Summary
Working with virological samples requires validated inactivation protocols for safe handling and disposal. Although many techniques exist to inactivate samples containing viruses, not all procedures have been properly validated or are compatible with subsequent assays. To aid in the development of inactivation protocols for Alphaviruses, and specifically Venezuelan equine encephalitis virus (VEEV), a variety of methods were evaluated for their ability to completely inactivate a high titer sample of the vaccine strain VEEV TC-83. The methods evaluated include reagents used in RNA extraction, fixation, treatment with a detergent, and heat inactivation. Most methods were successful at inactivating the sample; however, treatment with only Buffer AVL, SDS, and heat inactivation at 58°C for one hour were not capable of complete inactivation of the virus in the sample. These results provide a substantial framework for identifying techniques that are safe for complete inactivation of Alphaviruses and to advise protocol implementation.
Keywords: Virus inactivation, Venezuelan equine encephalitis virus, Alphavirus
Working with infectious agents requires inactivation to safely perform downstream procedures. This is especially important when working with viruses that are categorized as Biosafety level 3 (BSL3) agents or above. Inactivation of BSL3 agents is essential for many techniques and has significant safety implications if these procedures are not validated. In addition, the recent Division of Select Agents and Toxins (DSAT) regulations for select agents have mandated that inactivation procedures must be verified (Centers for Disease Control and Prevention, 2017). Here we present data that validates the inactivation and provides a blueprint for successful inactivation of Venezuelan equine encephalitis virus (VEEV) for which some strains are classified as select agents, as well as for other important Alphavirus pathogens.
While there are many methods to inactivate a pathogen, not all protocols are appropriate for downstream uses. Techniques for diagnostics or research may require an intact genome or structural proteins. For this reason, specific reagents have become widely used in virology. RNA extraction is often performed using Qiagen kits (Blow et al., 2008) or TRIzol (Hofmann et al., 2000) and proteins are preserved by formalin (Mussgay and Weiland, 1973; Tiwari et al., 2009) or methanol-acetone (Fauvel and Ozanne, 1989). These reagents can inactivate a wide range of viruses, but these need to be validated for each group of viruses. Protocols for inactivation of VEEV have been previously reported for RNA extraction reagents (Blow et al., 2004; Kochel et al., 2017). Other methods for fixation, and heat inactivation have not been reported for VEEV and are also not widely reported for other Alphaviruses. VEEV is an enveloped, single-stranded RNA virus in the genus Alphavirus, family Togaviridae and are classified as BSL3 with the exception of the vaccine strain TC-83. VEEV TC-83, which was used here, is derived from the select agent strain Trinidad Donkey and is, therefore, an appropriate substitute for this important family of viruses. VEEV TC-83 differs from Trinidad Donkey strain by 12 mutations, including 8 in the structural genes (Kinney et al., 1993). The structure of TC-83 does not suggest a significant deviation from Trinidad Donkey strain (Zhang et al., 2011). The attenuating structural mutation at E2–120, a switch from a neutral to positive residue, likely improves infection in cell culture because of selection for heparin sulfate binding (Klimstra et al., 1998). The same mutation consequently attenuates in vivo because of binding negatively charged molecules that interfere with spread (Byrnes and Griffin, 2000). One additional benefit is that TC-83 typically grows to a log higher than most Alphaviruses, so this also increases the effectiveness of this strain as a surrogate. VEEV is responsible for several outbreaks that have occurred in central and South America. In addition, the recent outbreaks of chikungunya virus have brought the need for Alphavirus inactivation to the fore to facilitate the safe sharing of samples.
To test inactivation protocols, VEEV TC-83 rescued in baby hamster kidney cells and passaged twice in African green monkey kidney (Vero) (American Type Culture Collection) cells was used for infections and all experiments were performed in BSL2 facilities. Virus stock was diluted to infect Vero cells at an MOI of 1 in Dulbecco’s modified Eagle medium (DMEM) (Gibco) with 10% fetal bovine serum (FBS) (Atlanta Biologicals) and 0.05 mg/mL gentamycin (Corning). Cells were incubated with inoculated media at 37°C for 24 hours. Media was aspirated from the cells and clarified by centrifugation at 1176 × g for 5 min. Cells were washed with PBS (Gibco), scraped from the surface, and added to a 1.5 mL microcentrifuge tube. Cells were pelleted by centrifugation at 188 × g for 5 min and the PBS was removed. Virus titers of the clarified media and washed cells were determined by plaque assay, using a previously described method (Beaty et al., 1995). Briefly, samples were serially diluted, and incubated with Vero cells for one hour before overlay with DMEM containing 2% FBS, 0.4% agarose and gentamycin. Plaques were allowed to develop for 48 hours at 37°C. Samples were fixed with 10% formalin (Fisher Scientific), and stained with 0.25% crystal violet solution (Fisher Scientific).
Protocols regularly used during RNA isolation, fixation, or inactivation of contaminated or infected samples were selected to evaluate their ability to inactivate VEEV TC-83. Clarified media was used for inactivation steps of RNA extraction protocols with Qiagen (QIAamp Viral RNA Mini Kit, Qiagen), Clontech (NucleoSpin Virus, Clontech), and TRIzol (TRIzol Reagent, Ambion) reagents. The buffers from Qiagen and Clontech, Buffer AVL and Buffer VL, respectively, contain guanidine hydrochloride, a chaotrope often used for denaturing proteins. TRIzol also contains a chaotrope, guanidinium thiocyanate, for protein denaturation. Manufacturer’s protocols were followed for incubation time, temperature, sample, and reagent amounts. Following the manufacturer’s protocol, sample volume was adjusted to 1 mL with DMEM with 10% FBS, where possible. Brief protocols are described in Table 1. Washed cells from 1 well of a 6-well plate were resuspended in 500 μL of 0.1% sodium dodecyl sulfate (SDS) (Corning), 10% formalin (Fisher Scientific), or methanol-acetone (Fisher Scientific). Methanol-acetone was mixed at a 1:1 ratio and stored at −20°C. Following the 30 min incubation, 500 μL of DMEM with 10% FBS was added to samples treated with 0.1% SDS, 10% formalin and methanol-acetone. Cells with 10% formalin and methanol-acetone were pelleted by centrifugation at 188 × g for 5 min. The supernatant was removed and cells were resuspended in 500 μL of DMEM with 10% FBS. Heat inactivation was performed with a heat block monitored with a thermometer on 500μL stock samples that contained 9.75 × 108 pfu. After exposure to 58°C (+/− 2°C) or 80°C (+/− 1°C) for 1 hour, 1 × 108 pfu was mixed with 5 mL of 2% FBS DMEM and added to Vero cells in T25 flasks. Protocols were performed in triplicate.
Table 1.
Brief inactivation protocols for each condition by time, temperature, and virus titer.
| Condition | Temperature (°C) | Time (min) | Sample (pfu) |
|---|---|---|---|
| Qiagen AVL | 21 | 10 | 1.47 × 109 |
| Qiagen AVL + ethanol | 21 | 10 | 1.47 × 109 |
| Clontech Nucleospin Virus | 21 | 8 (5 min - Buffer VL, 3 min - ethanol) | 2.1 × 109 |
| TRIzol | 21 | 5 | 1 × 108 |
| 0.1% SDS | 21 | 30 | 2.534 × 109 |
| 10% Formalin | 4 | 30 | 2.534 × 109 |
| 21 | 30 | 2.534 × 109 | |
| 37 | 30 | 2.534 × 109 | |
| Methanol/Acetone | 4 | 30 | 2.534 × 109 |
| 21 | 30 | 2.534 × 109 | |
| 37 | 30 | 2.534 × 109 | |
| Heat inactivation | 58 | 60 | 1 × 108 |
| 80 | 60 | 1 × 108 |
Samples inactivated in Qiagen Buffer AVL with or without ethanol, 0.1% SDS, 10% formalin and methanol-acetone were dialyzed (Float-A-Lyzer G2 MWCO: 3.5–5 kDa, Spectra/Por) in PBS to remove the toxic reagents. Due to the toxicity of the reagents used in chemical inactivation, inactivated samples cannot be applied directly to cells for analysis. Samples must be dialyzed or washed to maintain cell viability. Dialysis was performed overnight at room temperature with a complete buffer change. Additional positive control samples were dialyzed that were not treated with an inactivation procedure. These contained VEEV TC-83 in tenfold dilutions at titers of 1 × 105 pfu down to 1 × 101 pfu.
Due to the use of proteinase K in the protocol, Clontech Buffer VL treated samples were washed with 10 mL of PBS in centrifugal concentrators (Amicon Ultra MWCO: 100 kDa; Millipore). Due to the incompatibility of TRIzol with the dialysis membrane, TRIzol treated samples were washed with 25 mL of PBS in centrifugal concentrators (Amicon Ultra MWCO: 10 kDa, Millipore). All samples inactivated by Clontech Buffer VL and TRIzol were concentrated to a final volume of less than 1 mL.
All samples were added to 5 mL of DMEM with 2% FBS, applied to Vero cells in a T25 flask and incubated at 37°C for 4 days. Flasks were monitored daily for cytopathic effect (CPE). Samples that showed no evidence of CPE were passaged a second time to confirm the absence of CPE and the full inactivation of the sample. The first passage of supernatant was clarified by centrifugation at 1176 × g for 5 min. Clarified media was mixed 1:1 with fresh DMEM with 2% FBS, and 5 mL was added to a second passage of Vero cells. Conditions suspected to be toxic to cells were confirmed for presence of virus by titration on Vero cells in standard plaque assays (Beaty et al., 1995). Observation of plaques would indicate active virus in the sample, while widespread CPE would signal the presence of toxic reagents that require further dilution or exchange.
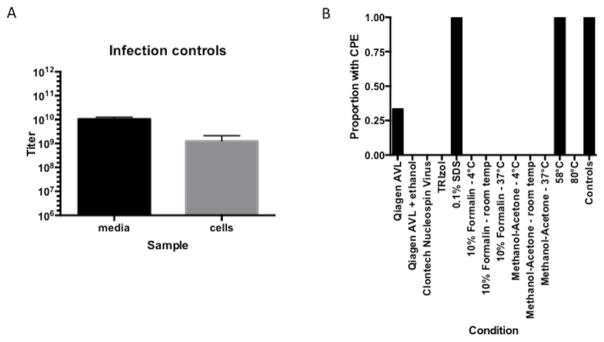
Cells inoculated with the stock VEEV TC-83 had CPE following 24 hours of incubation. The titer of the clarified media was 1.05 × 1010 pfu/mL, and the titer of the washed cells was 1.267 × 109 pfu/mL (Figure 1A). Positive control samples (dialyzed, untreated virus samples) from 1 × 105 to 1 × 101 pfu, were all positive for CPE in the first passage on Vero cells. These samples were able to demonstrate that the dialysis process and level of detection are sensitive and appropriate for the titers used in the inactivation protocols.
Figure 1.
The virus titer, and proportion of cytopathic effect (CPE) in each condition. A) The titer of virus produced in samples from media and Vero cells from infections with an MOI of 1 for 24 hours. B) The proportion of flasks with visible CPE from each condition. Control samples include 5 untreated, dialyzed samples serially diluted from 1 × 105 pfu to 1 × 101 pfu.
Using media that contained a high titer of VEEV TC-83 to evaluate common methods used in RNA extraction inactivated virus in most samples. Samples inactivated only with Qiagen Buffer AVL showed CPE in one out of three replicates (Figure 1B). A plaque assay confirmed the result. An additional step of the Qiagen protocol, which includes addition of ethanol, led to the inactivation of all replicates. A previous study reported the inactivation of VEEV 68U201, an endemic BSL3 strain, with Qiagen Buffer AVL only (Blow et al., 2004). The current study evaluated three experimental replicates, rather than technical replicates from a single sample, which revealed an inconsistency in the reagent’s ability to inactivate VEEV strains. The use of a higher virus titer, and differences in strain may also cause the discrepancies for inactivation. Although the differences in experiments may lead to different outcomes, these results add to a growing list of viruses, including Ebola virus, West Nile virus, and chikungunya virus, which are not effectively inactivated with only Qiagen Buffer AVL (Ngo et al., 2017; Smither et al., 2015). For this reason, the addition of ethanol to Qiagen Buffer AVL for complete inactivation of virus is recommended for the safe use of the sample or removal from high containment.
Successful inactivation of the entire virus sample was seen with Clontech NucleoSpin Virus and TRIzol protocols. Cell lysis was seen in two of the samples inactivated using Clontech Buffer VL with proteinase K; however, these were due to remaining toxic reagents rather than active virus, as confirmed by plaque assay. Inactivation of VEEV by TRIzol has also been confirmed in multiple previous reports (Blow et al., 2004; Kochel et al., 2017).
Infected cells treated with reagents common for fixation, 10% formalin and methanol-acetone, were all completely inactivated. These included incubation temperatures of 4°C, 21°C, and 37°C. Both reagents are widely used in preparation for microscopy, and their ability to successfully inactivate VEEV in cells was expected, although low concentrations of formaldehyde have been shown ineffective against yellow fever virus (Goodman et al., 2014). Glutaraldehyde is a more reactive crosslinker than formaldehyde, and may be used at concentrations as low as 0.1% to inactivate very high titers of Sindbis virus, another Alphavirus (Lawrence et al., 2016). The use of SDS to inactivate many types of virus samples has been recommended in previous protocols (Haddock and Feldmann, 2017; Howett et al., 1999). While the cells infected with VEEV were lysed following exposure to 0.1% SDS, the samples continued to be infective for all replicates. This differs from treatment of hepatitis C virus (HCV), which was successfully inactivated by 0.1% SDS in media, inoculated human serum and intracellular samples (Song et al., 2010). Inactivation with SDS is known to differ between viruses, and may need to be supplemented with heat in some cases (Boatman, 1972; Helenius and Simons, 1975). Heat inactivation at 58°C (+/− 2°C) for 1 hour was not able to inactivate the virus and resulted in CPE in all flasks. The higher temperature of 80°C (+/− 1°C) for 1 hour was successful, as no CPE was observed. Again, these results differ from those seen in HCV where 40 min at 56°C was able to reduce the titer below detection (Song et al., 2010). The increased titer used in these experiments or greater resilience of VEEV TC-83 could be responsible for the inability of the lower temperature to inactivate the virus.
Although not all methods were able to reliably inactivate VEEV TC-83, several options are validated from these experiments. These options represent some of the most widespread techniques used in diagnostics and research, and can safely be used while maintaining the integrity of the sample for downstream analysis. The results also support the use of VEEV TC-83 as a surrogate for inactivation of more virulent strains of VEEV, although exact strains of interest should be used to confirm inactivation procedures, if feasible. Updated guidelines for the inactivation of select agents from the Centers for Disease Control and Prevention stipulate that a surrogate virus should have equivalent or more resistant properties than the specific agent for inactivation, and that more resistant strains should be used for procedure validation (Centers for Disease Control and Prevention, 2017). TRIzol inactivation was performed on VEEV TC-83 with equal success to previous reports using other VEEV strains, and TC-83 showed greater resistance to Qiagen Buffer AVL (Blow et al., 2004; Kochel et al., 2017). Thus, VEEV TC-83 has met the requirements for use as a surrogate, and can be used to validate other methods for virus inactivation. It should be noted that as with all regulatory procedures, more replicates will instill greater confidence in these methods, and validation should be confirmed on a regular basis. The successful protocols outlined in this study address the lack of reports for Alphavirus inactivation and can be used as a template for developing in-house protocols and support compliance to regulations.
Acknowledgments
Funding: This work was supported by the National Institutes of Health R01-AI095753-01A1 to NLF.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Beaty, Calisher, Shope, Lennette, Lennette, Lennette . Diagnostic procedures for viral, rickettsial and chlamydial infections. 7. American Public Health Association; Washington, DC: 1995. Arboviruses; pp. 189–212. [Google Scholar]
- Blow J, Dohm D, Negley D, Mores C. Virus inactivation by nucleic acid extraction reagents. J Virol Methods. 2004;119:195–198. doi: 10.1016/j.jviromet.2004.03.015. [DOI] [PubMed] [Google Scholar]
- Blow J, Mores C, Dyer J, Dohm D. Viral nucleic acid stabilization by RNA extraction reagent. J Virol Methods. 2008;150:41–44. doi: 10.1016/j.jviromet.2008.02.003. [DOI] [PubMed] [Google Scholar]
- Byrnes A, Griffin D. Large-Plaque Mutants of Sindbis Virus Show Reduced Binding to Heparan Sulfate, Heightened Viremia, and Slower Clearance from the Circulation. J Virol. 2000;74:644–651. doi: 10.1128/jvi.74.2.644-651.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Guidance on the Inactivation or Removal of Select Agents and Toxins for Future Use. 2017. [Google Scholar]
- Fauvel, Ozanne Immunofluorescence assay for human immunodeficiency virus antibody: investigation of cell fixation for virus inactivation and antigen preservation. J Clin Microbiol. 1989;27:1810–3. doi: 10.1128/jcm.27.8.1810-1813.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boatman S. In: The Generation of Subcellular Structures. Markham R, Bancroft JB, editors. North Holland Publishing Co.; Amsterdam: 1972. pp. 123–134. [Google Scholar]
- Goodman CH, Russell BJ, Velez JO, Laven JJ, Nicholson WL, Bagarozzi DA, Moon JL, Bedi Johnson BW. Development of an algorithm for production of inactivated arbovirus antigens in cell culture. J Virol Methods. 2014;208:66–78. doi: 10.1016/j.jviromet.2014.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddock E, Feldmann F. Methods in molecular biology. Clifton, N.J: 2017. Ebolaviruses. [DOI] [PubMed] [Google Scholar]
- Helenius A, Simons K. Solubilization of membranes by detergents. Biochimica Et Biophysica Acta Bba - Rev Biomembr. 1975;415:29–79. doi: 10.1016/0304-4157(75)90016-7. [DOI] [PubMed] [Google Scholar]
- Hofmann MA, Thür B, Liu L, Gerber M, Stettler P, Moser C, Bossy S. Rescue of infectious classical swine fever and foot-and-mouth disease virus by RNA transfection and virus detection by RT-PCR after extended storage of samples in Trizol®. 2000;87:29–39. doi: 10.1016/s0166-0934(00)00154-3. [DOI] [PubMed] [Google Scholar]
- Howett M, Neely E, Christensen N, Wigdahl B, Krebs F, Malamud D, Patrick S, Pickel M, Welsh P, Reed C, Ward M, Budgeon L, Kreider J. A broad-spectrum microbicide with virucidal activity against sexually transmitted viruses. 1999;43:314–21. doi: 10.1128/aac.43.2.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinney, Chang, Tsuchiya, Sneider, Roehrig, Woodward, Trent Attenuation of Venezuelan equine encephalitis virus strain TC-83 is encoded by the 5′-noncoding region and the E2 envelope glycoprotein. Journal of virology. 1993;67:1269–77. doi: 10.1128/jvi.67.3.1269-1277.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klimstra, Ryman, Johnston Adaptation of Sindbis virus to BHK cells selects for use of heparan sulfate as an attachment receptor. J Virol. 1998;72:7357–66. doi: 10.1128/jvi.72.9.7357-7366.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochel TJ, Kocher GA, Ksiazek TG, Burans JP. Evaluation of TRIzol LS Inactivation of Viruses. 2017;22:52–55. [Google Scholar]
- Lawrence R, Zook J, Hogue B. Full inactivation of alphaviruses in single particle and crystallized forms. J Virol Methods. 2016;236:237–244. doi: 10.1016/j.jviromet.2016.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mussgay, Weiland Preparation of Inactivated Vaccines against Alphaviruses Using Semliki Forest Virus-White Mouse as a Model. II. Evaluation of Formalin-Inactivated Vaccines Treated with Tri(n-Butyl)Phosphate and/or Saponin and Properties of the Inactivated Virus. Intervirology. 1973;1:269–277. doi: 10.1159/000148855. [DOI] [PubMed] [Google Scholar]
- Ngo K, Jones S, Church T, Fuschino M, George K, Lamson D, Maffei J, Kramer L, Ciota A. Unreliable Inactivation of Viruses by Commonly Used Lysis Buffers. Applied Biosafety. 2017 153567601770338. [Google Scholar]
- Smither S, Weller S, Phelps A, Eastaugh L, Ngugi S, O’Brien L, Steward J, Lonsdale S, Lever M. Buffer AVL Alone Does Not Inactivate Ebola Virus in a Representative Clinical Sample Type. Journal of Clinical Microbiology. 2015;53:3148–3154. doi: 10.1128/JCM.01449-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song H, Li J, Shi S, Yan L, Zhuang H, Li K. Thermal stability and inactivation of hepatitis C virus grown in cell culture. Virology Journal. 2010;7:1–12. doi: 10.1186/1743-422X-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiwari M, Parida M, Santhosh SR, Khan M, Dash P, Rao PV. Assessment of immunogenic potential of Vero adapted formalin inactivated vaccine derived from novel ECSA genotype of Chikungunya virus. Vaccine. 2009;27:2513–2522. doi: 10.1016/j.vaccine.2009.02.062. [DOI] [PubMed] [Google Scholar]
- Zhang R, Hryc C, Cong Y, Liu X, Jakana J, Gorchakov R, Baker M, Weaver S, Chiu W. 4.4 Å cryo-EM structure of an enveloped alphavirus Venezuelan equine encephalitis virus. Embo J. 2011;30:3854–3863. doi: 10.1038/emboj.2011.261. [DOI] [PMC free article] [PubMed] [Google Scholar]