Abstract
Objective
To assess the relationship of restrictions on Medicaid benefits for addiction treatment to Medicaid acceptance among addiction treatment programs.
Data sources
We collected primary data from the 2013–2014 wave of the National Drug Abuse Treatment System Survey.
Study design
We created two measures of benefits restrictiveness. In the first, we calculated the number of addiction treatment services covered by each state Medicaid program. In the second, we calculated the total number of utilization controls imposed on each service. Using a mixed-effects logistic regression model, we estimated the relationship between state Medicaid benefit restrictiveness for addiction treatment and adjusted odds of Medicaid acceptance among addiction treatment programs.
Data collection
Study data come from a nationally-representative sample of 695 addiction treatment programs (85.5% response rate), representatives from Medicaid programs in forty-seven states and the District of Columbia (response rate 92%), and data collected by the American Society for Addiction Medicine.
Principal findings
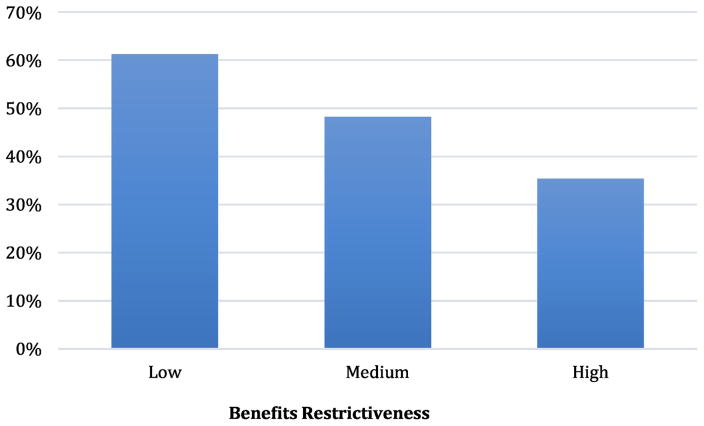
Addiction treatment programs in states with more restrictive Medicaid benefits for addiction treatment had lower odds of accepting Medicaid enrollees (AOR = 0.65; CI=0.43, 0.97). The predicted probability of Medicaid acceptance was 35.4% in highly restrictive states, 48.3% in moderately restrictive states, and 61.2% in the least restrictive states.
Conclusions
Addiction treatment programs are more likely to accept Medicaid in states with less restrictive benefits for addiction treatment. Program ownership and technological infrastructure also play an important role in increasing Medicaid acceptance.
Keywords: Addiction treatment, Medicaid, health policy
INTRODUCTION
Few Medicaid enrollees in need of addiction treatment ever receive it. Although they are 50% more likely to have an addiction than the general population (Busch et al. 2013; SAMHSA, 2010), fewer than one in three Medicaid enrollees with a substance use disorder reported any lifetime treatment for their condition (Busch et al. 2013). Medicaid enrollees face the same barriers that limit treatment access for all persons with addictive disorders: difficulty locating addiction treatment programs (McAuliffe & Dunn, 2004; Perron, et al. 2010), long wait times to enter treatment (Andrews et al. 2012; Carr et al. 2008; Hoffman et al. 2011), and challenges in getting to and from treatment (D’Aunno, 2006; Friedmann et al. 2000; Friedmann et al. 2003). But Medicaid enrollees also face another major challenge: At present, only about half of all addiction treatment programs in the United States report they accept Medicaid enrollees, and approximately 40% of U.S. counties lack a single outpatient addiction treatment program that accepts any Medicaid enrollees (Cummings et al. 2014).
Moreover, Medicaid acceptance varies significantly across the states. For example, in California, home to the nation’s largest Medicaid program and 14% of all Medicaid enrollees, fewer than 30% of addiction treatment programs accept Medicaid (SAMHSA, 2014). In contrast, approximately 85% of addiction treatment providers in Connecticut accept Medicaid (SAMHSA, 2014). Programs located in the South are among the least likely in the nation to accept Medicaid enrollees (Cummings et al. 2014). This variability derives from several factors. For-profit providers, which are over-represented in the Southern region of the country, are less likely to accept Medicaid enrollees than public and non-profit providers of addiction treatment (Andrews, 2014; Terry-McElrath, Chriqui, & McBride, 2011). Local socio-demographic characteristics are also important. For example, on average, Medicaid acceptance increases with the percentage of low-income individuals in a county or state, and decreases with the percentage of African-American residents (Andrews, 2014; Terry-McElrath, Chriqui, & McBride, 2011).
Some addiction treatment programs may face additional barriers to accepting Medicaid enrollees. Historically, addiction treatment programs have operated outside of the mainstream health care system, functioning with institutional values, practices, and funding streams separate from those of general health care (Andrews et al. 2015). Some addiction treatment programs may have the desire to accept Medicaid enrollees, but are unable to do so because they lack the technological infrastructure required to bill services and report on quality and performance measures as required by Medicaid (Andrews et al. 2015; McLellan & Meyers, 2004; Buck, 2011). Moreover, many addiction treatment programs do not employ staff who possess credentials and/or licensure required to serve as Medicaid-billable providers (Andrews et al. 2015). High front-end costs required for investment in new technology and professional staff may present formidable barriers for providers looking to gain entry into the Medicaid “market.”
Medicaid Benefits for Addiction Treatment
As the major public health insurance program for low-income citizens in the U.S., Medicaid has become an increasingly important payer of addiction treatment over the past several decades. The number of states providing benefits for addiction treatment expanded dramatically from just a handful of states in the 1980s to nearly every state in the country on the eve of the enactment of the Affordable Care Act (ACA) in 2010 (Andrews, 2014; Buck, 2011; SAMHSA, 2005). From 1986 to 2005, Medicaid funding for addiction treatment more than doubled, and increased its share of total addiction treatment expenditures from 9% to 21% (Mark et al. 2007). In 2014, 19 states expanded Medicaid eligibility, allowed under the ACA. By the end of 2016, 32 states had adopted the Medicaid expansion. As a result, Medicaid spending on addiction treatment is expected to more than double in the years ahead, from $5.2 billion in 2009 to $11.9 billion by 2020, and the share of addiction treatment expenditures paid for by Medicaid is also expected to increase over the same period, reaching 28% by 2020 (Mark et al. 2014).
While the Affordable Care Act requires that all state Medicaid programs provide at least some basic benefits for addiction treatment for newly-eligible enrollees through the Essential Health Benefits requirement, it does not define which specific services must be included, permitting wide variation in the benefits covered across states. In the absence of an established federal standard for addiction treatment benefits, the American Society of Addiction Medicine’s (ASAM) clinical guidelines for addiction treatment services represent the scientific and clinical consensus regarding the appropriate course of care, and are the most widely-used and evaluated set of guidelines for addiction treatment (ASAM, 2016). However, only 13 states provided benefits that meet ASAM recommendations, and 24 states lacked benefits in one or more of the four levels of care considered essential to the effective treatment of addiction (Grogan et al. 2016). States most commonly excluded treatment requiring higher levels of care, such as intensive outpatient, residential, and medically managed inpatient services.
Medicaid Benefit Design and Treatment Program Acceptance of Medicaid
Despite Medicaid’s varied role in financing addiction treatment across states, we know relatively little about the influence of its benefit design on acceptance of Medicaid by treatment programs. Prior research suggests a positive relationship between state Medicaid benefits and willingness of addiction treatment programs to treat Medicaid enrollees (Andrews, 2014; Terry-McElrath, Chriqui, & McBride, 2011). Terry-McElrath and colleagues (2011) found that programs receiving public funding were more likely to accept Medicaid in states in which Medicaid provided any kind of basic benefit for addiction treatment. Andrews (2014) found that the extent of benefits matters, as well. Medicaid acceptance among addiction treatment programs was positively associated with the number of treatment services covered.
Use of utilization controls—including preauthorization, concurrent review, and limits on the frequency and intensity of service use—have been inversely related to Medicaid acceptance (Cunningham & May, 2006; Mitchell, 1991; Berman, Dolins & Tang, 2002; Backus et al. 2001). For example, medical care providers are less likely to accept Medicaid enrollees in managed care plans, which commonly employ utilization controls, than they are to accept enrollees in fee-for-service plans (Backus et al. 2001; Barbee, 2016). In addition to the potential of these controls to reduce the overall volume of services received by Medicaid enrollees, providers also cite administrative burden related to some utilization controls as a disincentive to participate (Terry-McElrath, Chriqui, & McBride, 2011). Smaller medical care providers with smaller budgets and fewer patients may be especially ill-equipped to handle the financial and administrative burdens associated with more restrictive state Medicaid programs (Cunningham, 2006; Andrews et al. 2015).
The present study assesses whether the restrictiveness of Medicaid benefits—as measured by the comprehensiveness of services covered and use of utilization controls—is linked to addiction treatment providers’ choices regarding Medicaid acceptance. Understanding how Medicaid benefits design for addiction treatment may be linked to Medicaid acceptance is critical, as states continue to possess broad discretion in structuring Medicaid benefits for addiction treatment. Moreover, although the future of the ACA is uncertain under the Trump Administration, it is important to consider the potential effect that dismantling the ACA could have on SUD benefits within state Medicaid programs. For example, repeal could result in the removal of the Essential Health Benefits requirement that states provide benefits for addiction treatment to enrollees newly-eligible under the Medicaid expansion. Repeal could also remove behavioral health parity requirements imposed on Medicaid managed care programs through extension of the MHPAEA. If these requirements related to addiction treatment coverage and parity are repealed, it is possible that some states could elect to increase coverage restrictions and utilization controls. Deepening knowledge of the relationship between benefits design and providers’ willingness to serve Medicaid enrollees is a first step in understanding the potential impact of such policy changes on access to addiction treatment for Medicaid enrollees in the United States.
METHODS
This study draws on data and methods from the sixth wave of the National Drug Abuse Treatment System Survey (NDATSS). The study includes data from two surveys administered during this wave of data collection: first, a nationally-representative, longitudinal study of addiction treatment programs in the United States; and second, a survey of all 50 state Medicaid programs including the District of Columbia. To ensure that the sample of addiction treatment programs is nationally representative at each wave of data collection, we used a split panel design with replacement sampling to update it and fill-in for programs that exit the sample over time. In addition, survey weights were used to adjust for sample selection and account for nonresponse bias. We collected the data from November 2013 to June 2014. Survey questions focused on accessibility and quality of addiction treatment nationwide. Program directors and clinical services supervisors from 695 treatment programs completed 90-minute, internet-based surveys, resulting in a response rate of 85.5%.
For the Medicaid survey, representatives from state Medicaid agencies completed a 15-minute internet-based survey that included questions to assess the restrictiveness of Medicaid benefits for addiction treatment services. Representatives from forty-seven states and the District of Columbia completed the survey, representing a response rate of 92%. Prior to conducting the survey with Medicaid representatives, we reviewed all state Medicaid plans on file with CMS and agency websites to partially pre-populate the survey. Pre-fill data collected via the public records review were used for the three states that did not respond, although these data were less complete and comprehensive than the data we captured via the more comprehensive survey instrument. Finally, data on benefits for addiction treatment medications were taken from the ASAM Survey of Medication and Counseling for Treatment and Prevention of Relapse to Opiate Dependence, conducted in May 2013 (ASAM, 2013). More detailed information regarding the surveys can be found elsewhere (D’Aunno et al. 2015; D’Aunno et al. 2017; Grogan et al., 2017).
Measures
Dependent variables
The study’s dependent variable measured whether addiction treatment programs reported acceptance of any Medicaid enrollees during the most recent complete fiscal year.
Independent Variables
The study included two independent variables. The first assessed the restrictiveness of state Medicaid benefits for addiction treatment services. We measured state benefits of each of the seven services included in the American Society for Addiction Medicine’s (ASAM) continuum of care, including outpatient, group outpatient intensive outpatient, short-term residential, long-term residential, medically-managed inpatient detoxification and treatment, and recovery support. Medicaid representatives who participated in the survey were asked to indicate whether their state’s program covered each service.
Benefits restrictiveness was measured as the total number of the seven possible services covered by the state Medicaid program. Each state was assigned a value of benefits restriction ranging from 0–7, with one being the least restrictive and seven being the most restrictive. Two evidence-based medications for treatment of addiction were included in the model individually: methadone and oral naltrexone. Buprenorphine was excluded from model because 100% of state Medicaid programs covered it. Injectable naltrexone was excluded due to high correlation with oral naltrexone (ρ = 0.83) and resulting multicollinearity in modeling.
The second independent variable assessed the extent of use of utilization controls in relation to each of the seven services noted above. Controls included (1) cost-sharing (including co-pays and deductibles), (2) pre-authorization, and (3) annual maximums. Extent of use of utilization controls was measured by summing the total number of utilization controls (of a possible three controls) used for each of the seven benefits, for a range of possible scores spanning 0–21. More detailed information regarding state-level variation in benefits restrictiveness and utilization controls can be found elsewhere (Grogan et al., 2016).
Control Variables
We included measures of state-, program- and community-level factors that have been significantly related to addiction treatment programs’ willingness to accept Medicaid in prior research (Terry-McElrath, Chriqui, & McBride, 2011; Andrews, 2014). These include ownership (private for-profit, private non-profit, and public), program type (outpatient, inpatient/residential, opioid treatment), accreditation (Joint Commission or Commission on Accreditation of Rehabilitation Facilities) and program capacity (ability to bill in-house, use of electronic health records, percent of staff with computers). In addition, we controlled for average caseload, measured using four ordinal categories (0–10, 11–25, 26–40, >40), and reliance on private insurance, measured by the percentage of program revenues in the past year from private insurance. We included two variables to assess staff professionalization, including whether or not a physician was employed, and whether or not a physician was required for treatment. County level factors, such as geographic region, urbanicity, income level, and the number of addiction treatment programs, were also included. Finally, we controlled for factors related to the state Medicaid plan itself, such as the percentage of state residents eligible for Medicaid, and whether the state required physician involvement in treatment planning and/or provision to reimburse for addiction treatment services.
Analytic Technique
We calculated descriptive statistics and conducted t-tests and ANOVA to assess differences between addiction treatment programs that did and did not accept Medicaid enrollees. Using a mixed-effects logistic regression model, we estimated the relationship between state Medicaid benefit restrictiveness and use of utilization controls for addiction treatment and odds of Medicaid acceptance among treatment programs in our sample. Survey weights were used to adjust for sample selection. To account for missing data observed on several control variables (less than 10% missing data across all control variables), we conducted multiple imputation using STATA’s mi impute command suite. We also estimated the predicted probability of accepting Medicaid for programs in states with high benefits restriction (scores 5–7), medium benefits restriction (3–4), and low benefits restriction (1–2). In addition, we also developed a two-stage model to determine if technological capabilities act as pre-requisites for Medicaid acceptance (i.e., a program cannot accept Medicaid enrollees if they do have the technological capacity to do so). However, predicted values of technological capacity in the Stage 1 model were not a significant predictor of acceptance, so we retained the simplified model reported in the results below. All analyses were conducted in STATA SE 14.1.
RESULTS
Overall, 58% of addiction treatment programs reported that they accepted Medicaid as a form of payment for services (see Table 1 for descriptive statistics). Only about half of programs reported having a physician on staff, yet 42% of treatment programs were located in states that required physician involvement in treatment planning to bill Medicaid. Treatment programs included private for-profit programs (22%), private not-for-profit programs (62%), and publicly-owned programs (12%). The majority of programs in the sample focused on the provision of outpatient treatment, with 7% reporting provision of inpatient treatment, and 17% reporting provision of residential treatment. Roughly 34% offered opioid treatment.
TABLE 1.
Estimated Prevalence of State and Treatment Program Features
| Variable | Totala (n = 692) | s.d.b |
|---|---|---|
| Benefits Design | ||
| Benefits restrictiveness (scale) | 2.66 | 0.051 |
| Extent of use of utilization controls (scale) | 4.07 | 0.016 |
| Percent residents Medicaid eligible | 18.0 | 0.016 |
| Program Capacity | ||
| Use of electronic health records | 56.1 | |
| Ability to bill insurance | 72.5 | |
| Percent staff w/ computers | 96.5 | 0.063 |
| Physician employed on staff | 56.0 | |
| Physician required for treatment | 42.0 | |
| Control Variables | ||
| Private for-profit ownership | 21.9 | |
| Private non-profit ownership | 62.4 | |
| Publicly-owned | 12.1 | |
| Offers inpatient treatment | 6.8 | |
| Offers residential treatment | 17.4 | |
| Opioid treatment program | 34.4 | |
| Accredited | 62.0 | |
| Average caseload (ordinal) | 2.43 | 0.044 |
| Number of Tx programs in county | 50.8 | 3.385 |
Estimates in percentages unless otherwise noted
s.d. connotes standard deviation
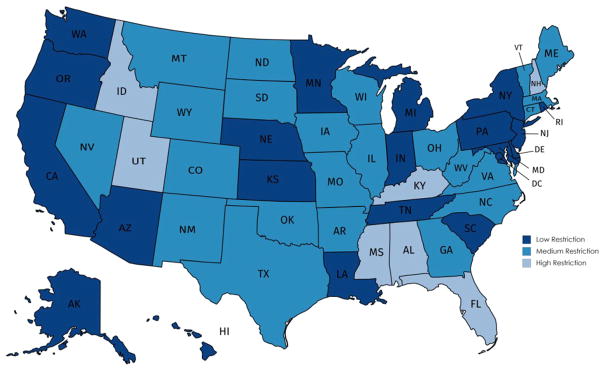
State Medicaid Benefits Restrictiveness
Our results show broad variation in states’ restriction of benefits for addiction treatment services (see Figure 1). About one in ten states (9.8%) rank among the highest for restrictiveness, with benefits for just 2 or fewer services and limitations placed on all of those services. Only one state provided benefits without limitations for all seven services outlined by ASAM. The average measure of restrictiveness across all states was 2.66 with a minimum score of 1 and a maximum score of 15. Among the states included in the study, the greatest number (9 states or 17.6%) provided benefits at the medium level (3–4 services covered) with limits imposed on all services. A more detailed description of state Medicaid benefits and utilization controls in these data can be found elsewhere (Grogan et al., 2016).
FIGURE 1.
Restrictiveness of Medicaid Benefits for Addiction Treatment by Statea,b
aData on restrictiveness of state Medicaid benefits for addiction treatment derived from the 2014 wave of the National Drug Abuse Treatment System Survey
bBenefits restrictiveness was measured as the total number of the seven possible services covered by the state Medicaid program, which included outpatient, group outpatient intensive outpatient, short-term residential, long-term residential, medically-managed inpatient detoxification and treatment, and recovery support.
Medicaid Acceptance Among Treatment Programs
Results of mixed effects logistic regression models are presented in Table 2. We found a significant relationship between the restrictiveness of state benefits for addiction treatment services and provider acceptance of Medicaid. Providers in states with less restrictive Medicaid benefits for addiction treatment were more likely to accept Medicaid enrollees (AOR = 1.299; CI=1.025, 1.645). As shown in Figure 2, the differences in the predicted probability of Medicaid acceptance among high, medium, and low restrictiveness states were substantial—35%, 48%, and 61% respectively.
TABLE 2.
Results of Mixed Logistic Regression Model for State Benefit Design and Program Features
| Variable | Adjusted Odds Ratio | Confidence Interval | |
|---|---|---|---|
| Lower | Upper | ||
| Benefits Design | |||
| Benefits restrictiveness | *0.65 | 0.43 | 0.97 |
| Covers oral naltrexone | 1.87 | 0.34 | 10.30 |
| Covers methadone | 0.67 | 0.15 | 2.93 |
| Number of utilization limits | 0.95 | 0.84 | 1.06 |
| Percent residents Medicaid eligible | 1.03 | 0.86 | 1.22 |
| Program Capacity | |||
| Use of electronic health records | **2.75 | 1.37 | 5.52 |
| Ability to bill insurance | *2.38 | 1.16 | 4.89 |
| Percent staff with computers | *1.02 | 1.01 | 1.03 |
| Physician employed on staff | 0.96 | 0.41 | 2.23 |
| Physician required for treatment | 0.73 | 0.19 | 2.78 |
| Control Variables | |||
| Nonprofit | **3.33 | 1.35 | 8.21 |
| Publicly-owned | *4.02 | 1.21 | 13.33 |
| Offers inpatient treatment | 1.33 | 0.36 | 4.91 |
| Offers residential treatment | **0.32 | 0.13 | 0.77 |
| Opioid treatment program (OTP) | 0.72 | 0.19 | 2.68 |
| Accredited | 2.06 | 0.86 | 4.93 |
| Average Caseload | 0.98 | 0.71 | 1.34 |
| Number of Tx Programs in county | 0.10 | 0.99 | 1.00 |
| Methadone* OTP interaction | *3.21 | 1.02 | 10.15 |
p<0.05;
p<0.01
FIGURE 2.
Predicted Probability of Medicaid Acceptance Among Addiction Treatment Programs
Across Selected Levels of Benefits Restrictivenessa
aBenefits restrictiveness was measured as the total number of the seven possible services covered by the state Medicaid program, which included outpatient, group outpatient intensive outpatient, short-term residential, long-term residential, medically-managed inpatient detoxification and treatment, and recovery support. Restrictiveness was measured as low (scores 1–2), medium (scores 3–4), or high (scores 5–7)
Several organizational factors were also positively associated with Medicaid acceptance. Addiction treatment programs that were accredited (AOR=2.998; CI=1.262, 7.127), and publicly-owned (AOR=4.56; CI=1.347, 15.425) had greater odds of accepting Medicaid enrollees. In addition, programs with more advanced technological capabilities were more likely to accept Medicaid. For example, the odds of accepting Medicaid were greater in facilities equipped with resources to maintain electronic health records (AOR=1.98; CI=1.203, 3.251), bill health insurance plans (AOR=2.54; CI=1.128, 5.708), and provide staff with computers (AOR=1.02; CI=1.004, 1.038). Addiction treatment programs offering residential treatment were less likely to accept Medicaid (AOR=0.385; CI= −5.995, 0.889).
DISCUSSION
Findings from this national survey of addiction treatment programs and state Medicaid agencies in the United States suggest that the restrictions placed on Medicaid addiction benefits may influence treatment programs’ likelihood of accepting Medicaid enrollees. We found that addiction treatment programs in states whose Medicaid programs provided more addiction treatment benefits were nearly twice as likely to accept Medicaid enrollees as those that provided few benefits. This finding suggests that addiction treatment programs may be looking closely at the restrictions on Medicaid benefits when making decisions about whether it will be worthwhile to accept Medicaid enrollees. This finding aligns with prior research suggesting that fewer restrictions on benefits are related to greater likelihood of provider acceptance (Andrews, 2014; McElrath, Chriqui, & McBride, 2011). However, our study also takes a step further by examining the use of utilization controls. Somewhat surprisingly, use of such controls was not associated with Medicaid acceptance. This finding suggests that states’ decisions regarding covering a service may have a more significant impact on Medicaid acceptance than their decisions to impose utilization controls on the service. This could be due to the relative ubiquity of utilization controls not only within Medicaid, but also among other major payers of addiction treatment, including private insurers and Substance Abuse Treatment and Prevention block grant funds. However, additional research is needed to further examine issue.
This study is also the first to explore the role of potential barriers to Medicaid acceptance among treatment programs, such as technological and staffing limitations on becoming Medicaid billable providers. We found that several organizational factors were strongly linked to increased odds of provider acceptance. All of the variables we used to assess the relationship of programs’ technological capabilities to Medicaid acceptance proved significant. Use of electronic health records, ability to bill insurance, and percent staff with computers were all associated with a greater odds of Medicaid acceptance. For example, the odds of accepting Medicaid doubled among those programs with access to electronic health records. Since nearly all state Medicaid programs require addiction treatment programs to provide detailed information regarding enrollee services and fees, as well as to report on outcomes, possessing the technology to achieve these ends is critical to participation in Medicaid. Our findings suggest that the absence of technological infrastructure—a common challenge among many addiction treatment programs—may inhibit their capacity to accept Medicaid.
Existing explanations that account for Medicaid acceptance among medical care providers may be inadequate to understand the forces that impact this decision within the context of the addiction treatment system. These explanations focus primarily on the perceived profitability of Medicaid as it relates to administrative hassles, reimbursement and local demand for care. While several accounts (e.g., Backus et al., 2001) highlight the significance of administrative burden on providers’ decisions to accept Medicaid, the administrative barriers to Medicaid acceptance facing addiction treatment differ. Existing accounts focus primarily on challenges related to time and resources required to bill Medicaid, and long wait times to receive payment. This situation differs somewhat from that of the addiction treatment system, in which a considerable proportion of treatment programs lack the technological capacity to bill Medicaid, and many also do not employ licensed professionals whose services are reimbursable under Medicaid (Andrews et al. 2015; McLellan & Meyers, 2004; Buck, 2011). Any theoretical framework for understanding Medicaid acceptance in addiction treatment must account for such barriers.
Accreditation and ownership were also linked to Medicaid acceptance. Publicly-owned addiction treatment programs had dramatically higher odds of accepting Medicaid than for-profit treatment programs. This finding aligns with prior research by McElrath and colleagues (2011), who found a relationship between benefits design and Medicaid acceptance for publicly-owned programs, but not for private for-profit and non-profit programs. Publicly-owned programs have a long history of providing services to individuals unable to pay for treatment in the private sector (Wheeler & Nahra, 2000). This finding is consistent with the mission of these programs. Accredited programs had three times greater odds of accepting Medicaid than programs without accreditation. Accreditation by the Joint Commission and CARF requires outcomes measurement and maintenance of a professional, licensed staff—also requirements for billing Medicaid.
Finally, our findings suggest that residential treatment programs are less likely to accept Medicaid. The Medicaid Institution for Mental Diseases (IMD) Exclusion, which prohibits the use of federal Medicaid financing for behavioral health treatment in residential facilities with more than 16 beds, may explain this finding. Hopefully, states will begin to address this issue in response to the ACA’s “final rule,” which granted Medicaid Managed Care Organizations an exception to the IMD exclusion in 2016 (MACPAC, 2016). However, because few states currently cover residential addiction treatment (Grogan et al., 2016), the effect of the final rule may be quite limited.
Limitations
Several limitations of this study are noteworthy. First, it draws from cross-sectional data. As a consequence, we are unable to assess causality. For example, it is possible that states in which the prevalence of addiction treatment programs that accept Medicaid is great may be more likely to lobby their state Medicaid programs to provide less restrictions on benefits for addiction treatment. Longitudinal studies are needed to track changes in benefits over time and assess the subsequent impact on rates of Medicaid acceptance among programs. Second, we were unable to measure reimbursement rates for addiction treatment services covered under state Medicaid fee-for-service arrangements. Our data collection, which attempted to gather this information via survey, yielded significant missing data. The high level of missing data resulted from a general lack of knowledge regarding the specifics of addiction treatment services reimbursement among survey respondents, as well as complexities in some state Medicaid program reimbursement structures (e.g. differential rates paid out for services to different populations and/or different providers). Furthermore, in some states, all addiction treatment benefits are provided under fully capitated financing models.
Additionally, our measures of Medicaid benefits may not accurately reflect the benefits some enrollees in Medicaid managed care programs may receive. While all Medicaid managed care programs must cover a minimum set of services defined by states, they often have some discretion with regard to use of utilization controls, and thus do not allow for a nuanced representation of within-state variation across these domains (Grogan et al., 2017). We were also unable to account for differences among states in the frequency of use of utilization controls. Lastly, it is possible that some addiction treatment programs that do not accept Medicaid may still yet serve Medicaid enrollees using Substance Abuse Prevent and Treatment block grant funds. Given that our data are aggregated at the program level, we not are not able to identify such instances in our study.
Implications
The findings of this study highlight an important link between restrictions placed on services for addiction treatment and programs’ decisions about whether to serve Medicaid enrollees. This insight is potentially important for policymakers who are interested in identifying strategies to enhance access to addiction treatment for the Medicaid population. Given the strong relationship between benefits restrictions and Medicaid acceptance, it is likely that programs are sensitive to benefits decisions made at the state levels, and that increasing the scope of covered services may result in more programs accepting Medicaid enrollees. Enhancing the number of addiction treatment programs that accept Medicaid is of particular importance in light of the opioid epidemic, which shows no signs of abating (Friedmann, Andrews, & Humphreys, 2017). Finally, our findings also have potential implications for the debate over repeal of the Affordable Care Act, which would result in the remove several regulations designed to ensure adequate benefits for addiction treatment under Medicaid. Our findings leave open the possibility that a decrease in the scope of Medicaid benefits for addiction treatment could result in more addiction treatment programs choosing to turn away Medicaid enrollees. However, further research is needed to assess how future proposals for ACA repeal may impact treatment availability and access for Medicaid enrollees.
HIGHLIGHTS.
Addiction treatment programs are more likely to accept Medicaid in states with less restrictive benefits for addiction treatment.
The predicted probability of Medicaid acceptance was 35.4% in highly restrictive states and 61.2% in the least restrictive states.
Technological infrastructure was also strongly linked to Medicaid acceptance.
Overall, 58% of addiction treatment programs reported that they accepted Medicaid as a form of payment for services.
Acknowledgments
The research reported in this article was supported by the National Institute on Drug Abuse of the National Institutes of Health (NIH) (Grant No. R01DA034634).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Society of Addiction Medicine (ASAM) The ASAM Criteria. 2016 Retrieved from: http://www.asam.org/quality-practice/guidelines-and-consensus-documents/the-asam-criteria.
- American Society of Addiction Medicine (ASAM) Advancing access to addiction medications: Implications for opioid addiction treatment. 2013 Retrieved from: http://www.asam.org/docs/default-source/advocacy/aaam_implications-for-opioid-addiction-treatment_final.
- Andrews CM, Shin HC, Marsh JC, Cao D. Client and program characteristics associated with wait time to substance abuse treatment entry. The American Journal Drug and Alcohol Abuse, Early Online. 2012:e1–8. doi: 10.3109/00952990.2012.694515. [DOI] [PubMed] [Google Scholar]
- Andrews CM. The relationship of state Medicaid coverage to Medicaid acceptance among substance providers in the United States. Journal of Behavioral Health Services & Research. 2014:1–12. doi: 10.1007/s11414-013-9387-2. [DOI] [PubMed] [Google Scholar]
- Andrews C, Abraham A, Grogan C, Pollack H, Bersamira C, Humphreys K, Friedmann P. Despite resources from the ACA, most states do little to help addiction treatment programs implement health care reform. Health Affairs. 2015;35(5):828–835. doi: 10.1377/hlthaff.2014.1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Backus L, Osmond D, Grumbach K, Vranizan K, Phuong L, Bindman AB. Specialists’ and primary care physicians’ participation in Medicaid managed care. Journal of General Internal Medicine. 2001;16(12):815–821. doi: 10.1111/j.1525-1497.2001.01239.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker LC, Royalty AB. Medicaid policy, physician behavior, and health care for the low-income population. 1997 Retrieved from: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=49206.
- Barbee A. When access isn’t equal: Enforcing the Medicaid equal access provision In Medicaid managed care contracts. Public Contract Law Journal. 2016;45(2):383–402. [Google Scholar]
- Berman S, Dolins J, Tang SF. Factors that influence the willingness of private primary care pediatricians to accept more Medicaid patients. Pediatrics. 2002;110:239–248. doi: 10.1542/peds.110.2.239. [DOI] [PubMed] [Google Scholar]
- Buck JA. The looming expansion and transformation of public substance abuse treatment under the Affordable Care Act. Health Affairs. 2011;30(8):1402–1410. doi: 10.1377/hlthaff.2011.0480. [DOI] [PubMed] [Google Scholar]
- Busch SH, Meara E, Huskamp HA, Barry CL. Characteristics of adults with addiction disorders expected to be eligible for Medicaid under the ACA. Psychiatric Services. 2013;64(6):520–526. doi: 10.1176/appi.ps.201200011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr CJA, Xu J, Redko C, Lane T, Rapp C, Goris J, Carlson RG. Individual and system influences on waiting time for substance abuse treatment. Journal of Substance Abuse Treatment. 2008;34(2):192–201. doi: 10.1016/j.jsat.2007.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings JR, Wen H, Ko M, Druss B. Race/Ethnicity and geographic access to Medicaid addiction disorder treatment facilities in the United States. JAMA Psychiatry. 2014;71(2):190–196. doi: 10.1001/jamapsychiatry.2013.3575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham P, May J. Medicaid patients increasingly concentrated among physicians. 2006 Retrieved from: p:// www.hschange.org/CONTENT/866/866.pdf. [PubMed]
- D’Aunno T. The role of organization and management in substance abuse treatment: Review and roadmap. Journal of Substance Abuse Treatment. 2006;31(3):221–233. doi: 10.1016/j.jsat.2006.06.016. [DOI] [PubMed] [Google Scholar]
- D’Aunno T, Friedmann PD, Chen Q, Wilson DM. Integration of substance abuse treatment organizations into accountable care organizations: Results from a national survey. Journal of Health Politics, Policy and Law. 2015;40(4):797–819. doi: 10.1215/03616878-3150062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Aunno T, Pollack H, Chen Q, Friedmann PD. Linkages between patient-centered medical homes and addiction treatment organizations: Results From a national survey. Medical Care. 2017;55(4):379–383. doi: 10.1097/MLR.0000000000000645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedmann PD, D’Aunno TA, Jin L, Alexander JA. Medical and psychosocial services in drug abuse treatment: Do stronger linkages promote client utilization. Health Services Research. 2000;35(2):443–465. [PMC free article] [PubMed] [Google Scholar]
- Friedmann PD, Lemon SC, Durkin EM, D’Aunno TA. Trends in comprehensive service availability in outpatient drug abuse treatment. Journal of Substance Abuse Treatment. 2003;24(1):81–88. doi: 10.1016/s0740-5472(02)00323-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedmann PD, Andrews CM, Humphreys K. How ACA repeal would worsen the opioid epidemic. New England Journal of Medicine. 2017;376(10):e16. doi: 10.1056/NEJMp1700834. [DOI] [PubMed] [Google Scholar]
- Gabel JR, Rice TH. Reducing public expenditures for physician’s services: The price of paying less. Journal of Health Politics, Policy and the Law. 1985;9:595–609. doi: 10.1215/03616878-9-4-595. [DOI] [PubMed] [Google Scholar]
- Grogan CM, Andrews C, Abraham A, Humphreys K, Pollack H, Smith BT, Friedmann PD. Survey highlights difference in Medicaid coverage for addiction treatment and opioid use disorder medications. Health Affairs. 2016;35(12):2289–2296. doi: 10.1377/hlthaff.2016.0623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman KA, Ford JH, Tillotson CJ, Choi D, McCarty D. Days to treatment and early retention among patients in treatment for alcohol and drug disorders. Addictive Behaviors. 2011;36:643–647. doi: 10.1016/j.addbeh.2011.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mark TL, Levit KR, Vandivort-Warren R, Coffey RM, Buck JA the SAMHSA Spending Estimates Team. Trends in spending for substance abuse treatment, 1986–2003. Health Affairs. 2007;26(4):1118–1128. doi: 10.1377/hlthaff.26.4.1118. [DOI] [PubMed] [Google Scholar]
- Mark TL, Levit KR, Yee T, Chow CM. Spending on mental and addiction disorders projected to grow more slowly than all health spending through 2020. Health Affairs. 2014;33(8):1407–1415. doi: 10.1377/hlthaff.2014.0163. [DOI] [PubMed] [Google Scholar]
- McAuliffe WE, Dunn R. Substance abuse treatment needs and access in the USA: interstate variations. Addiction. 2004;99(8):999–1014. doi: 10.1111/j.1360-0443.2004.00783.x. [DOI] [PubMed] [Google Scholar]
- McLellan TA, Meyers K. Contemporary addiction treatment: A review of systems problems for adults and adolescents. Biological Psychiatry. 2004;56(10):764–770. doi: 10.1016/j.biopsych.2004.06.018. [DOI] [PubMed] [Google Scholar]
- Medicaid and CHIP Payment and Access Commission (MACPAC) The Medicaid Institution for Mental Diseases (IMD) Exclusion. 2016 Mar; Retrieved from: https://www.macpac.gov/wp-content/uploads/2016/03/The-Medicaid-Institution-for-Mental-Diseases-IMD-Exclusion.pdf.
- Mitchell JB. Physician Participation in Medicaid Revisited. Medical Care. 1991;29(7):645–653. doi: 10.1097/00005650-199107000-00004. [DOI] [PubMed] [Google Scholar]
- Perron BE, Gillespie DF, Alexander-Eitzman B, Delva J. Availability of outpatient addiction disorder treatment programs in the United States. Addiction & Misuse. 2010:45. doi: 10.3109/10826080903443602. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Association (SAMHSA) State profiles of mental health and substance abuse services in Medicaid (HHS Publication No. NMH05-0202) Rockville, MD: Substance Abuse and Mental Health Services Administration; 2005. [Google Scholar]
- Substance Abuse and Mental Health Services Association (SAMHSA) National Survey of Substance Abuse Treatment Services (N-SSATS): 2010. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2010. [Google Scholar]
- Substance Abuse and Mental Health Services Association (SAMHSA) National Survey of Substance Abuse Treatment Services (N-SSATS): 2014. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. HHS Publication No. SMA 16-4963. [Google Scholar]
- Terry-McElrath YM, Chriqui JF, McBride D. Factors related to Medicaid payment acceptance at outpatient substance abuse treatment programs. Health Services Research. 2011;46(2):633–653. doi: 10.1111/j.1475-6773.2010.01206.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheeler JRC, Nahra TA. Private and public ownership in outpatient substance abuse treatment: Do we have a two-tiered system? Administration and Policy in Mental Health and Mental Health Services Research. 2000 Mar;27(4):197–209. doi: 10.1023/a:1021357318246. [DOI] [PubMed] [Google Scholar]