Abstract
Objective
To determine the geographic accessibility of emergency departments (EDs) with high pediatric-readiness by assessing the percentage of US children living within 30-minute drive time of an ED with high pediatric readiness as defined by collaboratively-developed, published guidelines.
Study design
In this cross-sectional analysis, we examined geographic access to an ED with high pediatric readiness among US children. Pediatric readiness was assessed using the weighted pediatric readiness score (WPRS) of US hospitals based on the 2013 National Pediatric Readiness Project (NPRP) survey. A WPRS of 100 indicates that the ED meets the essential guidelines for pediatric readiness. Using estimated drive time from ZIP code centroids, we determined the proportion of US children living within 30-minute driving time of EDs with WPRS of 100 (maximum), 94.3 (90th percentile), and 83.6 (75th percentile).
Results
Although 93.7% of children could travel to any ED within 30 minutes, only 33.7% of children could travel within 30 minutes with WPRS of 100. Additionally, 55.3% of children could travel to an ED scoring ≥90th percentile WPRS, and 70.2% of children to an ED scoring ≥75th percentile WPRS. Among children within 30 minutes of an ED with the maximum WPRS, 90.9% lived closer to at least one alternative ED scoring below the maximum WPRS. Access varied across census divisions, ranging from 14.9% of children in the East South Center to 56.2% in the Mid-Atlantic for EDs scoring a maximum WPRS.
Conclusion
A significant proportion of US children do not have timely access to EDs with high pediatric readiness.
Keywords: access, geographic access, emergency department, pediatric-ready
When medical emergencies occur, children require timely access to care that is prepared for their unique needs.1 As outlined in guidelines collaboratively developed and sponsored by the American Academy of Pediatrics, American College of Emergency Physicians, and Emergency Nurses Association,2, 3 these needs include pediatric-specific equipment, medication, and supplies; staff with pediatric expertise; and pediatric-specific policies, procedures, and protocols. However, in prior work, only 59% of emergency departments (EDs) nationally were aware of pediatric guidelines,4 only 53.5% had written transfer agreements with a hospital with pediatric intensive care services,5 and only 23% had pediatric emergency physicians on staff.6 Such findings prompted efforts to improve the pediatric emergency care system over the last decade.7, 8
To understand current pediatric readiness of EDs, the 2013 National Pediatric Readiness Project (NPRP) assessment surveyed all US EDs on individual components of the published guidelines and developed a weighted pediatric readiness score (WPRS) to reflect the availability of pediatric-specific equipment, personnel, and processes.9 A WPRS of 100 indicated meeting the essential requirements for pediatric readiness, such that it is the target score recommended for all EDs. In the 2013 NPRP assessment, the median WPRS for EDs nationally was 68.9,9 indicating that the majority of EDs in the US are still not fully compliant with published guidelines. Over 70% of pediatric emergency visits occur in community hospitals rather than pediatric hospitals,5 including the majority of visits by infants and by children with medical complexity,10 underscoring the importance of assessing and improving pediatric readiness across all EDs.
Although these findings highlight the potential for further improvements in pediatric readiness, they do not address the degree to which pediatric-ready emergency care is geographically accessible for the nation’s children. Prior work identified that the majority of pediatric ED visits occur at non-pediatric EDs, and that 9% of pediatric ED visits at general EDs are by children less than 1 year old. Thus a pressing question remains: when emergencies occur, will parents and families be able to quickly travel to an ED with high pediatric readiness? The goal of this study is to address this knowledge gap by examining the distribution of EDs with high pediatric readiness relative to the pediatric population in order to understand how accessible pediatric-ready EDs are for children nationally and regionally.
Methods
We performed a cross-sectional analysis of geographic access to pediatric-ready EDs for the US pediatric population in 2013, the most recent year of available data. We defined geographic access as living within 30-minutes driving time of an ED meeting specified thresholds of the WPRS. We used 30 minutes of drive time based on prior work reporting that adults with children in the household were willing to spend up to 30 minutes traveling for urgent concerns11 and that less than 4% of children arrive to ED by ambulance.12 We examined access nationally and for the nine US Census divisions.
To identify US hospital-based EDs, we used the comprehensive list of hospitals developed for the 2013 NPRP assessment. The detailed methods of the development and deployment of the 55 question web-based survey are available elsewhere.9 Briefly, the NPRP survey was designed to assess adherence to guidelines for pediatric readiness. The NPRP national steering committee identified hospitals in each state from the 2009 American Hospital Association database, and then requested that Emergency Medical Services for Children (EMSC) program managers in all states review and finalize the list to ensure inclusion of all hospitals with EDs open continuously, excluding federal and prison hospitals. The survey focused on these EDs because the guidelines were intended to apply to hospital-based EDs with 24/7 staffing. With assistance of multiple professional organizations at national and local levels and EMSC state managers, the NPRP survey was deployed to nurse managers at 5017 identified hospitals across the US and US territories.
Hospitals were surveyed from January 1 to August 23, 2013 with each hospital given a 3-month period to complete the survey. Among the 5017 surveyed hospitals, 4959 were within the nonterritorial US. Of these, 4090 (82%) responded to the survey. To understand the characteristics of responding and non-responding hospitals, we linked NPRP survey data with 2011 American Hospital Association (AHA) data using hospital name, state, county, and zip code. Among the 869 non-responders, 79 could not be matched to an AHA-identified hospital, including after manual review, with many representing healthcare facilities that either closed or did not appear to meet original inclusion criteria. These 79 hospitals, representing 1.6% of the original sample, were dropped from further analysis. The 790 matched non-responders and the 4090 responders comprised the final cohort.
We used the WPRS to determine pediatric readiness for each ED. The WPRS was developed through expert panel and an initial pilot, ultimately weighting 24 of 55 questions. A WPRS of 100 indicates that the ED meets the essential guidelines for pediatric readiness. In addition to examining total WPRS, we separated scored items into three subscores, maintaining the same weighting for each item as used in the total WPRS: equipment (33 points including equipment, supplies, and medications), personnel (29 points including staffing and physician and nurse coordinators), and processes (38 points including quality improvement, safety, processes, policies, and procedures).
For the 4090 hospitals that responded to the survey, we determined total WPRS and three subscores from survey responses. For the 790 non-responding hospitals, we performed multiple imputation13, 14 of the 3 subscores (personnel, equipment, and processes). Multiple imputation generates multiple simulated datasets, each containing plausible values for missing data, which are then analyzed and pooled.13, 14 To perform the imputation, we first evaluated hospital characteristics associated with both non-response and WPRS based on AHA linkage. The goal of this step was to evaluate the degree to which non-response was associated with measured variables. We then developed a regression model for each WPRS subscore in which the model covariates included ED characteristics (pediatric ED, trauma center level, total volume, triage system), hospital characteristics (bed size, inpatient pediatric ward, pediatric intensive care unit (ICU), neonatal ICU, pediatric cardiology, computed tomography scanner, magnetic resonance imaging), accreditations (The Joint Commission, Accreditation Council for Graduate Medical Education), and geographic characteristics (rural/urban status, state). We then used the univariate conditional probability distributions from these models to create 10 multiply imputed datasets with three imputed subscores and a summed total WPRS.
We dichotomized the WPRS and the three subscores in each of the 10 multiply imputed datasets to reflect whether each ED met a high level of pediatric-readiness. For our primary analysis, we used a cut-point of 100 WPRS, the maximal readiness score. Because only a small number of EDs received a score of 100, we repeated our analysis using cut-points at the 75th percentile (83.6) and 90th percentile (94.3), recognizing that many hospitals not achieving a maximal score still possess pediatric readiness that is approaching the maximal score.
We obtained the population ages 14 years and younger and 17 years and younger in each zip code from 2013 US Census data. Recognizing variation in the definition of “pediatric patients,” we used these cut points to focus our primary analysis on a cohort recognized as “pediatric” by the vast majority of EDs (0–14 years old, recognized as pediatric by 83% of EDs), and also performing a sensitivity analysis with a more inclusive definition of pediatric (0–17 years old, recognized as pediatric by 71% of EDs).4
Statistical Analyses
We used descriptive statistics to compare hospital characteristics for responders and non-responders, using chi-squared tests to test significant differences for categorical variables. We performed each subsequent analysis separately using each imputed dataset and then combined results using standard methodology.15
We determined national and census division geographic access to EDs with WPRS of 100, as well as to EDs scoring at or above the 75th and 90th percentiles for WPRS. We also determined national and census division access to EDs with maximal subscores. Using driving time, we built 30-minute travel radii around each hospital meeting the indicated score threshold. Using the geometric centroid of each zip code, we determined the percentage of children 14 years and younger living within 30-minute travel radii of identified EDs nationally and for each of the nine census divisions, using methods similar to previous evaluations of access to care.16–18 We allowed travel across state lines. For children within 30 minutes of a hospital scoring either 100 or at the 75th or 90th percentile, we also determined the percentage who had the option of a closer ED with a WPRS below the specified score.
We performed sensitivity analyses to assess the robustness of our results to study assumptions. To assess the robustness of our results to missing WPRS scores, we re-performed the analyses under two extreme assumptions about hospitals with missing WPRS scores: first, that all non-responding hospitals scored below the indicated threshold (“worst case”); second, that all non-responding hospitals scored at or above the indicated threshold (“best case”). To assess the robustness of our results to our definition of the pediatric population, we re-performed the analysis using the pediatric population ages 17 years and younger rather than ages 14 years and younger.
We performed statistical analysis in Stata 14.2 (StataCorp, College Station, Texas) and geographic information systems (GIS) analysis in ArcGIS version 10.4 (Esri, Redlands, California). This study was reviewed and deemed exempt from human subjects review by both the University of Pittsburgh Human Research Protections Office and the University of Utah Institutional Review Board.
Results
The 4090 responding EDs were similar to the 790 non-responding EDs with respect to total ED volume, trauma level, and having a pediatric ED, pediatric inpatient service, and neonatal ICU (Table 1). Compared with non-responders, responders were more likely to have a large number of inpatient beds (31.4% of responders with >200 beds versus 26.8% of non-responders, p=0.02), more likely to have a pediatric ICU (17% of responders versus 13.8% of non-responders, p=0.03), and more likely to be located in smaller non-metropolitan counties (31.2% of responders versus 23.5% of non-responders, P < .001).
Table 1.
ED and Hospital Characteristics for National Pediatric Readiness Project Survey Respondents and Non-Respondents, 2013
| Respondents (n=4090) |
Non-Respondents (n=790) |
p-value | |
|---|---|---|---|
| ED Characteristics | |||
| Total ED Volume | 0.54 | ||
| – 0–4999 Visits | 739 (18.1%) | 145 (18.4%) | |
| – 5000–9999 Visits | 490 (12.0%) | 105 (13.3%) | |
| – >10,000 Visits | 2861 (70.00%) | 540 (68.4%) | |
| Pediatric ED | 670 (16.4%) | 109 (13.8%) | 0.07 |
| Trauma Center Level | 0.21 | ||
| – Not Trauma Center | 2575 (63.0%) | 519 (65.7%) | |
| – Level 1 | 330 (8.1%) | 53 (6.7%) | |
| – Level 2 | 427 (10.4%) | 66 (8.4%) | |
| – Level 3 | 589 (14.4%) | 114 (14.4%) | |
| – Level 4 | 169 (4.1%) | 38 (4.8%) | |
|
| |||
| Hospital Characteristics | |||
| Bed Size* | 0.02 | ||
| – 6–49 beds | 1196 (31.9%) | 255 (32.3%) | |
| – 50–199 beds | 1373 (36.6%) | 323 (40.9%) | |
| – >200 beds | 1176 (31.4%) | 212 (26.8%) | |
| Inpatient Pediatric Service | 1944 (47.5%) | 376 (47.6%) | 0.97 |
| Pediatric ICU | 696 (17.0%) | 109 (13.8%) | 0.03 |
| Neonatal ICU | 1138 (27.8%) | 231 (29.2%) | 0.42 |
|
| |||
| Geographic Characteristics | |||
| County Rural/Urban | <0.001 | ||
| – Metropolitan | 2442 (59.7%) | 493 (62.4%) | |
| – Non-metro, urban pop>20,000 | 369 (9%) | 81 (10.3%) | |
| – Non-metro, urban pop <20000 | 1277 (31.2%) | 186 (23.5%) | |
| – Missing | 2 (0.1%) | 30 (3.8%) | |
| Region | <0.001 | ||
| – Northeast | 126 (3.4%) | 57 (7.2%) | |
| – Mid-Atlantic | 335 (9.0%) | 54 (6.8%) | |
| – East North Central | 530 (14.2%) | 141 (17.9%) | |
| – West North Central | 583 (15.6%) | 110 (13.9%) | |
| – South Atlantic | 296 (7.9%) | 92 (11.7%) | |
| – East South Central | 606 (16.2%) | 40 (5.1%) | |
| – West South Central | 509 (13.6%) | 200 (25.3%) | |
| – Mountain | 340 (9.1%) | 33 (4.2%) | |
| – Pacific | 420 (11.2%) | 63 (8.0%) | |
Data missing for some hospitals in AHA data for indicated variable.
In primary analysis, 93.7% of children nationally could travel to any ED within 30 minutes (Table 2). However, only 33.7% of children nationally could travel within 30 minutes to an ED with a WPRS of 100. Approximately half of children (55.3%) could travel within 30 minutes to an ED with WPRS at or above the 90th percentile (94.3), and 70.2% to an ED at or above the 75th percentile (83.6).
Table 2.
Percent of Pediatric Population within 30 minutes of Driving Time to any ED and to ED at or above maximum, 90th, and 75th percentile WPRS, National Pediatric Readiness Project, 2013
| Any ED within 30 min | No ED within 30 min | ED with max WPRS within 30 min | Only EDs with WPRS below maximum score within 30 min | ED with WPRS ≥90th percentile within 30 min | Only EDs with WPRS <90th percentile within 30 min | ED with WPRS ≥75th percentile within 30 min | Only EDs with WPRS <75th percentile within 30 min | |
|---|---|---|---|---|---|---|---|---|
| Specified Score Threshold | NA | 100 | 94.3 | 83.6 | ||||
|
| ||||||||
| National | 93.7% | 6.3% | 33.7% | 60.0% | 55.3% | 38.4% | 70.2% | 23.5% |
| Census Division | ||||||||
| – New England | 98.2% | 1.8% | 21.5% | 76.7% | 63.8% | 34.4% | 78.6% | 19.6% |
| – East North Central | 97.5% | 2.5% | 31.5% | 66.0% | 53.3% | 44.2% | 76.0% | 21.5% |
| – West North Central | 90.9% | 9.1% | 32.6% | 58.3% | 40.1% | 50.8% | 55.7% | 35.2% |
| – Mid Atlantic | 98.0% | 2.0% | 56.2% | 41.8% | 68.2% | 29.8% | 83.1% | 14.9% |
| – South Atlantic | 95.5% | 4.5% | 24.1% | 71.4% | 50.4% | 45.1% | 68.2% | 27.3% |
| – East South Central | 94.1% | 5.9% | 14.9% | 79.2% | 40.4% | 53.7% | 60.3% | 33.8% |
| – West South Central | 93.0% | 7.0% | 29.8% | 63.2% | 56.3% | 36.7% | 67.0% | 26.0% |
| – Mountain | 79.9% | 20.1% | 38.4% | 41.5% | 59.3% | 20.6% | 64.7% | 15.2% |
| – Pacific | 91.9% | 8.1% | 41.8% | 50.1% | 60.7% | 31.2% | 70.9% | 21.0% |
Percent of the population of children 0–14 years old nationally and within each of 9 census divisions with access within 30 minutes of drive time to any ED and to an ED scoring at or above the maximum score, 90th percentile, and 75th percentile weighted readiness score (WPRS).
Across census divisions, the percentage of children able to travel to any ED within 30 minutes ranged from 79.9% (Mountain division) to 98.2% (New England division). The percentage of children able to travel to an ED with WPRS of 100 ranged from 14.9% (East South Central division) to 56.2% (Mid Atlantic division) (Table 2 and Figure). The percentage of children able to travel to an ED scoring at or above the 75th percentile and 90th percentile ranged from 55.7% to 83.1% and 40.1% to 68.2%, respectively (Figure). The census division with the highest proportion of children who could travel only to EDs scoring below the 75th percentile WPRS within 30 minutes was the West North Central division (35.2%).
Figure: Percent of children within 30 minutes of driving time to ED with specified WPRS by census division, National Pediatric Readiness Project, 2013.
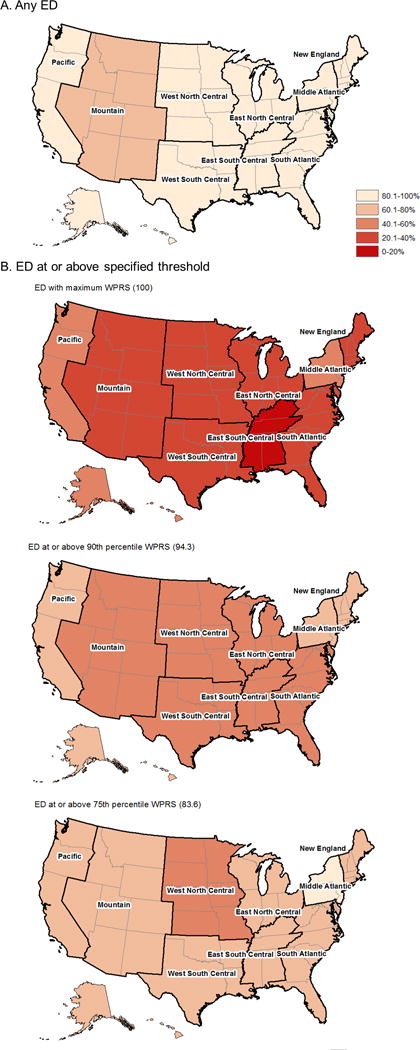
Figure legend: Among children 0–14 years old, the percent of the population able to travel within 30 minutes to (A) any ED and to (B) EDs scoring at or above specified WPRS thresholds, specifically maximum WPRS (100), 90th percentile WPRS (94.3), and 75th percentile WPRS (83.6).
Results for WPRS subscores were similar to total WPRS (Table 3). The percentage of children nationally within 30-minute drive time of an ED with personnel, equipment, and processes subscores at maximum were 64.2%, 66.2%, and 45.2%, respectively. In all regions, the percentage of children within 30 minutes of an ED with maximum subscore for processes was lower than the percentage of children within 30 minutes of an ED with maximum subscores for personnel or equipment.
Table 3.
Percent of Pediatric Population within 30 minutes of Driving Time to any ED and to ED with maximum WPRS subscores, National Pediatric Readiness Project, 2013
| ED with Maximum WPRS Subscore within 30 Min | |||
|---|---|---|---|
|
| |||
| Personnel Subscore | Equipment Subscore | Process Subscore | |
| Specified Score Threshold | 29 | 33 | 38 |
|
| |||
| National | 64.2% | 66.2% | 45.2% |
|
| |||
| Census Division | |||
| – New England | 74.5% | 72.1% | 47.7% |
| – East North Central | 70.9% | 70.5% | 47.1% |
| – West North Central | 49.2% | 48.9% | 36.4% |
| – Mid Atlantic | 79.5% | 80.5% | 64.0% |
| – South Atlantic | 61.2% | 64.0% | 36.2% |
| – East South Central | 48.2% | 48.0% | 26.1% |
| – West South Central | 60.1% | 64.6% | 43.9% |
| – Mountain | 61.5% | 62.9% | 53.4% |
| – Pacific | 65.1% | 70.5% | 47.6% |
Percent of the population of children 0–14 years old nationally and within each of 9 census divisions with access within 30 minutes of travel time to an ED achieving the maximum score for the three subscores of the WPRS.
Among children within 30-minute drive time of an ED with WPRS of 100, 90.9% had the choice of at least one other ED that was closer but scored below 100. Among children within 30-minute drive time of an ED with WPRS at or above the 90th percentile, 79.2% had the choice of at least one other ED that was closer but scored below the 90th percentile. Finally, among children within 30-minute drive time of an ED with WPRS at or above the 75th percentile, 57.8% had the choice of at least one other ED that was closer but scored below the 75th percentile.
In sensitivity analyses examining possible results under extreme assumptions for non-responders, the percentage of children nationally with access to an ED scoring at or above the 75th percentile WPRS had the potential to vary by 10 percentage points (68.3% to 77.6%), if we assumed that either none or all of the non-responding EDs scored at or above that mark (Table 4; available at www.jpeds.com). Results using higher WPRS thresholds had the potential to be more sensitive to assumptions about missing hospitals.
Table 4.
online only. Sensitivity Analysis of National Results: Best Case and Worst Case Estimates of Percent of Pediatric Population within 30 minutes of Driving Time to ED at Specified WPRS Threshold, National Pediatric Readiness Project, 2013
| Access to ED with Maximum WPRS | Access to ED with WPRS ≥90th percentile | Access to ED with WPRS ≥75th percentile | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Missing data assumption | All <Max Score (“Worst Case”) |
All >Max Score (“Best Case”) |
All <90th percentile (“Worst Case”) |
All ≥90th percentile (“Best Case”) |
All <75th percentile (“Worst Case”) |
All ≥75th percentile (“Best Case”) |
| National | 33.7% | 59.4% | 54.9% | 69.3% | 68.3% | 77.6% |
| Census Division | ||||||
| – New England | 21.5% | 80.0% | 62.8% | 86.2% | 73.9% | 89.8% |
| – East North Central | 31.5% | 53.5% | 52.6% | 68.0% | 74.2% | 82.0% |
| – West North Central | 32.6% | 40.9% | 40.0% | 48.1% | 54.9% | 60.5% |
| – Mid Atlantic | 56.2% | 70.3% | 68.0% | 78.1% | 81.9% | 87.4% |
| – South Atlantic | 24.1% | 56.8% | 49.9% | 69.6% | 66.3% | 78.1% |
| – East South Central | 14.9% | 54.7% | 40.0% | 61.8% | 57.8% | 73.8% |
| – West South Central | 29.8% | 66.9% | 56.2% | 74.2% | 64.5% | 78.0% |
| – Mountain | 38.4% | 49.7% | 59.3% | 61.7% | 64.6% | 65.8% |
| – Pacific | 41.8% | 62.7% | 60.4% | 70.7% | 68.9% | 76.8% |
Sensitivity analysis examining potential results with alternative assumptions about missing hospital scores. Results are percent of children estimated to be within 30 minutes of EDs with maximum WPRS and EDs at or above 75th and 90th percentile WPRS score thresholds under “worst case” and “best case” assumptions. The “worst case” assumes all 790 non-responding EDs had scores below specified threshold. The “best case” assumes all 790 non-responding EDs had scores at or above the specified threshold.
In sensitivity analysis examining the impact of a broader definition of pediatric patients, we found minimal difference in results, with the percentage of children 0–17 years old living within 30 minutes of a ED at each studied threshold varying by only 0.1% from the results for children 0–14 years old.
Discussion
Although 93.7% of US children can access an ED within a 30-minute drive, only 33.7% of children lived within 30 minutes of an ED with a WPRS of 100. Because the WPRS was developed based on the essential recommendations for pediatric readiness, our results show that nearly two-thirds of children cannot readily access an ED that is highly compliant with pediatric emergency care guidelines. These results were supported by our sensitivity analyses which show that even under “best case” assumptions about the readiness of non-responding hospitals, there are substantial gaps in geographic access nationwide.
Our national and regional findings have important implications for health policy and planning surrounding pediatric emergency care delivery in the US. Because the major gaps in access were not due to the lack of an available ED but due instead to the lack of an ED with high pediatric readiness, our findings demonstrate that efforts to increase pediatric readiness across all EDs will successfully increase geographic access. This was not necessarily a given – we could have found that most children lived near EDs that are already highly pediatric-ready, or we could have found that most children did not live near any ED. In such cases, increasing readiness at additional EDs would have little or no effect on geographic access to high pediatric-readiness EDs. Instead, our findings provide empirical support that efforts by hospitals and policymakers to improve ED readiness should accomplish their intended effect of increasing access to pediatric-ready emergency care.
One way to achieve this goal is through verification and recognition of ED pediatric capabilities by state agencies or other regulatory bodies, as promoted through the EMSC quality improvement collaborative.19 Prior work demonstrated that hospitals participating in a state-led verification of pediatric readiness have higher WPRS,20 and that completing the verification process is associated with a trend towards decreased pediatric mortality.21 Relatedly, hospitals with higher WPRS also have improved performance during simulated resuscitations.22 Expanding this initiative to more states may facilitate further improvement, and should especially be considered in regions with the greatest gaps in access to pediatric-ready EDs. Investment in pediatric resources by health systems and federal agencies is another option. Certainly, multiple barriers face EDs seeking to improve pediatric readiness, ranging from limited awareness of pediatric guidelines to finite financial, educational, and human resources.9 These barriers are reported more frequently at hospitals with lower pediatric ED volume, which also have lower WPRSs on average.9 Our results underscore the value of geographic analyses in guiding investments in specific hospitals and resources, because health systems and government agencies could use such analyses to better understand regional needs and to determine which hospitals should be targeted to maximize access.
Our results also highlight the choices facing families seeking emergent care. Although one in three children could quickly reach an ED with a WPRS score of 100, 90% of these children could present to a closer but less pediatric-ready alternative ED. Similarly, among children within 30 minutes of an ED scoring at or above the 75th percentile WPRS, more than half had a closer but less pediatric-ready alternative ED. Thus for most children, the closest ED is different from the closest pediatric-ready ED. Providing families with objective information about the readiness of EDs for pediatric emergencies (i.e., through public reporting, through point-of-care apps,23 or through education of families by primary care physicians) may allow families to make more informed choices when seeking care.
These same decisions are faced by emergency medical service (EMS) providers, such that our results underscore the need for pediatric-specific protocols to assist with transport decisions. For example, in California, pediatric patients are preferentially transported to the closest ED that completed a pediatric verification process.20 As a result, 93% of pediatric 911 calls in Los Angeles County, California, are transported to pediatric-verified EDs, which have high pediatric readiness (median WPRS of 89.6).20 However, not all states have pediatric verification processes or pediatric transport guidelines.7 Additional research is needed to support the development of optimal guidance for directing children to emergency care with attention to trade-offs between travel time and pediatric readiness.
In interpreting these results, note that we focused on only one aspect of overall access: geographic accessibility. More broadly, access to emergency care also requires availability (i.e., capacity), accommodation (i.e., hours), acceptability (i.e., cultural competency), and affordability (i.e., costs).24 Because the NPRP assessment was limited to EDs open continuously, accommodation may be assumed for included hospitals, but the capacity, acceptability, and affordability of emergency care may further limit access for some children. Additionally, examination of 30-minute travel time does not account for other dimensions of geographic accessibility. For example, families relying on public transit, unreliable vehicles, or limited financial resources may not perceive care to be geographically accessible despite living within 30-minute drive time. Families may seek ambulance transport in the absence of other transportation options, but unless bypass protocols are in place, the closest pediatric-ready hospital may still remain out of reach if another hospital is closer.7 Thus our results should be considered high-end estimates of the percentage of children with geographic access to pediatric-ready ED care, with recognition that additional geographic and non-geographic barriers may further limit access.
Our study has several limitations. First, the NPRP assessment on which our analysis was based had an 18% non-response rate among US hospitals. Although this is a low non-response rate, the nature of our analysis is such that dropping missing data could significantly skew results. To address this limitation, we used rigorous imputation methods and estimates of best/worst scenarios. In best/worst case scenarios, assumptions about missing data had the greatest potential impact at the highest WPRS thresholds. However, “best case” assumptions become increasingly unlikely at higher thresholds, as it is unlikely that all missing hospitals achieved a score attained by <10% of responding hospitals. Second, many families have a choice in where they seek care, and our results do not address how these choices are made or where children ultimately seek care; rather we focused on whether a pediatric-ready ED is one of the choices available. Third, the NPRP assessment was completed in 2013. Although there has been no systematic reassessment since the 2013 assessment, nearly a quarter of hospitals reassessed voluntarily in 2015–16, with median score increasing by only 3 points, suggesting our analysis remains relevant. Relatedly, federal legislation over recent years altered emergency care affordability, with associated increases and decreases in ED utilization for different populations.25–28 However, such legislation did not target the readiness of EDs for pediatric emergencies. Fourth, we recognize there are multiple definitions of pediatric patients. Our analysis focused on children 0–14 years old, but we would not expect results for other age groups to be dramatically different unless there was a significant difference in the distribution of children of different ages across the country. Our analysis of children 0–17 years old confirms that our results are unlikely to change with different definitions of pediatric patients. Fifth, the survey and our analysis did not include other potential sites of urgent and emergent care, such as urgent care centers and free-standing EDs, instead focusing on hospital-based EDs open continuously. Sixth, it is worth noting that at the 90th and 75th percentile thresholds studied, the missing components of readiness may vary across hospitals. However, this analysis is complemented by our subscore analysis, which allows assessment of access to EDs meeting essential guidelines for specific components, regardless of their scores in the other components, which may ultimately have varying impact on quality and outcomes. Seventh, survey responses were entirely self-reported, with the potential for biases, although a range of responses were obtained. Finally, the WPRS is based upon portions of the guidelines for pediatric readiness, such that a WPRS of 100 indicates that the ED meets the essential guidelines. Because few EDs met this threshold, our analysis also included lower thresholds (75th percentile and 90th percentile) to quantify access to EDs approaching a WPRS of 100. Future evaluations could choose to examine access using the same absolute WPRSs as our assessment (100, 94.3, 83.6) to monitor change in access over time. Future work may reveal additional characteristics supporting ED pediatric readiness, such as telemedicine capabilities,29–32 not included in the WPRS.
In conclusion, this study quantifies geographic access to EDs with high pediatric readiness for children nationally. Through GIS analysis, we built upon prior studies that examined the pediatric readiness of EDs4, 9, 33 by examining whether children could travel to these EDs within 30 minutes. By identifying gaps between children who could travel to any ED versus children who could travel to a pediatric-ready ED, this study highlights the potential impact of efforts to improve pediatric readiness in existing EDs. Our study also paves the way for future efforts to prioritize investment in infrastructure and pediatric emergency care coordination between hospitals or within healthcare systems, in order to improve access and ultimately improve outcomes for children in need of emergency care.
Acknowledgments
Supported in part by grants from the US Agency for Healthcare Research and Quality (K12HS022989 to K.R.), the Children’s Hospital of Pittsburgh of the UPMC Health System (to K.R.), the US National Institutes of Health (K08 HL122478 to D.W.), the US Department of Health and Human Services (HHS) Health Resources and Services Administration (HRSA) (U03MC00008 to E.E.; HSAMC24076 to J.K.; U07MC09174 to L.O.; and U07MCO5036 to L.O.).
Abbreviations
- AHA
American Hospital Association
- ED
emergency department
- EMSC
Emergency Medical Services for Children
- GIS
geographic information systems
- NPRP
National Pediatric Readiness Project
- ICU
intensive care unit
- US
United States
- WPRS
weighted pediatric readiness score
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors declare no conflicts of interest.
References
- 1.American Academy of Pediatrics Committee on Pediatric Emergency M. Yamamoto LG. Access to optimal emergency care for children. Pediatrics. 2007;119(1):161–4. doi: 10.1542/peds.2006-2900. [DOI] [PubMed] [Google Scholar]
- 2.American Academy of Pediatrics Committee on Pediatric Emergency Medicine, American College of Emergency Physicians Pediatric Committee, Emergency Nurses Association Pediatric Committee. Joint policy statement–guidelines for care of children in the emergency department. Ann Emerg Med. 2009;54(4):543–52. doi: 10.1016/j.annemergmed.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 3.American Academy of Pediatrics, Committee on Pediatric Emergency Medicine, American College of Emergency Physicians Pediatric Committee, Emergency Nurses Association Pediatric Committee. Joint policy statement–guidelines for care of children in the emergency department. Pediatrics. 2009;124(4):1233–43. doi: 10.1542/peds.2009-1807. [DOI] [PubMed] [Google Scholar]
- 4.Gausche-Hill M, Schmitz C, Lewis RJ. Pediatric preparedness of US emergency departments: a 2003 survey. Pediatrics. 2007;120(6):1229–37. doi: 10.1542/peds.2006-3780. [DOI] [PubMed] [Google Scholar]
- 5.Schappert SM, Bhuiya F. Availability of pediatric services and equipment in emergency departments: United States, 2006. Natl Health Stat Report. 2012(47):1–21. [PubMed] [Google Scholar]
- 6.Middleton KR, Burt CW. Availability of pediatric services and equipment in emergency departments: United States, 2002–03. Adv Data. 2006(367):1–16. [PubMed] [Google Scholar]
- 7.Institute of Medicine Committee of the Future of Emergency Care in the US Health System. Emergency Care for Children: Growing Pains. Washington, DC: National Academies Press; 2007. [Google Scholar]
- 8.Pediatric Readiness Project. Pediatric emergency department pediatric readiness resource site. Available from: www.pediatricreadiness.org.
- 9.Gausche-Hill M, Ely M, Schmuhl P, Telford R, Remick KE, Edgerton EA, et al. A national assessment of pediatric readiness of emergency departments. JAMA Pediatr. 2015;169(6):527–34. doi: 10.1001/jamapediatrics.2015.138. [DOI] [PubMed] [Google Scholar]
- 10.Hudgins JD, Monuteaux MC, Bourgeois FT, Nigrovic LE, Fine AM, Lee LK, et al. Complexity and Severity of Pediatric Patients Treated at United States Emergency Departments. J Pediatr. 2017;186:145–9 e1. doi: 10.1016/j.jpeds.2017.03.035. [DOI] [PubMed] [Google Scholar]
- 11.Yen W, The Health Care Research Group . Washington State Health Services Research Project. 2013. How long and how far do adults travel and will adults travel for primary care? (Research Brief No 70). [Google Scholar]
- 12.McCaig LF, Burt CW. Advance Data from Vital and Health Statistics. 385. 2005. National Hospital Ambulatory Medical Care Survey: 2003 Emergency Department Summary. [PubMed] [Google Scholar]
- 13.Greenland S, Finkle WD. A critical look at methods for handling missing covariates in epidemiologic regression analyses. Am J Epidemiol. 1995;142(12):1255–64. doi: 10.1093/oxfordjournals.aje.a117592. [DOI] [PubMed] [Google Scholar]
- 14.Rubin DB, Shenker N. Multiple imputation in health-care databases: an overview and some applications. Stat Med. 1991;10(4):585–98. doi: 10.1002/sim.4780100410. [DOI] [PubMed] [Google Scholar]
- 15.Rubin DB. Multiple imputation for nonresponse in surveys. New York: John Wiley and Sons; 1987. [Google Scholar]
- 16.Wallace DJ, Angus DC, Seymour CW, Yealy DM, Carr BG, Kurland K, et al. Geographic access to high capability severe acute respiratory failure centers in the United States. PLoS One. 2014;9(4):e94057. doi: 10.1371/journal.pone.0094057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carr BG, Branas CC, Metlay JP, Sullivan AF, Camargo CA., Jr Access to emergency care in the United States. Ann Emerg Med. 2009;54(2):261–9. doi: 10.1016/j.annemergmed.2008.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nance ML, Carr BG, Branas CC. Access to pediatric trauma care in the United States. Arch Pediatr Adolesc Med. 2009;163(6):512–8. doi: 10.1001/archpediatrics.2009.65. [DOI] [PubMed] [Google Scholar]
- 19.Emergency Medical Services for Children Innovation and Improvement Center. Facility Recognition Collaborative. 2017 Available from: https://emscimprovement.center/collaboratives/facilityrecognition-collaborative/about/
- 20.Remick K, Kaji AH, Olson L, Ely M, Schmuhl P, McGrath N, et al. Pediatric Readiness and Facility Verification. Ann Emerg Med. 2016;67(3):320–8 e1. doi: 10.1016/j.annemergmed.2015.07.500. [DOI] [PubMed] [Google Scholar]
- 21.Rice A, Dudek J, Gross T, Mars T, St, Woolridge D. The Impact of a Pediatric Emergency Department Facility Verification System on Pediatric Mortality Rates in Arizona. J Emerg Med. 2017;52(6):894–901. doi: 10.1016/j.jemermed.2017.02.011. [DOI] [PubMed] [Google Scholar]
- 22.Auerbach M, Whitfill T, Gawel M, Kessler D, Walsh B, Gangadharan S, et al. Differences in the Quality of Pediatric Resuscitative Care Across a Spectrum of Emergency Departments. JAMA Pediatr. 2016;170(10):987–94. doi: 10.1001/jamapediatrics.2016.1550. [DOI] [PubMed] [Google Scholar]
- 23.EMNet. National Emergency Department Survey. Available from: http://www.emnetusa.org/studies/nationaledsurvey.htm.
- 24.Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981;19(2):127–40. doi: 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
- 25.Medford-Davis LN, Eswaran V, Shah RM, Dark C. The Patient Protection and Affordable Care Act’s Effect on Emergency Medicine: A Synthesis of the Data. Ann Emerg Med. 2015;66(5):496–506. doi: 10.1016/j.annemergmed.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 26.Hernandez-Boussard T, Morrison D, Goldstein BA, Hsia RY. Relationship of Affordable Care Act Implementation to Emergency Department Utilization Among Young Adults. Ann Emerg Med. 2016;67(6):714–20 e1. doi: 10.1016/j.annemergmed.2015.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dresden SM, Powell ES, Kang R, McHugh M, Cooper AJ, Feinglass J. Increased Emergency Department Use in Illinois After Implementation of the Patient Protection and Affordable Care Act. Ann Emerg Med. 2017;69(2):172–80. doi: 10.1016/j.annemergmed.2016.06.026. [DOI] [PubMed] [Google Scholar]
- 28.Sommers BD, Simon K. Health Insurance and Emergency Department Use – A Complex Relationship. N Engl J Med. 2017;376(18):1708–11. doi: 10.1056/NEJMp1614378. [DOI] [PubMed] [Google Scholar]
- 29.Dayal P, Hojman NM, Kissee JL, Evans J, Natale JE, Huang Y, et al. Impact of Telemedicine on Severity of Illness and Outcomes Among Children Transferred From Referring Emergency Departments to a Children’s Hospital PICU. Pediatr Crit Care Med. 2016;17(6):516–21. doi: 10.1097/PCC.0000000000000761. [DOI] [PubMed] [Google Scholar]
- 30.Mollen CJ, Henien M, Jacobs LM, Myers S. Parent Perceptions on Transfers to Pediatric Emergency Departments and the Role of Telemedicine. Pediatr Emerg Care. 2016 doi: 10.1097/PEC.0000000000000957. [DOI] [PubMed] [Google Scholar]
- 31.Ray KN, Felmet KA, Hamilton MF, Kuza CC, Saladino RA, Schultz BR, et al. Clinician Attitudes Toward Adoption of Pediatric Emergency Telemedicine in Rural Hospitals. Pediatr Emerg Care. 2016 doi: 10.1097/PEC.0000000000000583. [DOI] [PubMed] [Google Scholar]
- 32.Yang NH, Dharmar M, Kuppermann N, Romano PS, Nesbitt TS, Hojman NM, et al. Appropriateness of disposition following telemedicine consultations in rural emergency departments. Pediatr Crit Care Med. 2015;16(3):e59–64. doi: 10.1097/PCC.0000000000000337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sadovich J, Adirim T, Telford R, Olson LM, Gausche-Hill M, Edgerton EA. Pediatric Readiness in Indian Health Service and Tribal Emergency Departments: Results from the National Pediatric Readiness Project. J Emerg Nurs. 2015 doi: 10.1016/j.jen.2015.09.004. [DOI] [PubMed] [Google Scholar]


