Abstract
A cyclist reported gradual onset, bilateral leg claudication without any atherosclerotic risk factors and with a normal vascular examination. Duplex ultrasound and magnetic resonance angiography revealed bilateral focal stenoses due to coralline plaques of the common femoral arteries (CFAs) but normal proximal and distal vasculature. A surgical endarterectomy with vein patch angioplasty resolved all symptoms. Cyclist’s iliac syndrome (whereby mechanical and anatomical factors in competitive cyclists and runners lead to arterial kinking and subsequent intimal hyperplasia, endofibrosis and, ultimately, stenoses of the external iliac arteries) is well documented. This is the first report to our knowledge of a similar process isolated to the CFA.
Keywords: Femoral artery, Stenosis, Vascular diseases
Case history
A 59-year-old man presented to the vascular outpatients clinic with a 4-year history of cramping bilateral calf and thigh pain on exercising. He had been a keen amateur cyclist since his teenage years and regularly cycled over 100 miles per week. He also ran 40 miles per week. Initially, his symptoms came on after cycling for 2 miles or jogging for half a mile. However, they had progressed over time and now occurred on walking 50 yards. The pain affected the left leg more than the right and resolved after resting for five minutes.
Our patient had no past medical history of note (specifically, no diabetes, hypertension, hypercholesterolaemia, ischaemic heart disease or peripheral vascular disease). His only regular medication was lansoprazole. He had never smoked cigarettes and had no history of trauma to his legs. There was no family history of any cardiovascular disease. He was employed as a maintenance worker in a health club.
On examination he was of slim build with a body mass index of 23.4kg/m2. His feet were both warm and well perfused with a normal capillary refill time. He had a full compliment of strong peripheral pulses. Doppler signals were triphasic in all pedal pulses. The ankle–brachial pressure index was 1 bilaterally. Routine blood tests were all normal.
The patient underwent arterial duplex ultrasonography of his lower limbs, which showed a tight stenosis of the left common femoral artery (CFA) and a less severe narrowing of the right CFA. Good flow was seen throughout the vessels distal to the stenoses. Lower limb magnetic resonance angiography confirmed these findings (Fig 1). Stenoses were seen in both CFAs but all distal vessels were disease free (Fig 2).
Figure 1.
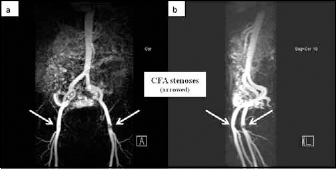
Magnetic resonance angiography of lower limbs showing bilateral common femoral artery stenoses
Figure 2.
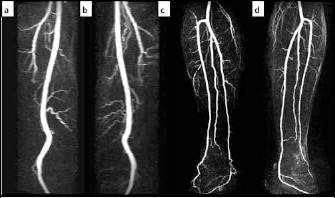
Magnetic resonance angiography showing disease free superficial femoral artery, popliteal and crural vessels bilaterally
The patient was scheduled for bilateral common femoral endarterectomies, which were performed under general anaesthetic. On the left side there was a near-occlusive coralline plaque situated in the CFA with no surrounding atheroma (Fig 3). A similar but smaller plaque was present in the right CFA. The arteries were repaired with autologous vein patches. Postoperatively, his feet were well perfused with strong bilateral dorsalis pedis and posterior tibial pulses. He was discharged home after three days. At his six-week follow-up appointment he was well and reported a complete resolution of his symptoms. At his six-month follow up he had returned to his pre-disease level of activity without complication.
Figure 3.
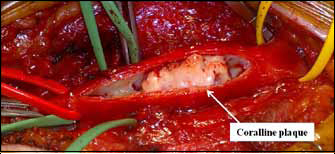
Arteriotomy showing coralline plaque in left common femoral artery
Discussion
Given the lack of risk factors for peripheral vascular disease and the unusual appearance of the plaques, we propose that this man developed femoral artery disease from cycling-inflicted repetitive strain injury.
A review of the literature reveals no reports of isolated CFA disease related to cycling. Cyclist’s iliac syndrome is a well documented condition whereby endofibrosis of the external iliac arteries results in structural change and subcritical stenoses. This is seen in competitive cyclists and runners, and leads to claudication symptoms at near maximal exercise levels. It is caused by a number of mechanical and anatomical factors that lead to arterial kinking and subsequent intimal hyperplasia.1–3
We propose a new pathology whereby chronic repetitive strain injury to the CFA as a result of cycling leads to localised intimal damage and the formation of obstructive coralline plaques. This leads to claudication symptoms despite an absence of risk factors for peripheral vascular disease and an excellent distal arterial supply. It should be considered in otherwise healthy patients with a background of cycling who present with symptoms indicative of claudication.
References
- 1.Ford SJ, Rehman A, Bradbury AW. External iliac endofibrosis in endurance athletes: a novel case in an endurance runner and a review of the literature. Eur J Vasc Endovasc Surg 2003; 26: 629–634. [DOI] [PubMed] [Google Scholar]
- 2.Wijesinghe LD, Coughlin PA, Robertson I et al. Cyclist’s iliac syndrome: temporary relief by balloon angioplasty. Br J Sports Med 2001; 35: 70–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feugier P, Chevalier JM. Endofibrosis of the iliac arteries: an underestimated problem. Acta Chir Belg 2004; 104: 635–640. [DOI] [PubMed] [Google Scholar]


