Abstract
Objective
To examine the prevalence of overweight and obesity in firefighters.
Methods
Body mass index (BMI), waist circumference, and body fat percentage (BF%) were assessed in 478 career and 199 volunteer male firefighters from randomly selected departments.
Results
High prevalence rates of overweight + obesity (BMI ≥ 25 kg/m2) and obesity (BMI ≥ 30 kg/m2) were found in career (79.5%; 33.5%) and volunteer firefighters (78.4%; 43.2%). False-positive obesity misclassification based on BMI, compared to waist circumference and BF%, was low (9.8% and 2.9%, respectively). False negatives were much higher: 32.9% and 13.0%. Obese firefighters demonstrated unfavorable cardiovascular disease (CVD) profiles.
Conclusions
The prevalence of overweight and obesity exceeded that of the US general population. Contrary to common wisdom, obesity was even more prevalent when assessed by BF% than by BMI, and misclassifying muscular firefighters as obese by using BMI occurred infrequently.
Our nation depends on the fire service to respond to major emergencies. Firefighters and emergency medical services personnel are a crucial part of the public health safety net and represent more than two million individuals nationally.1,2 Other occupational groups, such as the military, have received considerable attention from the public health research community on issues related to health and fitness. Conversely, the substantial health and fitness issues faced by the fire service have, in large part, not been adequately addressed.
There is a wide agreement that firefighters should maintain high levels of physical fitness, including aerobic capacity, flexibility, muscular endurance, strength, and power.3 There is no agreed-upon standard for firefighter fitness; however, it has been suggested that firefighting activities require up to 12.0 metabolic equivalents (METs) of aerobic capacity and that this could be considered the minimum level of fitness necessary to safely perform required activities.4 It also corresponds to the suggested minimal level necessary to perform firefighting tasks after the diagnosis of coronary artery disease.5 Experts have placed such a high value on fitness in the fire service that guidance from the Fire Service Joint Labor Management Wellness Fitness Initiative3 recommends 60 to 90 minutes be allocated for firefighters’ exercise on every work shift. Unfortunately, there is troubling evidence from previous studies, largely based on convenience samples from individual fire departments or regions, that firefighters struggle with overweight and obesity and low levels of physical fitness.
Several studies found that the prevalence of overweight and obesity combined (body mass index [BMI] ≥ 25) is very high in the career fire service, ranging from 73% to 88%. 4,6–10 Similar prevalence estimates (76% to 87%) have been documented for volunteer firefighters.11,12 These studies suggest that the prevalence of overweight and obesity among firefighters is actually greater than that found for the general US population.13 Nevertheless, because none of the previously mentioned studies are population-based and provide only crude, unadjusted rates, it is not clear how representative they are of the entire US fire service.
Comorbidities related to obesity also appear to be highly prevalent among firefighters. Donovan et al4 found that 15% of the firefighters in their sample met the National Cholesterol Education Program (NCEP) criteria for metabolic syndrome. Soteriades et al9,14 prospectively evaluated cardiovascular disease (CVD) and disability risk in a cohort of hazardous materials firefighters in Massachusetts and found that the prevalence of obesity (BMI ≥ 30) increased from 33.7% to 40.4% over the 5-year period of observation.14 In addition, they found that obesity was a significant risk factor for subsequent disability, with each one-unit increase in BMI associated with a 5% increase in risk of job disability. Those with class 1 obesity or classes 2 and 3 obesity combined had 17% and 56% greater risk for disability when compared with normal-weight firefighters.9 Evidence also suggests that firefighters with high BMIs have impaired vascular function and greater risk for CVD.7,14,15 Cardiovascular disease remains the leading cause of firefighter line-of-duty death (LODD, ie, fatalities on the job),16 accounting for about 45% of all on-duty firefighter deaths since at least the late 1970s. This proportionate on-duty mortality is substantially higher than that reported for police (22%), other emergency medical service providers (11%), and on-the-job deaths for all occupations (15%).16,17
The epidemic of overweight and obesity among firefighters is critical because, in addition to greater risk for morbidity and mortality, excess body fat is correlated with low fitness. For example, overweight and obese adolescents and adults experienced between 2 and 3 times greater risk for low fitness when compared with their normal-weight counterparts.18 Tsismenakis et al10 found that no lean firefighter recruits failed to achieve 12.0 METs, while 7% and 42% of overweight and obese recruits failed, respectively. Donovan et al4 found that 25% of firefighters studied did not meet a 12.0 METs minimal exercise tolerance threshold. Moreover, physical fitness is associated with better performance on job-related and simulated firefighting tasks.19–21 For example, Elsner and Kolkhorst19 found a strong, inverse relationship (r = −0.725) between cardiorespiratory fitness and performance time on simulated firefighting tasks, with more-fit firefighters completing tasks (eg, hose and ladder carry, donning self-contained breathing apparatus,, climbing three flights of stairs, and rescue and body drag) faster than those who were less fit.
Because of the growing evidence of low fitness, unfavorable body composition, and a disproportionate number of LODD due to CVD, there is a critical need for large, well-designed epidemiological studies that better characterize rates of overweight and obesity and general fitness levels of firefighters and examine important correlates and risks for overweight and obesity. The purpose of this study is to examine both crude and adjusted rates of overweight and obesity by using several objective methods of determining excess adiposity. This is significant because concerns have been raised about the potential problem of BMI-based obesity overestimating risk in athletic and/or active populations.22 For example, some firefighter health Web sites suggest that the BMI is inaccurate for determining body composition and cite a study that found the correlation between BMI and body fat percentage (BF%) to be very low, but the sample was 109 male bodybuilders.23 Our study is the first to use multiple measures of body composition/adiposity to address this concern. In addition, we also examined the prevalence of low fitness and relationships between weight status, fitness, and CVD risk factors in the first epidemiological study of firefighter health by using systematic random sampling and a population-based design.
METHODS
Participating Fire Departments
The data reported are from the baseline evaluation of an ongoing longitudinal cohort study examining risk factors for injury in both career and volunteer firefighters (“A prospective evaluation of health behavior risk for injury among firefighters” EMW-2007-FP-02571) in the International Association of Fire Chief’s (IAFC) Missouri Valley region (Colorado, Iowa, Kansas, Missouri, North Dakota, Nebraska, South Dakota, and Wyoming).
Fire departments in the IAFC Missouri Valley region were randomly selected by using a one-stage, randomized, cluster-sampling approach, stratified by department type (volunteer/mostly volunteer vs career/mostly career). Departments were drawn from the US Fire Administration’s Fire Department Census Database24 for each of the eight Missouri Valley states by using a computerized random selection program. One additional volunteer department that was involved in piloting our measures was also included, even though it was not randomly selected. Participating career departments ranged in size from 1 to 18 stations, with a mix of settings ranging from urban inner city, suburban, and rural. Volunteer departments were primarily in small to medium rural towns and cities and ranged from 1 to 3 stations.
Procedures
The protocol for the protection of human subjects for this study was approved by the National Development and Research Institute institutional review board. Among career departments, a total of 14 career departments were contacted, with two declining participation because of competing priorities and one department not meeting inclusion criteria of at least 20 personnel.
On the basis of the logistics and staffing patterns of volunteer departments, contacting a department’s administration was more difficult. Therefore, for each department selected, phone calls were made to the listed department number in the US Fire Administration’s Fire Department Census Database, as well as any number located through extensive internet searches. Phone calls were made during the day, in the evening, and on a weekend day. If an address was provided, a letter also was sent to the station to the attention of the chief, with a brief description of the study and a request for them to contact the research team. If no response was received within 2 weeks of attempted contact, a replacement department was selected. In addition to the challenges of contacting the volunteer personnel, the database did not always have current census numbers and, therefore, some departments were ruled out because of low numbers of volunteer personnel. A total of 47 volunteer departments contacted, and of the 47 volunteer departments, 13 were enrolled (17 were unreachable, 8 did not meet the inclusion criteria of having at least 20 personnel, and 9 declined participation).
Eleven career and 13 volunteer departments were enrolled and contributed data to this study. A core team of investigators traveled to each fire department for 2 to 5 days, depending on the type of department (career vs volunteer) and shift structure of career departments, thus maximizing the potential to recruit study participants from all available firefighters. To solicit participation from firefighters in selected departments, each data collection session included refreshments and/or participant incentives such as study T-shirts. Firefighters who agreed to participate in the study were provided an overview of the study, its specific aims, and the risks and benefits involved in study participation. Of the firefighters solicited, 97% agreed to participate in the research and were consented. They were then provided with a survey to complete and moved through different assessment stations involving the measures described later.
Measures
Body composition—weight, BMI, BF%, and waist circumference
Height was assessed by using a portable stadiometer. Body weight and BF% were determined by using foot-to-foot bioelectrical impedance (ie, the Tanita 300, Tanita Corporation of America, Inc., Arlington Heights, Illinois). The Tanita 300 demonstrated strong evidence of concurrent validity (r = 0.94; P < 0.001)25 when compared with the “criterion standard” of dual energy x-ray absorptiometry for body fat assessment. The Tanita 300 is a commonly used bioelectrical impedance field measure because of its portability and accuracy in determining BF%. Waist circumference (WC) was determined by using a spring-loaded nonstretchable tape measure in accordance with recommendations by US Government obesity guidelines.22,26 The BMI (kg/m2) and obesity categories for BMI, BF%, and WC also were computed by using these standards.22,26
CVD risk factors—blood pressure and pulse and cholesterol
Blood pressure was assessed by using the Omron HEM-711AC (Omron Healthcare, Inc., Bannockburn, Illinois) in accordance with the Hypertension Detection and Follow-Up Program following the standard epidemiological protocol.27 The first blood pressure reading was omitted and the last two averaged to obtain each subject’s blood pressure. Eight-hour fasting lipids (total cholesterol, high-density lipoproteins (HDL), low-density lipoproteins, and triglycerides) were determined by using the CardioCheck R Analyzer (Polymer Technology Systems, Inc, Indianapolis, IN), which met evaluative criteria required by Cholesterol Reference Method Laboratory Network.
Self-Report of Physical Activity questionnaire and estimated maximal oxygen consumption
The Self-Report of Physical Activity (SRPA) questionnaire provides a global, self-rating of physical activity patterns. Indicators of the questionnaire’s validity in adult populations (significant correlation between SRPA ratings and measured maximal oxygen consumption [VO2max]) have been established.28 Participants were instructed to select a value from the questionnaire that best described their physical activity pattern during the past 30 days.29 These values, along with BMI, age, and gender were used to estimate VO2max. This method has been tested by comparing it with measured VO2max and has demonstrated equal, if not better, accuracy as methods using submaximal exercise heart rate to estimate aerobic capacity,28–33 making it an ideal field measure.
Strength and flexibility
The Jackson Strength Evaluation System, which is commonly used for the lift tasks of the National Institute of Occupational Safety and Health, was used to assess isometric strength. The system comes with standardized measures of strength and is recommended by National Fire Protection Association (NFPA) 1500 for firefighters.34 The adjustable sit-and-reach flexibility tester was used to assess flexibility and also was recommended by NFPA 1500.34
International Physical Activity Questionnaire
The International Physical Activity Questionnaire queries participants about the number of days during the past week they engaged in moderate and vigorous physical activity and how much time per week they spent sitting and watching television. This International Physical Activity Questionnaire has been shown to be a reliable (Spearman P = 0.8) and valid (Spearman P = 0.33) instrument for obtaining detailed assessments of physical activity in 18- to 65-year-old men and women.35,36
Statistical Analyses
Sample size determination
On the basis of randomly selected 12 volunteer and 11 career departments among a total of 1985 and 273 departments, respectively, in a one-stage cluster sampling design, we estimated the margin of error for prevalence estimates of ±3% for volunteer departments and ±0.9% for career departments, thus having sufficient sample sizes to produce highly reliable estimates of population health parameters.
Analytic approach
Because of the small number of female firefighters in this study (career, n = 21; volunteer, n = 15) and the resulting inability to examine the potential moderating impact of gender, only male firefighters were included in the study and statistical models. Crude (unstandardized) prevalence rates of overweight and obesity combined (BMI ≥ 25 kg/m2), obesity only (BMI ≥ 30 kg/m2) by using BMI, and obesity based on BF% (BF% > 25% for men) and WC (WC > 40 in or 102 cm for men) were computed according to National Institutes of Health standards.13,22,26 In addition, specific classes of obesity based on BMI, that is, class 1 obesity (BMI ≥ 30 kg/m2 but <35 kg/m2) and classes 2 and 3 obesity (BMI ≥ 35 kg/m2) were also derived using National Institutes of Health standards.13,22,26
Metabolic syndrome criteria for elevated systolic and diastolic blood pressure, low HDL, and elevated triglycerides were computed using the NCEP cut points.37 Unadjusted characteristics of career and volunteer firefighters based on these three methods of defining obesity were computed (means [SD] or percentage). Aerobic capacity sufficient to exceed the NFPA minimum postcardiac event exercise tolerance threshold was evaluated by comparing the estimated VO2max with the suggested cut point of ≥12 METs (VO2max ≥ 42 mL/kg/min).4,5,10 Estimated VO2max levels were converted to METs by using the standard conversion of dividing VO2max by 3.5 mL/kg/min.
Age-standardized prevalence rates of overweight and obesity combined and obesity were computed to facilitate comparison with national estimates.13 2008 US census population estimates38 were used for the standard population, and StatsDirect Statistical Software version 2.3.8 (StatsDirect Ltd, 2004, Cheshire, UK) was used to compute the age-standardized rates. Crude rates of overweight and obesity and obesity were age-standardized using the direct method of standardization.39 The accuracy of the BMI-based standard for categorizing individuals as obese (ie, BMI ≥ 30 kg/m2) was compared with BF% (BF% > 25% for men) and WC (WC > 40 in or 102 cm for men) standards. Rates of overall accuracy, false positives, and false negatives were computed using standard methods.39 We also conducted analyses adjusted for highly athletic individuals, for example, those engaging in greater than or equal to 10 hours per week of vigorous activity or having a resting heart rate of 60 beats per minute or less.
To explore associations between important indicators of health and fitness and the weight status of firefighters, statistical models were developed, in which normal-weight firefighters were compared either with class 1 (BMI ≥ 30 kg/m2 but <35 kg/m2) or classes 2 and 3 obese (BMI ≥ 35 kg/m2) firefighters. Each model was created within the SAS PROC GLIMMIX (SAS 9.2, SAS Institute Inc., Cary, North Carolina) module and was adjusted for age. Department also was included as a random effect in each model to adjust for the sampling approach used in this study.
RESULTS
A total of 677 career and volunteer male firefighters were enrolled into the cohort and completed a baseline health evaluation. Demographic and health characteristics of enrolled firefighters are presented in Table 1.
TABLE 1.
Baseline Demographic and Clinical Characteristics (M [SD] or %) of Male Career and Volunteer Firefighters in the Firefighter Injury and Risk Evaluation Study
| Demographics | Career (n = 478) |
Volunteer (n = 199) |
|---|---|---|
| Age, yrs | 38.2 (9.9) | 39.7 (12.0) |
| Gender (% male) | 100 | 100 |
| Race (% white) | 86.4 | 97.5 |
| Marital status (% married or living with partner) | 72.6 | 75.4 |
| Education (% at least some college or college graduate) | 82.4 | 61.8 |
| Years in the fire service | 14.0 (9.1) | 11.1 (10.2) |
| Rank (%) | ||
| Firefighter | 31.8 | 60.3 |
| Firefighter/paramedic | 16.9 | 4.5 |
| Driver/operator | 18.8 | 9.0 |
| Officer | 21.8 | 10.6 |
| Chief | 6.5 | 10.1 |
| Other | 0.6 | 4.5 |
| Health status variables | ||
| Weight (kg; lb) 91.3 | (15.6); 200.9 (34.2) | 94.8 (18.2); 208.6 (40.0) |
| Height (cm; in) | 178.3 (6.3); 70.2 (2.5) | 178.8 (6.8); 70.4 (2.7) |
| BMI (kg/m2) | 28.6 (4.6) | 29.5 (5.3) |
| WC (in) | 38.3 (4.8) | 40.2 (5.3) |
| Body fat (%) | 25.3 (6.6) | 26.2 (7.7) |
| SBP (mmHg) | 124.0 (12.5) | 130.6 (13.7) |
| DBP (mmHg) | 78.5 (10.2) | 81.0 (11.3) |
| Total cholesterol (mg/dL) | 155.8 (39.2) | 160.3 (41.6) |
| HDL (mg/dL) | 38.6 (12.7) | 36.9 (11.5) |
| LDL (mg/dL) | 97.6 (35.8) | 102.0 (34.4) |
| Triglycerides (mg/dL) | 119.4 (76.6) | 132.9 (86.5) |
| Self-Reported Medication Use (% yes) | ||
| Type 1 diabetes | 0.4 | 0.5 |
| Type 2 diabetes | 1.7 | 3.5 |
| Hypertension | 9.2 | 15.6 |
| High cholesterol | 9.8 | 10.6 |
| Cardiovascular disease | 0.6 | 2.0 |
| Sleep apnea | 1.0 | 0.0 |
BMI, body mass index; DBP, diastolic blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein; SBP, systolic blood pressure; WC, waist circumference.
Career and volunteer firefighters in this study were predominantly white and had completed at least some college and, on average, had more than one decade of service. Their weight status and CVD risk factors also are provided in Table 1. It is notable that for both groups, the average BMI was greater than 28.0 kg/m2 and average BF% for male career and volunteer firefighters exceeded 25%, which is the current definition of obesity for men based on BF%.22,26 They also demonstrated fairly low HDL levels, but other mean values for CVD risk factors were in the reference range on average.
Figure 1A presents the crude (unstandardized) prevalence of overweight and obesity combined and obesity only by using current BMI, WC, and BF% standards.22,26 Figure 1B provides age-standardized estimates based on 2008 US census population estimates40 and the current prevalence for US adults.13
FIGURE 1.
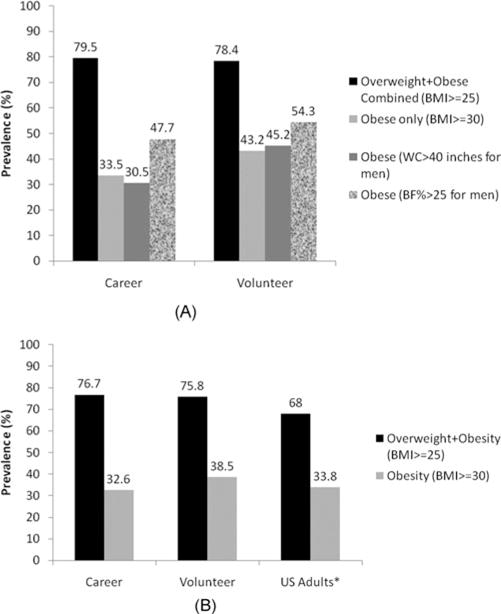
(A) Unstandardized prevalence of overweight and obese combined (BMI ≥ 25) and obese only (BMI ≥ 30; WC >40 inches; and BF% > 25) in male career and volunteer firefighters. (B) Age-standardized prevalence of overweight and obese combined (BMI ≥ 25) and obese only (BMI ≥30) in male career and volunteer firefighters compared to US Adults∗.
High rates of overweight and obesity combined (BMI ≥ 25 kg/m2) were demonstrated in both career and volunteer firefighters, with more than 75% of both samples having a BMI that exceeded 25 kg/m2. Rates of obesity also were high regardless of how obesity was defined (ie, using BMI-, WC-, or BF%-based definitions), and both groups had the highest estimates when using the BF% definition of obesity.
Both career and volunteer firefighters age-standardized rates of overweight and obesity (BMI ≥ 25 kg/m2) exceeded current US prevalence, and the age-standardized rates of obesity were similar to the US sample (Fig. 1B). Because firefighting is thought to be a physically active profession, some concerns have been raised about relying solely on BMI as method for estimating body composition, suggesting that many firefighters might have elevated BMIs but have low body fat and WC. Figure 2 illustrates the relationship between the three methods of defining obesity to examine rates of misclassification, false positives (ie,, individuals with high BMI but with WC or BF% below cutoffs for obesity), and false negatives (ie,, individuals with normal BMI but with WC or BF% exceeding the cut point for obesity) among career firefighters alone.
FIGURE 2.
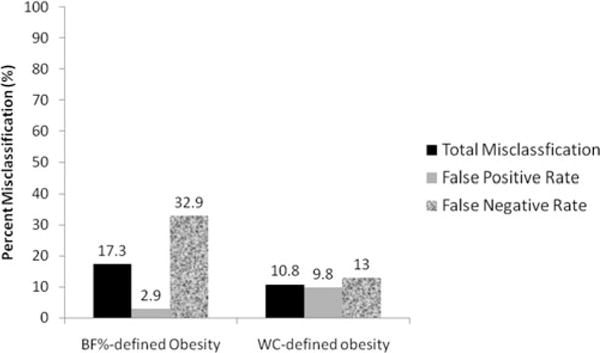
Accuracy of BMI classification of obesity compared to BF% and WC among male career firefighters only.
This analysis was restricted to career firefighters because they were most likely to present the concern about overestimation of obesity based on BMI and because of their activity levels on the job. When comparing BMI-defined obesity with obesity defined using BF% or WC, the overall rates of misclassification were modest to low; in particular, the likelihood that a career firefighter would have a BMI in the obese range but BF% or WC in the nonobese ranges was very low (2.9% and 9.8%, respectively). It was much more likely that a career firefighter who was obese by the BF% or WC standard would be classified as not obese by using BMI; that is, 32.9% and 13.0% of firefighters met the BF% or WC standard for obesity but were in the nonobese range on BMI. There were no significant differences in either the proportion of individuals classified as obese using BF% as the standard or the rates of misclassification, false positives, or false negatives when analyses were adjusted to account for high levels of vigorous activity and use of the athletic setting on the Bioelectrical Impedance scale.
Unadjusted body composition and CVD risk differences by obesity status were evaluated using the three different methods for defining obesity in career and volunteer firefighters (Table 2).
TABLE 2.
Unadjusted Health Parameters of Male Career and Volunteer Firefighters Stratified by Obesity Status (BMI ≥ 30) (M [SD] or %)
| BMI-Defined Obesity | Department Type
|
|||
|---|---|---|---|---|
| Career
|
Volunteer
|
|||
| Yes (33.5%) | No (66.5%) | Yes (43.2%) | No (56.8%) | |
| Demographics | ||||
| Age, yrs | 41.5 (9.2) | 36.6 (9.8) | 41.6 (9.9) | 38.9 (13.5) |
| Race (% white) | 89.7 | 88.3 | 96.5 | 98.2 |
| Years in the fire service | 16.2 (8.8) | 12.9 (9.0) | 12.7 (10.1) | 10.8 (10.4) |
| Body composition | ||||
| Weight (kg; lb) | 107.3 (12.7) | 83.1 (9.2) | 111.0 (13.5) | 82.3 (9.1) |
| 236.2 (28.0) | 182.9 (20.2) | 244.2 (29.7) | 181.0 (20.1) | |
| BMI (kg/m2) | 33.7 (3.6) | 26.1 (2.3) | 34.4 (3.6) | 25.7 (2.6) |
| WC (in) | 43.1 (3.9) | 35.8 (3.0) | 44.8 (3.7) | 36.6 (3.1) |
| Body fat (%) | 32.0 (4.6) | 21.9 (4.6) | 32.8 (5.0) | 21.0 (5.1) |
| Cardiovascular risk factors | ||||
| SBP (mmHg) | 128.4 (13.2) | 121.7 (11.5) | 135.3 (14.0) | 127.0 (12.4) |
| DBP (mmHg) | 83.5 (10.3) | 76.0 (9.2) | 86.1 (11.7) | 77.1 (9.3) |
| Total cholesterol (mg/dL) | 166.7 (43.2) | 149.9 (35.6) | 165.6 (47.3) | 156.7 (36.9) |
| HDL (mg/dL) | 36.4 (13.7) | 39.7 (12.0) | 33.2 (10.3) | 39.6 (11.3) |
| LDL (mg/dL) | 108.1 (40.7) | 91.9 (31.6) | 105.1 (41.1) | 99.6 (28.3) |
| Triglyceride (mg/dL) | 141.6 (83.6) | 107.4 (69.9) | 162.3 (95.5) | 112.3 (73.5) |
| NCEP metabolic syndrome criteria | ||||
| SBP ≥ 130 mmHg | 39.6 | 21.9 | 67.4 | 39.8 |
| DBP ≥ 85 mmHg | 40.9 | 15.8 | 53.5 | 19.5 |
| HTN or medications | 4.4 | 1.6 | 12.8 | 1.8 |
| Triglyceride ≥ 150 mg/dL | 32.8 | 20.2 | 30.2 | 17.7 |
| Low HDL (<40 mg/dL in men; <50 mg/dL in women) | 66.4 | 56.3 | 80.3 | 62.1 |
| Fitness | ||||
| VO2 max (mL/kg/min) | 33.5 (6.1) | 41.4 (6.5) | 30.8 (7.5) | 38.9 (9.0) |
| METs | 9.5 (2.0) | 12.1 (2.1) | 8.8 (2.1) | 11.1 (2.6) |
| IPAQ weekly vigorous energy expenditure (vigorous MET-mins/week)* | 1931.8 (1795.3) | 2381.6 (1750.8) | 4160.5 (5124.3) | 3634.4 (4868.8) |
| IPAQ weekly total energy expenditure (total MET-mins/week)† | 4720.4 (3639.2) | 5472.4 (3776.0) | 9310.8 (8486.7) | 10885.6 (9584.4) |
| Maximum torso strength (lb) | 328.2 (57.6) | 317.0 (52.9) | 338.8 (54.5) | 311.8 (55.8) |
| Flexibility (in) | 12.8 (2.9) | 13.5(3.0) | 12.9 (3.0) | 13.8 (3.0) |
BMI, body mass index; DBP, diastolic blood pressure; HDL, high-density lipoprotein; HTN, hypertension; IPAQ, International Physical Activity Questionnaire; MET, metabolic equivalent; NCEP, National Cholesterol Education Program; LDL, low-density lipoprotein; SBP, systolic blood pressure; VO2, maximal oxygen consumption; WC, waist circumference.
Vigorous activity level; MET-min/wk = 8.0 × vigorous-intensity activity minutes × vigorous-intensity days.
Total physical activity MET-min/wk can be computed as the sum of walking + moderate + vigorous MET-min/wk scores.
All three methods demonstrated that obese firefighters were more likely to exhibit adverse metabolic profiles and substantially lower fitness and physical activity levels than their nonobese counterparts. Figure 3 illustrates the prevalence of low fitness (ie,, those who did not meet a minimal exercise tolerance standard of 12.0 METs,4,5,10 even though workload demands of firefighters had been shown to exceed these levels) by obesity status, using all three body composition standards (ie,, BMI> 30 kg/m2; BF% > 25% for men, and WC > 40 in or 102 cm for men) in both career and volunteer obese firefighters. It should be noted that the overall proportions of career (38.7%) and volunteer (23.6%) firefighters who met or exceeded a minimal criterion of 12.0 METs, regardless of weight status, were quite low.
FIGURE 3.
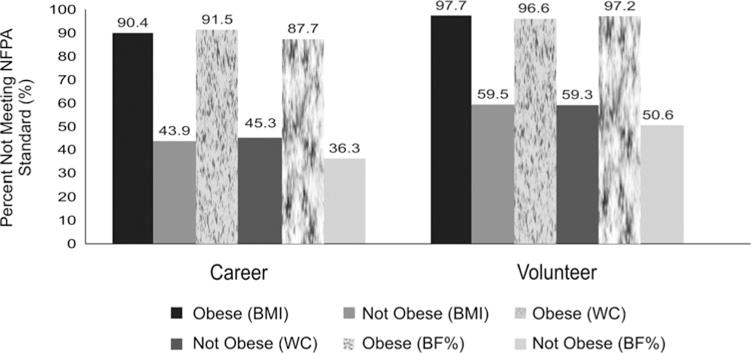
Unadjusted prevalence of low fitness levels using the NFPA 1582 suggested minimal post-cardiac event exercise tolerance threshold among male career and volunteer firefighters by weight status.
Finally, age-adjusted univariate associations between obesity, significant unadjusted CVD-risk parameters (note: we only examined one risk factor for those who overlapped, such as systolic blood pressure and whether or not they met the NCEP systolic blood pressure elevation criterion), and the NFPA postcardiac event exercise tolerance criterion4,5,10 were computed by comparing normal-weight firefighters with firefighters with class 1 obesity. The same associations were examined comparing normal-weight firefighters with those meeting the criterion for classes 2 and 3 obesity combined (Table 3). All models also were adjusted for the department as the unit of selection and odds ratios (ORs) are presented.
TABLE 3.
Health Outcomes for Male Normal Weight Versus Class 1 Obese Firefighters and for Normal Weight Versus Classes 2 and 3 Obese Firefighters*
| Normal Weight vs Class 1 Obese Male Firefighters
|
Volunteer Firefighters, N = 95 (n = 54 Class 1 Obesity vs n = 41 Normal Weight) | Normal Weight vs classes 2 and 3 Obese Male Firefighters
|
||||||
|---|---|---|---|---|---|---|---|---|
| Career Firefighters, N = 206 n = 113 Class 1 Obesity vs n = 93 Normal Weight) | Career Firefighters, N = 139 (n = 46 Class 2/3 Obesity vs n = 93 Normal Weight) | Volunteer Firefighters, N = 73 (n = 32 Class 1 Obesity vs n = 41 Normal Weight) | ||||||
|
| ||||||||
| Health Outcome | Odds Ratio | P | Odds Ratio | P | Odds Ratio | P | Odds Ratio | P |
| Meets NFPA fitness criteria† | 0.06 | <0.001 | 0.002 | <0.001 | ‡ | − − − | 0.003 | <0.001 |
| METs | 0.35 | <0.001 | 0.31 | <0.001 | 0.25 | <0.001 | 0.251 | <0.001 |
| Max strength (per 50 lb of pull) | 0.62 | 0.007 | 0.45 | 0.002 | 0.44 | 0.002 | 0.46 | 0.005 |
| Flexibility (in) | 1.04 | 0.525 | 1.01 | 0.872 | 1.04 | 0.562 | 1.07 | 0.477 |
| SBP ≥ 130 mmHg† | 2.71 | 0.013 | 7.01 | <0.001 | 8.59 | <0.001 | 11.81 | <0.001 |
| DBP ≥ 85 mm Hg† | 3.86 | 0.001 | 14.40 | <0.001 | 5.80 | 0.001 | 23.80 | <0.001 |
| Triglyceride ≥ 150 mg/dL† | 4.20 | 0.003 | 3.88 | 0.059 | 3.33 | 0.062 | 6.04 | 0.021 |
| Low HDL (<40 mg/dL in men; <50 mg/dL in women)† | 2.64 | 0.010 | 1.43 | 0.540 | 1.52 | 0.404 | 2.83 | 0.273 |
| Taking hypertension medication† | 4.29 | 0.066 | 2.09 | 0.396 | 7.03 | 0.033 | 5.61 | 0.058 |
HDL, high-density lipoprotein; DBP, diastolic blood pressure; MET, metabolic equivalent; NFPA, National Fire Protection Association; SBP, systolic blood pressure.
Each model represents a generalized linear mixed model predicting weight classification with normal-weight firefighters serving as the referent group. Models are adjusted for age and include department as a random covariate.
for each categorical variable, the referent group represents those who did not meet the criterion.
Odds ratios were undefined due to empty cells in the predictor variable. For instance, no career firefighters in the class 2 or class 3 obese weight categories met the NFPA fitness criteria.
Firefighters meeting class 1 obesity and those meeting classes 2 and 3 combined were significantly less likely to meet the 12.0 METs threshold,4,5,10 with ORs suggesting that obese firefighters were between 94% and 99% less likely to meet 12.0 METs than normal-weight firefighters. Nevertheless, we were unable to create a model for classes 2 and 3 combined obese firefighters on this standard because none met the standard and the model could not converge because of the empty cell (70.8% of normal-weight firefighters met 12.0 METs). Similarly, all obese groups, regardless of department type, demonstrated significantly lower overall fitness levels (METs) and strength, both important components of firefighting- and rescue-related activities.
As a group, firefighters with classes 2 and 3 combined obesity (n = 46) were all obese using the BF% criterion and 95.6% exceeded the WC standard of 40 in or 102 cm. Their average BF% (M ± SD = 36.5 ± 4.4) and WC (47.2 ± 4.0 in) also was very high. The majority of the firefighters with classes II 2 and 3 combined obesity met the NCEP standard for elevated systolic (≥130 mm Hg; 58.7%) and/or diastolic blood pressure (≥85 mm Hg; 52.2%).37 In addition, their average systolic (134.9 ± 15.2) and diastolic (87.0 ± 12.6) blood pressures were elevated in the prehypertension range.27
Not surprisingly, obese firefighters in both career and volunteer departments tended to have less-favorable cardiovascular health profiles, with increased risks for elevated systolic and diastolic blood pressure most common (ORs ranging from 2.71 to 23.80). Other CVD risk factors were less consistent with respect to whether they were statistically significant and some models did not converge because of empty cells (eg, 0.0% normal-weight volunteer firefighters took medications for Type 2 diabetes or high cholesterol vs 5.5% and 12.7% of those with class 1 obesity and 3.0% and 9.1% with classes 2 and 3 obesity, respectively).
DISCUSSION
The prevalence of overweight and obesity combined (BMI ≥ 25 kg/m2) in our cohort of career and volunteer firefighters was consistent with previously published studies that only included single or few departments, typically using convenience samples and, in some cases, using self-report data11,12 and providing only crude prevalence rates. Surprisingly, even after age-standardizing estimates to facilitate comparison with US population estimates,13 this population-based sample of firefighters had higher rates of overweight and obesity and similar rates of obesity (BMI ≥ 30 kg/m2) when compared with the US general adult population. This is surprising because firefighting is not considered to be a sedentary profession, and professional firefighting groups believe that high fitness levels should be expected and supported.3–5,10
Crude rates of obesity based on BF% and WC are similar to those reported for the US adult population using those indices.41–44 Data from this study suggest that firefighters’ body composition is more similar to the general American public, which is plagued by high rates of overweight, obesity, inactivity, and the resulting morbidities.22 This is troubling, given the public expectation that firefighters should be healthy and fit as the job often requires significant exertion for both fire- and rescue-related tasks. On the contrary, perhaps this trend is not so surprising since it also appears to be affecting the US military,45,46 another population thought to be more active and fit than the general public.
Some concerns could be raised about the use of BMI as a primary method of categorizing firefighters as overweight or obese. Because firefighting is an active profession that can have significant physical demands, firefighters with elevated BMIs could have more muscle mass and low body fat, but still be categorized as overweight or obese, as can be the case with some groups of athletes.40,47,48 The false-positive rate for BMI-derived obesity was relatively low when compared with both BF% and WC. It was more likely to be the case that BMI-based obesity classification missed individuals who either had excessive body fat or visceral trunk adiposity (indicated by large WC) but BMIs in the reference or overweight range.
In this sample of career firefighters, who likely should be more active than the general population, 32.7% of those classified as overweight (BMI ≥ 25 kg/m2 but <30 kg/m2) were obese based on the BF% standard. These individuals would experience greater risk for morbidities associated with obesity but would not be considered obese based on BMI. This is the recently discovered problem referred to as “skinny fat” obesity, which appears to confer increased risk for metabolic syndrome and related pathologies and, at least in women, confers greater risk for CVD-related mortality.49 Also, it is clear from these data that BMI is more likely to underestimate obesity than overestimate it by using two other measures of body composition in a population-based sample. Ideally, future research should attempt to replicate this finding by using dual-energy X-ray absorptiometry, the body composition “criterion standard.”
Obesity, regardless of how it was defined, was a strong correlate of not meeting a minimal postcardiac event exercise tolerance standard of 12.0 METs.4,5,10 More than 80% and 95% of the obese career and volunteer firefighters did not meet the standard, while rates were significantly lower among nonobese firefighters, even after adjusting for other significant covariates. In addition, overall MET/VO2max ratio and strength levels were substantially lower in obese firefighters, who also demonstrated more unfavorable CVD risk profiles than their normal-weight counterparts. Obesity and low fitness levels must become priority health issues for the US fire service that wants to reduce LODD related to CVD, other CVD morbidity, disability retirements, and other excess injury, illness, disability, and related costs attributable to excess adiposity.
Few studies have evaluated interventions for addressing weight gain, obesity, and fitness in the fire service culture. One of the largest interventions to date failed to produce significant weight loss or improvements in fitness parameters, although firefighters receiving the intervention experienced less weight gain and improvements in fruit and vegetable consumption.50 More innovative studies are needed to determine what types of interventions would be most successful in improving health and fitness in firefighters.
While this study is the largest population-based study of firefighter obesity to date, there are some important limitations. First, we only conducted cholesterol screening tests, which are not as accurate as laboratory-based assessments. Therefore, the overall pattern of low total cholesterol levels in our sample, particularly among the obese firefighters, is somewhat concerning and suggests potential measurement error in the screening test. Thus, even though low HDL levels also were common in our sample, suggesting elevated risk for CVD, it is likely that these values were affected by potential measurement error. Future studies should consider having a subsample undergo laboratory-based lipid assessments so that the validity of the screening measure can be ascertained.
Second, a nonexercise method was used to estimate VO2max and METs levels. While this method was useful for field epidemiology studies because it was easy to administer and had demonstrated validity when compared to measured VO2max,28–33 it might underestimate fitness levels in firefighters because it was developed and validated using more sedentary occupational groups. Future research is needed to develop and validate nonexercise estimation models for firefighters that include the use of the SRPA and measured VO2max. Third, the 12.0 METs threshold is not a universally accepted fitness standard for all firefighters and was suggested by NFPA 1582 as the minimally acceptable exercise tolerance after a diagnosis of coronary artery disease.5 However, several investigators have suggested 12.0 METs as a minimal threshold for studying firefighter cardiorespiratory fitness.4,10
Fourth, there may be some limits to the generalizability of the study results. Because the population being considered was limited to the IAFC Missouri Valley region (ie,, eight Mid-western states), it is unknown how representative these data are of the national fire service, although they are consistent with previous studies not using population-based random sampling of fire departments.4,6–10 Nevertheless, a study of the Missouri Valley region fire service is a very important first step in establishing an ongoing surveillance program for the fire service and will naturally lead to studies focusing on other regions of the United States. Until now, almost all studies of firefighter obesity have been limited to single or small numbers of fire departments selected as convenience samples. Even though this study was limited to one region of the country, it is by far the largest population-based study of firefighter obesity and fitness using a randomly selected sample. While random selection from the population would limit selection bias somewhat, it was not possible to ensure that every department contacted or every firefighter invited participated, which introduced the possibility of the self-selection bias that is inherent to this type of research.
Conducting an ambitious study of this type nationally was not feasible, given the time and budgetary constraints. It is hoped that the leaders of the primary stakeholder organizations for the fire service (eg, the general public, IAFC, International Association of Fire Fighters, National Volunteer Firefighter Council, National Fallen Firefighter Foundation, National League of Cities, and the Federal Emergency Management Agency) will provide more funding and support as more research on the health of the fire service continues to identify critical issues that need attention. This support will be critical to the future success of programs and interventions aimed at improving fitness and reducing obesity to reduce CVD-related morbidity and mortality, other obesity-related morbidity, and related problems, such as disability and premature retirements among firefighters.6,9,14–16
Acknowledgments
This study was funded by a grant from the Assistance to Firefighters Grants program managed by the Federal Emergency Management Agency in the Department of Homeland Security (“A prospective evaluation of health behavior risk for injury among firefighters— the Firefighter Injury Risk Evaluation [FIRE] study” EMW-2007-FP-02571). The authors thank the departments that participated in this study.
Contributor Information
Walker S. C. Poston, Institute for Biobehavioral Health Research, National Development and Research Institute, Inc, Leawood, Kan.
C. Keith Haddock, Institute for Biobehavioral Health Research, National Development and Research Institute, Inc, Leawood, Kan.
Sara A. Jahnke, Institute for Biobehavioral Health Research, National Development and Research Institute, Inc, Leawood, Kan.
Nattinee Jitnarin, Institute for Biobehavioral Health Research, National Development and Research Institute, Inc, Leawood, Kan; National Development and Research Institute, Inc, New York, NY.
Brianne C. Tuley, Institute for Biobehavioral Health Research, National Development and Research Institute, Inc, Leawood, Kan.
Stefanos N. Kales, Harvard School of Public Health, Occupational Health Program, Boston, Mass.
References
- 1.National Association of Emergency Medical Technicians. About EMS. Available at: http://www.naemt.org/become_a_member/careers/aboutems.aspx. Accessed May 16, 2010.
- 2.US Fire Administration. Fire fighters statistics. http://www.usfa.dhs.gov/statistics/firefighters/index.shtm. Published April 22, 2010. Accessed May 16, 2010.
- 3.International Association of Fire Fighters. The Fire Service Joint Labor Management Wellness-Fitness Initiative. Washington, DC: International Association of Fire Fighters; 2008. [Google Scholar]
- 4.Donovan R, Nelson T, Peel J, Lipsey T, Voyles W, Israel RG. Cardiorespiratory fitness and the metabolic syndrome in firefighters. Occup Med (Lond) 2009;59:487–492. doi: 10.1093/occmed/kqp095. [DOI] [PubMed] [Google Scholar]
- 5.National Fire Protection Association. NFPA 1582, Standards on Comprehensive Occupational Medicine Programs for Fire Departments. Quincy, MA: National Fire Protection Association; 2006. [Google Scholar]
- 6.Kales SN, Polyhronopoulos GN, Aldrich JM, Leitao EO, Christiani DC. Correlates of body mass index in hazardous materials firefighters. J Occup Environ Med. 1999;41:589–595. doi: 10.1097/00043764-199907000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Clark S, Rene A, Theurer WM, Marschall M. Association between body mass index and health status in firefighters. J Occup Environ Med. 2002;44:940–946. doi: 10.1097/00043764-200210000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Mancuso J. Overweight and Obesity on the Omaha Fire Department. Emmitsburg, MD: National Fire Academy; 2003. [Google Scholar]
- 9.Soteriades ES, Hauser R, Kawachi I, Christiani DC, Kales SN. Obesity and risk of job disability in male firefighters. Occup Med (Lond) 2008;58:245–250. doi: 10.1093/occmed/kqm153. [DOI] [PubMed] [Google Scholar]
- 10.Tsismenakis AJ, Christophi CA, Burress JW, Kinney AM, Kim M, Kales SN. The obesity epidemic and future emergency responders. Obesity. 2009;17:1648–1649. doi: 10.1038/oby.2009.63. [DOI] [PubMed] [Google Scholar]
- 11.Yoo HL, Franke WD. Prevalence of cardiovascular disease risk factors in volunteer firefighters. J Occup Environ Med. 2009;51:958–962. doi: 10.1097/JOM.0b013e3181af3a58. [DOI] [PubMed] [Google Scholar]
- 12.National Volunteer Fire Council. NVFC Heart Healthy Firefighter Program, 2004 and 2005 Summary of Screening Results. Available at: http://www.healthy-firefighter.org/files/documents/2006nvfcsummarycharts.pdf. Accessed May 16, 2010.
- 13.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 14.Soteriades ES, Hauser R, Kawachi I, Liarokapis D, Christiani DC, Kales SN. Obesity and cardiovascular disease risk factors in firefighters: a prospective cohort study. Obes Res. 2005;13:1756–1763. doi: 10.1038/oby.2005.214. [DOI] [PubMed] [Google Scholar]
- 15.Fahs CA, Smith DL, Horn GP, et al. Impact of excess body weight on arterial structure, function, and blood pressure in firefighters. Am J Cardiol. 2009;104:1441–1445. doi: 10.1016/j.amjcard.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Fatalities among volunteer and career firefighters—United States, 1994–2004. MMWR Morb Mortal Wkly Rep. 2006;55:453–455. [PubMed] [Google Scholar]
- 17.Maguire BJ, Hunting KL, Smith GS, Levick NR. Occupational fatalities in emergency medical services: a hidden crisis. Ann Emerg Med. 2002;40:625–632. doi: 10.1067/mem.2002.128681. [DOI] [PubMed] [Google Scholar]
- 18.Carnethon MR, Gulati M, Greenland P. Prevalence and cardiovascular disease correlates of low cardiorespiratory fitness in adolescents and adults. JAMA. 2005;294:2981–2988. doi: 10.1001/jama.294.23.2981. [DOI] [PubMed] [Google Scholar]
- 19.Elsner KL, Kolkhorst FW. Metabolic demands of simulated firefighting tasks. Ergonomics. 2008;51:1418–1425. doi: 10.1080/00140130802120259. [DOI] [PubMed] [Google Scholar]
- 20.Michaelides MA, Parpa KM, Thompson J, Brown B. Predicting performance on firefighter’s ability test from fitness parameters. Res Q Exerc Sport. 2008;79:468–475. doi: 10.1080/02701367.2008.10599513. [DOI] [PubMed] [Google Scholar]
- 21.Rhea MR, Alvar BA, Gray R. Physical fitness and job performance of firefighters. J Strength Cond Res. 2004;18:348–352. doi: 10.1519/R-12812.1. [DOI] [PubMed] [Google Scholar]
- 22.US Department of Health and Human Services. The Surgeon General’s Call to Action to Prevent and Decrease Overweight and Obesity. Rockville, MD: US Department of Health and Human Services, Public Health Service, Office of the Surgeon General; 2001. [PubMed] [Google Scholar]
- 23.Mendenhall D. Assessing body composition. http://www.foodfit.com/iaff/articles/body_composition.asp. Accessed September 20, 2010.
- 24.US Fire Administration. National Fire Department Census database. http://www.usfa.dhs.gov/applications/census/. Published 2007. Accessed November 23, 2007.
- 25.Rubiano F, Nunez C, Heymsfield SB. A comparison of body composition techniques. Ann NY Acad Sci. 2000;904:335–338. doi: 10.1111/j.1749-6632.2000.tb06477.x. [DOI] [PubMed] [Google Scholar]
- 26.National Institutes of Health, National Heart, Lung, and Blood Institute. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity: The Evidence Report. Washington, DC: US Government Press; 1998. [Google Scholar]
- 27.US Department of Health and Human Resources. Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. Washington, DC: 2007. [Google Scholar]
- 28.Jackson A, Blair SN, Mahar MT, Wier L, Ross RM, Stuteville JE. Prediction of functional aerobic capacity without exercise testing. Med Sci Sports Exerc. 1990;22:863–870. doi: 10.1249/00005768-199012000-00021. [DOI] [PubMed] [Google Scholar]
- 29.Jackson A, Ross RM. Understanding Exercise for Health and Fitness. 3rd. Dubuque, IA: Kendall/Hunt; 1997. [Google Scholar]
- 30.Jackson A, Beard E, Wier L, Ross R, Stuteville J, Blair S. Changes in aerobic power of men ages 25–70 years. Med Sci Sports Exerc. 1995;27:113–120. [PubMed] [Google Scholar]
- 31.Jackson A, Wier L, Ayers G, Beard E, Stuteville J, Blaire S. Changes in aerobic power of women, ages 20–64 yr. Med Sci Sports Exerc. 1996;28:884–891. doi: 10.1097/00005768-199607000-00016. [DOI] [PubMed] [Google Scholar]
- 32.Jurca R, Jackson AS, LaMonte MJ, et al. Assessing cardiorespiratory fitness without performing exercise testing. Am J Prev Med. 2005;29:185–193. doi: 10.1016/j.amepre.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 33.Wier L, Jackson AS, Ayers GW, Arenare B. Nonexercise models for estimating VO2 max with waist girth, percent fat, or BMI. Med Sci Sports Exerc. 2006;38:555–561. doi: 10.1249/01.mss.0000193561.64152. [DOI] [PubMed] [Google Scholar]
- 34.National Fire Protection Association. NFPA 1500, Standards on fire Department Occupational Safety and Health Program. Quincy, MA: National Fire Protection Association; 2007. [Google Scholar]
- 35.Booth ML. Assessment of physical activity: an international perspective. Res Q Exerc Sport. 2000;71:S114–S120. [PubMed] [Google Scholar]
- 36.Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 37.Miranda PJ, DeFronzo RA, Califf RM, Guyton JR. Metabolic syndrome: definition, pathophysiology, and mechanisms. Am Heart J. 2005;149:33–45. doi: 10.1016/j.ahj.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 38.US Census Bureau. DP-1 General Demographic Characteristics, 2008 Population Estimates, United States. http://factfinder.census.gov/servlet/QTTable?-ds_name=PEP_2008_EST&-qr_name=PEP_2008_EST_DP1&-geo_id=01000US. Accessed August 17, 2010.
- 39.Hennekens CH, Buring JE. Epidemiology in Medicine. Philadelphia, PA: Lippincott Williams & Wilkins; 1987. [Google Scholar]
- 40.Ford ES, Mokdad AH, Giles WH. Trends in waist circumference among U.S. adults. Obes Res. 2003;11:1223–1231. doi: 10.1038/oby.2003.168. [DOI] [PubMed] [Google Scholar]
- 41.Flegal KM, Shepherd JA, Looker AC, et al. Comparisons of percentage body fat, body mass index, waist circumference, and waist-stature rations in adults. Am J Clin Nutr. 2009;89:500–508. doi: 10.3945/ajcn.2008.26847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Borrud LG, Flegal KM, Looker AC, Everhart JE, Harris TB, Shepherd JA. Body composition data for individuals 8 years of age and older: U.S. population, 1999–2004. Vital Health Stat. 2010;250:1–87. [PMC free article] [PubMed] [Google Scholar]
- 43.Rothman KJ. BMI-related errors in the measurement of obesity. Int J Obes (Lond) 2008;32:S56–S59. doi: 10.1038/ijo.2008.87. [DOI] [PubMed] [Google Scholar]
- 44.Poston WSC, Haddock CK, Peterson AL, et al. Comparison of weight status among two cohorts of US Air Force recruits. Prev Med. 2005;40:602–609. doi: 10.1016/j.ypmed.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 45.Bray RM, Pemberton MR, Hourani LL, et al. 2008 Department of Defense Survey of health-related behaviors among active military personnel: A component of the Defense Lifestyle Assessment Program (DLAP) Research Triangle Park, NC: RTI International; 2009. [Google Scholar]
- 46.Jonnalagadda SS, Skinner R, Moore L. Overweight athlete: fact or fiction? Curr Sports Med Rep. 2004;3:198–205. doi: 10.1249/00149619-200408000-00005. [DOI] [PubMed] [Google Scholar]
- 47.Nevill AM, Stewart AD, Olds T, Holder R. Relationship between adiposity and body size reveals limitations of BMI. Am J Phys Anthropol. 2006;129:151–156. doi: 10.1002/ajpa.20262. [DOI] [PubMed] [Google Scholar]
- 48.Adams JR, Horn T, Potteiger J, Claytor R. Does BMI determine obesity levels in Division I college football players? Med Sci Sports Exerc. 2008;40:S276. [Google Scholar]
- 49.Romero-Corral A, Somers VK, Sierra-Johnson J, Korenfeld Y, Boarin S, Korinek J, et al. Normal weight obesity: a risk factor for cardiometabolic dysregulation and cardiovascular mortality. Eur Heart J. 2010;31:737–746. doi: 10.1093/eurheartj/ehp487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Elliot DL, Goldberg L, Kuehl KS, Moe EL, Breger RKR, Pickering MA. The PHLAME (promoting healthy lifestyles: alternative models’ effects) firefighter study: outcomes of two models of behavior change. J Occup Environ Med. 2007;49:204–213. doi: 10.1097/JOM.0b013e3180329a8d. [DOI] [PubMed] [Google Scholar]


