Abstract
Jejunal diverticulosis is usually an asymptomatic condition characterized by herniation of mucosa through sites of weakening on the mesenteric border of the jejunum, leading to variable number of discrete outpouchings from the bowel. They are usually discovered incidentally on imaging or surgery done for some other reason. Complications such as diverticulitis with perforation and bowel obstruction and life-threatening gastrointestinal bleeding are rare. Our review highlights the correlation between radiological and surgical findings in 2 different cases of complicated jejunal diverticulitis. Both of the cases were successfully managed surgically.
Keywords: Jejunal diverticulosis, Complications, Perforation, Gastrointestinal bleeding
Introduction
Diverticular disease, also termed as “disease of western civilization,” was first described by Soemmerring in 1794 and later by Astley Cooper in 1809. In 1906, Gordinier and Shil performed the first operation for diverticulum [1]. Diverticulum is a sac-like protrusion in the wall of any portion of the gastrointestinal (GI) tract and is called real diverticula when composed of all layers of intestine and false diverticula when composed of only the mucosa and submucosa. In the small bowel duodenum is the most common site followed by jejunum and ileum, with duodenum diverticula almost 5 times more common than jejunoileal diverticula. Jejunoileal diverticula are seen in the sixth and seventh decades [2], with a male predominance of 1.5:1, whereas duodenal diverticular disease occurs after the fifth decade of life, with equal predominance among men and women [3].
Case reports
Case 1
A 68 year old man ,under treatment for polycythemia vera for last two years, presented to the emergency department with history of pain in the abdomen especially after taking meals and decreased frequency of stools for 5-6 days' duration, with pain increasing in severity for last 24 hours and with absolute constipation. On per abdomen examination, the abdomen was distended with diffuse tenderness all over. Laboratory tests were insignificant except for raised total leukocyte count. X-ray of the abdomen (Fig. 1) showed dilated small bowel loops with air fluid levels consistent with small bowel obstruction. Multidetector computed tomography (MDCT) was advised and showed dilated jejunal loops with multiple outpouchings arising from the mesenteric side of the jejunum, suggestive of diverticula (Fig. 2A-D). An adhesion band was seen causing internal hernia with resultant intestinal obstruction, a finding seen on retrospective imaging. The adhesion band formed a bridge between band and mesentery through which 2 thick, narrowed loops of jejunal segment were seen traversing (Fig. 3A-D) with significant stranding, and increased attenuation of the adjoining mesenteric fat was seen. A few small mesenteric lymph nodes were also seen (Fig. 2, Fig. 3). There was also short segment thrombosis of superior mesenteric artery (SMA) (Fig. 4A-C) at its origin, which also led to some diagnostic dilemma of whether the cause of thick narrowed jejunal segment is inflammatory only or caused by ischemic bowel with superadded inflammation. No evidence of any free air seen on computed tomography imaging was suggestive of perforation. Surgical exploration showed dilated jejunal loops with multiple jejunal diverticula. One perforated inflamed mid-jejunal diverticulum and an adhesion band was also seen during surgery with significant inflammatory changes in the adjoining mesentery and reactive mesenteric lymph nodes. The adhesion band was causing internal herniation of small bowel through a bridge formed between adhesion band and mesentery with resultant intestinal obstruction (Fig. 5A-D). Vascularity was normal, wedge excision and closure of perforated diverticula was done, and adhesion band was released. Perforation may have occurred while the patient was managed conservatively, as no signs of perforation could be seen, even on retrospective analysis of preoperative imaging. Nothing was done for SMA thrombosis as bowel vascularity was normal.
Fig. 1.

Ray abdomen showing multiple dilated small bowel loops with air fluid levels consistent with small bowel intestinal obstruction.
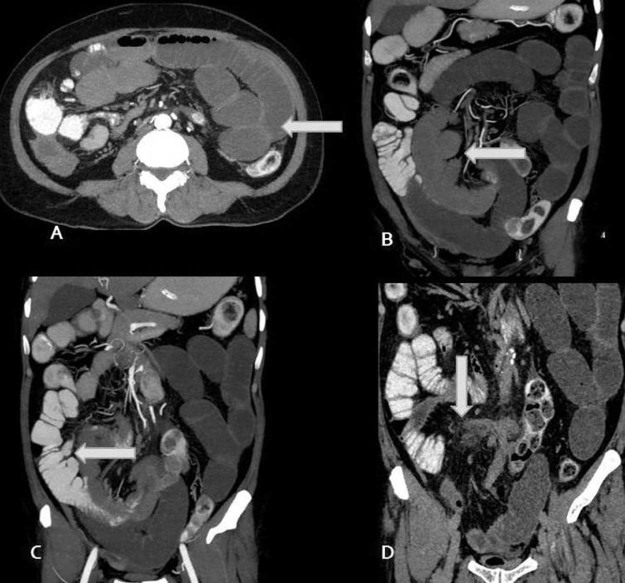
Fig. 2.
(A-D) Axial image (A) showing dilated jejunal loops (arrow) with coronal images (B-C) showing multiple variable-sized outpouchings from mesenteric side of dilated jejunal loops representing the diverticula (arrows) and last coronal image (D) showing inflammatory changes in the mesentery (arrow) in the form of high attenuation and marked stranding of mesenteric fat with small mesenteric lymph nodes. Adhesion band and adjoining thick narrowed small bowel jejunal loops can also be seen in the last image.
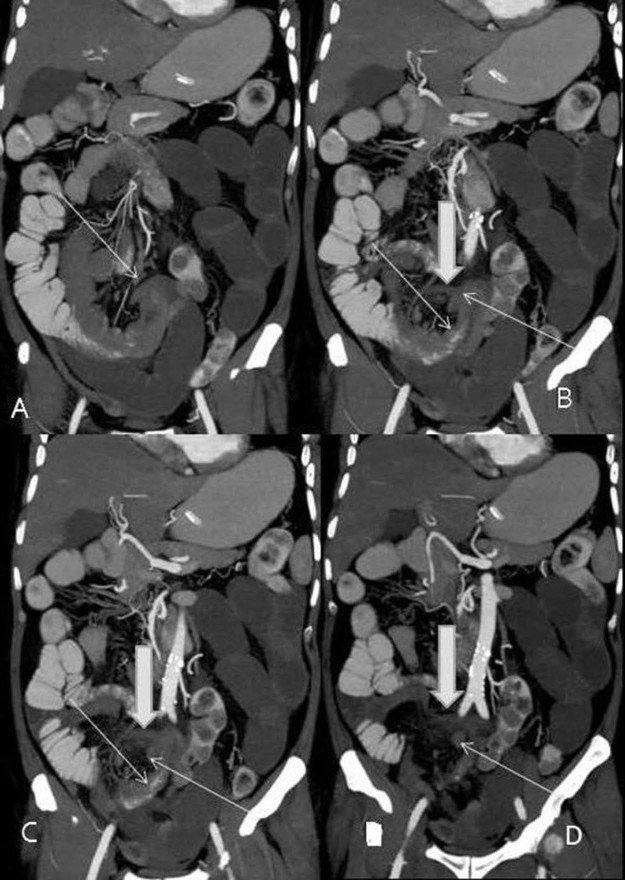
Fig. 3.
(A-D) Coronal CT images nicely showing adhesion band (wide arrows in B-D) forming a tunnel through which thick narrowed 2 loops of jejunal segment (thin arrows) can be seen traversing, indicating internal hernia leading to small bowel obstruction. Surrounding mesentery shows significant inflammatory changes (C, D, adjoining wide arrows).
CT, computed tomography.
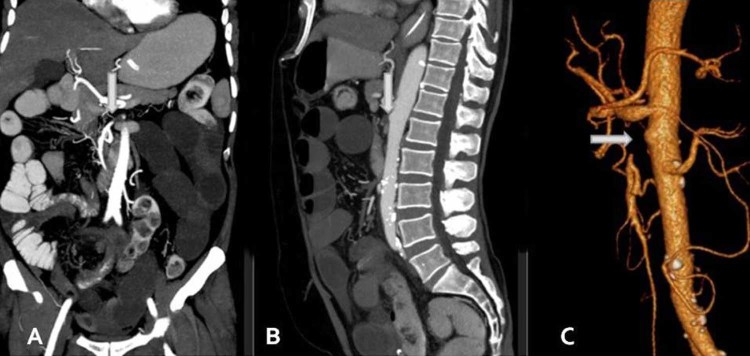
Fig. 4.
(A-C) Coronal, sagittal, and 3D volume-rendering images show short segment occlusion of SMA (arrows) at its origin due to thrombus.
SMA, superior mesenteric artery.
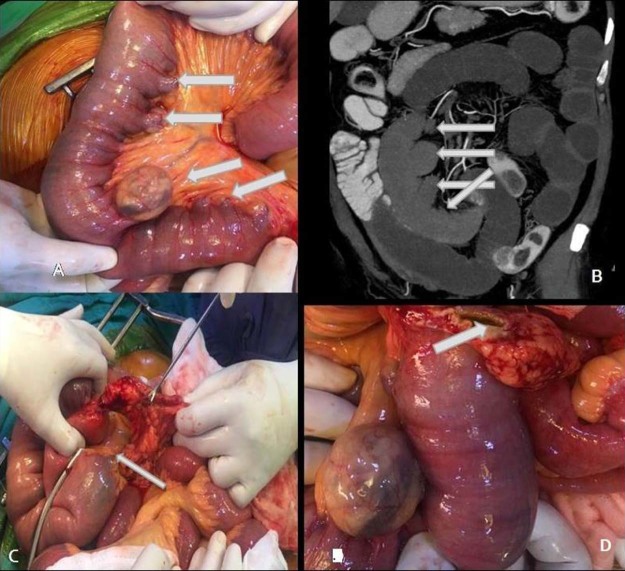
Fig. 5.
(A-D) Intraoperative image (A) shows multiple diverticula (arrows) arising from the mesenteric side of jejunal loops and almost corresponding coronal CT images (B) for comparison. Intraoperative image (C) shows adhesion band-forming tunnel (arrow) between mesentery and adhesion band with herniation of jejunal loops through this, and image D shows perforated diverticulum (arrow).
Case 2
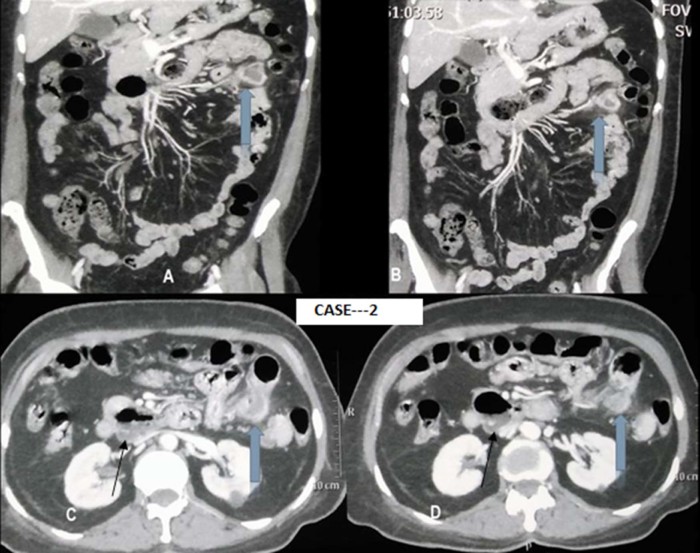
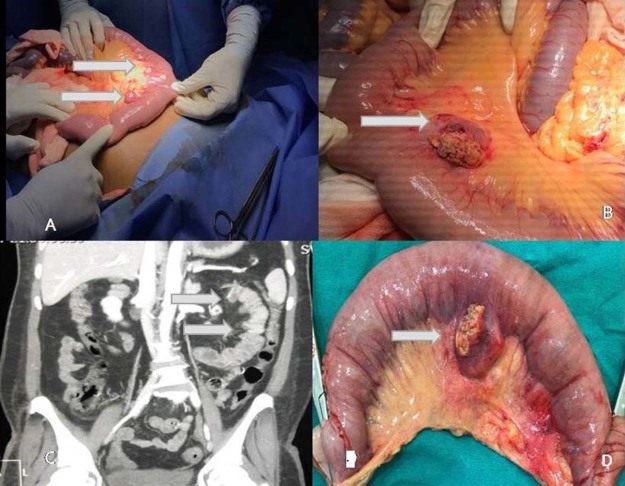
A 60-year-old woman presented to the emergency department with clinical features of melena for the previous 7 days, which slowly increased in severity for the last 3 days, and had features of shock with blood pressure of 68/40 mm Hg, heart rate of 130 beats per minute, respiratory rate of 24/minute, and oxygen saturation of 94% at time of presentation. Patient was also a known case of type 2 diabetes mellitus for the last 10 years and had percutaneous transluminal angioplasty 3 years back for acute coronary syndrome. Physical examination revealed severe pallor and pedal edema with mild abdominal tenderness. Laboratory tests showed decreased hemoglobin (7.2 g/dL) and raised total leukocyte count (15,300) with predominance of neutrophils. Upper GI endoscopy was normal with no evidence of varices. Contrast-enhanced computed tomography abdomen showed multiple outpouchings arising from the mesenteric border of jejunum with one of them in the left hypochondriac region showing features of inflammation with increased attenuation and significant fat stranding of the adjoining mesentery with formation of small inflammatory mass (Fig. 6A-D). The patient was planned for emergency surgery. Four units of packed red blood cells and fresh frozen plasma were transfused preoperatively. Midline laparotomy confirmed the radiological findings and showed multiple diverticula. Large inflamed diverticula of approximately 4 cm and a small inflammatory mass was seen in the left hypochondriac region. Dense adhesions with omentum and gut were seen in the left upper and infracolic quadrant. Another diverticulum was seen arising from the posterior aspect of third part of duodenum. No any other cause of bleeding seen on laparotomy (Fig. 7A-D).
Fig. 6.
(A-D) CECT images show (wide arrows) inflamed jejunal diverticulum with formation of inflammatory mass showing peripheral enhancing wall with adjoining mesentery showing increased attenuation and significant stranding. Axial CECT image B (thin arrow) shows D3 duodenum diverticulum.
CECT, contrast-enhanced computed tomography.
Fig. 7.
(A-D) Surgical pictures showing multiple small jejunal diverticula (A) with CT images for comparison (C). Intraoperative picture (B) and postsurgical resected jejunal segment (D) containing inflamed diverticulum.
CT, computed tomography.
Discussion
Small bowel diverticulosis was first described by Baillie and von Soemmerring in 1794 and Cooper first described jejunal diverticulosis in 1807 [4]. Diverticulosis involves the large intestine more commonly than the small bowel, with reported incidence of small bowel diverticulosis being 0.6%-2.3% in autopsy series [5] and with reported radiological incidence of 2.3% [6]. In the small bowel, duodenum is the most common site of diverticulosis followed by the jejunum and the ileum. Diverticulum is more frequent in the jejunum than in the ileum due to greater diameter of penetrating jejunal artery [7]. The proposed etiopathogenesis of small bowel diverticulosis is abnormalities in intestinal peristalsis, intestinal dyskinesia, and very high intraluminal pressure, with diverticulum arising at the site where mesenteric vessels enter into the muscular layer of the small intestine [7], [8]. It has also been hypothesized that vegetarian diet and a high intake of dietary fiber lowers the risk of diverticular disease, as this diet leads to rapid bowel transit time, causing less water to be reabsorbed from the lower GI tract resulting in larger, softer stools that are easier to pass; this in turn could lead to a lower intraluminal pressure and a reduced likelihood of pouches or bulges formation through the weakened intestinal wall that are characteristic of diverticula [9].
The diverticulosis is usually asymptomatic in approximately 42% cases, and is detected incidentally on imaging done for some other reasons. Diarrhea and chronic pain are present in 40% cases, whereas 18% of cases present with emergency complications, half of which require surgical intervention [10]. Complications such as malabsorption, diverticulitis, obstruction, abscess formation, and rarely, diverticular perforation or hemorrhage have been reported in 10%-30% of patients [11], with mortality rates associated with these acute complications ranging from 25% to 50% [12].
In radiological evaluation of complications of diverticulosis, abdominal x-ray may show air fluid level and free intraperitoneal air. MDCT with oral and IV contrast is highly sensitive for assessment of various complications and is superior for demonstrating the mural, serosal, and mesenteric extent of the disease.
On MDCT, diverticula appear as a discrete round or ovoid, air-containing outpouching from lumen of the small bowel, with a smooth, barely discernible wall and no recognizable small-bowel folds.
Inflamed diverticula, called diverticulitis, typically show nonspecific changes that are consistent with inflammation and infection. Frequent findings seen in diverticulitis are an inflammatory mass, which may contain gas; wall thickening of an involved segment; edema of the surrounding tissues; and fluid collection [5], [12].
Abscess formation is seen as fluid collection with enhancing walls and may show air in it on MDCT imaging [5].
Perforation, one of the most severe complications of jejunal diverticula with a mortality rate of up to 40% [12], [13], may result in free air in peritoneal cavity or it may be contained within an interloop abscess. Underlying necrotic tumor may also have this appearance and should always be considered [5], [14].
Usually, bowel ischemia of arterial origin shows a thinning of bowel wall, although there can be wall thickening in case of reperfusion and lumen may be filled with fluid, gas, or both, and there can be surrounding inflammatory changes in case of superadded infection [15]. Our case also showed thickening of involved segment with associated short segment SMA thrombosis at its origin, which raised doubt if there is associated ischemic etiology, although no bowel ischemia was seen preoperatively. Polycythemia vera predisposes to thrombotic state [16], which is also a likely cause of SMA thrombosis in our case.
Mechanical intestinal obstruction, another complication of diverticulitis, has reported incidence of approximately 2.3%-4.6% [17], which may occur as a result of adhesion band formation due to inflammation, or obstruction can be due to extrinsic compression from an adjoining bowel loop with large diverticulum or from intussusception. Obstruction can be secondary to enterolith as an acidic environment within the diverticulum is ideal for metabolism of bile salts to choleic acid, hence enterolith obstruction [5], [6], [14], [15], [18]. Our first case also presented with intestinal obstruction due to internal herniation of jejunal loops caused by an adhesion band which most likely formed due to previous episodes of diverticulitis.
GI bleeding from jejunal diverticulosis, first reported by a British surgeon, Dr L.R. Braithwaite in 1923, has a reported incidence of approximately 3.4%-8.1%, although severe GI bleeding secondary to jejunal diverticulosis is rare, with 1 study quoting approximately 50 cases reported in the literature to date [19]. Hemorrhage can be due to ulceration or foreign body impaction [5]. Our second case presented with life-threatening upper GI bleeding due to complicated jejunal diverticulitis, with preoperative MDCT imaging helping the surgeon to provide a roadmap for the surgery.
To conclude, our study describes and highlights the role of preoperative imaging of 2 uncommon complications of jejunal diverticulitis which were managed successfully. A preoperative accurate diagnosis of the complications of diverticulitis helps in better surgical planning and thus helps in better patient management.
Acknowledgment
Special thanks to Dr. Rakesh Kumar and Dr. MP Singh for providing surgical images in case 1 and case 2, respectively.
Footnotes
Competing Interest: The authors have declared that no competing interests exist.
Research involving human participants or animals: This is a case report and no trial on humans or animals was done.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
Source of Funding: This is a case study, and no funding was required.
References
- 1.Igwe P.O., Ray-Offor E., Allison A.B., Alufohai E.F. Volvulus complicating jejunal diverticulosis: a case report. Int J Surg Case Rep. 2015;9:61–64. doi: 10.1016/j.ijscr.2015.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Akhrass R., Yaffe M.B., Fischer C., Ponsky J., Shuck J.M. Small-bowel diverticulosis: perceptions and reality. J Am CollSurg. 1997;184:383. [PubMed] [Google Scholar]
- 3.Weizman A.V., Nguyen G.C. Diverticular disease: epidemiology and management. Can J Gastroenterol. 2011;25(7):385–389. doi: 10.1155/2011/795241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kwak J.Y., Park E.H., Park C.S., Kim J.H., Han M.S., Kwak J.H. Uncomplicated jejunal diverticulosis with pneumoperitoneum. Ann Surg Treat Res. 2016;90(6):346–349. doi: 10.4174/astr.2016.90.6.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coulier B., Maldague P., Bourgeois A., Broze B. Diverticulitis of the small bowel: CT diagnosis. Abdom Imaging. 2007;32:228–233. doi: 10.1007/s00261-006-9045-8. [DOI] [PubMed] [Google Scholar]
- 6.Patel V.A., Jefferis H., Spiegelberg B., Iqbal Q. Jejunal diverticulosis is not always a silent spectator: a report of 4 cases and review of the literature. World J Gastroenterol. 2008;14(38):5916–5919. doi: 10.3748/wjg.14.5916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ferreira-Aparicio F.E., Gutiérrez-Vega R., Gálvez-Molina Y., Ontiveros-Nevares P., Athie-Gútierrez C., Montalvo-Javé E.E. Diverticular disease of the small bowel. Case Rep Gastroenterol. 2012;6:668–676. doi: 10.1159/000343598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hobson K.G., Roberts P.L. Etiology and pathophysiology of diverticular disease. Clin Colon Rectal Surg. 2004;17(3):147–153. doi: 10.1055/s-2004-832695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Crowe F.L., Appleby P.N., Allen N.E., Key T.J. Diet and risk of diverticular disease in Oxford cohort of European Prospective Investigation into Cancer and Nutrition (EPIC): Prospective study of British vegetarians and non-vegetarians. BMJ. 2011;343:d4131. doi: 10.1136/bmj.d4131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tsiotos G.G., Farnell M.B., Ilstrup D.M. Nonmeckelianjejunal or ileal diverticulosis: an analysis of 112 cases. Surgery. 1994;116:726. [PubMed] [Google Scholar]
- 11.Falidas E., Vlachos K., Mathioulakis S., Archontovasilis F., Villias C. Multiple giant diverticula of the jejunum causing intestinal obstruction: report of a case and review of the literature. World J Emerg Surg. 2011;6:8. doi: 10.1186/1749-7922-6-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kirbaş I., Yildirim E., Harman A., Başaran Ö. Perforated ileal diverticulitis: CT findings. Diagn Interv Radiol. 2007;13:188–189. [PubMed] [Google Scholar]
- 13.Okino Y., Kiyosue H., Mori H., Komatsu E., Matsumoto S., Yamada Y. Root of the small-bowel mesentery: correlative anatomy and CT features of pathologic conditions. Radiographics. 2001;21:1475–1490. doi: 10.1148/radiographics.21.6.g01nv121475. [DOI] [PubMed] [Google Scholar]
- 14.Fintelmann F., Levine M.S., Rubesin S.E. Jejunal diverticulosis: findings on CT in 28 patients. AJR Am J Roentgenol. 2008;190:1286–1290. doi: 10.2214/AJR.07.3087. [DOI] [PubMed] [Google Scholar]
- 15.Furukawa A., Kanasaki S., Kono N., Wakamiya M., Tanaka T., Takahashi M. CT diagnosis of acute mesenteric ischemia from various causes. AJR Am J Roentgenol. 2009;192(2):408–416. doi: 10.2214/AJR.08.1138. [DOI] [PubMed] [Google Scholar]
- 16.Kroll M.H., Michaelis L.C., Verstovsek S. Mechanisms of thrombogenesis in polycythemia vera. Blood Rev. 2015;29:215–221. doi: 10.1016/j.blre.2014.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nejmeddine A., Bassem A., Mohamed H., Hazem B.A., Ramez B., Issam BM. Complicated jejunal diverticulosis: a case report with literature review. N Am J Med Sci. 2009;1(4):196–199. [PMC free article] [PubMed] [Google Scholar]
- 18.Hayee B., Khan H.N., Al-Mishlab T., McPartlin J.F. A case of enterolith small bowel obstruction and jejunal diverticulosis. World J Gastroenterol. 2003;9:883–884. doi: 10.3748/wjg.v9.i4.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abegunde A.T., Christman E., Hassell L.A., Kastens D. Rare jejunal diverticular bleeding. ACG Case Rep J. 2016;3(4) doi: 10.14309/crj.2016.119. [DOI] [PMC free article] [PubMed] [Google Scholar]