Abstract
The rendezvous technique typically involves combined efforts of interventional radiology, endoscopy, and surgery. It can be done solely percutaneously, whereby the interventionalist gains desired access to one point in the body by approaching it from two different access sites. We present the case of a woman who underwent cholecystectomy complicated by a bile duct injury. A percutaneous rendezvous procedure enabled placement of an internal-external drain from the intrahepatic ducts through the biloma and distal common bile duct and into the duodenum. Thus, a percutaneous rendezvous technique is feasible for managing a bile duct injury when endoscopic retrograde cholangio-pancreatography or percutaneous transhepatic cholangiogram alone has been unsuccessful.
Keywords: Rendezvous, Biloma, Bile duct injury
Introduction
A rendezvous technique classically involves a combination of surgical, endoscopic, and percutaneous approaches to reach 1 point in the body through 2 access points. It is often employed in the management of hepatobiliary dysfunction, such as biliary stenosis, stones, injury, and leakage when either endoscopic retrograde cholangio-pancreatography (ERCP) or percutaneous drainage alone is not sufficient [1]. We present a case whereby percutaneous intervention was the sole mechanism used to perform the rendezvous procedure. Our institutional review board does not need to routinely review or approve case report forms.
Case summary
A 44-year-old woman with a history of systemic lupus erythematosus and hypertension presented with a 2-month history of postprandial epigastric pain radiating to the back and nausea. One month before, an ultrasound revealed gallstones. The patient underwent laparoscopic converted to open cholecystectomy. On the first postoperative day, bilious drainage from the surgical drain appeared. A hepatobiliary (HIDA) scan suggested a bile leak. Endoscopic retrograde cholangio-pancreatography (ERCP) was unsuccessful because of ampullary stenosis. Percutaneous transhepatic cholangiogram (PTC) was performed revealing right and left intrahepatic ducts filling a subhepatic biloma. The distal common bile duct was not visualized, and the small bowel could not be accessed (Fig. 1). An 8Fr external biliary drain was placed from a right intrahepatic duct into the biloma. The patient was discharged on postoperative day 9 asymptomatic but returned 2 days later with abdominal pain, fever, and chills. She was hospitalized for 13 days and treated with antibiotics for sepsis. Computed tomography scan identified multiple abdominal fluid collections, which were drained, and a second 10Fr external drain was placed percutaneously directly into the biloma. Eleven days later, she was admitted to the hospital with nausea, vomiting, and right upper quadrant pain. The decision was made to do a rendezvous procedure to place an internal-external drain.
Fig. 1.
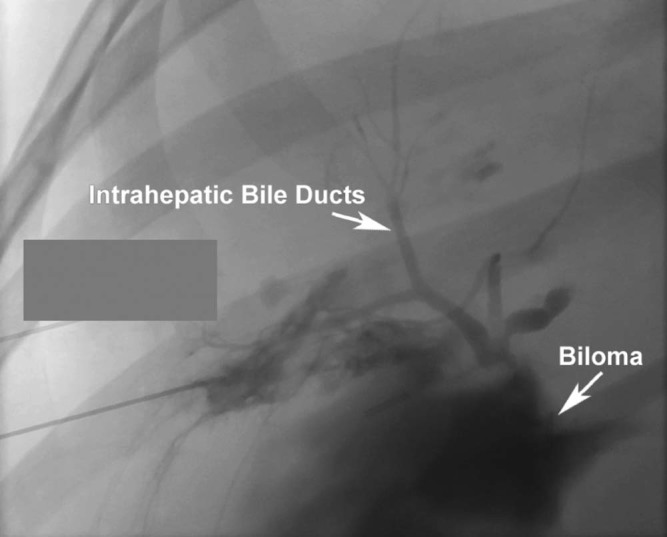
A 21-gauge needle was inserted into the right intrahepatic bile duct, and contrast medium filled a subhepatic biloma but not the common bile duct.
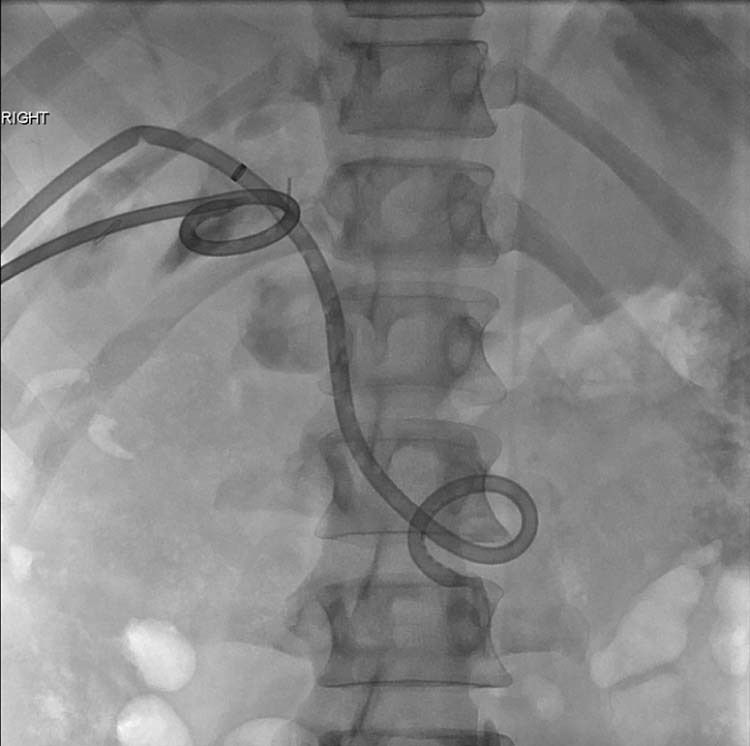
During the rendezvous procedure, a 0.035-inch Bentson guidewire (Cook, Inc, Bloomington, IN) was inserted through the biloma access point and a 10Fr 11-cm vascular sheath (Cook, Inc, Bloomington, Indiana) was placed. A Kumpe catheter (Cook, Inc) was placed through the biloma access site and a contrast medium was injected. The common bile duct and small bowel were clearly visualized (Fig. 2). A 150-cm 0.018-inch glidewire (Terumo, Tokyo, Japan) was manipulated through the distal common bile duct and into the duodenum (Fig. 3). A Kumpe catheter was advanced over the glidewire and into the small bowel. A 0.035-inch Amplatz wire (Boston Scientific Corporation, Natick, MA) was positioned outside the sheath and into the small bowel as a safety wire. The glidewire was removed and the “back end” of a 260 cm 0.035-inch Bentson guidewire was inserted through the catheter at the biloma access point and was placed into the duodenum. The catheter was then removed. The “floppy end” of the guidewire was inserted through the sheath into the subhepatic biloma space. A loop of wire remained external to the patient at the biloma access point. An EnSnare (En Snare Endovascular Snare System, Merit Medical Systems, South Jordan, UT) was placed into the biloma through the right intrahepatic bile duct access (Fig. 4). The “floppy end” of the guidewire was snared and brought out of the patient (Fig. 5). The sheath in the biloma was removed over the “in and out” wire. Tension was placed on the external “floppy end” of the guidewire at the hepatic access as the external loop at the biloma was maneuvered completely into the body and the loop straightened. This maneuver resulted in continuous access from the intrahepatic ducts, through the biloma, across the injured bile duct, and into the duodenum with the guidewire. A 14Fr internal-external drain was placed over the wire, and a 12Fr drain was placed in the subhepatic biloma space (Fig. 6).
Fig. 2.
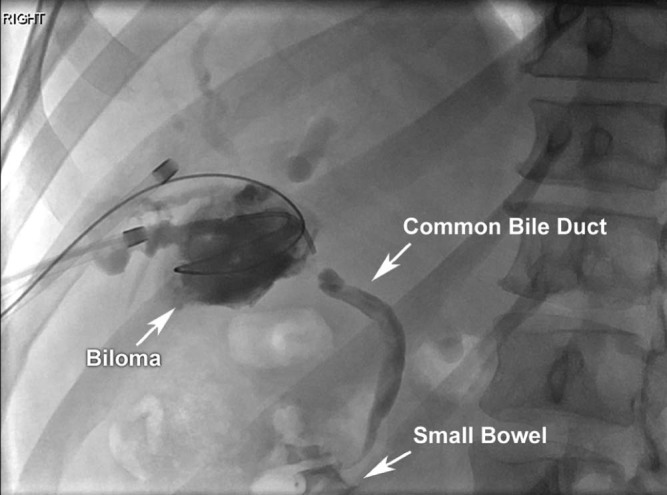
A 10Fr sheath is in the right intrahepatic bile duct, and a 0.035-inch Bentson guidewire (Cook, Inc) is visualized traveling through the right intrahepatic bile duct to the biloma. An additional 10Fr sheath is positioned directly into the biloma, and a Kumpe catheter (Cook, Inc) was used to inject contrast medium into the biloma. Contrast medium filled the common bile duct and small bowel.
Fig. 3.
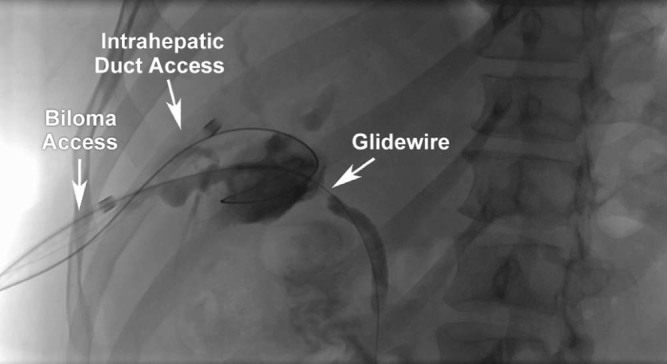
A 0.018-inch glidewire was manipulated from the biloma access point through the common bile duct and into the small bowel. A 0.035-inch Bentson wire is in place from the right intrahepatic bile duct access point into the biloma.
Fig. 4.
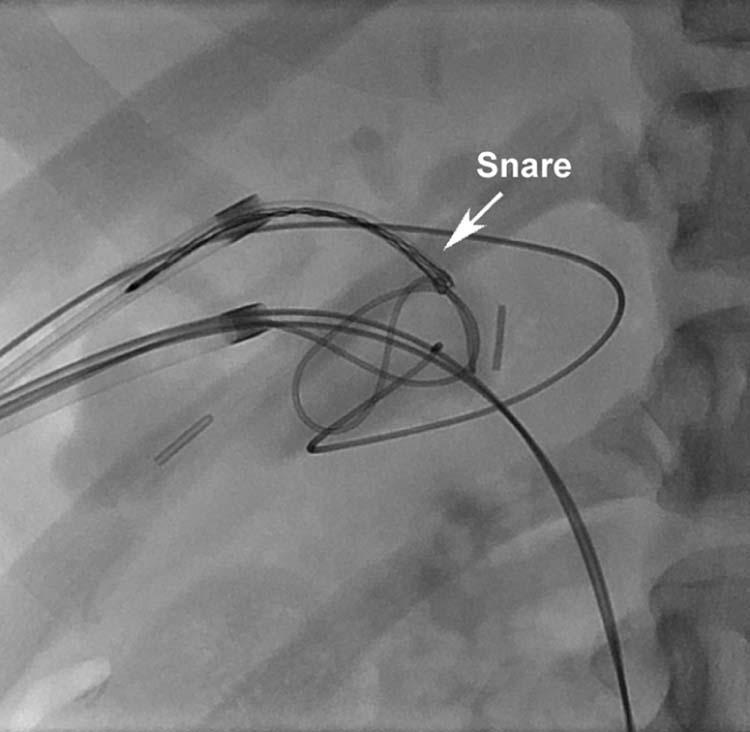
An EnSnare (En Snare Endovascular Snare System, Merit Medical Systems) was placed into the biloma through the right intrahepatic bile duct, and it snared the floppy end of a 0.035-inch guidewire. The back end of the guidewire crossed the common bile duct and entered the duodenum.
Fig. 5.
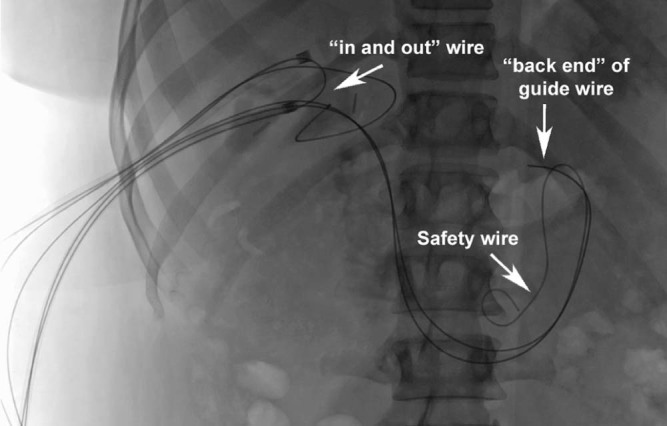
A 0.035-inch Amplatz wire is in place as a safety wire outside the vascular sheath through the biloma access point and into the small bowel. The 260 cm 0.035-inch Bentson guidewire is seen in its “in and out” position with the “back end” of the wire in the small bowel, a loop of wire external to the patient at the biloma access point, and the “floppy end” of the wire external to the patient at the right intrahepatic duct access point. A 0.035-inch Bentson guidewire is in place as a safety wire through the right intrahepatic duct access point and into the biloma.
Fig. 6.
A 14Fr drain was placed over the wire from the intrahepatic ducts, through the biloma, and into the duodenum. The proximal kinks were corrected. The short 12Fr drain remained in the subhepatic biloma at this time.
Discussion
Bile duct injuries are a potential complication of cholecystectomy and can range from mild to severe in their consequences [2]. As a result of these injuries, bile leaks can occur, causing intra-abdominal collections, fistula formation, or peritonitis [3]. The incidence of bilomas after laparoscopic cholecystectomy has been reported to be 2.5%. Patients with a biloma typically present with right upper quadrant or epigastric pain, jaundice, elevated liver function tests, abdominal distention, fever, and leukocytosis [2]. Biliary leakage can also present as in this case with increased bilious output from surgical drains [3]. Typical nonoperative management involves percutaneous drainage or sphincterotomy and stenting by ERCP, with the goal being to decompress the biliary tree and close the defect [3], [4]. However, ERCP can exacerbate biloma formation because of increased pressure in the proximal bile ducts from contrast medium injection and is limited in cases of severe ampullary stenosis [3].
A similar case was reported where an internal-external drain was unable to be placed by either ERCP or PTC alone. ERCP was used to place a guidewire into the biloma, and the wire was snared during PTC to allow the biliary tree to drain into the duodenum [5]. This technique can also be performed solely using percutaneous mechanisms without endoscopy as discussed in our case. De Robertis et al. also described the use of percutaneous rendezvous mechanisms to overcome biliary confluence stenosis for bilateral drainage, bridge iatrogenic biliary defects, and create a percutaneous biliodigestive anastomosis after failed surgical anastomosis [1]. The result is the restoration of biliary continuity to relieve symptoms and possibly prevent additional surgical interventions [1].
Conclusion
Injuries to the common bile duct resulting in noncommunication between proximal and distal ends of the duct can cause biloma formation and pose a logistical problem both for ERCP and PTC. A percutaneous rendezvous technique without endoscopy is a feasible option for the management of postcholecystectomy bile duct injury and biloma formation.
Acknowledgment
We would like to extend our sincere appreciation to Lacie Covington, Donna Ashlock, and Dr. Linda Deloney for their assistance in the creation of this manuscript.
This research did not receive any specific grant from funding agencies in the public, commercial, or non-for-profit sectors.
Footnotes
Competing Interests: The authors have no conflicts of interest or financial disclosures.
References
- 1.De Robertis R., Contro A., Zamboni G., Mansueto G. Totally percutaneous rendezvous techniques for the treatment of bile strictures and leakages. J Vasc Interv Radiol. 2014;25(4):650–654. doi: 10.1016/j.jvir.2013.12.584. [DOI] [PubMed] [Google Scholar]
- 2.Tiwari C., Makhija O.P., Makhija D., Jayaswal S., Shah H. Post laparoscopic cholecystectomy biloma in a child managed by endoscopic retrograde cholangio-pancreatography and stenting: a case report. Pediatr Gastroenterol Hepatol Nutr. 2016;19(4):281–285. doi: 10.5223/pghn.2016.19.4.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mehmedovic Z., Mehmedovic M., Hasanovic J. A rare case of biliary leakage after laparoscopic cholecystectomy-diagnostic evaluation and nonsurgical treatment: a case report. Acta Inform Med. 2015;23(2):116–119. doi: 10.5455/aim.2015.23.116-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee J.H., Suh J.I. A case of infected biloma due to spontaneous intrahepatic biliary rupture. Korean J Intern Med. 2007;22(3):220–224. doi: 10.3904/kjim.2007.22.3.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shin S., Klevan A., Fernandez C.A., Astudillo J.A., Martinez J. Rendezvous technique for the treatment of complete common bile duct transection after multiple hepatobiliary surgeries. J Laparoendosc Adv Surg Tech A. 2014;24(10):728–730. doi: 10.1089/lap.2014.0374. [DOI] [PubMed] [Google Scholar]


