Abstract
Pancreaticoduodenectomy is the standard treatment for localised neoplasms of the pancreatic head. The operation can be performed safely in specialist units but good outcome is compromised if postoperative blood flow to the liver and biliary tree is inadequate. Coeliac artery occlusion with blood supply to the liver arising from the superior mesenteric artery via the gastroduodenal artery is difficult to recognise, especially intraoperatively. Recognition of absent hepatic artery pulsation after occlusion of the gastroduodenal artery opens a dilemma: should the resection be abandoned or should vascular reconstruction be undertaken, adding risk to an already complex procedure? We describe two cases with a resectable pancreatic endocrine tumour in which coeliac artery occlusion caused by median arcuate ligament compression was identified from cross-sectional imaging and reconstructions. We highlight two different strategies to correct the vascular insufficiency and allow safe pancreatic resection.
Keywords: Pancreaticoduodenectomy; Endocrine gland neoplasms; Radiology, interventional; Diaphragm
Coeliac axis stenosis is common and occurs in up to 24% of the general population.1–5 It is usually asymptomatic owing to compensatory collateral supply via anastomotic connections between the inferior pancreaticoduodenal and gastroduodenal arteries (GDAs). If symptoms do occur, these most frequently consist of weight loss, post-prandial abdominal pain, nausea and vomiting or diarrhoea.6,7 The aetiology of coeliac stenosis includes atherosclerotic plaques or thrombus in the coeliac trunk as well as compression by extrinsic masses originating in the pancreas, local lymph nodes and para-aortic ganglionic tissue. It is now recognised that diaphragmatic fibres close to the aorta may also impinge on the coeliac axis, causing stenosis (median arcuate ligament syndrome; MALS) either as a consequence of low insertion of the diaphragm or high origin of the coeliac trunk.6
The clinical significance of coeliac axis stenosis remains uncertain in the general population. However, in patients requiring pancreaticoduodenectomy, coeliac trunk patency is essential because of the requirement for intraoperative division of the GDA and the potential for postoperative hepatic and biliary ischaemia as a result of interruption of the collateral blood supply.8 Coeliac axis stenosis due to MALS has traditionally been identified intraoperatively when the GDA is temporarily clamped. The absence of pulsatile flow in the common hepatic artery suggests coeliac occlusion and proximal dissection towards the aorta and diaphragm may then reveal a tight median arcuate ligament in close proximity to the coeliac trunk. Recently, the use of computed tomography (CT) and duplex ultrasound has improved the preoperative diagnosis of MALS in patients requiring pancreaticoduodenectomy.9 This opens the possibility of treating MALS prior to pancreaticoduodenectomy, either by laparoscopic median arcuate ligament release or endovascular coeliac artery stenting. We report two cases of MALS in patients undergoing pancreaticoduodenectomy for endocrine tumours and highlight different strategies to manage this difficult situation.
Case history: one
A previously fit and well 53-year-old woman presented in July 2007 with iron deficiency anaemia. Abdominal CT and magnetic resonance imaging revealed a 10cm x 7cm heterogeneous, hypervascular mass originating in the head of the pancreas in association with a small hypervascular nodule in the liver, consistent with a metastatic pancreatic endocrine tumour. There was extensive venous drainage from the tumour and the patient was offered preoperative embolisation of the pancreatic primary (to reduce blood flow) and the metastasis (for ablation). Curative surgery was deemed possible after successful embolisation. However, angiography repeatedly demonstrated a 75% stenosis below the origin of the coeliac axis with the typical hooking configuration and anterior indentation associated with MALS (Fig 1).
Figure 1.
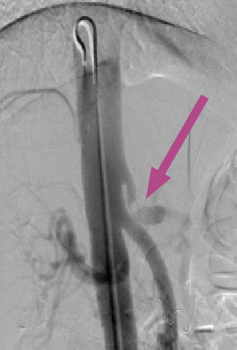
Aortic angiography of the patient in case one, demonstrating coeliac axis stenosis of >75% and the typical ‘hooking’ indentation associated with MALS (arrow)
Two unsuccessful attempts were made to perform endovascular stenting of the coeliac axis using a transfemoral approach, with failure attributed to the tight stenosis. Subsequently, a Genesis® stent (Cordis Corporation, Bridgewater, NJ, US) was successfully deployed across the lesion and dilated to 6.5mm, via a left brachial arteriotomy. Completion angiography demonstrated excellent antegrade flow through the proximal hepatic and splenic arteries (Fig 2).
Figure 2.
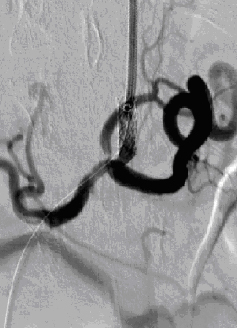
Angiographic stenting of the coeliac trunk in case one, demonstrating good run-off blood flow through the common hepatic, splenic and left gastric arteries
Pancreaticoduodenectomy was performed three weeks later, complicated by a period of delayed gastric emptying that was managed conservatively. The patient was discharged on the 27th postoperative day. Histology confirmed a non-functioning pancreatic endocrine tumour with local invasion and lymph node involvement. Postoperative octreotide scanning demonstrated no further metastases except for the small intrahepatic nodule observed on initial imaging. This was further treated with radio frequency ablation. The patient remains well 30 months after surgery.
Case history: two
A 64-year-old man presented with abdominal pain, vomiting and diarrhoea. His past medical history included chronic kidney disease, ulcerative colitis, hypertension and recurrent deep vein thromboses. Abdominal ultrasound and CT identified a mass (14mm x 14mm) in the uncinate process with no distant metastases. The CT and subsequent angiography also demonstrated a tight functional stenosis of the coeliac axis origin (>75% stenosis) with back-filling of the hepatic artery and coeliac axis suggestive of MALS (Fig 3). Endoscopic ultrasound with fine needle aspiration of the mass confirmed a pancreatic endocrine tumour of uncertain malignant potential.
Figure 3.
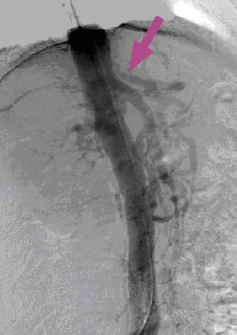
Coeliac axis angiogram in case two, demonstrating coeliac stenosis (black arrow) as a consequence of impingement by the median arcuate ligament
The patient was offered a two-stage procedure: the median arcuate ligament was divided laparoscopically 1 month before definitive surgery. At laparoscopy, dense crura were identified with a tortuous and angulated coeliac artery. The gastrohepatic ligament was divided and the right sided fibres of the diaphragmatic crus were dissected free from the right anterolateral border of the aorta and cleared down to the left renal vein. The origin of the coeliac trunk was cleared completely to remove all median arcuate ligament fibres. Subsequent CT angiography demonstrated improved flow through the coeliac trunk although there was a residual stenosis of 25–50% and a reduction in diameter of the GDA with the inferior pancreaticoduodenal artery remaining prominent (Fig 4). Stenting of the remaining stenosis was not undertaken because of the long-term risk of neointimal hyperplasia.
Figure 4.
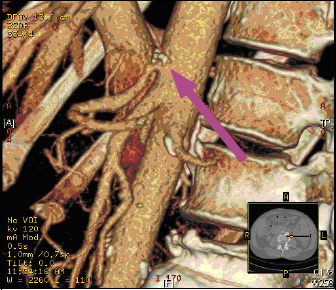
CT angiogram of the aorta showing improved blood flow through the coeliac axis in case two after laparoscopic division of the median arcuate ligament (black arrow)
The patient underwent elective pancreaticoduodenectomy. Good flow through the hepatic artery was confirmed after occlusion and subsequent ligation of the GDA. Post-operatively, there were no signs of hepatic or anastomotic ischaemia although recovery was complicated by grade 2 pancreatic fistula. Histology of the resected pancreas confirmed a well differentiated endocrine tumour confined to the pancreas with a Ki-67 index of <1%, a low mitotic rate and no lymph node involvement (Stage T1, N0, M0, R0). The malignant potential of this tumour remains uncertain.
Discussion
Coeliac artery patency is vital to successful outcome in pancreaticoduodenectomy; impairment of coeliac flow results in potentially catastrophic hepatic and biliary ischaemia. Intraoperative assessment of flow through the hepatic artery is routine in pancreatic resection but may not be reliable. However, if flow is found to be abnormal, the surgeon is posed with a difficult problem. Advances in preoperative imaging have allowed identification of arterial insufficiency prior to surgery.5 Coeliac stenosis is present in 7.6% of patients undergoing pancreaticoduodenectomy, with the majority of cases attributable to MALS.10,11 The first case reports of pancreaticoduodenectomy in the presence of MALS emerged in 1981; these were managed intraoperatively with either median arcuate ligament release or vascular reconstruction.2,12 Since then, advances in cross-sectional imaging and interventional radiology have permitted the preoperative management of MALS using laparoscopic median arcuate ligament release or endovascular angioplasty and stenting. Confirmation of the restoration of coeliac blood flow prior to pancreatic resection may help to reduce post-operative ischaemic complications.
These cases illustrate two different approaches to the preoperative management of MALS in patients who require pancreaticoduodenectomy. Both interventions resulted in successful resection without ischaemic complications and avoided high risk vascular reconstructions. In addition, restoration of coeliac flow was confirmed prior to resection, which simplified surgical planning and reduced the dependence on assessment by palpation of flow through the common hepatic artery on clamping of the GDA. Intraoperative management of MALS in patients undergoing pancreaticoduodenectomy may be dangerous.13 Complications related to revascularisation occurred in 14% of patients, with two incidences of postoperative common hepatic or coeliac artery occlusion following hepatic artery endarterectomy and median arcuate ligament release respectively. There was subsequent biliary anastomotic leak in one patient and the need for endovascular stenting in the other.
There are potential risks associated with the two pre-resection interventions presented here. In the case of endovascular stenting, these include stent occlusion from thrombus or neo-intimal hyperplasia and subsequent haemorrhage from systemic antiplatelet therapy.14 Laparoscopic median arcuate ligament release in accomplished hands may be safer although damage to the aorta and coeliac trunk may theoretically occur. It is also impossible to assess successful recanalisation of the coeliac trunk at the time of laparoscopy, making subsequent intravenous contrast imaging necessary.
The choice between endovascular stenting and laparoscopic median arcuate ligament release in this case series was based on the size of the tumour. Large upper gastrointestinal masses can impede visualisation of the median arcuate ligament on laparoscopy, making endovascular stenting the treatment of choice. The period from diagnosis to definitive resection in our series was also not critical and allowed full investigation and treatment before resection because both patients had endocrine tumours. A similar two-staged approach to pancreaticoduodenectomy would be suitable for the treatment of benign disease such as chronic pancreatitis. However, it may be inappropriate to delay definitive surgery in patients with ductal adenocarcinoma and, in such patients, two-staged management of MALS may be logistically difficult.
Conclusions
MALS presents a unique challenge to pancreaticoduodenectomy and can be successfully managed preoperatively, especially in cases of slow growing pancreatic endocrine tumours. Laparoscopic median arcuate ligament release is best employed in small pancreaticoduodenal tumours, while first-line endovascular stenting should be reserved for larger masses.
References
- 1.Kwon JW, Chung JW, Song SY et al. Transcatheter arterial chemoembolization for hepatocellular carcinomas in patients with celiac axis occlusion. J Vasc Interv Radiol 2002; 13: 689–694. [DOI] [PubMed] [Google Scholar]
- 2.Thompson NW, Eckhauser FE, Talpos G, Cho KJ. Pancreaticoduodenectomy and celiac occlusive disease. Ann Surg 1981; 193: 399–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park CM, Chung JW, Kim HB et al. Celiac axis stenosis: incidence and etiologies in asymptomatic individuals. Korean J Radiol 2001; 2: 8–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pfeiffenberger J, Adam U, Drognitz O et al. Celiac axis stenosis in pancreatic head resection for chronic pancreatitis. Langenbecks Arch Surg 2002; 387: 210–215. [DOI] [PubMed] [Google Scholar]
- 5.Berney T, Pretre R, Chassot G, Morel P. The role of revascularization in celiac occlusion and pancreatoduodenectomy. Am J Surg 1998; 176: 352–356. [DOI] [PubMed] [Google Scholar]
- 6.Gloviczki P, Duncan AA. Treatment of celiac artery compression syndrome: does it really exist? Perspect Vasc Surg Endovasc Ther 2007; 19: 259–263. [DOI] [PubMed] [Google Scholar]
- 7.Mensink PB, van Petersen AS, Kolkman JJ et al. Gastric exercise tonometry: the key investigation in patients with suspected celiac artery compression syndrome. J Vasc Surg 2006; 44: 277–281. [DOI] [PubMed] [Google Scholar]
- 8.Bull DA, Hunter GC, Crabtree TG et al. Hepatic ischemia, caused by celiac axis compression, complicating pancreaticoduodenectomy. Ann Surg 1993; 217: 244–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gaujoux S, Sauvanet A, Vullierme MP et al. Ischemic complications after pancreaticoduodenectomy: incidence, prevention, and management. Ann Surg 2009; 249: 111–117. [DOI] [PubMed] [Google Scholar]
- 10.Kurosaki I, Hatakeyama K, Nihei KE, Oyamatsu M. Celiac axis stenosis in pancreaticoduodenectomy. J Hepatobiliary Pancreat Surg 2004; 11: 119–124. [DOI] [PubMed] [Google Scholar]
- 11.Kohler TR, Debas H, Crames M, Strandness DE Jr. Pancreaticoduodenectomy and the celiac artery compression syndrome. Ann Vasc Surg 1990; 4: 77–80. [DOI] [PubMed] [Google Scholar]
- 12.Fortner JG, Watson RC. Median arcuate ligament obstruction of celiac axis and pancreatic cancer. Ann Surg 1981; 194: 698–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farma JM, Hoffman JP. Nonneoplastic celiac axis occlusion in patients undergoing pancreaticoduodenectomy. Am J Surg 2007; 193: 341–344. [DOI] [PubMed] [Google Scholar]
- 14.Sakorafas GH, Sarr MG, Peros G. Celiac artery stenosis: an underappreciated and unpleasant surprise in patients undergoing pancreaticoduodenectomy. J Am Coll Surg 2008; 206: 349–356. [DOI] [PubMed] [Google Scholar]


