Abstract
Background
In preparation for a randomized controlled trial (RCT), we conducted a pilot RCT of the acceptability and feasibility of diaphragms and candidate vaginal microbicide for sexually transmitted infection prevention among high-risk women in Madagascar.
Methods
Participants were randomized to four arms: (1) diaphragm (worn continuously) with Acidform™ applied in the dome; (2) diaphragm (worn continuously) with placebo gel hydroxyethylcellulose (HEC) in the dome; (3) HEC applied intravaginally before sex; (4) Acidform applied intravaginally before sex. All women were given condoms. Participants were followed weekly for 4 weeks. We fit unadjusted negative binomial regression models with robust variance estimators to generate the proportion of sex acts with casual partners where condoms and experimental study products were used.
Results
Retention was 98% among 192 participants. Experimental product use with casual partners was high, reported in 85%, 91%, 74%, and 81% of sex acts for women in the Acidform-diaphragm, HEC-diaphragm, HEC-alone, and Acidform-alone arms, respectively. However, the proportion reporting product use during 100% of acts with casual partners over the full follow-up period was much lower: 28% to 29% in the gel-diaphragm arms and 6% to 10% in gel-alone arms. Women used condoms in 62% to 67% of sex acts with casual partners, depending on the randomization arm. Participants found diaphragms easy to insert (97%) and remove (96%). Acidform users (with or without the diaphragm) reported more genitourinary symptoms than HEC users (14% vs. 5% of visits).
Conclusions
A sexually transmitted infection prevention RCT of candidate microbicide with and without the diaphragm appears acceptable and feasible in this population.
Women in resource-poor settings suffer disproportionately from sexually transmitted infections (STIs).1,2 Madagascar is a low-income country where STIs constitute a major public health concern, and rates are particularly high among women who exchange sex for money or goods. In 2001, among asymptomatic sex workers, 74% to 78% were infected with Neisseria gonorrhoeae (GC), Chlamydia trachomatis (CT), trichomoniasis, or syphilis.3 In a separate 2001 trial of male and female condom promotion among 1000 female sex workers, 6 months after receiving presumptive treatment, the combined prevalence of GC/CT infection was 26%.4 The high STI prevalence indicates that better control efforts are needed, especially given that STIs are likely to increase risk of HIV acquisition.5–7 HIV rates in Madagascar are currently low: the estimated prevalence in 2006 was <2% in vulnerable groups and 0.95% in the general population.8
Although male condoms, when used correctly and consistently, are the most effective method currently available for prevention of most STIs,9 many women lack the social and economic power to insist that their sex partners use them.2 Therefore, additional prevention methods are needed that are appropriate for and accessible to women.10,11 The diaphragm, used worldwide for prevention of pregnancy, has received attention as a possible infection-prevention method.12–14 Because GC, CT, and probably HIV preferentially infect the cervix and upper genital tract in women,15 physical barriers, such as diaphragms, may prevent sexually transmitted pathogens from reaching the cervix and thereby reduce infection risk. Several observational studies report protective effects for diaphragms against STIs and their long-term sequelae,16–21 though a recent large-scale randomized controlled trial (RCT) of women in Zimbabwe and South Africa [Methods for Improving Reproductive Health in Africa (MIRA)] found no added protective benefit of a diaphragm with commercial lubricant (compared with male condoms only) for HIV or STI prevention.22,23 Topical vaginal microbicides have also been promoted as female-initiated methods to prevent STI/HIV acquisition, although no effective product is yet available.24 Several studies have reported high acceptability of microbicides and diaphragms for STI prevention among both women and men.25–31
We plan to conduct an RCT evaluating the STI-prevention effectiveness of 2 women-initiated methods—candidate vaginal microbicide and latex diaphragm—individually and in combination. In anticipation of the RCT, we carried out this 4-arm, partially masked, randomized, prospective pilot trial to assess the acceptability of assigned study products (diaphragm, candidate microbicide and placebo gels, gel applicators, and male condoms) and the feasibility of conducting a large clinical trial measuring their effectiveness for GC and CT prevention. Over 4 weeks, we measured participants’ use of and comfort with study products.
Materials and Methods
Study Sites and Population
Participants were recruited through community outreach in 4 cities in Madagascar: Antananarivo, Antsiranana, Mahajanga, and Toamasina. Eligible women were 15 to 55 years old (though the youngest participant was 16 years old), had at least 4 sex partners in the past month, reported less than 100% condom use in the past 2 weeks, intended to stay in the area for the next month, were not pregnant or planning pregnancy in the next 2 months, had no allergy to latex and no physical abnormality that precluded diaphragm use, and were able to give informed consent.
Study Products
Participants used various combinations (see below) of 6 study products: candidate topical microbicide Acidform™ (Instead, LA Jolla, CA); placebo gel, hydroxyethylcellulose (HEC) (ReProtect LLC, Baltimore, MD); latex diaphragm (All-Flex Arcing Spring Diaphragm, Ortho-McNeil Pharmaceutical, Titusville, NJ); disposable, paper gel applicator (TekPak, Marion, AL); reusable, plastic gel applicator (Nik Thread Applicator, HTI Plastics, Lincoln, NE); and nonlubricated male condoms (Alatech Health Care, Dothan, AL and Protector Plus, Surtex Limited, Thailand; distributed by Population Services International in Madagascar).
Acidform
Acidform gel has acidifying, bioadhesive, and viscosity-retaining properties intended to serve 2 purposes: to provide effective acidification of male ejaculate in the vagina, and to form a long-lasting layer of gel over the vaginal and cervical surfaces. Acid-form is buffered at pH 3.5, thus maintaining an acidic pH in the vagina after semen deposition. In addition, the gel bioadheres to form a protective layer with prolonged retention in the vagina.32,33 Acidform shows antimicrobial activity against herpes simplex virus type 2, CT, GC, Trichomonas vaginalis and microbes leading to bacterial vaginosis.33–35 Phase I human safety trials and small-scale pilot studies indicate that Acidform is safe, well tolerated, and generally acceptable to women and men.36–42
HEC (Placebo Gel)
HEC is a safe, water-based gel formulation designed to be an inert control gel for masked trials of vaginal microbicides.43–45 The pH of HEC gel is 4.4.
All-Flex Arcing Spring Diaphragm
The All-Flex Arcing Spring Diaphragm is a molded, natural rubber vaginal diaphragm, approved by the US Food and Drug Administration for contraception when used with spermicide.
Study Procedures
At screening, women underwent testing for pregnancy and urinary tract infection (UTI) (Clearview HCG Combo, Wampole Laboratories, Cranbury, NJ and Multistix 10SG; Bayer, Tarry-town, NY) and face-to face eligibility evaluation using a brief questionnaire. Eligible women were randomized to 4 groups: Acidform with diaphragm; HEC with diaphragm; HEC alone; and Acidform alone. Each woman was also randomly assigned a disposable paper or reusable plastic applicator; after 2 weeks, women switched applicator type for the second half of the study. Randomization was stratified by site. Treatment assignments were partially masked. Because of the nature of the intervention, assignment of diaphragms was not masked. However, neither participants, the on-site research staff, nor data analysts were aware of gel assignments.
At enrollment, 1 week after screening, participants received clinician-administered face-to-face interviews to collect demographic, reproductive, and sexual behavior data. Clinicians also performed pregnancy testing for all women and diaphragm fitting for women randomized to the gel-diaphragm arms. All participants received counseling on use of their assigned study products, including male condoms, as well as sufficient supplies to last until the next study visit. All women received presumptive treatment for gonococcal, chlamydial, and trichomonal infections according to Madagascar’s national guidelines.3
Participants were instructed to use male condoms with every sex act. Women in the gel-diaphragm arms were asked to use the diaphragm continuously, removing it once per 24-hour period for cleaning. After cleaning, we requested that they fill the diaphragm dome with their assigned gel, using an applicator to ensure consistency in dose, and then reinsert the diaphragm. Participants in gel-only arms were instructed to insert their assigned gel intravaginally, again using an applicator, before each sex act. All women were instructed not to practice internal vaginal cleaning while participating in the study.
Participants returned once weekly for 4 weeks. At each visit, they again received face-to-face interviews about their use of and problems with study products. Participants also underwent pelvic examination and received resupplies of study products. At the final follow-up visit, women returned their diaphragms, applicators, and any unused gel.
Ethical Approval
All women gave written informed consent for screening and again for enrollment. The study was approved by institutional review boards at the University of North Carolina at Chapel Hill and the US Centers for Disease Control and Prevention (CDC), as well as the Comité d’Ethique auprès du Ministere de la Santé in Madagascar.
Young women aged 16 and 17 participated in this pilot trial. As with our other research in this population, we petitioned each of the 3 ethical review boards and were approved to classify adolescents as young as 15 years old as adults for the purposes of this study. The rationale for this classification was 2-fold. First, the highest STI morbidity among attendees of our clinics in Madagascar is seen among the youngest women,46 making these participants the very group most likely to benefit from the proposed research. Second, parental permission for participation was not feasible. Many adolescents receiving care in study clinics have run away from home and are living on their own or residing with a boyfriend. Most have no contact with a parent or guardian.
Statistical Analysis
Data from questionnaires and clinical examination were double entered in EpiInfo (Version 6, CDC, Atlanta, GA) by staff at the data management unit LARTIC at the Université d’Antananarivo in Antananarivo, Madagascar and were verified at CDC. All analyses were conducted using SAS (SAS Institute, Version 9.1.3, Cary, NC).
Outcome measures—acceptability and feasibility—are summaries of several constructs. We evaluated participants’ comfort with products and recommended protocols for using them, including their patterns of use of gel with diaphragm and gel alone, and their reported ease of insertion, removal and cleaning of diaphragms and applicators; we assessed these behaviors by study arm and visit. We also examined the occurrence of self-reported genitourinary symptoms (itching, discharge, bleeding, pain, or problems urinating), clinician-identified abnormalities on pelvic examination, and adverse events (AEs) in each randomization group.
We assessed self-reported use of (a) condoms and (b) assigned experimental products by computing the proportion of sex acts with casual partners during which products were used. Using the total number of acts with casual partners as the offset variable, we fit separate unadjusted negative binomial regression models with robust variance estimators to generate the proportion and 95% confidence intervals (CIs) of sex acts with casual partners where condoms and experimental study products were used over the last week, by randomization group and follow-up visit. We used negative binomial regression rather than Poisson regression because of substantial extra-Poisson variability in some models. Because of the small number of women reporting primary partners and the low reported frequency of sex with those partners, and because sexual behavior is expected to differ depending on partner type, we restricted our measures of condom use and experimental product use to sex acts with casual partners.
We used intent-to-treat analysis guidelines47 and included all person-time contributed by all participants in the presented analyses. Because of the small sample size and the exploratory, descriptive purpose of this pilot study, we did not conduct formal statistical significance testing.
Results
The study was conducted between September and November 2005 and enrolled a total of 192 women from the 4 clinical sites: 48 women per site and 48 women per randomization group.
Screening
Of 314 screened women, 192 (61%) were enrolled. The most common reasons for ineligibility were using condoms consistently in the past 2 weeks (37%), having fewer than 4 partners in the past month (25%), planned or existing pregnancy (15%), and self-reported allergy to latex (11%).
Baseline Characteristics
We saw few differences in baseline participant characteristics between randomization groups (Table 1). Few participants (11%) were married or cohabitating. In response to the question, “what kind of work do you do to earn money?” 81% reported sex work; when directly asked, 100% reported that they had ever had sex to earn money. Age (median: 29 years), age at coital debut (median: 17 years), and completed years of education (median: 5.5 years) were similar across groups. More than half of participants (59%) had electricity in their homes, but running water was less common (18%). A majority (55%) had ever used highly effective contraception (hormonal methods, IUD, or sterilization), but use of these methods at the last sex act was lower (24%). Women frequently engaged in extensive vaginal hygiene practices (88% reported cleaning internally more than once daily).
TABLE 1.
Baseline Demographic, Reproductive, and Sexual Characteristics, by Randomization Group
| AF-Diaphragm (n = 48) |
HEC-Diaphragm (n = 48) |
HEC-Alone (n = 48) |
AF-Alone (n = 48) |
Total (n = 192) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | n | % | n | % | n | % | n | % | n | % |
| Marital status | ||||||||||
| Never married | 20 | 42 | 24 | 50 | 18 | 38 | 25 | 52 | 87 | 45 |
| Cohabitating/married | 6 | 13 | 5 | 10 | 6 | 13 | 5 | 10 | 22 | 11 |
| Divorced/separated/widowed | 22 | 46 | 19 | 40 | 24 | 50 | 18 | 38 | 83 | 43 |
| Sex work reported as profession | 37 | 77 | 35 | 73 | 43 | 90 | 41 | 85 | 156 | 81 |
| Electricity in home | 27 | 56 | 30 | 63 | 27 | 56 | 29 | 60 | 113 | 59 |
| Tap water in house/on property | 10 | 21 | 6 | 13 | 10 | 21 | 8 | 17 | 34 | 18 |
| Ever used highly effective* contraception | 31 | 65 | 24 | 50 | 22 | 46 | 29 | 60 | 106 | 55 |
| Highly-effective* contraception at last sex | 14 | 29 | 10 | 21 | 10 | 21 | 12 | 25 | 46 | 24 |
| Ever used condom for HIV/STI or pregnancy prevention | 47 | 98 | 48 | 100 | 48 | 100 | 48 | 100 | 191 | 99 |
| Condom for HIV/STI or pregnancy prevention at last sex | 30 | 63 | 36 | 75 | 34 | 71 | 31 | 65 | 131 | 68 |
| Always/almost always use condom in the last week with | ||||||||||
| Husband/boyfriend† | 1 | 5 | 2 | 11 | 4 | 16 | 2 | 12 | 9 | 11 |
| Casual partners | 22 | 46 | 19 | 40 | 25 | 52 | 26 | 54 | 92 | 48 |
| Ever experienced violence from casual partner after suggestion of condom use | 5 | 10 | 9 | 19 | 14 | 29 | 12 | 25 | 40 | 21 |
| Reported history of ulcers or STI diagnosis | 24 | 50 | 28 | 58 | 29 | 60 | 25 | 52 | 106 | 55 |
| Ever received more money for sex without condom | 21 | 44 | 15 | 31 | 19 | 40 | 17 | 35 | 72 | 38 |
| Ever anal sex | 4 | 8 | 5 | 10 | 9 | 19 | 5 | 10 | 23 | 12 |
| Internal vaginal cleaning | ||||||||||
| More than once a day | 41 | 85 | 44 | 92 | 43 | 90 | 40 | 83 | 168 | 88 |
| Once a day or less often | 7 | 15 | 4 | 8 | 5 | 10 | 8 | 17 | 24 | 13 |
| Median | IQR | Median | IQR | Median | IQR | Median | IQR | Median | IQR | |
|
| ||||||||||
| Age (yrs) | 29 | 24–37 | 27.5 | 23.5–33.5 | 29 | 25–35.5 | 30.5 | 24–36 | 29 | 24–36 |
| Age at coital debut (yrs) | 17 | 16–18 | 16 | 15–18 | 17 | 15–18 | 16 | 15.5–17.5 | 17 | 15–18 |
| Education (yrs) | 6 | 4–9 | 5 | 3.5–8 | 5 | 4.5–8 | 6 | 4–8 | 5.5 | 4–8 |
| Number of pregnancies | 3 | 2–5 | 2 | 1–4 | 3 | 2–4 | 3 | 2–4.5 | 3 | 2–4 |
| Casual partners in typical week | 7 | 5–11 | 5 | 3–8 | 6 | 4–8.5 | 5 | 3–9 | 6 | 4–9 |
| Sex acts in typical week | 10 | 6.5–16.5 | 9 | 6–13 | 8.5 | 5–11.5 | 10 | 6–15 | 10 | 6–15 |
| Sex acts with primary partner in last week† | 2 | 1–4 | 2 | 0–3 | 2 | 1–3 | 2 | 2–3 | 2 | 1–3 |
Effective contraception = sterilization, hormonal methods (oral contraceptive pills, injectable depot medroxyprogesterone acetate, or implant Norplant) and intrauterine devices.
Among 79 women reporting a husband or boyfriend (19 in AF-diaphragm arm, 18 in the HEC-diaphragm, 25 in the HEC-alone arm, and 17 in the AF-alone arm.
AF indicates Acidform; HEC, hydroxyethylcellulose (placebo gel); IQR, interquartile range.
Reported condom use was much higher with casual partners than with primary partners (husbands or boyfriends). Despite the exclusion at screening of women reporting consistent condom use with all partners, 48% of enrolled women reported always or almost always using condoms with casual partners compared with 11% with primary partners. More than half (55%) self-reported a previous STI or genital ulcer. The number of casual partners in a typical week [median: 6 partners, interquartile range (IQR): 4–9 partners], total sex acts in a typical week (median: 10 acts, IQR: 6–15 acts), and sex acts with the primary partner in the last week [among the subgroup of participants reporting a husband or boyfriend (n = 79, median: 2 acts, IQR: 1–3 acts)] were also similar across randomization groups (Table 1).
Follow-Up
Retention over the 4-week study period was 98% (188 participants attended the week 4 visit). One participant voluntarily withdrew from the study, 1 woman was lost to follow-up, and 2 women were discontinued by study staff during follow-up because they were unable to insert the diaphragm. (All 4 participants had been randomized to the Acidform-diaphragm arm.)
Our analyses include 753 person-weeks (PW) of follow-up time: 178, 192, 192, and 191 PWs from the Acidform-diaphragm, HEC-diaphragm, HEC-alone, and Acidform-alone arms, respectively.
Sexual Behavior
The median number of weekly sex acts with all partners, as well as the median number of casual partners, was higher during follow-up than at baseline for all randomization groups, though these figures are not strictly comparable because the baseline questionnaire asked about behavior during a typical week and the follow-up questionnaire asked about behavior in the past week. At enrollment, women’s median number of sex acts with all partners in a typical week was 10, 9, 8.5, and 10 acts for women in the Acidform-diaphragm, HEC-diaphragm, HEC-alone, and Acid-form-alone arms, respectively. Over follow-up, the median sex acts with all partners in the past week were 15, 14, 14, and 12 acts, respectively. Women’s reported numbers of casual partners were similarly higher at follow-up than baseline; 7, 5, 6, and 5 casual partners in a typical week were reported at baseline by women in the Acidform-diaphragm, HEC-diaphragm, HEC-alone, and Acid-form-alone arms, respectively, compared with 15, 12, 12, and 11 casual partners in the last week on average over follow-up.
Condom Use
Over the full follow-up period, participants used condoms in 66% of sex acts with casual partners (95% CI: 63%–68%) (Fig. 1). On average, Acidform-diaphragm users used condoms in 62% of acts with casual partners (95% CI: 57%–67%), HEC-diaphragm users in 67% of acts (95% CI: 62%–73%), HEC-alone users in 66% of acts (95% CI: 60%–73%), and Acidform-alone users in 67% of acts (95% CI: 61%–73%). Generally, condom use increased throughout the study period, with the exception of the Acidform-diaphragm arm, in which condom use declined somewhat between weeks 3 and 4 (Fig. 1).
Fig. 1.
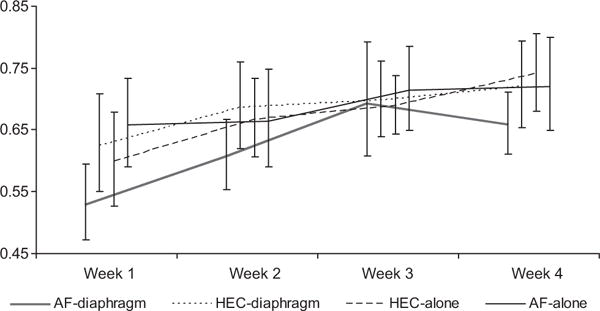
Proportion of sex acts with casual partners in the last week in which male condoms were used, with 95% confidence intervals, by randomization group and study visit.
The proportion of sex acts with casual partners in which neither male condoms nor experimental products were used was low for all study groups (4% of sex acts overall, 95% CI: 3%–5%).
Diaphragm and Gel Use During Sex
The proportion of sex acts with casual partners in which experimental study products were used (regardless of condom use) ranged over follow-up and by arm, from a minimum of 66% (HEC-alone arm, week 2) to a maximum of 94% of sex acts (HEC-diaphragm arm, week 4) (Fig. 2). In general, women in the 2 gel-diaphragm arms used products with casual partners more consistently (in 88% of acts, 95% CI: 84%–92%) than women in the 2 gel-only arms (in 78% of acts, 95% CI: 74%–81%).
Fig. 2.
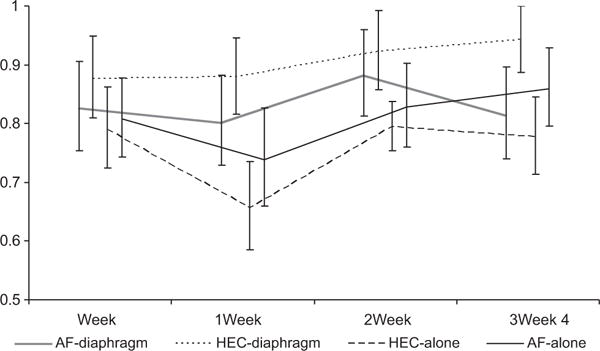
Proportion of sex acts with casual partners in the last week in which experimental study products were used (gel and diaphragm for gel-diaphragm groups and gel only for gel-only groups), with 95% confidence intervals, by randomization group and study visit.
A comparison of the 2 gel-diaphragm groups indicates that women assigned to the HEC-diaphragm arm used their study products with casual partners more consistently at every time point than women in the Acidform-diaphragm arm. This difference is most extreme at the final visit, with women in the Acidform-diaphragm arm using products in 81% of sex acts with casual partners and women in the HEC-diaphragm arm at 94% of acts. Comparing the gel-only arms, those in the Acid-form-alone arm used their products more consistently than those in the HEC-alone arm at every time point. Again, the most extreme difference occurred at the week 4 visit, where women in the HEC-alone arm used gel in 78% of sex acts with casual partners and women in the Acidform-alone arm in 86% of acts.
The number of participants in each study group who reported using experimental study products in 100% of sex acts with casual partners over the full 4 weeks of follow-up was low: 28% of women randomized to the Acidform-diaphragm arm, 29% of HEC-diaphragm users, 6% HEC-alone users, and 10% of Acid-form-alone users.
Participant Experiences With Diaphragm
Women in the 2 gel-diaphragm arms reported at 92% of follow-up visits that they were somewhat comfortable or comfortable wearing their diaphragms continuously, and the proportion expressing comfort with continuous use increased over time from 88% at the first follow-up visit to 95% at the final visit (Table 2). However, at approximately 20% of these visits, women also reported inserting the diaphragm more than once daily during the previous week (an indication that they had not followed the continuous use protocol). Women reported at few visits that they ever left their devices in longer than 24 hours in the past week (reported at 4% of visits by 11 participants). Removal of the diaphragm after every sex act, regardless of partner type, was also rarely reported (at 4% of visits by 13 participants). Most women (at 91% of visits in the Acidform-diaphragm arm and 96% of visits in the HEC-diaphragm arm) also said they did not reinsert gel intravaginally after the diaphragm was in place (reinsertion was not recommended under the protocol). Nearly all participants found inserting and removing the diaphragm easy (at 97% and 96% of visits, respectively).
TABLE 2.
Diaphragm Use Patterns and Problems
| AF-Diaphragm
|
HEC-Diaphragm
|
Total
|
||||
|---|---|---|---|---|---|---|
| Reported Behavior | n = 178 Visits | %* | n = 192 Visits | %* | n = 370 Visits | %* |
| Somewhat comfortable/comfortable with continuous diaphragm use | 163 | 92 | 177 | 92 | 340 | 92 |
| Ever left diaphragm in continuously for more than 24 h | 7 | 4 | 9 | 5 | 16 | 4 |
| Diaphragm and gel insertion very/somewhat easy | 173 | 97 | 187 | 97 | 360 | 97 |
| Diaphragm removal very/somewhat easy | 170 | 96 | 187 | 97 | 357 | 96 |
| Diaphragm cleaning very/somewhat easy | 174 | 98 | 191 | 99 | 365 | 99 |
| Typically removed the diaphragm after each sex act in the last week | 10 | 6 | 4 | 2 | 14 | 4 |
| Ever removed and reinserted the diaphragm more than once a day | 43 | 24 | 34 | 18 | 77 | 21 |
| Inserted more gel after inserting diaphragm with gel (i.e., used gel more often than recommended by protocol) | ||||||
| Never | 162 | 91 | 185 | 96 | 347 | 94 |
| Sometimes | 10 | 6 | 4 | 2 | 14 | 4 |
| Inserted gel before each sex act | 1 | 1 | 1 | 1 | 2 | 1 |
| Reported any problem with diaphragm and gel† | 20 | 11 | 15 | 8 | 35 | 9 |
| Participant-reported genitourinary symptom(s) at physical exam: itching, discharge, bleeding, pain, dysuria, pelvic pain | 22 | 12 | 10 | 5 | 32 | 9 |
| Clinician-identified abnormalities on urethra, labia minora, labia majora, vagina, cervix, uterus, or adnexae | 10 | 6 | 5 | 3 | 15 | 4 |
Because of rounding and missing data, not all categories sum to 100%.
For example: difficulty inserting, removing, or keeping the diaphragm in continuously, device discovery by partners, etc.
AF indicates Acidform; HEC, hydroxyethylcellulose (placebo gel).
Participant Experiences With Gel
At approximately half of visits, gel-only users reported that they inserted gel before each sex act as instructed (Table 3). The protocol did not recommend removing gel, but at roughly one-third of visits, women in both gel-only groups reported that they removed the gel after every sex act (regardless of partner type). Most reported that partners did not ask about the amount of lubrication or discharge (64% of visits in the HEC-alone arm and 73% in the Acidform-alone arm). Almost all women were somewhat or very comfortable using the gel applicator, with no differences by applicator type (paper or plastic); the proportion expressing comfort with the applicator also increased with time from 90% at the first follow-up visit to 97% at the final visit. We did not directly ask participants which applicator they preferred.
TABLE 3.
Gel Use Patterns and Problems
| HEC-Alone
|
AF-Alone
|
Total
|
||||
|---|---|---|---|---|---|---|
| Reported Behavior | n = 192 Visits | %* | n = 191 Visits | %† | n = 383 Visits | %* |
| Typically inserted gel before every sex act | 97 | 51 | 104 | 54 | 201 | 53 |
| Typically removed gel after every sex act | 71 | 37 | 64 | 34 | 135 | 35 |
| Partner asked about amount of lubrication/vaginal discharge before sex | ||||||
| At least once | 67 | 35 | 46 | 24 | 113 | 30 |
| Never | 123 | 64 | 139 | 73 | 262 | 68 |
| Somewhat comfortable or comfortable with using gel applicator | 173 | 90 | 171 | 90 | 344 | 90 |
| Reported any problem with gel† | 21 | 11 | 20 | 11 | 41 | 11 |
| Participant-reported genitourinary symptom(s) at physical exam: itching, discharge, bleeding, pain, dysuria, and pelvic pain | 9 | 5 | 28 | 15 | 37 | 10 |
| Clinician-identified abnormalities on urethra, labia minora, labia majora, vagina, cervix, uterus, or adnexae | 11 | 6 | 17 | 9 | 28 | 7 |
Because of rounding and missing data, not all categories sum to 100%.
For example: difficulty finding time, privacy or opportunity to insert the gel, problems handing, filling or using the gel applicator, complaints of excess wetness, etc.
AF indicates Acidform; HEC, hydroxyethylcellulose (placebo gel).
Problems With Study Products
Women reported problems with study products at 76 visits (10%) over the study period. Gel-diaphragm users were most likely to report trouble keeping the diaphragm in continuously or to have problems with partners’ reactions to study product use (for example, partner discovery of products or insistence on product removal before sex) (Tables 2 and 3). In gel-only arms, most problems related to finding the time, opportunity or privacy to insert gel; trouble using the applicator; or problems with partners (such as a partner discovering the gel or applicator, or requesting that the participant wash before sex due to excess wetness). Problems declined somewhat by the end of follow-up: 19 women (10%) reported problems with study products at the first follow-up visit, 24 women (13%) at the second visit, 19 women (10%) at the third visit, and 14 women (7%) at the final visit (Tables 2 and 3).
Genitourinary Signs and Symptoms
Women using Acidform (with the diaphragm or alone) reported more gynecological symptoms, including itching, discharge, bleeding, pain, or problems urinating, compared with those using placebo gel. During examination of the external and internal genitalia, clinicians noted more abnormalities (such as ulcers, mucopurulent cervicitis, inflammation, or discharge) among women in the Acidform-alone arm (Tables 2 and 3).
Adverse Events
A total of 131 AEs were reported in 88 women over the follow-up period. Fifty-six women (29% of all participants) had 1 AE, 25 participants (13%) had 2 AEs, and 7 (4%) had 3 or more AEs (Table 4). AEs were more common in women using Acidform (62% of all AEs) than in participants using HEC. Most events (84%) required no action regarding product use, although investigators recommended stopping product use in 15 women (who reported 21 events). Of those 15, 9 restarted product use within 1 week of the AE diagnosis; the other 6 never reinitiated product use (2 of these experienced AEs at the final visit, so reinitiation was not an option). Most AEs (n = 103, 79%) resolved without sequellae, but a substantial minority (n = 23, 18%) remained unresolved at study exit. Information on resolution was missing for 5 AEs.
TABLE 4.
Adverse Events
| AF-Diaphragm
|
HEC-Diaphragm
|
HEC-Alone
|
AF-Alone
|
Total
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n = 32 | %* | n = 24 | %† | n = 26 | %* | n = 49 | %* | n = 131 | %* | |
| Type of adverse event | ||||||||||
| Genitourinary | 24 | 75 | 18 | 75 | 20 | 77 | 42 | 86 | 104 | 79 |
| Other (respiratory, digestive, other) | 8 | 25 | 6 | 25 | 6 | 23 | 7 | 14 | 27 | 21 |
| Action taken | ||||||||||
| None | 25 | 78 | 20 | 83 | 23 | 88 | 42 | 86 | 110 | 84 |
| Products discontinued today | 7 | 22 | 4 | 17 | 3 | 12 | 7 | 14 | 21 | 16 |
| Outcome | ||||||||||
| Resolved without sequellae | 25 | 78 | 20 | 83 | 19 | 73 | 39 | 80 | 103 | 79 |
| Unresolved at study exit† | 5 | 16 | 3 | 13 | 5 | 19 | 10 | 20 | 23 | 18 |
| Unknown, participant lost to follow-up | 1 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 |
| Unknown, missing | 1 | 3 | 1 | 4 | 2 | 8 | 0 | 0 | 4 | 3 |
| Adverse event classification | ||||||||||
| Not or unlikely to be related to study products | 8 | 25 | 5 | 21 | 10 | 38 | 11 | 22 | 34 | 26 |
| Possibly related to study products | 21 | 66 | 17 | 71 | 10 | 38 | 32 | 65 | 80 | 61 |
| Probably/definitely related to study products | 3 | 9 | 2 | 8 | 6 | 23 | 6 | 12 | 17 | 13 |
Because of rounding and missing data, not all categories sum to 100%.
14 of these 23 AEs were diagnosed at the final visit (3 among women in the Acidform-diaphragm arm, 1 in a woman in the HEC-diaphragm arm, 2 among women in the HEC-alone arm, and 3 among women in the Acidform-alone arm.
AF indicates Acidform; HEC, hydroxyethylcellulose (placebo gel).
For all groups, the highest number of AEs was reported at the first follow-up visit. Most AEs (79%) were genitourinary (including cervical or vaginal discharge, irritation, frequent urination, reports of burning sensations or “local heat,” pelvic pain, or inflammation). Nongenitourinary AEs (21%) included headache, asthma, fever, influenza, and other respiratory and digestive infections. Three-quarters of AEs (n = 97, 74%) were possibly, probably or definitely related to use of study products; of these, the 3 events that were definitely related to product use occurred in women in the Acidform-diaphragm arm (2 reports of temporary vaginal irritation and 1 report of pelvic pain). No serious AEs occurred.
No UTIs were detected during follow-up. A total of 3 pregnancies (1 in each of the Acidform-diaphragm, HEC-diaphragm, and HEC-alone arms) occurred. For the 1 pregnancy confirmed at the week 3 visit, product use was discontinued. The 2 other pregnancies were diagnosed at the last study visit, when products were removed from all participants.
Discussion
Our findings show that an intervention trial to assess the effectiveness of 2 woman-initiated methods of STI prevention will be both feasible and acceptable among high-risk women of low socioeconomic status whose main source of income is sex work. Women’s self-reported use of products during sex was high, and we saw no evidence of declining condom use (in fact, condom use increased between the first and final follow-up visits). Few women reported problems with their assigned products.
We enrolled 61% of screened women for this study, compared with 94% previously with this population using similar screening criteria.26 Recruitment took place during the Muslim holy month of Ramadan, when some women (particularly in Toamasina) in our target population abstained from sex and consequently failed to meet the inclusion criteria. Retention was very high.
Noncompliance with the recommended protocol was most pronounced among women in the 2 gel-only arms, in which gel use was coitally-dependent: only half inserted gel before each sex act, and one-third removed the gel after each sex act. We hypothesize that an underlying issue affecting compliant vaginal gel use, particularly among the group that reported removing the gel after each act, is that many women engage in extensive internal vaginal hygiene practices.48 Exploration of participants’ genital hygiene practices and ramifications for adherent study product use, in particular gel use, was a secondary aim of this pilot trial, and a separate analysis on this topic is forthcoming. Following this pilot study, we convened a workgroup including peer counselors, potential participants and clinicians to discuss new counseling strategies and modified vaginal hygiene practices that aim to optimize compliance with recommended protocols for product use for the RCT.
This pilot study was not powered to detect statistical differences between study groups for any outcome. However, we note that women in the 2 arms using active microbicide (with and without the diaphragm) had more self-reported gynecological symptoms and genitourinary AEs than women using placebo gel; women using the microbicide alone also had more clinician-noted abnormalities. Participants’ complaints (irritation, burning and itching) were similar to those described in previous safety studies of Acidform.38,39 As a result of these findings, we will replace Acid-form in the upcoming RCT with another candidate microbicide that has a similar acidifying mechanism of action, but with a superior safety profile. In addition, we will closely monitor safety related to product use among all participants. Sixty-four women will also be followed in an intensive safety substudy using colposcopy. This subset will be recruited for the coloscopy safety study at the start of the trial by inviting each newly enrolled participant to join, until 64 women have agreed to take part.
Two important findings from this formative work warrant additional attention. First, participants’ self-reported male condom use generally increased over the follow-up period. Free condom supplies and frequent counseling likely contributed to this increase, and it represents a positive health outcome. However, improved use of male condoms will likely also lower the expected STI incidence in the planned trial, potentially affecting power and precision. Lower-than-expected incidence, due in part to increased condom use, has been described in some HIV prevention studies.49,50 Second, self-reported weekly median number of sex partners and sex acts were higher during follow-up for every randomization group than had been reported at the baseline visit (although the enrollment questionnaire asked about the number of acts and partners in a typical week and follow-up questionnaires asked about the last week). Whether this finding represents true behavioral differences over time or simply reporting differences (for example, if participants intentionally underreported the number of partners or acts at enrollment because of social desirability concerns) is not known. Women completed a coital diary during follow-up; although diary data were not used for these analyses, perhaps making notes about their weekly behavior led to improved recall of sexual activity.
This study was designed to pilot-test several aspects of our proposed protocol to provide information about the best way to implement a large-scale RCT. It is limited by the small sample size and short follow-up time. In addition, a common limitation of research involving sexual behavior—assessing self-reported sensitive behavior through face-to-face interviews—exists in this study, making these data subject to misreporting because of recall and social desirability biases. Also, because of the low number of women reporting a primary partner, and the low sexual frequency with primary partners among participants who had them, we were unable to examine product use with primary partners and therefore limited our modeling analyses to reported behavior during sex with casual partners. Finally, because of the study product characteristics, complete masking of randomization assignment was not possible.
The recently published results of the MIRA trial showed no difference in HIV or STI risk between women assigned to use a diaphragm with a lubricant and male condoms, compared with women using condoms only.22,23 Of note, self-reported condom use was similar for both arms at baseline, but during follow-up, significantly more women in the diaphragm arm than in the control arm reported condom use during the last sex act.22 For the upcoming RCT, we are developing strategies to minimize possible product substitution by ensuring that participants understand the lack of evidence regarding the study products’ effectiveness.
In the MIRA trial, women were asked to insert the diaphragm before sex, whereas we instructed women to wear the diaphragm continuously. Throughout follow-up, 73% of the women in the MIRA diaphragm arm reported diaphragm use at last sex act. Noncoitally dependent diaphragm use could improve adherence. A second possible effect of continuous diaphragm use is that the device may remain in place longer after sex, providing more extended protection of vulnerable cervical tissue and possibly improving the effectiveness of the method against infection acquisition.
Unlike MIRA, our trial will evaluate the protective effect of the diaphragm plus candidate microbicide. Even if diaphragms alone do not provide protection against HIV, they may serve as effective vehicles for microbicide distribution,16 and our trial will answer this question with regard to STI outcomes.
Acknowledgments
Supported by the United States Centers for Disease Control and Prevention through an Inter-Agency Agreement with the United States Agency for International Development and CONRAD.
References
- 1.Mabey D, Mayaud P. Approaches to the control of sexually transmitted infections in developing countries: Old problems and modern challenges. Sex Transm Infect. 2004;80:174–182. doi: 10.1136/sti.2002.004101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Glasier A, Gulmezoglu AM, Schmid GP, et al. Sexual and reproductive health: A matter of life and death. Lancet. 2006;368:1595–1607. doi: 10.1016/S0140-6736(06)69478-6. [DOI] [PubMed] [Google Scholar]
- 3.Behets FM, Rasolofomanana JR, Van Damme K, et al. Evidence-based treatment guidelines for sexually transmitted infections developed with and for female sex workers. Trop Med Int Health. 2003;8:251–258. doi: 10.1046/j.1365-3156.2003.01017.x. [DOI] [PubMed] [Google Scholar]
- 4.Feldblum PJ, Hatzell T, Van Damme K, et al. Results of a randomised trial of male condom promotion among Madagascar sex workers. Sex Transm Infect. 2005;81:166–173. doi: 10.1136/sti.2004.010074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fleming DT, Wasserheit JN. From epidemiological synergy to public health policy and practice: The contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Infect. 1999;75:3–17. doi: 10.1136/sti.75.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cohen MS. Sexually transmitted diseases enhance HIV transmission: No longer a hypothesis. Lancet. 1998;351:5–7. doi: 10.1016/s0140-6736(98)90002-2. [DOI] [PubMed] [Google Scholar]
- 7.Corbett EL, Steketee RW, ter Kuile FO, et al. HIV-1/AIDS and the control of other infectious diseases in Africa. Lancet. 2002;359:2177–2187. doi: 10.1016/S0140-6736(02)09095-5. [DOI] [PubMed] [Google Scholar]
- 8.The Madagascar Action Plan 2007–2012. Available at: http://www.madagascar-presidency.gov.mg/MAP/?id=56&idy=23&lang=1.
- 9.Holmes KK, Levine R, Weaver M. Effectiveness of condoms in preventing sexually transmitted infections. Bull World Health Organ. 2004;82:454–461. [PMC free article] [PubMed] [Google Scholar]
- 10.D’Cruz OJ, Uckun FM. Clinical development of microbicides for the prevention of HIV infection. Curr Pharm Des. 2004;10:315–336. doi: 10.2174/1381612043386374. [DOI] [PubMed] [Google Scholar]
- 11.Stein ZA. HIV prevention: The need for methods women can use. Am J Public Health. 1990;80:460–462. doi: 10.2105/ajph.80.4.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maher JE, Harvey SM, Bird ST, et al. Acceptability of the vaginal diaphragm among current users. Perspect Sex Reprod Health. 2004;36:64–71. doi: 10.1363/psrh.36.64.04. [DOI] [PubMed] [Google Scholar]
- 13.Bird ST, Harvey SM, Maher JE, et al. Acceptability of an existing, female-controlled contraceptive method that could potentially protect against HIV: A comparison of diaphragm users and other method users. Womens Health Issues. 2004;14:85–93. doi: 10.1016/j.whi.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 14.Minnis AM, Padian NS. Effectiveness of female controlled barrier methods in preventing sexually transmitted infections and HIV: Current evidence and future research directions. Sex Transm Infect. 2005;81:193–200. doi: 10.1136/sti.2003.007153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moench TR, Chipato T, Padian NS. Preventing disease by protecting the cervix: The unexplored promise of internal vaginal barrier devices. AIDS. 2001;15:1–8. doi: 10.1097/00002030-200109070-00001. [DOI] [PubMed] [Google Scholar]
- 16.Rosenberg MJ, Davidson AJ, Chen JH, et al. Barrier contraceptives and sexually transmitted diseases in women: A comparison of female-dependent methods and condoms. Am J Public Health. 1992;82:669–674. doi: 10.2105/ajph.82.5.669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Austin H, Louv WC, Alexander WJ. A case-control study of spermicides and gonorrhea. JAMA. 1984;251:2822–2824. [PubMed] [Google Scholar]
- 18.Magder LS, Harrison HR, Ehret JM, et al. Factors related to genital Chlamydia trachomatis and its diagnosis by culture in a sexually transmitted disease clinic. Am J Epidemiol. 1988;128:298–308. doi: 10.1093/oxfordjournals.aje.a114970. [DOI] [PubMed] [Google Scholar]
- 19.Becker TM, Wheeler CM, McGough NS, et al. Contraceptive and reproductive risks for cervical dysplasia in southwestern Hispanic and non-Hispanic white women. Int J Epidemiol. 1994;23:913–922. doi: 10.1093/ije/23.5.913. [DOI] [PubMed] [Google Scholar]
- 20.Wolner-Hanssen P, Eschenbach DA, Paavonen J, et al. Decreased risk of symptomatic chlamydial pelvic inflammatory disease associated with oral contraceptive use. JAMA. 1990;263:54–59. doi: 10.1001/jama.1990.03440010052029. [DOI] [PubMed] [Google Scholar]
- 21.Kelaghan J, Rubin GL, Ory HW, et al. Barrier-method contraceptives and pelvic inflammatory disease. JAMA. 1982;248:184–187. [PubMed] [Google Scholar]
- 22.Padian NS, van der Straten A, Ramjee G, et al. Diaphragm and lubricant gel for prevention of HIV acquisition in southern African women: A randomised controlled trial. Lancet. 2007;370:251–261. doi: 10.1016/S0140-6736(07)60950-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.De Bruyn G, Shiboski S, Ramjee G, et al. The diaphragm and lubricant gel for prevention of cervical sexually transmitted infections: Results of a randomized controlled trial. Abstract O-5, International Society for Sexually Transmitted Disease Research (ISSTDR) Annual Meeting; July 29-August 1, 2007; Seattle. [Google Scholar]
- 24.McGowan I. Microbicides: A new frontier in HIV prevention. Biologicals. 2006;34:241–255. doi: 10.1016/j.biologicals.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 25.Luchters S, Chersich MF, Jao I, et al. Acceptability of the diaphragm in Mombasa Kenya: A 6-month prospective study. Eur J Contracept Reprod Health Care. 2007;12:345–353. doi: 10.1080/13625180701516989. [DOI] [PubMed] [Google Scholar]
- 26.Behets F, Norris Turner A, Van Damme K, et al. Acceptability and feasibility of continuous diaphragm use among sex workers in Madagascar. Sex Trans Inf. 2005;81:472–476. doi: 10.1136/sti.2005.015107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van der Straten A, Kang MS, Posner SF, et al. Predictors of diaphragm use as a potential sexually transmitted disease/HIV prevention method in Zimbabwe. Sex Transm Dis. 2005;32:64–71. doi: 10.1097/01.olq.0000148301.90343.3a. [DOI] [PubMed] [Google Scholar]
- 28.Coggins C, Blanchard K, Alvarez F, et al. Preliminary safety and acceptability of a Carrageenan gel for possible use as a vaginal microbicide. Sex Transm Infect. 2000;76:480–483. doi: 10.1136/sti.76.6.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mauck CK, Weiner DH, Ballagh SA, et al. Single and multiple exposure tolerance study of polystyrene sulfonate gel: A phase I safety and colposcopy study. Contraception. 2004;70:77–83. doi: 10.1016/j.contraception.2004.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mantell JE, Myer L, Carballo-Dieguez A, et al. Microbicide acceptability research: Current approaches and future directions. Soc Sci Med. 2005;60:319–330. doi: 10.1016/j.socscimed.2004.05.011. [DOI] [PubMed] [Google Scholar]
- 31.Moon MW, Khumalo-Sakutukwa GN, Heiman JE, et al. Vaginal microbicides for HIV/STI prevention in Zimbabwe: What key informants say. J Transcult Nurs. 2002;13:19–23. doi: 10.1177/104365960201300104. [DOI] [PubMed] [Google Scholar]
- 32.Garg S, Anderson R, Chany C, et al. Properties of a new acid-buffering bioadhesive vaginal formulation (Acidform) Contraception. 2001;64:67–75. doi: 10.1016/s0010-7824(01)00217-7. [DOI] [PubMed] [Google Scholar]
- 33.AcidForm Investigator’s Brochure, 2005.
- 34.Tuyama AC, Cheshenko N, Carlucci MJ, et al. ACIDFORM inactivates herpes simplex virus and prevents genital herpes in a mouse model: Optimal candidate for microbicide combinations. J Infect Dis. 2006;194:795–803. doi: 10.1086/506948. [DOI] [PubMed] [Google Scholar]
- 35.Spencer SE, Valentin-Bon IE, Whaley K, et al. Inhibition of Neisseria gonorrhoeae genital tract infection by leading-candidate topical microbicides in a mouse model. J Infect Dis. 2004;189:410–419. doi: 10.1086/381125. [DOI] [PubMed] [Google Scholar]
- 36.Tabet SR, Callahan MM, Mauck CK, et al. Safety and acceptability of penile application of 2 candidate topical microbicides: BufferGel and PRO 2000 Gel: 3 randomized trials in healthy low-risk men and HIV-positive men. J Acquir Immun Defic Syndr. 2003;33:476–483. doi: 10.1097/00126334-200308010-00008. [DOI] [PubMed] [Google Scholar]
- 37.Schwartz JL, Poindexter A, Schmitz SW, et al. Male tolerance of ACIDFORM gel. Contraception. 2005;71:443–446. doi: 10.1016/j.contraception.2004.11.008. [DOI] [PubMed] [Google Scholar]
- 38.Amaral E, Perdigao A, Souza MH, et al. Vaginal safety after use of a bioadhesive, acid-buffering, microbicidal contraceptive gel (ACIDFORM) and a 2% nonoxynol-9 product. Contraception. 2006;73:542–547. doi: 10.1016/j.contraception.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 39.Amaral E, Faundes A, Zaneveld L, et al. Study of the vaginal tolerance to acidform, an acid-buffering, bioadhesive gel. Contraception. 1999;60:361–366. doi: 10.1016/s0010-7824(99)00102-x. [DOI] [PubMed] [Google Scholar]
- 40.Williams DL, Creinin MD, Barnhart K, et al. Safety Analysis of the diaphragm in combination with vaginal microbicide gels (ACIDFORM and BufferGel): Results of a 14 Day Trial. Abstract # OB21, Microbicides 2006; Cape Town, South Africa. April 24-26, 2006. [Google Scholar]
- 41.Schwartz J, Lai J, Creinin M, et al. Fourteen day safety and acceptability study of ACIDFORM Gel: A randomized phase I safety study. Abstract # OB4, Microbicides 2006; Cape Town, South Africa. April 24-26, 2006. [Google Scholar]
- 42.Williams DL, Newman DR, Ballagh SA, et al. Phase I safety trial of two vaginal microbicide gels (Acidform or BufferGel) used with a diaphragm compared to KY jelly used with a diaphragm. Sex Transm Dis. 2007;34:977–984. doi: 10.1097/olq.0b013e31813347e9. [DOI] [PubMed] [Google Scholar]
- 43.Trifonova RT, Pasicznyk JM, Fichorova RN. Biocompatibility of solid-dosage forms of anti-HIV-1 microbicides with the human cervico-vaginal mucosa modeled ex vivo. Antimicrob Agents Chemother. 2006;50:4005–4010. doi: 10.1128/AAC.00588-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tien D, Schnaare RL, Kang F, et al. In vitro and in vivo characterization of a potential universal placebo designed for use in vaginal microbicide clinical trials. AIDS Res Hum Retroviruses. 2005;21:845–853. doi: 10.1089/aid.2005.21.845. [DOI] [PubMed] [Google Scholar]
- 45.Schwartz J, Ballagh S, Kwok C, et al. Fourteen-day safety and acceptability study of the HEC-based universal placebo gel. Abstract # PB68 Microbicides 2006; Cape Town, South Africa. April 24-26, 2006. [Google Scholar]
- 46.Pettifor AE, Turner AN, Van Damme K, et al. Increased risk of chlamydial and gonococcal infection in adolescent sex workers in Madagascar. Sex Transm Dis. 2007;34:475–478. doi: 10.1097/01.olq.0000251239.85295.81. [DOI] [PubMed] [Google Scholar]
- 47.Lachin JM. Statistical considerations in the intent-to-treat principle. Control Clin Trials. 2000;21:167–89. doi: 10.1016/s0197-2456(00)00046-5. [DOI] [PubMed] [Google Scholar]
- 48.Legardy-Williams J, Bell A, Jamieson D, et al. Attitudes and beliefs about vaginal cleansing among women, men, and healthcare providers in Antananarivo, Madagascar. Abstract # OC19, Microbicides 2006; Cape Town, South Africa. April 24-26, 2006. [Google Scholar]
- 49.Family Health International press release. Phase 3 Trial in Nigeria Evaluating the Effectiveness of SAVVY Gel in Preventing HIV Infection in Women Will Close. 2006 Aug 28; Available at: http://www.fhi.org/en/AboutFHI/Media/Releases/Phase3SAVVY082806.htm. Accessed December 4, 2007.
- 50.Kaul R, Kimani J, Nagelkerke NJ, et al. Reduced HIV risk-taking and low HIV incidence after enrollment and risk-reduction counseling in a sexually transmitted disease prevention trial in Nairobi, Kenya. J Acquir Immune Defic Syndr. 2002;30:69–72. doi: 10.1097/00042560-200205010-00009. [DOI] [PubMed] [Google Scholar]


