ABSTRACT
Dalbavancin activity was assessed against a large collection of Staphylococcus aureus isolates (n = 59,903), including isolates with decreased susceptibility to vancomycin (MIC, ≥2 mg/liter; n = 1,141), daptomycin (MIC, ≥2 mg/liter; n = 48), telavancin (MIC, ≥0.12 mg/liter; n = 52), teicoplanin (MIC, ≥4 mg/liter; n = 143), and/or linezolid (MIC, ≥8 mg/liter; n = 25). Dalbavancin displayed susceptibility rates ranging from 90.4% (isolates with telavancin MIC ≥0.12 mg/liter) to 100.0% (linezolid-resistant isolates) and lower MIC values than the comparators against these resistant subsets.
KEYWORDS: glycopeptides, lipoglycopeptides, vancomycin-intermediate S. aureus
TEXT
Staphylococcus aureus continues to be a major cause of community-acquired and health care-associated infections, including skin and skin structure infections, pneumonia, bacteremia, endocarditis, osteomyelitis, prosthetic joint infections, and catheter-related infections (1). The prevalence of nosocomial infections caused by methicillin-resistant S. aureus (MRSA) has remained markedly high in the United States in the last years (2, 3).
Vancomycin has been used to treat MRSA infections for >50 years. Although susceptibility rates remain high (>99%) in the United States and worldwide, there have been numerous reports of treatment failure, which appears to be related to increased vancomycin MICs that occur within the susceptibility range (2 mg/liter); however, the reasons related to treatment failure remain an area of clinical debate (4, 5). Linezolid and daptomycin have been used increasingly worldwide in the last decade, and resistance to these two compounds is still very uncommon among S. aureus strains isolated in U.S. hospitals (3).
Dalbavancin is a semisynthetic lipoglycopeptide derived structurally from antibiotic A-40926, a natural antibiotic similar to teicoplanin and produced by Nonomuraea spp. (6). Dalbavancin exerts its antimicrobial activity by binding to the terminal d-alanyl-d-alanine residues of peptidoglycan precursors. This binding prevents transpeptidation and subsequent transglycosylation, interfering with cross-linking and polymerization in the cell wall and ultimately causing bacterial death (7).
Dalbavancin was approved by the U.S. Food and Drug Administration (FDA) in 2014 and by the European Medicines Agency (EMA) in 2015 to treat adults with acute bacterial skin and skin structure infections (ABSSSIs) caused by susceptible isolates of S. aureus, including MRSA and methicillin-susceptible S. aureus (MSSA), Streptococcus pyogenes, Streptococcus agalactiae, Streptococcus dysgalactiae, Streptococcus anginosus group, and vancomycin-susceptible Enterococcus faecalis. Dalbavancin allows for convenient parenteral administration to treat ABSSSI, which can be a single dose of 1,500 mg or a dose of 1,000 mg followed by 500 mg a week later (8, 9).
Although vancomycin, linezolid, daptomycin, telavancin, and teicoplanin are very active against S. aureus, isolates with decreased susceptibility to these antimicrobial agents are isolated sporadically. In the present study, we assessed the in vitro activity of dalbavancin against a large collection of S. aureus clinical isolates with decreased susceptibility to these key antimicrobial agents that are used to treat severe S. aureus infections.
The organism collection evaluated in this investigation included 1,141 isolates with decreased susceptibility to vancomycin (MIC, ≥2 mg/liter), 48 isolates nonsusceptible to daptomycin (MIC, ≥2 mg/liter), 52 isolates with decreased susceptibility to telavancin (MIC, ≥0.12 mg/liter), 143 isolates with decreased susceptibility to teicoplanin (MIC, ≥4 mg/liter), and 25 isolates resistant to linezolid (MIC, ≥8 mg/liter).
This organism collection was selected from among 59,903 isolates collected from 139 U.S. medical centers between 2002 and 2016. Telavancin was only tested against isolates collected during 2011 to 2016 (n = 22,120), whereas all other antimicrobial agents evaluated in this investigation were tested against the entire S. aureus collection. Isolates were determined to be clinically significant based on local guidelines and were submitted to a central monitoring laboratory (JMI Laboratories, North Liberty, IA). Isolates were initially identified by the participating laboratory, and bacterial identifications were confirmed by the reference monitoring laboratory, when necessary.
Isolates were tested for susceptibility to dalbavancin and comparator agents by reference broth microdilution methods as described in the Clinical and Laboratory Standards Institute (CLSI) document M07-A10, and susceptibility interpretations were based on CLSI document M100-S27 and/or FDA guidelines and EUCAST breakpoint criteria (10–12). Dalbavancin breakpoints approved by the FDA for S. aureus were applied (i.e., ≤0.25 mg/liter) (11, 13).
MIC panels were manufactured at JMI Laboratories (2015 to 2016) or purchased from Thermo Fisher Scientific (before 2015) (Cleveland, OH). Organisms were tested in cation-adjusted Mueller-Hinton broth (Thermo Fisher Scientific). Quality assurance was performed by concurrently testing CLSI-recommended quality control reference strains (S. aureus ATCC 29213 and E. faecalis ATCC 29212).
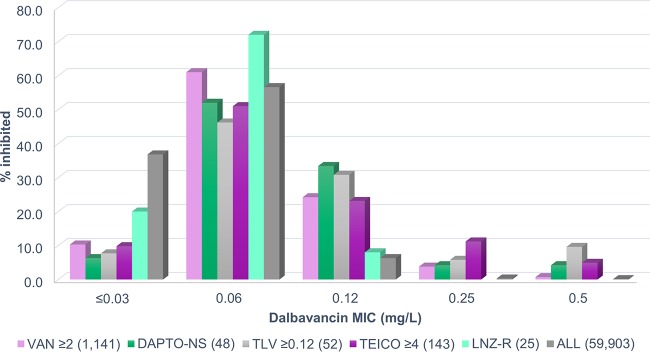
MRSA rates ranged from 65.4% to 96.0% among these resistant subsets (Table 1). Among the entire collection of S. aureus isolates tested against dalbavancin (n = 59,903), only 8 (0.01%) were categorized as dalbavancin nonsusceptible (MIC, >0.25 mg/liter), all with a dalbavancin MIC value of 0.5 mg/liter (Table 2 and Fig. 1) and vancomycin MIC values of 2 to 4 mg/liter (data not shown). Dalbavancin retained activity against 99.3% of isolates with vancomycin MICs of ≥2 mg/liter (MIC50/90, 0.06/0.12 mg/liter) (Tables 1 and 2), and dalbavancin MIC50 and MIC90 values were 8-fold lower than those of daptomycin (MIC50/90, 0.5/1 mg/liter; 96.8% susceptible) (Table 1). Teicoplanin (MIC50/90, ≤2/≤2 mg/liter; 99.9/93.5% susceptible [CLSI/EUCAST]) and linezolid (MIC50/90, 1/2 mg/liter; 99.6% susceptible) exhibited good activity against isolates with decreased susceptibility to vancomycin (Table 1).
TABLE 1.
Activity of dalbavancin and comparator antimicrobial agents tested against S. aureus isolates with decreased susceptibility to glycopeptides, daptomycin, and/or linezolid from U.S. medical centers
| Organism subset and antimicrobial agent | MIC50 (mg/liter) | MIC90 (mg/liter) | MIC range (mg/liter) | CLSIa |
EUCASTa |
||
|---|---|---|---|---|---|---|---|
| %S | %R | %S | %R | ||||
| Vancomycin MIC ≥2 mg/liter (n = 1,141) | |||||||
| Dalbavancin | 0.06 | 0.12 | ≤0.03 to 0.5 | 99.3b | 95.5 | 4.5 | |
| Daptomycin | 0.5 | 1 | ≤0.12 to 4 | 96.8 | 96.8 | 3.2 | |
| Vancomycin | 2 | 2 | 2 to 4 | 99.3 | 0.0 | 9.3 | 0.7 |
| Teicoplanin | ≤2 | ≤2 | ≤2 to 16 | 99.9 | 0.0 | 93.5 | 6.5 |
| Linezolid | 1 | 2 | ≤0.12 to >8 | 99.6 | 0.4 | 99.6 | 0.4 |
| Oxacillin | >2 | >2 | ≤0.25 to >2 | 26.9 | 73.1 | 26.9 | 73.1 |
| Daptomycin nonsusceptible (n = 48) | |||||||
| Dalbavancin | 0.06 | 0.12 | ≤0.03 to 0.5 | 95.8b | 91.7 | 8.3 | |
| Daptomycin | 2 | 4 | 2 to 4 | 0.0 | 0.0 | 100.0 | |
| Vancomycin | 2 | 2 | 1 to 4 | 95.8 | 0.0 | 95.8 | 4.2 |
| Teicoplanin | ≤2 | 4 | ≤2 to 16 | 97.9 | 0.0 | 87.5 | 12.5 |
| Linezolid | 1 | 2 | 0.5 to 4 | 100.0 | 0.0 | 100.0 | 0.0 |
| Oxacillin | >2 | >2 | ≤0.25 to >2 | 12.5 | 87.5 | 12.5 | 87.5 |
| Telavancin MIC ≥0.12 mg/liter (n = 52)c | |||||||
| Dalbavancin | 0.06 | 0.25 | ≤0.03 to 0.5 | 90.4b | 84.6 | 15.4 | |
| Daptomycin | 0.5 | 1 | 0.25 to 2 | 96.2 | 96.2 | 3.8 | |
| Vancomycin | 1 | 2 | 1 to 4 | 98.1 | 0.0 | 98.1 | 1.9 |
| Telavancin | 0.12 | 0.12 | 0.12 to 0.25 | 96.2 | 96.2 | 3.8 | |
| Teicoplanin | ≤2 | 4 | ≤2 to 16 | 98.1 | 0.0 | 76.9 | 23.1 |
| Linezolid | 1 | 1 | 0.25 to 2 | 100.0 | 0.0 | 100.0 | 0.0 |
| Oxacillin | >2 | >2 | ≤0.25 to >2 | 34.6 | 65.4 | 34.6 | 65.4 |
| Teicoplanin MIC ≥4 mg/liter (n = 143) | |||||||
| Dalbavancin | 0.06 | 0.25 | ≤0.03 to 0.5 | 95.1b | 83.9 | 16.1 | |
| Daptomycin | 0.5 | 1 | 0.12 to 4 | 95.8 | 95.8 | 4.2 | |
| Vancomycin | 2 | 2 | 0.5 to 4 | 97.9 | 0.0 | 97.9 | 2.1 |
| Teicoplanin | 4 | 8 | 4 to 16 | 99.3 | 0.0 | 0.0 | 100.0 |
| Linezolid | 1 | 2 | 0.25 to 4 | 100.0 | 0.0 | 100.0 | 0.0 |
| Oxacillin | >2 | >2 | ≤0.25 to >2 | 26.6 | 73.4 | 26.6 | 73.4 |
| Linezolid resistant (n = 25) | |||||||
| Dalbavancin | 0.06 | 0.06 | ≤0.03 to 0.12 | 100.0b | 100.0 | 0.0 | |
| Daptomycin | 0.5 | 0.5 | 0.25 to 0.5 | 100.0 | 100.0 | 0.0 | |
| Vancomycin | 1 | 2 | 0.5 to 2 | 100.0 | 0.0 | 100.0 | 0.0 |
| Teicoplanin | ≤2 | ≤2 | ≤2 to ≤2 | 100.0 | 0.0 | 100.0 | 0.0 |
| Linezolid | 8 | >8 | 8 to >8 | 0.0 | 100.0 | 0.0 | 100.0 |
| Oxacillin | >2 | >2 | ≤0.25 to >2 | 4.0 | 96.0 | 4.0 | 96.0 |
TABLE 2.
Summary of dalbavancin activity tested against S. aureus isolates with decreased susceptibility to glycopeptides, daptomycin, and/or linezolid from U.S. medical centers
| Resistance phenotype | No. of isolates (cumulative %) inhibited at dalbavancin MIC (mg/liter) ofa: |
MIC50 (mg/liter) | MIC90 (mg/liter) | ||||
|---|---|---|---|---|---|---|---|
| ≤0.03 | 0.06 | 0.12 | 0.25 | 0.5 | |||
| Vancomycin MIC ≥2 mg/liter (n = 1,141) | 117 (10.3) | 697 (71.3) | 276 (95.5) | 43 (99.3) | 8 (100.0) | 0.06 | 0.12 |
| Daptomycin nonsusceptible (n = 48) | 3 (6.3) | 25 (58.3) | 16 (91.7) | 2 (95.8) | 2 (100.0) | 0.06 | 0.12 |
| Telavancin MIC ≥0.12 mg/liter (n = 52)b | 4 (7.7) | 24 (53.8) | 16 (84.6) | 3 (90.4) | 5 (100.0) | 0.0.6 | 0.25 |
| Teicoplanin MIC ≥4 mg/liter (n = 143) | 14 (9.8) | 73 (60.8) | 33 (83.9) | 16 (95.1) | 7 (100.0) | 0.06 | 0.25 |
| Linezolid resistant (n = 25) | 5 (20.0) | 18 (92.0) | 2 (100.0) | 0.06 | 0.06 | ||
| All isolates (n = 59,903) | 22,066 (36.8) | 33,879 (93.4) | 3,795 (99.7) | 155 (>99.9) | 8 (100.0) | 0.06 | 0.06 |
Boldface data represent dalbavancin modal MIC results. The dalbavancin-susceptible breakpoint approved by the FDA for S. aureus is ≤0.25 mg/liter (13).
Telavancin was only tested against isolates collected in 2011 to 2016.
FIG 1.
Summary of dalbavancin activity when tested against S. aureus isolates with decreased susceptibility to glycopeptides, daptomycin, and/or linezolid from U.S. medical centers. Abbreviations: VAN ≥2, isolates with vancomycin MICs of ≥2 mg/liter; DAPTO-NS, daptomycin nonsusceptible (MIC, ≥2 mg/liter); TLV ≥0.12 mg/liter, isolates with telavancin MICs of ≥0.12 mg/liter; TEICO ≥4, isolates with teicoplanin MICs of ≥4 mg/liter; LNZ-R, linezolid resistant.
Dalbavancin (MIC50/90, 0.06/0.12 mg/liter; 95.8% susceptible [FDA]), vancomycin (MIC50/90, 2/2 mg/liter; 95.8% susceptible), teicoplanin (MIC50/90, ≤2/4 mg/liter; 97.9/87.5% susceptible [CLSI/EUCAST]), and linezolid (MIC50/90, 1/2 mg/liter; 100.0% susceptible) retained good activity against daptomycin-nonsusceptible S. aureus, and dalbavancin MIC50 and MIC90 values were 16- to 32-fold lower than those of vancomycin and teicoplanin when tested against these organisms (Table 1). Dalbavancin was also active against isolates with decreased susceptibility (MIC, ≥0.12 mg/liter) to telavancin, with MIC50/90 values of 0.06/0.25 mg/liter and 90.4% susceptibility (Tables 1 and 2). Furthermore, dalbavancin was more active (lower MIC values) than daptomycin (MIC50/90, 0.5/1 mg/liter; 96.2% susceptible) and vancomycin (MIC50/90, 1/2 mg/liter; 98.1% susceptible) against these organisms (Table 1).
When tested against S. aureus isolates with teicoplanin MICs of ≥4 mg/liter (nonsusceptible per EUCAST criteria), susceptibility rates for dalbavancin (MIC50/90, 0.06/0.25 mg/liter), daptomycin (MIC50/90, 0.5/1 mg/liter), vancomycin (MIC50/90, 2/2 mg/liter), and linezolid (MIC50/90, 1/2 mg/liter) were 95.1%, 95.8%, 97.9%, and 100.0%, respectively (Table 1).
All linezolid-resistant isolates were susceptible to dalbavancin (MIC50/90, 0.06/0.06 mg/liter), daptomycin (MIC50/90, 0.5/0.5 mg/liter), and vancomycin (MIC50/90, 1/2 mg/liter), and dalbavancin MIC50 and MIC90 values were 8- and 16- to 32-fold lower than those of daptomycin and vancomycin, respectively (Table 1).
Dalbavancin has demonstrated potent in vitro and broad-spectrum activity against Gram-positive organisms commonly involved in ABSSSIs, including MRSA and other multidrug-resistant organisms (14, 15). Dalbavancin's high protein binding and prolonged half-life allow for easily and consistently attainable therapeutic levels. The free serum drug levels are adequate to provide excellent tissue penetration, and several clinical trials have demonstrated its tolerability, efficacy, and noninferiority compared with standard therapy for ABSSSI (8, 9). The results of this investigation corroborate and expand published data on the in vitro activity of dalbavancin against S. aureus. Dalbavancin displayed potent activity against a large collection of S. aureus isolates (n = 59,903) collected from U.S. medical centers and retained good activity against isolates with decreased susceptibility to vancomycin, daptomycin, teicoplanin, telavancin, and/or linezolid. Dalbavancin MIC90 values were only slightly higher among these resistant subsets (0.12 to 0.25 mg/liter) compared to those of the overall collection (0.06 mg/liter), and the vast majority of isolates with decreased susceptibility to other lipoglycopeptides remained susceptible to dalbavancin. The highest dalbavancin MIC value was only 0.5 mg/liter, which is 1 doubling dilution above the susceptible breakpoint established by the FDA.
Although dalbavancin has shown excellent coverage against Gram-positive organisms, including multidrug-resistant isolates (14, 15), and it is approved by the FDA and EMA since 2014 and 2015, respectively, very few commercial dalbavancin susceptibility tests have been validated for clinical microbiology laboratory use. Thus, until such reagents are readily available, the use of a surrogate drug in the same class, such as vancomycin, to predict or infer dalbavancin susceptibility remains a viable option with predictive accuracy of 99.98% to 100.0% (16).
In summary, the in vitro characteristics presented here, along with the prolonged half-life and convenient administration, make dalbavancin a valuable option for treating S. aureus infections, including those caused by multidrug-resistant organisms.
ACKNOWLEDGMENTS
This study was supported by Allergan. Allergan was involved in the design and decision to present these results, and JMI Laboratories received compensation for services in relation to preparing this presentation. Allergan had no involvement in the collection, analysis, or interpretation of data.
We disclose that JMI Laboratories contracted to perform services in 2016 for Achaogen; Actelion; Allecra Therapeutics; Allergan; AmpliPhi Biosciences; API; Astellas Pharma; AstraZeneca; Basilea Pharmaceutica; Bayer AG; BD; Biomodels; Cardeas Pharma Corp.; CEM-102 Pharma; Cempra; Cidara Therapeutics, Inc.; CorMedix; CSA Biotech; Cutanea Life Sciences, Inc.; Debiopharm Group; Dipexium Pharmaceuticals, Inc.; Duke; Entasis Therapeutics, Inc.; Fortress Biotech; Fox Chase Chemical Diversity Center, Inc.; Geom Therapeutics, Inc.; GSK; Laboratory Specialists, Inc.; Medpace; Melinta Therapeutics, Inc.; Merck & Co., Inc.; Micromyx; MicuRx Pharmaceuticals, Inc.; Motif Bio; N8 Medical, Inc.; Nabriva Therapeutics, Inc.; Nexcida Therapeutics, Inc.; Novartis; Paratek Pharmaceuticals, Inc.; Pfizer; Polyphor; Rempex; Scynexis; Shionogi; Spero Therapeutics; Symbal Therapeutics; Synlogic; TenNor Therapeutics; TGV Therapeutics; The Medicines Company; Theravance Biopharma; Thermo Fisher Scientific; VenatoRx Pharmaceuticals, Inc.; Wockhardt; Zavante Therapeutics, Inc. We have no speakers' bureaus or stock options to declare.
REFERENCES
- 1.Bal AM, David MZ, Garau J, Gottlieb T, Mazzei T, Scaglione F, Tattevin P, Gould IM. 2017. Future trends in the treatment of methicillin-resistant Staphylococcus aureus (MRSA) infection: an in-depth review of newer antibiotics active against an enduring pathogen. J Glob Antimicrob Resist 10:295–303. doi: 10.1016/j.jgar.2017.05.019. [DOI] [PubMed] [Google Scholar]
- 2.Weiner LM, Webb AK, Limbago B, Dudeck MA, Patel J, Kallen AJ, Edwards JR, Sievert DM. 2016. Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2011–2014. Infect Control Hosp Epidemiol 37:1288–1301. doi: 10.1017/ice.2016.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sader HS, Mendes RE, Streit JM, Flamm RK. 2017. Antimicrobial susceptibility trends among Staphylococcus aureus from U.S. hospitals: results from 7 years of the ceftaroline (AWARE) surveillance program, 2010 to 2016. Antimicrob Agents Chemother 61:e01043. doi: 10.1128/AAC.01043-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Hal SJ, Lodise TP, Paterson DL. 2012. The clinical significance of vancomycin minimum inhibitory concentration in Staphylococcus aureus infections: a systematic review and meta-analysis. Clin Infect Dis 54:755–771. doi: 10.1093/cid/cir935. [DOI] [PubMed] [Google Scholar]
- 5.Kalil AC, Van Schooneveld TC, Fey PD, Rupp ME. 2014. Association between vancomycin minimum inhibitory concentration and mortality among patients with Staphylococcus aureus bloodstream infections: a systematic review and meta-analysis. JAMA 312:1552–1564. doi: 10.1001/jama.2014.6364. [DOI] [PubMed] [Google Scholar]
- 6.Malabarba A, Goldstein BP. 2005. Origin, structure, and activity in vitro and in vivo of dalbavancin. J Antimicrob Chemother 55(Suppl 2):ii15–ii20. [DOI] [PubMed] [Google Scholar]
- 7.Smith JR, Roberts KD, Rybak MJ. 2015. Dalbavancin: a novel lipoglycopeptide antibiotic with extended activity against Gram-positive infections. Infect Dis Ther 4:245–258. doi: 10.1007/s40121-015-0077-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boucher HW, Wilcox M, Talbot GH, Puttagunta S, Das AF, Dunne MW. 2014. Once-weekly dalbavancin versus daily conventional therapy for skin infection. N Engl J Med 370:2169–2179. doi: 10.1056/NEJMoa1310480. [DOI] [PubMed] [Google Scholar]
- 9.Garnock-Jones KP. 2017. Single-dose dalbavancin: a review in acute bacterial skin and skin structure infections. Drugs 77:75–83. doi: 10.1007/s40265-016-0666-0. [DOI] [PubMed] [Google Scholar]
- 10.Clinical and Laboratory Standards Institute. 2015. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; approved standard—10th ed. CLSI document M07-A10. Clinical and Laboratory Standards Institute, Wayne, PA. [Google Scholar]
- 11.Clinical and Laboratory Standards Institute. 2017. Performance standards for antimicrobial susceptibility testing; 27th informational supplement. CLSI document M100-S27. Clinical and Laboratory Standards Institute, Wayne, PA. [Google Scholar]
- 12.EUCAST. 2017. Breakpoint tables for interpretation of MICs and zone diameters, version 7.1, March 2017. http://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_7.1_Breakpoint_Tables.pdf.
- 13.DurataTherapeutics U.S. Limited. 2016. Dalvance package insert. DurataTherapeutics U.S. Limited, Parsipanny, NJ: http://www.allergan.com/assets/pdf/dalvance_pi. [Google Scholar]
- 14.Mendes RE, Castanheira M, Farrell DJ, Flamm RK, Sader HS, Jones RN. 2016. Update on dalbavancin activity tested against Gram-positive clinical isolates responsible for documented skin and skin-structure infections in US and European hospitals (2011–13). J Antimicrob Chemother 71:276–278. doi: 10.1093/jac/dkv303. [DOI] [PubMed] [Google Scholar]
- 15.Pfaller MA, Mendes RE, Sader HS, Castanheira M, Flamm RK. 2017. Activity of dalbavancin tested against Gram-positive clinical isolates causing skin and skin-structure infections in paediatric patients from US hospitals (2014–2015). J Glob Antimicrob Resist 11:4–7. doi: 10.1016/j.jgar.2017.06.003. [DOI] [PubMed] [Google Scholar]
- 16.Jones RN, Rhomberg PR, Mendes RE. 2016. Reproducibility of dalbavancin MIC test results and an updated surrogate accuracy analysis of vancomycin MIC values to infer dalbavancin susceptibility (2014). Diagn Microbiol Infect Dis 86:249–251. doi: 10.1016/j.diagmicrobio.2016.02.007. [DOI] [PubMed] [Google Scholar]