Abstract
Although laparoscopic adjustable gastric banding is considered the most minimally invasive surgical technique for the treatment of morbid obesity, the procedure has a reported overall complication rate of up to 26%. Among the various complications, gastric band erosion with intragastric band migration is the most worrisome because of the risk of subsequent obstruction, peritonitis, and sepsis. Therefore, prompt and accurate diagnosis is crucial during imaging evaluation of these patients in the late postoperative setting. In this article, we report a case of a 47-year-old woman with a gastric band that had eroded into the gastric wall with intragastric migration demonstrating classic findings on fluoroscopic and computed tomography imaging.
Introduction
Morbid obesity continues to be a major chronic healthcare problem worldwide with an estimated annual medical cost in the United States alone totaling $147 billion [1]. In recent decades, bariatric surgery has evolved from a nascent pioneer phase to a myriad of sophisticated surgeries numbering 196,000 performed in 2015 [2]. First introduced in 1993, laparoscopic adjustable gastric banding (LAGB) consists of an inflatable gastric band placed below the gastroesophageal junction resulting in the creation of a gastric pouch, with the effective diameter of the band controlled by a subcutaneous port via a connecting tube [3]. Although originally a popular surgical technique at the time of its introduction, highly reported complication rates of 10%-26% have resulted in a marked decline of LAGB insertion, now accounting for only 6% of all bariatric surgeries [4], [5], [6]. Reported complications and incidence of laparoscopic gastric banding include band erosion (28%), port-tubing disconnection (20%), band slippage (4%-13%), incisional hernia (5%), port infection (2%), gastric band erosion with intragastric band migration (2%-4%), and gastric perforation (0.1%-0.8%) [7], [8], [9]. Among these complications, gastric band erosion with intragastric band migration is most worrisome because of the risk of subsequent obstruction, peritonitis, and sepsis [4]. Therefore, prompt and accurate diagnosis is crucial during imaging evaluation of these patients in the postoperative setting. Here, we report a case of gastric band erosion with subsequent migration into the stomach.
Case report
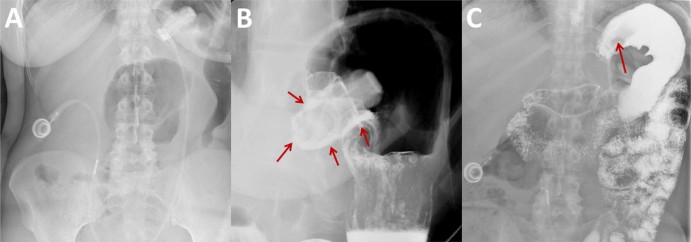
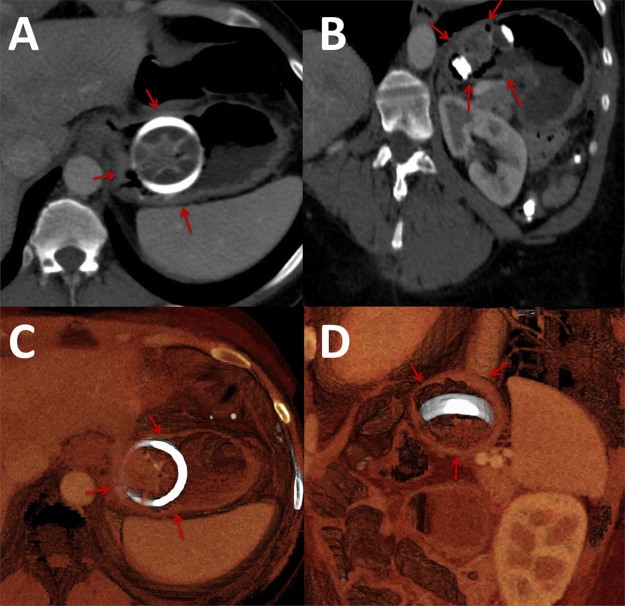
A 47-year-old Caucasian woman with a history of laparoscopic gastric band placement 9 years prior presented to our outpatient bariatric surgery clinic with a 1-month history of intermittent shortness of breath and epigastric tenderness. The patient reported a total weight loss of 120 pounds, which she had maintained for the previous 5 years with the last gastric band adjustment performed 2 years prior without apparent complication. The patient denied nausea, vomiting, or significant weight gain. Physical examination revealed tenderness superficial to the laparoscopic gastric band port site with abdominal pain exacerbated by movement. Vital signs and laboratory data were within normal limits. A precontrast radiograph from a double contrast upper gastrointestinal study (Fig. 1) demonstrated a gastric band with a normal phi angle of 48°. After administration of barium oral contrast, contrast was identified pooling circumferentially around the band suspicious for intragastric band migration without evidence of gastric leak. A subsequent contrast-enhanced computed tomography (CT) of abdomen examination (Fig. 2) confirmed a completely intraluminal location of the gastric band within the stomach cardia. The patient was admitted to the hospital and underwent an esophagogastroduodenoscopy (Fig. 3) at which time the gastric band was found to have completely eroded through the gastric wall and was located almost entirely intraluminally. The gastric band was removed laparoscopically through the abdomen with the gastrostomy site repaired by incorporation of a fat patch and adjacent gastric wall around the closure site. In addition, a Dor fundoplication was performed. Two days later, a single contrast upper gastrointestinal study demonstrated an intact anastomosis without evidence of obstruction or leak. The patient had an uncomplicated postoperative hospital course and was subsequently discharged 1 week later.
Fig. 1.
Supine radiograph (A) demonstrates the laparoscopic gastric band in appropriate orientation with a normal phi angle. After administration of oral contrast during a double contrast upper gastrointestinal study, an upright spot radiograph (B) demonstrates pooling of oral contrast surrounding the intragastric portion of the laparoscopic adjustable gastric band (arrows) compatible with band erosion with intragastric migration. A prone radiograph obtained at the conclusion of the study (C) demonstrates a completely contrast-filled stomach fundus and body with nonvisualization of the normal radiopaque gastric band. A filling defect in the gastric cardia (arrow) corresponds to the gastric band located within the stomach lumen. There is no extraluminal contrast identified to suggest a gastric leak.
Fig. 2.
Axial (A) and coronal (B) contrast-enhanced computed tomography images demonstrate a complete intraluminal location of the laparoscopic adjustable gastric band (arrows mark the gastric wall) secondary to gastric band erosion. Volumetric 3-dimensional reformatted images in the axial (C) and sagittal (D) planes confirm the intragastric location of the band (arrows mark the gastric wall).
Fig. 3.
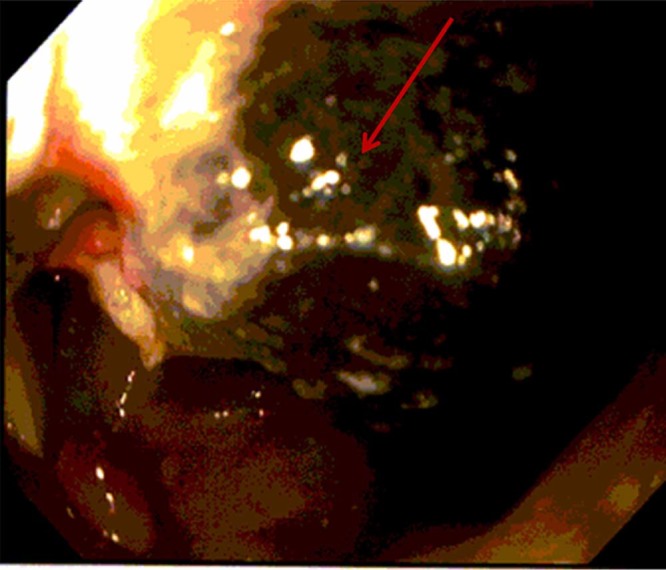
Intraoperative esophagogastroduodenoscopy demonstrates a complete intragastric location of the laparoscopic adjustable gastric band (arrow) confirming findings on fluoroscopy and computed tomography imaging.
Discussion
Although a common form of bariatric surgery at the turn of the century and considered the least invasive bariatric surgical procedure, the incidence of LAGB has declined in the past decade as a result of the relatively high complication rate and increasing popularity of alternative procedures, including sleeve gastrectomy and Roux-en-Y gastric bypass [10]. Of the reported complications, gastric band erosion with intragastric band migration is considered particularly worrisome because of the increased risk of obstruction and peritonitis.
First described in 1998, gastric erosion is a major complication of LAGB with an incidence reported to be between 0.3% and 28%, with the wide range likely attributed to variation in the routine imaging follow-up period of patients in different institutions [8], [11], [12]. Gastric erosion and intragastric band migration may occur either in the early or in the late postoperative settings. Pathogenesis of gastric band erosion is multifactorial and is dependent on the postoperative time frame. In the early setting, gastric erosion is thought to be secondary to iatrogenic gastric wall damage from the initial procedure or microperforation after postoperative infection [6], [13]. Additional risk factors have been reported in the early postoperative setting including formation of adhesions and the use of nonsteroidal anti-inflammatory drugs [14], [15]. Late band erosions typically occur at least 2 years after surgery and are favored to be secondary to sequela of a pressure-induced response or a foreign body rejection reaction. In the pressure-induced setting, overfilling of the band, inclusion of excess gastric wall during initial surgery, and ingestion of large food boluses in the early postoperative setting have been implicated as risk factors for erosion resulting in subsequent gastric wall ischemia and necrosis [16]. Foreign body rejection from the band material itself has been hypothesized to produce weak fibrous tissue formation and eventual mural erosion [16].
Intragastric band migration after erosion is a much rarer complication with a reported incidence of 2%-4% [9], [17]. Although typically seen in the late postoperative setting, intragastric band migration has been reported as early as 1 year postoperatively [10]. Although the majority of migrated bands are intragastric in location, several case reports have described free migration into the abdominal cavity as well as small bowel and colonic erosion [5], [6], [18]. Migrated gastric bands have also been reported to have passed distally beyond the initial site of erosion throughout the alimentary tract, including 1 case with the band migrating to the rectum resulting in a transient large bowel obstruction [5], [18], [19]. Patients are frequently asymptomatic with studies reporting 7%-46% of asymptomatic patients with intragastric band migration incidentally found on routine screening with gastroscopy [14], [20]. Symptomatic patients may present with vague epigastric pain, weight gain secondary to loss of band function, hematemesis, infection, transient or complete obstruction, and rarely intestinal perforation [8], [10].
The earliest finding of band erosion on radiographic and fluoroscopic studies is an abnormal position of the gastric band with migration of the band compared with baseline postoperative radiographs [8], [21]. In the absence of previous imaging studies for comparison or in the early stages of gastric band erosion, fluoroscopic studies may appear normal [8]. In later stages, oral contrast material may be identified surrounding the portion of the band that has eroded into the gastric lumen. CT imaging is a useful cross-sectional tool for evaluation of the degree of gastric erosion and band migration. When partially eroded, the diagnostic accuracy of CT imaging can be increased by administering water-soluble neutral oral contrast material to distend the stomach and by thorough review of multiplanar images [8]. In equivocal cases, a definitive diagnosis can be made with endoscopic examination [14]. Our case demonstrates classic findings on both fluoroscopic and CT imaging with findings confirmed on endoscopic examination.
Once diagnosed, the eroded band should be removed based on patient symptomatology. In asymptomatic patients, there is no immediate need for removal, and after band removal, gastric repair and band replacement may be performed [13]. In the setting of infection or obstruction, surgery should be performed promptly with band replacement in these patients withheld until complete recovery is achieved [6], [13]. As our patient did not have findings of obstruction or infection, gastric repair was performed immediately after band removal.
Historically, gastric band erosions were treated with open or laparoscopic approaches and required lengthy postoperative hospital stays [22], [23]. However, recent advances in endoscopic techniques have allowed endoluminal division and removal of eroded gastric bands, which may result in a shorter postoperative hospitalization and decreased perioperative and postoperative complications [22].
In conclusion, this is a case of gastric band erosion with intragastric band migration highlighting classic imaging findings on fluoroscopy and CT with endoscopic correlation. As gastric erosion with intragastric band migration is a rare but serious complication of LAGB, knowledge and identification of the diagnostic imaging characteristics is crucial in evaluating these postsurgical patients.
Footnotes
No institutional review board approval was required for this manuscript.
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Khan L.K., Sobush K., Keener D., Goodman K, Lowry A, Kakietek J, Centers for Disease Control and Prevention Recommended community strategies and measurements to prevent obesity in the United States. MMWR Recomm Rep. 2009;58(RR–7):1–26. [PubMed] [Google Scholar]
- 2.Ponce J., DeMaria E.J., Nguyen N.T., Hutter M., Sudan R., Morton J.M. American Society for Metabolic and Bariatric Surgery estimation of bariatric surgery procedures in 2015 and surgeon workforce in the United States. Surg Obes Relat Dis. 2017;12(9):1637–1639. doi: 10.1016/j.soard.2016.08.488. [DOI] [PubMed] [Google Scholar]
- 3.Belachew M., Legrand M.J., Defechereux T.H., Burtheret M.P., Jacquet N. Laparoscopic adjustable silicone gastric banding in the treatment of morbid obesity. A preliminary report. Surg Endosc. 1994;8(11):1354–1356. doi: 10.1007/BF00188302. [DOI] [PubMed] [Google Scholar]
- 4.Chevallier J.-M., Zinzindohoue F., Douard R., Blanche J.-P., Berta J.-L., Altman J.-J. Complications after laparoscopic adjustable gastric banding for morbid obesity: experience with 1,000 patients over 7 years. Obes Surg. 2004;14(3):407–414. doi: 10.1381/096089204322917954. [DOI] [PubMed] [Google Scholar]
- 5.Bilkhu A., Harvey H., Davies J.B., Steward M.A., Halstead J.C. Laparoscopic repair of a migrated adjustable gastric band connecting tube with colonic erosion. J Surg case reports. 2017;2017(5):rjx089. doi: 10.1093/jscr/rjx089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Povoa A.A., Soares C., Esteves J., Gandra A., Maciel R., Cardoso J.M. Simultaneous gastric and colic laparoscopic adjustable gastric band migration. Complication of bariatric surgery. Obes Surg. 2010;20(6):796–800. doi: 10.1007/s11695-009-0046-x. [DOI] [PubMed] [Google Scholar]
- 7.Himpens J., Cadiere G.-B., Bazi M., Vouche M., Cadiere B., Dapri G. Long-term outcomes of laparoscopic adjustable gastric banding. Arch Surg. 2011;146(7):802–807. doi: 10.1001/archsurg.2011.45. [DOI] [PubMed] [Google Scholar]
- 8.Sonavane S.K., Menias C.O., Kantawala K.P., Shanbhogue A.K., Prasad S.R., Eagon J.C. Laparoscopic adjustable gastric banding: what radiologists need to know. Radiographics. 2012;32(4):1161–1178. doi: 10.1148/rg.324115177. [DOI] [PubMed] [Google Scholar]
- 9.Laghi A., Rengo M. 2017. Imaging in bariatric surgery. Cham, Switzerland. [Google Scholar]
- 10.Abeysekera A., Lee J., Ghosh S., Hacking C. Migration of eroded laparoscopic adjustable gastric band causing small bowel obstruction and perforation. BMJ Case Rep. 2017;2017 doi: 10.1136/bcr-2017-219954. pii: bcr-2017-219954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chapman A.E., Kiroff G., Game P., Foster B., O'Brien P., Ham J. Laparoscopic adjustable gastric banding in the treatment of obesity: a systematic literature review. Surgery. 2004;135(3):326–351. doi: 10.1016/S0039-6060(03)00392-1. [DOI] [PubMed] [Google Scholar]
- 12.Brown W.A., Egberts K.J., Franke-Richard D., Thodiyil P., Anderson M.L., O'Brien P.E. Erosions after laparoscopic adjustable gastric banding: diagnosis and management. Ann Surg. 2013;257(6):1047–1052. doi: 10.1097/SLA.0b013e31826bc21b. [DOI] [PubMed] [Google Scholar]
- 13.Silecchia G., Restuccia A., Elmore U., Polito D., Perrotta N., Genco A. Laparoscopic adjustable silicone gastric banding: prospective evaluation of intragastric migration of the lap-band. Surg Laparosc Endosc Percutan Tech. 2001;11(4):229–234. doi: 10.1097/00129689-200108000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Chisholm J., Kitan N., Toouli J., Kow L. Gastric band erosion in 63 cases: endoscopic removal and rebanding evaluated. Obes Surg. 2011;21(11):1676–1681. doi: 10.1007/s11695-011-0468-0. [DOI] [PubMed] [Google Scholar]
- 15.Abu-Abeid S., Bar Zohar D., Sagie B., Klausner J. Treatment of intra-gastric band migration following laparoscopic banding: safety and feasibility of simultaneous laparoscopic band removal and replacement. Obes Surg. 2005;15(6):849–852. doi: 10.1381/0960892054222696. [DOI] [PubMed] [Google Scholar]
- 16.Mozzi E., Lattuada E., Zappa M.A., Granelli P., De Ruberto F., Armocida A. Treatment of band erosion: feasibility and safety of endoscopic band removal. Surg Endosc. 2011;25(12):3918–3922. doi: 10.1007/s00464-011-1820-0. [DOI] [PubMed] [Google Scholar]
- 17.De Palma G.D., Formato A., Pilone V., Rega M., Giuliano M.E., Simeoli I. Endoscopic management of intragastric penetrated adjustable gastric band for morbid obesity. World J Gastroenterol. 2006;12(25):4098–4100. doi: 10.3748/wjg.v12.i25.4098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rogalski P., Hady H.R., Baniukiewicz A., Dabrowski A., Kaminski F., Dadan J. Gastric band migration following laparoscopic adjustable gastric banding (LAGB): two cases of endoscopic management using a gastric band cutter. Wideochirurgia i inne Tech maloinwazyjne = Videosurgery other miniinvasive Tech. 2012;7(2):114–117. doi: 10.5114/wiitm.2011.25983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zengin K., Sen B., Ozben V., Taskin M. Detachment of the connecting tube from the port and migration into jejunal wall. Obes Surg. 2006;16(2):206–207. doi: 10.1381/096089206775565131. [DOI] [PubMed] [Google Scholar]
- 20.Bassam A. Unusual gastric band migration outcome: distal small bowel obstruction and coming out per-rectum. Pan Afr Med J. 2012;13:59. [PMC free article] [PubMed] [Google Scholar]
- 21.Mehanna M.J., Birjawi G., Moukaddam H.A., Khoury G., Hussein M., Al-Kutoubi A. Complications of adjustable gastric banding, a radiological pictorial review. AJR Am J Roentgenol. 2006;186(2):522–534. doi: 10.2214/AJR.04.0655. [DOI] [PubMed] [Google Scholar]
- 22.Spann M.D., Aher C., V, English W.J., Williams D.B. Endoscopic management of erosion after banded bariatric procedures. Surg Obes Relat Dis. 2017;13(11):1875–1879. doi: 10.1016/j.soard.2017.07.025. [DOI] [PubMed] [Google Scholar]
- 23.Kohn G.P., Hansen C.A., Gilhome R.W., McHenry R.C., Spilias D.C., Hensman C. Laparoscopic management of gastric band erosions: a 10-year series of 49 cases. Surg Endosc. 2012;26(2):541–545. doi: 10.1007/s00464-011-1916-6. [DOI] [PubMed] [Google Scholar]