport athletes playing year-round.
Keywords: youth baseball, Little League shoulder, rotator cuff tears, magnetic resonance imaging
Each year more than 2.5 million American children play Little League baseball.13,28 While this participation provides many benefits for the young athlete, youth baseball is also responsible for a growing number of overuse injuries.12 Approximately 20% of baseball players between the ages of 8 and 12 years will experience arm pain during a single youth baseball season.12,13,26,27 This is particularly concerning given that this injury rate has increased over the past 2 decades.6 Multiple potential risk factors may be responsible, including year-round play, pitching for more than 1 team, pitch velocity, player height and weight, and loss of shoulder internal rotation.1,9,18,19,22
The shoulder is frequently injured in Little League athletes.13 Common diagnoses include labral tears, rotator cuff injury, internal impingement lesions, and growth plate abnormalities. Many of these diagnoses have long-term implications, sometimes necessitating surgery and putting young athletes at risk for future shoulder arthritis and disability.10
While heightened awareness of these injuries has resulted in the institution of Little League pitching guidelines, few scientific studies have critically assessed injury patterns in Little League athletes. The purpose of the current study was to examine magnetic resonance imaging (MRI) abnormalities in the shoulders of asymptomatic Little League baseball players and to correlate these findings with the players’ throwing history and physical examinations. We hypothesized that pitchers as well as year-round baseball players would have a greater incidence of abnormalities of the shoulder.
Methods
After internal review board approval was obtained, 23 Little League baseball players were enrolled in and gave consent for this study. Players were recruited from a single Little League district in Southern California after the team rosters were created but prior to the start of any games. Players were recruited from the “major division,” or highest league within the district. Four teams existed within the major division, each with 10 to 12 players. Prior to recruitment, the research team was present at the Little League registration as well as at tryouts to interact with families, familiarize them with the study, and answer any questions. Recruitment was voluntary and was conducted on a first-come, first-served basis, given that our budget allowed us to study only 23 or 24 players. Patients were considered asymptomatic if they were currently pain free, had never seen a clinician for any shoulder problem, and had never received treatment for a shoulder problem. Patients ranged in age from 10 to 12 years; exclusion criteria entailed any contraindication to an MRI or inability to tolerate the MRI. No participants were excluded from the study, and all were able to complete the MRI.
A detailed history was taken on each player. The throwing history focused on several key factors, including years of play, primary positions played, months of play per year, number of teams on which each player had participated, private coaching history, and age at which various pitches (change-ups, sliders, and curveballs) were initiated. Participants were asked whether they had a prior history of arm pain or throwing injury. Additionally, participants were asked whether they were familiar with the Little League throwing guidelines and whether they had ever exceeded these guidelines.
A detailed physical examination of both upper extremities, including range of motion (ROM), strength, and stability testing, was performed by 1 of 2 orthopaedic surgeons (A.T.P., J.M.). Prior to the examination, the surgeons standardized their testing approach. All angular measurements were performed with an electronic inclinometer. Manual strength testing was performed bilaterally and graded on a scale of 1 to 5 (5 being strongest). Shoulder instability was defined as a positive physical examination finding for any of the following: apprehension test, Jobe relocation test, or posterior load and shift testing. Elbow instability was defined as a side-to-side difference with valgus or varus stress. Each patient then underwent bilateral shoulder MRIs with a GE HDxT 3.0-T MRI scanner with the following sequences: axial T1-weighted (echo time [TE] 12-13 ms; repetition time [TR] 580-610 ms), axial inversion recovery (TE 45-50 ms; TR 3475-3500 ms), sagittal T2-weighted MERGE (multiple echo recombined gradient echo; TE 13.5-14 ms; TR 600-650 ms), coronal inversion recovery (TE 45-50 ms; TR 3475-3500 ms), and coronal T2-weighted fat-saturated (TE 64-70 ms; TR 2020-2070 ms). A single radiologist (J.D.) with a clinical focus on pediatric musculoskeletal imaging read all of the MRI images and was blinded as to any history of arm pain or the arm dominance of the player. The radiologist filled out a data sheet with dichotomized responses that allowed only positive or negative responses to the presence or absence of each abnormality. Bilateral shoulder ultrasonography was performed to assess humeral torsion, as previously described.17
Players who reported a history of shoulder pain or injury from baseball were compared with players who had a negative history in terms of clinical examination, questionnaire data, and MRI findings. The clinical examination and questionnaire data for players whose MRI results indicated an abnormality of their dominant arm (not present in the nondominant arm) were compared with the data for players whose MRI results did not indicate dominant-arm abnormality. These comparisons were made through use of chi-square test for categorical variables and analysis of variance (ANOVA) for interval data. The prevalence of particular findings (ie, a positive sulcus sign) was compared through use of z ratio for the significance of the difference between 2 independent proportions. Dominant versus nondominant findings were compared by use of repeated-measures ANOVA or McNemar test. All interval data were checked for normality and homogeneity of variance prior to application of parametric statistics. Alpha was set at P < .05, and all analyses were performed through use of SPSS v12 (SPSS Inc).
Results
The average age of the cohort was 11.4 years (range, 10-12 years) and all baseball players were boys. The majority of players were right-hand dominant (19/23, 83%). The participants had been playing on average for 6.4 years, and 43% were “year-round baseball players” (indicating they played at least 8 months per year); 22% (5/23) of the athletes played only baseball and no other sports. All participants played a variety of positions, but 65% of athletes listed themselves as pitchers and 26% listed themselves as catchers; 17% of the players had attended private baseball camps or used a private pitching or throwing coach. The majority of the athletes (83%) were aware that Little League baseball has pitching guidelines and stated that they had been compliant with these guidelines. The throwing history data are summarized in Table 1.
TABLE 1.
Player Responses to Baseball History Questionnaire
| Player Response, n (%) | ||
|---|---|---|
| No | Yes | |
| Primary positions | ||
| Pitching | 8 (35) | 15 (65) |
| Catching | 17 (74) | 6 (26) |
| Infield or outfield | 15 (65) | 8 (35) |
| Play year-round (≥8 months) | 13 (57) | 10 (43) |
| Play on multiple teams during the year | 11 (48) | 12 (52) |
| Private coaching | 19 (83) | 4 (17) |
| Single-sport athlete | 18 (78) | 5 (22) |
| Report baseball-related elbow or shoulder pain or injury | 4 (17) | 19 (83) |
| Know the Little League throwing guidelines | 4 (17) | 19 (83) |
| Pitchers only (n = 15) | ||
| Threw curveballs in past 12 months | 3 (20) | 12 (80) |
| Threw sliders/cutters/sinkers in past 12 months | 12 (80) | 3 (20) |
| Age started organized pitching, average (range), y | 8.2 (7-10) | |
The baseline physical examination findings are recorded in Table 2. Shoulder motion was asymmetric between the dominant and nondominant arms, revealing decreased internal rotation of 7° in the dominant arm (P < .01). A greater than 10° deficit in internal rotation in the dominant arm was present in 26% of players. Otherwise, no significant differences were identified between the dominant and nondominant arms with respect to elbow or shoulder stability, elbow ROM, carrying angle, or tenderness to palpation. The humeral torsion measurements revealed 5° of retrotorsion of the dominant arm compared with the nondominant arm.
TABLE 2.
Clinical Examination Findingsa
| Dominant | Nondominant | P | |
|---|---|---|---|
| Shoulder internal rotation, deg, mean ± SD | 40 ± 15 | 47 ± 16 | <.001b |
| Shoulder external rotation, deg, mean ± SD | 89 ± 15 | 88 ± 13 | .25 |
| Shoulder tenderness to palpation | 0 (0) | 0 (0) | N/Ac |
| Sulcus sign | 8 (43) | 9 (52) | .99 |
| Shoulder instability | 0 (0) | 0 (0) | N/Ac |
| Impingement test | 0 (0) | 0 (0) | N/Ac |
| O’Brien test | 3 (13) | 5 (22) | .5 |
| Rotator cuff weakness | 0 (0) | 0 (0) | N/Ac |
aAt least 1 variable in each 2-way table upon which measures of association are computed is a constant. Values are presented as n (% positive) unless otherwise specified. N/A, not available.
bStatistically significant difference (P < .05).
cMcNemar P value cannot be calculated.
In all, 83% of the players responded positively to having experienced arm pain from throwing, and 61% had previously experienced shoulder pain. None of these players had sought medical attention, received a formal diagnosis of their pain, or required any special treatment. A history of shoulder pain was associated with player position (pitchers) and more specifically with pitchers throwing curveballs or cutters, sliders, or sinkers (P < .05). Otherwise, a history of arm pain was not associated with players’ demographics, their baseball history, or their physical examination findings.
Overall, 17 asymmetric MRI abnormalities were observed in the dominant shoulders of 12 players, representing 52% of the cohort, and 4 of these 12 players had multiple abnormalities. By comparison, the nondominant arm MRIs revealed only 2 abnormalities, representing a 6-fold higher rate of abnormality in the throwing arm of these athletes. The most common abnormality was edema or widening of the proximal humeral physis (5 players), followed by labral tear (4 players), partial rotator thickness tear (4 players), hypertrophy of the acromioclavicular joint capsule (2 players), subacromial bursitis (1 player), and cystic change of the greater tuberosity (1 player) (Figures 1 –3). All of the abnormalities involving the rotator cuff were partial articular-sided tears measuring less than 50% of the thickness of the cuff. All involved the supraspinatus tendon, but 1 extended into the infraspinatus. The abnormalities involving the labrum included 2 anterosuperior labral tears, 1 anterior labral tear, and 1 posterosuperior labral tear. The 2 abnormal MRIs of the nondominant arm were both labral tears. The physeal width as measured by MRI was 1.4 mm in the dominant arm compared with 1.3 mm in the nondominant arm (P > .05).
Figure 1.
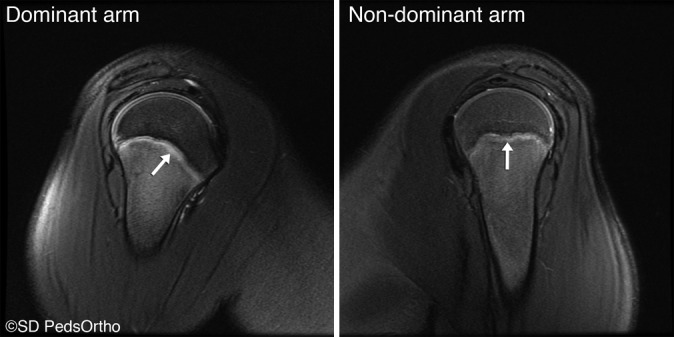
Sagittal T2-weighted fat-suppressed image demonstrating periphyseal edema. (Reprinted with permission from San Diego Pediatric Orthopedics.)
Figure 2.
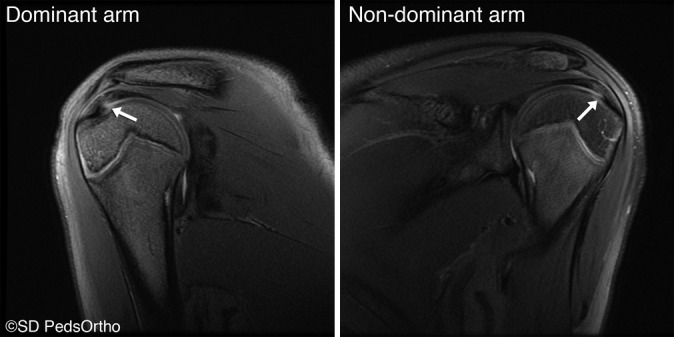
Coronal T2-weighted fat-suppressed image demonstrating a partial articular-sided rotator cuff tear involving the supraspinatus. (Reprinted with permission from San Diego Pediatric Orthopedics.)
Figure 3.
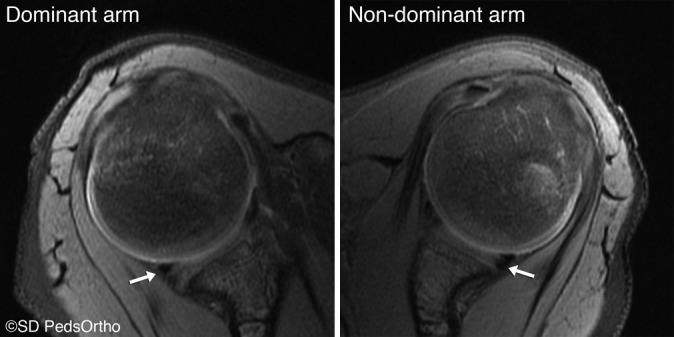
Axial proton density fat-suppressed image demonstrating a posterior labral tear. (Reprinted with permission from San Diego Pediatric Orthopedics.)
Abnormal MRI findings did not correlate with player position, years of play, compliance with Little League throwing guidelines, or a prior history of arm or shoulder pain. Instead, MRI abnormalities were associated with 2 factors: year-round play and single-sport participation (P < .05). Players with neither of these risk factors had a 25% chance of having an abnormal MRI. Players with 1 risk factor had a 71% chance of having an abnormal MRI, and players with both risk factors had a 100% chance of having an abnormal MRI. Table 3 summarizes the rate of abnormalities based on the possible combinations of these 2 associated variables. Players with an abnormal MRI played an average of 9.1 months of baseball per year, whereas players with normal MRIs averaged 6.3 months of play per year (P < .01).
TABLE 3.
Prevalence of Positive MRI Findings Based on Number of Associated Factorsa
| Positive MRI, n (%) | |||
|---|---|---|---|
| No. of Associated Factors | No | Yes | |
| 0 | Not year-round, not single-sport specialized | 9 (75) | 3 (25) |
| 1 | Year-round or single sport specialized | 2 (29) | 5 (71) |
| 2 | Year-round and single sport specialized | 0 (0) | 4 (100) |
aMRI, magnetic resonance imaging.
Discussion
A large percentage of Little League players aged 10 to 12 years (52%) were found to have MRI abnormalities of the shoulder, primarily involving the physis, the labrum, and the rotator cuff. These abnormalities were correlated with year-round play and single-sport specialization. Additionally, a large percentage of these players had a history of shoulder pain despite the fact that all of them began their baseball careers after implementation of the Little League throwing guidelines and nearly all of the players were aware of and compliant with these guidelines.
Radiographic abnormalities in the dominant arm of baseball players have been well documented in the literature. Asymptomatic rotator cuff tears and labral tears have been shown to be present in 21%-52% and 40%-48% of Major League Baseball pitchers, respectively.2,4,11,15 Imaging studies have also shown that degenerative changes of the acromioclavicular joint (21%-29%) and cystic changes of the humeral head (36%-76%) are common in these professional athletes.4,11,15,23 These radiographic abnormalities likely represent cumulative degenerative changes of the shoulder and have been associated with patient age and total innings pitched. From the literature, it is unclear at what point in an athlete’s career these abnormalities develop. One study focusing on asymptomatic pitchers with an age range of 17 to 22 years showed a similar rate of rotator cuff tears (32%) and labral tears (42%) compared with the professional pitchers.4 To date, no study has looked at younger throwers, particularly those who are of Little League age. The results of the current study suggest that these changes are occurring much earlier than previously recognized. Historically, authors have suggested that the weak link in the young thrower’s shoulder is the physis, which is prone to epiphysiolysis or Little League shoulder.3 While our study clearly shows that the physis is being stressed and altered in these young throwers, damage is also occurring to the labrum, rotator cuff, and acromioclavicular joint, representing structural abnormalities that might put these youth at increased risk of future pain, surgery, and disability. Clinicians need to be aware of the frequency of these radiographic abnormalities in baseball players, especially when interpreting the results of MRI scans obtained in this unique athletic population.
The results of the current study identified 2 risk factors for MRI abnormalities of the shoulder: year-round play and single-sport specialization. Previous studies have shown that shoulder pain is more closely associated with the cumulative number of hard throws over the course of a season than with the actual number of pitches in a game.4,7,13 Our data also suggest that MRI abnormalities are driven more by months of play than by position. In fact, 38% of nonpitchers in our study had an MRI abnormality of the shoulder. Year-round play was also recently shown to be the most significant risk factor for MRI abnormalities of the elbow in asymptomatic Little League players.19,20 Furthermore, the current study showed that 100% of “specialized” single-sport athletes with a focus on baseball had an abnormal MRI. This finding mirrors other recent data showing that the odds of an overuse injury are greater in athletes participating in a single sport year-round.8
While the results of this study revealed that physeal changes including edema and widening of the proximal humeral physis are common, the results also demonstrated that torsional differences exist between the dominant and nondominant arms of these young throwers. Our cohort revealed a relatively symmetric change in shoulder ROM rotation of the dominant arm relative to the nondominant arm, with internal rotation decreasing by 7°. This compared similarly to ultrasonographic torsion measurements, which showed that the humerus was 5° retroverted in the dominant arm relative to the nondominant arm. This bony adaptation has been well documented in young baseball players as well as professional baseball pitchers and is believed to occur secondary to morphological adaptations resulting from throwing prior to skeletal maturity. Shear stress arising from high torque during the arm-cocking phase of throwing produces deformation of the relatively weak proximal humeral epiphyseal cartilage, causing humeral retrotorsion.21 Some investigators have hypothesized that this process may be protective against shoulder injury, but this theory has yet to be confirmed.14,24 In contrast, glenohumeral internal rotation deficit secondary to contracture of the posterior capsule is not believed to be compensatory but is likely pathological and has been associated with shoulder and elbow injury in throwing athletes.16,21,24,25 In our cohort, 30% of the players had an internal rotation deficit of at least 10°. Interestingly, rates of MRI abnormalities were not significantly associated with loss of shoulder internal rotation, but our study was potentially underpowered to detect this difference.
Over the past decade, increased recognition of Little League throwing injuries has led to the development of several injury prevention and awareness campaigns, such as Sports Trauma and Overuse Prevention (STOP) and PitchSmart. Pitch count restrictions and mandatory rest days are now required of Little League pitchers.5 These rules have been effectively instituted in most Little Leagues in the United States. For example, in the case of our athletes, nearly all players were aware of the guidelines and reported never having violated these restrictions. A major limitation of programs such as STOP and PitchSmart, however, is that while they make recommendations about position play, avoiding year-round play (4 months off per year), and postponing off-speed pitches (sliders and curveballs) until later in the athlete’s development, these recommendations are not enforced. In the current study, many athletes (43%) played baseball more than 8 months per year, 22% were single-sport “specialized” athletes, and 80% of pitchers threw curveballs, sliders, and sinkers. Until these larger issues are addressed, the epidemic of throwing injuries in the United States is unlikely to change.
This study had several limitations. First, patient recruitment was performed at a single competitive Little League program in Southern California, where year-round baseball is common. Therefore, it is unclear how these data extrapolate to other leagues across the United States. Second, radiographic assessment of the shoulder was not performed because of radiation exposure concerns. It is unclear whether radiographs would have been more sensitive at picking up subtle bony changes about the physis. Third, patient histories, especially pertaining to pain and player position, were obtained retrospectively and thus are subject to recall bias; it is not clear when exactly the patients had experienced previous pain relative to their preseason MRI. Fourth, cost restraints limited the recruitment and imaging to only 23 athletes (46 shoulders). A larger cohort would have enabled further data analysis and risk stratification. Fifth, patient motivation for participating in the study was not known; patients with current pain or a history of pain potentially had more motivation to participate in the study. Other limitations of this study are that we included only male athletes, and we do not know the longer term implications of the noted abnormalities. These are important questions to address in future studies.
In conclusion, MRI abnormalities involving the shoulder are common in Little League baseball players, especially those who play baseball more than 8 months per year and who are single-sport athletes. While Little League guidelines potentially decrease injuries in pitchers, these guidelines require further refinement addressing year-round play, early sports specialization, pitch type, and pain. It is hoped that addressing these issues will decrease the high prevalence of arm pain and radiographic abnormalities in this throwing population.
Acknowledgment
The authors thank Lacey Lee and Mike Frederick from Sharp and Children’s MRI Center, LLC, for scheduling and performing the MRIs for this study. The authors also thank James Bomar from Rady Children’s Hospital for preparing the figures for this manuscript.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was funded by the Rady Children’s Hospital 2016 Academic Enrichment Grant.
Ethical approval for this study was obtained from the University of California—San Diego Human Research Protections Program.
References
- 1. Chalmers PN, Sgroi T, Riff AJ, et al. Correlates with history of injury in youth and adolescent pitchers. Arthroscopy. 2015;31(7):1349–1357. [DOI] [PubMed] [Google Scholar]
- 2. Connor PM, Banks DM, Tyson AB, et al. Magnetic resonance imaging of the asymptomatic shoulder of overhead athletes: a 5-year follow-up study. Am J Sports Med. 2003;31(5):724–727. [DOI] [PubMed] [Google Scholar]
- 3. Curtis R. Shoulder injuries in young athletes In DeLee & Drez’s Orthopaedic Sports Medicine. Philadelphia, PA: Elsevier: 2014:1864. [Google Scholar]
- 4. Del Grande F, Aro M, Jalali Farahani S, et al. High-resolution 3-T magnetic resonance imaging of the shoulder in nonsymptomatic professional baseball pitcher draft picks. J Comput Assist Tomogr. 2016;40(1):118–125. [DOI] [PubMed] [Google Scholar]
- 5. Fazarale JJ, Magnussen RA, Pedroza AD, et al. Knowledge of and compliance with pitch count recommendations: a survey of youth baseball coaches. Sports Health. 2012;4(3):202–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fleisig GS, Andrews JR. Prevention of elbow injuries in youth baseball pitchers. Sports Health. 2012;4(5):419–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fleisig GS, Andrews JR, Cutter GR, et al. Risk of serious injury for young baseball pitchers: a 10-year prospective study. Am J Sports Med. 2011;39(2):253–257. [DOI] [PubMed] [Google Scholar]
- 8. Hall R, Barber Foss K, Hewett TE, et al. Sport specialization’s association with an increased risk of developing anterior knee pain in adolescent female athletes. J Sport Rehabil. 2015;24(1):31–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Harada M, Takahara M, Mura N, et al. Risk factors for elbow injuries among young baseball players. J Shoulder Elbow Surg. 2010;19(4):502–507. [DOI] [PubMed] [Google Scholar]
- 10. Kim YS, Kim SE, Bae SH, et al. Tear progression of symptomatic full-thickness and partial-thickness rotator cuff tears as measured by repeated MRI. Knee Surg Sports Traumatol Arthrosc. 2017;25(7):2073–2080. [DOI] [PubMed] [Google Scholar]
- 11. Lesniak BP, Baraga MG, Jose J, et al. Glenohumeral findings on magnetic resonance imaging correlate with innings pitched in asymptomatic pitchers. Am J Sports Med. 2013;41(9):2022–2027. [DOI] [PubMed] [Google Scholar]
- 12. Lyman S, Fleisig GS, Andrews JR, et al. Effect of pitch type, pitch count, and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am J Sports Med. 2002;30(4):463–468. [DOI] [PubMed] [Google Scholar]
- 13. Lyman S, Fleisig GS, Waterbor JW, et al. Longitudinal study of elbow and shoulder pain in youth baseball pitchers. Med Sci Sports Exerc. 2001;33(11):1803–1810. [DOI] [PubMed] [Google Scholar]
- 14. Meister K, Day T, Horodyski M, et al. Rotational motion changes in the glenohumeral joint of the adolescent/Little League baseball player. Am J Sports Med. 2005;33(5):693–698. [DOI] [PubMed] [Google Scholar]
- 15. Miniaci A, Mascia AT, Salonen DC, et al. Magnetic resonance imaging of the shoulder in asymptomatic professional baseball pitchers. Am J Sports Med. 2002;30(1):66–73. [DOI] [PubMed] [Google Scholar]
- 16. Nakamizo H, Nakamura Y, Nobuhara K, et al. Loss of glenohumeral internal rotation in little league pitchers: a biomechanical study. J Shoulder Elbow Surg. 2008;17(5):795–801. [DOI] [PubMed] [Google Scholar]
- 17. Noonan TJ, Shanley E, Bailey LB, et al. Professional pitchers with glenohumeral internal rotation deficit (GIRD) display greater humeral retrotorsion than pitchers without GIRD. Am J Sports Med. 2015;43(6):1448–1454. [DOI] [PubMed] [Google Scholar]
- 18. Olsen SJ II, Fleisig GS, Dun S, et al. Risk factors for shoulder and elbow injuries in adolescent baseball pitchers. Am J Sports Med. 2006;34(6):905–912. [DOI] [PubMed] [Google Scholar]
- 19. Pennock AT, Pytiak A, Stearns P, et al. Preseason assessment of radiographic abnormalities in elbows of Little League baseball players. J Bone Joint Surg Am. 2016;98(9):761–767. [DOI] [PubMed] [Google Scholar]
- 20. Pytiak AV, Stearns P, Bastrom TP, et al. Are the current Little League pitching guidelines adequate? A single-season prospective MRI study. Orthop J Sports Med. 2017;5(5):23259 67117704851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sabick MB, Kim YK, Torry MR, et al. Biomechanics of the shoulder in youth baseball pitchers: implications for the development of proximal humeral epiphysiolysis and humeral retrotorsion. Am J Sports Med. 2005;33(11):1716–1722. [DOI] [PubMed] [Google Scholar]
- 22. Shitara H, Kobayashi T, Yamamoto A, et al. Prospective multifactorial analysis of preseason risk factors for shoulder and elbow injuries in high school baseball pitchers. Knee Surg Sports Traumatol Arthrosc. 2017;25(10):3303–3310. [DOI] [PubMed] [Google Scholar]
- 23. Wright RW, Steger-May K, Klein SE. Radiographic findings in the shoulder and elbow of Major League Baseball pitchers. Am J Sports Med. 2007;35(11):1839–1843. [DOI] [PubMed] [Google Scholar]
- 24. Wyland DJ, Pill SG, Shanley E, et al. Bony adaptation of the proximal humerus and glenoid correlate within the throwing shoulder of professional baseball pitchers. Am J Sports Med. 2012;40(8):1858–1862. [DOI] [PubMed] [Google Scholar]
- 25. Yamamoto N, Itoi E, Minagawa H, et al. Why is the humeral retroversion of throwing athletes greater in dominant shoulders than in nondominant shoulders? J Shoulder Elbow Surg. 2006;15(5):571–575. [DOI] [PubMed] [Google Scholar]
- 26. Yang J, Mann BJ, Guettler JH, et al. Risk-prone pitching activities and injuries in youth baseball: findings from a national sample. Am J Sports Med. 2014;42(6):1456–1463. [DOI] [PubMed] [Google Scholar]
- 27. Yukutake T, Nagai K, Yamada M, et al. Risk factors for elbow pain in Little League baseball players: a cross-sectional study focusing on anthropometric characteristics. J Sports Med Phys Fitness. 2015;55(9):962–968. [PubMed] [Google Scholar]
- 28. Yukutake T, Yamada M, Aoyama T. A survey examining the correlations between Japanese Little League baseball coaches’ knowledge of and compliance with pitch count recommendations and player elbow pain. Sports Health. 2013;5(3):239–243. [DOI] [PMC free article] [PubMed] [Google Scholar]


