Abstract
Objective
This study examined whether assisted outpatient treatment (AOT) under New York’s “Kendra’s Law” is associated with reduced arrests for violent and nonviolent offenses.
Methods
Arrest records of 183 study participants attending outpatient clinics in New York City, 86 of whom were ever and 97 of whom were never assigned to AOT, were compiled to yield 16,890 months of observation. For each month the data indicated whether an arrest did or did not occur and whether a participant was or was not assigned to AOT. Generalized estimating equations and fixed-effects analyses were used to compare arrest rates within different periods (before, during or shortly after, and more than six months after) for those ever assigned and between the ever- and never-assigned groups.
Results
For those who received AOT, the odds of any arrest were 2.66 times greater (p<.01) and the odds of arrest for a violent offense 8.61 times greater (p<.05) before AOT than they were in the period during and shortly after AOT. The group never receiving AOT had nearly double the odds (1.91, p<.05) of arrest compared with the AOT group in the period during and shortly after assignment.
Conclusions
Outpatient commitment under Kendra’s Law in New York State is associated with a reduced risk of arrest. The coercion necessitated by application of the law may forestall, at least for some people, the potentially more potent and consequential coercion they would have experienced in the criminal justice system.
Determining whether court-ordered psychiatric outpatient commitment reduces arrest among people with mental illnesses is critically important for multiple reasons. Arrest is a devastating experience for individuals and their families, and its societal costs are enormous (1). Further, given the intense debate about outpatient commitment, it is important to assess whether legally mandated outpatient treatment forestalls the subsequent and even more noxious forms of coercion that arrest brings. This possible trade-off of a milder form of coercion for a more severe one could represent useful information in considering the value of outpatient commitment.
New York State established outpatient commitment in 1999 through Mental Health Law 9.60 (known as “Kendra’s Law”), under which court-ordered assisted outpatient treatment (AOT) could be mandated for certain individuals with mental illness and a history of multiple hospitalizations or violence toward self or others. Specific legal criteria are required for an assignment to AOT, including a judgment based on a history of treatment noncompliance whereby the individual is considered unlikely to voluntarily adhere to treatment and has a high likelihood of benefiting from mandated treatment. Individuals entering AOT are assigned a case manager and prioritized for enhanced services that include housing and vocational services.
There are several reasons why outpatient commitment approaches such as AOT might reduce the risk of arrest. Comprehensive reviews of outpatient commitment report lower rates and durations of subsequent psychiatric hospitalizations, enhanced adherence to medication, and reduced disruptive symptoms (2,3). Two recent studies conducted in New York support this general conclusion. In the first, New York City residents receiving AOT were found to have reduced suicide risk, better illness-related social functioning, and lower rates of violence than a propensity score–matched comparison group (4). In the second, AOT recipients’ hospitalization rates were lower while receiving AOT than they had been before AOT (5). Broad-based benefits like these might be expected to reduce arrests. On the other hand, most mental health interventions aim to reduce symptoms and associated impairments and do not directly target factors leading to arrests of people with mental illnesses (6). Also, outpatient commitment involves heightened surveillance that could elevate the chance of being apprehended. Finally, some argue that, in the long run, the coercion associated with outpatient commitment impedes treatment engagement (7), thereby facilitating untoward outcomes such as arrest.
Existing evidence on outpatient commitment and arrest
There have been only two randomized trials to examine the consequences of outpatient commitment for arrests (8,9). In the first study, Steadman and colleagues (8) found overall arrests during an 11-month follow-up to be almost identical for individuals assigned to outpatient commitment (18%) and a control group who did not receive outpatient commitment (16%). In the second study, Swartz and colleagues (9) reported no significant difference in overall arrests during a 12-month follow-up (outpatient commitment group, 18.6%; control group, 19.3%). Although these studies showed no significant effect of outpatient commitment on arrest, three facts suggest the need for additional investigations. First, probably because they are rare, arrests for violent offenses were not assessed separately from overall arrests. Second, the duration of follow-up in these studies was relatively brief, thereby providing a smaller number of person-months of observation than would be considered ideal. Third, individuals posing the most serious violence risk were excluded from the randomized component of both studies for ethical and safety reasons.
A recent assessment of outpatient commitment in New York State (10) also included an assessment of the effects of AOT on arrest (11). The analysis involved samples of AOT clients and individuals receiving enhanced voluntary services in New York State. The study did not exclude people at high risk of violence and did include a longer follow-up to assemble 9,255 months of observation. Gilbert and colleagues (11) found that overall arrests were significantly higher in the months before AOT than in the months during AOT. No statistically significant difference in arrest was found between the AOT group and the individuals who voluntarily accepted enhanced treatment.
We conducted a quasi-experimental study (N=183) that included individuals at high risk of violence and observed them over several years to yield 16,890 person-months of observation. Our study builds on the study by Gilbert and colleagues (11) in three important ways. First, we included a group of patients who were recruited from the same clinics as the AOT patients but who had never received AOT. This group is important for understanding the effects of AOT because it enabled us to give an estimate of the risk of arrest in a group that was not deemed to be in need of AOT. It therefore provides a useful benchmark that allowed us to ask how closely the AOT group approached the risk level of this much-lower-risk group. Second, because sufficient events accrued over the long period of observation, our study allowed us to test the effect of AOT on violent offenses. Third, there were sufficient months of observation after AOT ended to provide an estimate of risk during that important period.
Methods
Sample and procedure
We analyzed officially recorded arrests of individuals attending outpatient clinics in the New York City boroughs of the Bronx and Queens. Participants were recruited for a longitudinal study conducted between January 2003 and January 2006, which focused on self-reported psychosocial outcomes associated with AOT (4). After a complete description of the study, written informed consent was obtained from participants, including consent to conduct searches of records. Institutional review board approval was obtained from the New York State Psychiatric Institute, Bronx Psychiatric Center, Creedmoor Psychiatric Center, Bronx-Lebanon Medical Center, and the New York State Office of Mental Health (NYS OMH).
The sample for this report included 183 participants—86 who were assigned to AOT at some point in their lives and a comparison group of 97 individuals never assigned to AOT.
Dependent variables
Official arrest data, including the date of each offense and the associated charge, were obtained from the New York State Department of Criminal Justice Services (DCJS) for each participant from the date he or she turned 18 until January 1, 2007. The DCJS database includes excellent coverage of arrests by local and state police within New York, but coverage of arrests outside of the state is less consistent. For this reason, rather than using data from age 18 onward, we began recording arrests 60 months before participants were recruited into our study because we were certain of residence in New York at time of interview. Using the information provided by DCJS, we constructed a data file indicating whether a study participant was arrested or not arrested in every month of observation. In addition to analyzing arrests for any offense, we also categorized arrests according to whether the charge was for a violent offense (murder, non-negligent manslaughter, forcible rape, robbery, and aggravated assault).
Independent variable
We used NYS OMH records to accurately identify periods in which individuals were assigned to AOT. For individuals who were ever assigned to AOT, we constructed three periods—before AOT, during and six months after AOT, and more than six months after AOT ended. We reasoned that any effects of AOT would be sustained for at least a few months and that, as a result, the six-month period after AOT ended might be more appropriately grouped with the period in which participants were assigned to AOT. Within-group analyses using these three time points were conducted as described below. In addition, we conducted between-group analysis to compare arrests in these three periods with arrests in the comparison group that never received AOT.
Covariates
We controlled for age, gender, race-ethnicity (black, Hispanic, white, and other), psychiatric diagnosis category at recruitment, educational attainment, and the number of months of observation.
Analysis
We used logistic regression estimated via generalized estimating equations (GEE) to compare the odds of arrest during the period of AOT assignment and the six months after it with the odds of arrest before AOT and six months or more after completion of AOT and among individuals never assigned to AOT. Thus our analysis provided both within- and between-person comparisons. GEE was appropriate because it could use all information from individuals who contributed different numbers of months of follow-up and because it could take into account the correlated nature of the responses in the within-person component of the design. Our analysis used an exchangeable correlation matrix in the GEE procedure (12).
We used fixed-effects logistic regression as an ancillary approach because it controls for the stable effects of stable confounding variables even if those confounding variables were not measured (13). The approach removes between-person variance, leaving only within-person variance for analysis. By removing the between-person variance, the effects of stable determinants of individual differences, whether measured or not, are effectively controlled. Because fixed-effects analyses addressed within-person changes in variables (that is, arrest and assignment to AOT), only individuals who experienced changes in these variables could be included in the analysis, leaving 40 persons who contributed 3,815 months of observation. Fixed-effects analyses were conducted only for all arrests combined, because arrests for violent offenses were too rare to produce stable estimates. We compared our estimates of the effect of AOT on arrest from the fixed-effects and GEE analyses to determine whether our conclusion about the effect of AOT was the same in these complementary analytic approaches.
Results
Sample
Table 1 is based on data collected in interviews and chart reviews. The sample was mostly male, young to middle-aged, with relatively low levels of education. Reflecting the communities where the clinics were located, the sample was largely African American and Hispanic. The only significant difference between those ever and never receiving AOT was that men were overrepresented in the AOT group (67% versus 54%).
Table 1.
Characteristics of participants never or ever receiving assisted outpatient treatment (AOT)
| Characteristic | Total sample (N=183) |
Never on AOT (N=97) |
Ever on AOT (N=86) |
|||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Demographic | ||||||
| Malea | 110 | 60 | 52 | 54 | 58 | 67 |
| Completed high school or GED | 111 | 61 | 59 | 61 | 52 | 60 |
| Race-ethnicity | ||||||
| African American | 98 | 54 | 49 | 51 | 49 | 57 |
| Hispanic | 53 | 29 | 30 | 31 | 23 | 27 |
| White or other | 32 | 18 | 18 | 19 | 14 | 16 |
| Age (M±SD) | 37.0±11.1 | 37.5±11.8 | 36.5±10.2 | |||
| Primary chart diagnosis | ||||||
| Psychotic disorder | 128 | 70 | 63 | 65 | 65 | 76 |
| Mood disorder | 45 | 25 | 28 | 29 | 17 | 20 |
| Other | 10 | 5 | 6 | 6 | 4 | 5 |
p<.05
Arrests
Arrests for individuals never assigned to AOT occurred in 1.2% of the 8,546 months of follow-up. For individuals assigned to AOT, arrests occurred in 2.2% of the 4,182 months before AOT, .9% of the 2,327 months during and six months after AOT, and 1.4% of the 1,835 months occurring more than six months after AOT.
GEE analyses
Table 2 shows logistic regression coefficients comparing risks of arrest in the different periods of observation for all arrests and for arrests for violent offenses. As expected, overall arrests were far less common among women, declined with age, and were less common among individuals with higher education. African Americans were more likely to have experienced a contact with police that led to arrest. No differences according to category of psychiatric diagnosis were found. Within-group results showed that the risk of arrest was significantly higher during the period before AOT than during the period of AOT, and although the risk of arrest went up slightly in the period after AOT, this difference was not significant. Moreover, between-group results showed that risk of arrest among individuals who were never assigned to AOT was significantly higher than that of the AOT group while assigned to AOT. Using within-group analyses, we also compared (not shown in Table 2) the period before AOT with the period after AOT, finding the risk in the earlier period to be significantly higher than in the later period. Because arrests for violent offenses were relatively rare, many of the covariates were not statistically significant (Table 2). However, even with small numbers, individuals receiving AOT were at significantly lower risk of arrest than they were before AOT.
Table 2.
Logistic regression to determine predictors of arrest among persons receiving or not receiving assisted outpatient treatment (AOT)
| Characteristic | All arrests
|
Arrests for violent offenses
|
||
|---|---|---|---|---|
| Coefficient | SE | Coefficient | SE | |
| Before AOTa | .977*** | .262 | 2.153* | 1.046 |
| >6 months after AOTa | .454 | .310 | .903 | 1.230 |
| Never on AOTa | .645* | .307 | 1.638 | 1.046 |
| Age | −.036*** | .011 | −.043* | .020 |
| Male | 1.56*** | .323 | .503 | .452 |
| African American | .828* | .329 | .039 | .478 |
| Hispanic | .094 | .373 | −.403 | .577 |
| Psychotic disorder | −.509 | .421 | .273 | 1.068 |
| Mood disorder | −.435 | .461 | .753 | 1.090 |
| High school or higher education | −.465* | .198 | −.392* | .363 |
| Months of follow-up | .041** | .013 | .052* | .026 |
Reference: receiving or within six months of receiving AOT
p<.05
p<.01
p<.001
Figure 1 portrays results from Table 2 in the form of odds ratios (ORs). As the figure shows, for persons who had ever received AOT, the risk of any arrest was 2.66 times greater (95% confidence interval [CI]=1.58–4.44) and the risk of arrest for a violent offense was 8.61 times greater (CI=1.12–65.97) before AOT than it was while receiving AOT. In addition, compared with individuals during and shortly after the period of assignment to AOT, the comparison group that had never received AOT had nearly double the odds (OR=1.91, CI=1.05–3.48) of arrest. As an additional check, when we included as “receiving AOT” only those months actually assigned to AOT rather than “AOT plus six months after the termination of AOT,” our models showed very similar results.
Figure 1. Odds of arrest among persons who did or did not receive assertive outpatient treatment (AOT)a.
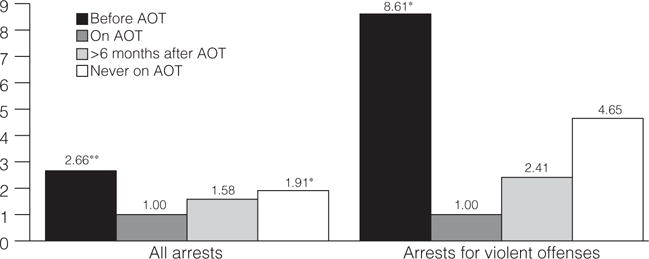
aOdds ratios were adjusted for age, gender, race-ethnicity, education level, psychiatric diagnosis, and months of follow-up. Reference group: those currently receiving AOT. *p<.05, **p<.001
Fixed-effects analyses supply some degree of control of unmeasured confounding and therefore provided a useful comparison to GEE analyses. Compared with arrests during and six months after participants were enrolled in AOT, arrests before AOT were 2.24 (CI=1.14–4.39) times more likely, a point estimate that was reasonably close to the OR of 2.66 from the GEE analyses. The OR for arrest in the period after AOT indicated a nonsignificant increase compared with the period of AOT (OR=1.82, CI=.94–3.52). This consistency across analyses that differed in strengths and weaknesses (GEE and fixed-effects) increased confidence that AOT was associated with a reduction in arrests.
Discussion
Main findings
We found AOT to be associated with a sizeable reduction in the probability of arrest for both overall and violent offenses. Before assignment, individuals who would later be enrolled in AOT were substantially more likely than the same individuals while receiving AOT to experience arrest for both overall and violent offenses. In addition, we found that while individuals were enrolled in AOT the risk of arrest was actually lower than that of a comparison group of individuals never assigned to AOT and that the risk of arrest after AOT ended remained significantly lower than the risk in the period before AOT began.
AOT, as implemented under Kendra’s Law in New York State, is a policy that substantially reduces the risk of arrest, including arrests for violent offenses among people with serious mental illnesses. From the vantage point of a general public concerned with violence and who hold prevalent perceptions of dangerousness concerning people with mental illnesses (14,15), this is a very positive and straightforward outcome: Kendra’s Law directly results in reduced crime and violence. In addition, the result pushes us to consider a very beneficial trade-off in coercion, with a relatively small exposure under Kendra’s Law forestalling a substantially larger exposure delivered by arrest. Our results can be read as an indication that both the general public and people assigned to AOT benefit—the former through a reduction in crime and violence and the latter through a reduction in experienced coercion and all of its untoward consequences.
The idea of a powerful mutual benefit, however, is complicated by the following considerations. First, a majority (53%), of the 86 study participants assigned to AOT were never arrested—not before, during, or after their assignment. It is, of course, possible that AOT forestalled some arrests during and after assignment of people who had never been arrested before assignment. At the same time, given that a majority of the AOT group was never arrested, it is likely that some people assigned to AOT were at extremely small or even no risk of arrest. For these individuals, there was no arrest reduction benefit to procure. It is also true that AOT strives to affect outcomes other than arrest, such as quality of life and reduction in self-harm, and previous research has shown benefits in these other domains (2–5). Still, in considering the trade-off in coercion, we must also consider that some people received the coercion of AOT without the possibility of a benefit in reduced coercion due to arrest. Second, although the coercion embodied in outpatient commitment is less severe than that involved in arrest, an important difference exists in the administration of the two forms of coercion. Arrest, at least in theory, is a specific response to a specific illegal action, whereas outpatient commitment is coercion administered to forestall events—illegal and otherwise—that might happen in the future. From a procedural justice point of view, the two types of coercion are quite different and might reasonably be experienced as such by individuals exposed to them (16,17).
Considerations concerning study validity
To minimize the influence of out-of-state arrests, we included as follow-up only months relatively close to a time when we knew the individual was living in New York (that is, at time of interview). In addition, we would expect coverage of arrests to be much better during AOT when the individual is mandated to treatment and known to be a New York State resident. As a result, any bias would be toward higher arrest rates during AOT than at other times, but we found just the opposite. Another consideration is that although outpatient clinics in New York City provided a good situation in which to test the effects of AOT, generalization to other populations should be made cautiously.
A strength of our quasi-experimental study is that it included individuals at risk of arrest for violent offenses and observed them for a period totaling more than 1,400 person-years. A limitation of our study is that it was not an experimental study with random assignment to study conditions. Yet the design, the analysis, and the pattern of achieved results increase confidence in our findings for the following reasons. First, one would expect the AOT group to have a greater risk of violence because selection into that group depends, in part, on the risk of violence and arrest. The finding that while participants received AOT their risk of arrest was lower than in the comparison group who had never received AOT runs counter to the bias one would expect in our quasi-experimental design. Second, our study provides results of within-group comparisons (before, during, and after AOT) that are not contaminated by biases associated with nonequivalence between groups. Finally, by controlling the effects of stable confounding variables, the fixed-effects analysis added a stringent test that provided concordant findings. Nevertheless, we caution that an ideal study would include both the analytic and design strengths of our study and random assignment to treatment conditions. As a result, we suggest that readers consider our findings in light of their deviation from such an ideal design.
Conclusions
Conclusions about the effectiveness of outpatient commitment as a policy cannot, of course, be based on results about arrest alone. With respect to this issue, studies have shown not only positive consequences but the absence of negative ones as well (2–4,18). When considered in combination with these other studies, the conclusion about the effectiveness of outpatient commitment is generally positive, and in New York State, where this evaluation took place, the decision has been made to extend outpatient commitment. Still we end with a caution. So far, evaluations of outpatient commitment have occurred in the uptake of new policies when scrutiny of them by critics, policy makers, and the general public is intense. Waves of prior policy changes in public psychiatry have initially been met with enthusiasm and bold reports of effectiveness, only to later be deemed near total failures. In light of this history we need to be sure that the integrity of the enhanced services associated with outpatient commitment remains strong and that ongoing assessments of the policy are actively pursued.
Acknowledgments
This research was funded by the New York State Office of Mental Health.
Footnotes
Disclosures
The authors report no competing interests.
Contributor Information
Dr. Bruce G. Link, Mailman School of Public Health and the New York State Psychiatric Institute, Columbia University, 722 W. 168th St., Room 1609, New York, NY 10032
Dr. Matthew W. Epperson, School of Social Service Administration, University of Chicago
Dr. Brian E. Perron, School of Social Work, University of Michigan, Ann Arbor
Dr. Dorothy M. Castille, Department of Epidemiology, Columbia University, New York City
Dr. Lawrence H. Yang, Department of Epidemiology, Columbia University, New York City
References
- 1.McCollister KE, French MT, Fang H. The cost of crime to society: new crime-specific estimates for policy and program evaluation. Drug and Alcohol Dependence. 2010;108:98–109. doi: 10.1016/j.drugalcdep.2009.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Swartz MS, Swanson JW. Involuntary outpatient commitment, community treatment orders, and assisted outpatient treatment: what’s in the data? Canadian Journal of Psychiatry. 2004;49:585–591. doi: 10.1177/070674370404900903. [DOI] [PubMed] [Google Scholar]
- 3.Hiday VA. Outpatient commitment: the state of empirical research on its outcomes. Psychology, Public Policy, and Law. 2003;9:8–32. doi: 10.1037/1076-8971.9.1-2.8. [DOI] [PubMed] [Google Scholar]
- 4.Phelan JC, Sinkewicz M, Castille DM, et al. Effectiveness and outcomes of assisted outpatient treatment in New York State. Psychiatric Services. 2010;61:137–143. doi: 10.1176/ps.2010.61.2.137. [DOI] [PubMed] [Google Scholar]
- 5.Swartz MS, Wilder CM, Swanson JW, et al. Assessing outcomes for consumers in New York’s assisted outpatient treatment program. Psychiatric Services. 2010;61:976–981. doi: 10.1176/ps.2010.61.10.976. [DOI] [PubMed] [Google Scholar]
- 6.Skeem JL, Manchak S, Peterson JK. Correctional policy for offenders with mental illness: creating a new paradigm for recidivism reduction. Law and Human Behavior. 2011;35:110–126. doi: 10.1007/s10979-010-9223-7. [DOI] [PubMed] [Google Scholar]
- 7.Pollack DA. SMA 04-3869. Rockville, Md: Substance Abuse and Mental Health Services Administration, Center for Mental Health Services; 2004. Moving From Coercion to Collaboration in Mental Health Services. [Google Scholar]
- 8.Steadman HJ, Gounis K, Dennis D, et al. Assessing the New York City involuntary outpatient commitment pilot program. Psychiatric Services. 2001;52:330–336. doi: 10.1176/appi.ps.52.3.330. [DOI] [PubMed] [Google Scholar]
- 9.Swartz M, Swanson J, Hiday V, et al. A randomized controlled trial of outpatient commitment in North Carolina. Psychiatric Services. 2001;52:325–329. doi: 10.1176/appi.ps.52.3.325. [DOI] [PubMed] [Google Scholar]
- 10.Swartz MS. Introduction to the special section on assisted outpatient treatment in New York State. Psychiatric Services. 2010;61:967–969. doi: 10.1176/ps.2010.61.10.967. [DOI] [PubMed] [Google Scholar]
- 11.Gilbert AR, Moser LL, Van Dorn RA, et al. Reductions in arrest under assisted outpatient treatment in New York. Psychiatric Services. 2010;61:996–999. doi: 10.1176/ps.2010.61.10.996. [DOI] [PubMed] [Google Scholar]
- 12.Hanley JA, Negassa A, Edwardes MD, et al. Statistical analysis of correlated data using generalized estimating equations: an orientation. American Journal of Epidemiology. 2003;156:364–375. doi: 10.1093/aje/kwf215. [DOI] [PubMed] [Google Scholar]
- 13.Allison PD. Fixed Effects Regression Methods for Longitudinal Data Using SAS. Cary, NC: SAS Institute; 2005. [Google Scholar]
- 14.Link BG, Phelan JC, Bresnahan M, et al. Public conceptions of mental illness: labels, causes, dangerousness, and social distance. American Journal of Public Health. 1999;89:1328–1333. doi: 10.2105/ajph.89.9.1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang LH, Wonpat-Borja AJ, Opler M, et al. Potential stigma associated with inclusion of the psychosis risk syndrome in the DSM-V: an empirical question. Schizophrenia Research. 2010;120:42–48. doi: 10.1016/j.schres.2010.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Monahan J, Bonnie RJ, Appelbaum PS, et al. Mandated community treatment: beyond outpatient commitment. Psychiatric Services. 2001;52:1198–1205. doi: 10.1176/appi.ps.52.9.1198. [DOI] [PubMed] [Google Scholar]
- 17.Watson AC, Angell B. Applying procedural justice theory to law enforcement’s response to persons with mental illness. Psychiatric Services. 2007;58:787–793. doi: 10.1176/ps.2007.58.6.787. [DOI] [PubMed] [Google Scholar]
- 18.Link BG, Castille DM, Stuber J. Stigma and coercion in the context of outpatient treatment for people with mental illnesses. Social Science and Medicine. 2008;67:408–419. doi: 10.1016/j.socscimed.2008.03.015. [DOI] [PubMed] [Google Scholar]


