Abstract
Capnograph is an indispensable tool for monitoring metabolic and respiratory function. In this study, the aim was to review the applications of end-tidal carbon dioxide (ETCO2) monitoring in emergency department, multiple databases were comprehensively searched with combination of following keywords: “ETCO2”, “emergency department monitoring”, and “critical monitoring” in PubMed, Google Scholar, Scopus, Index Copernicus, EBSCO and Cochrane Database.
Key Words: Capnography, Emergency service, hospital, exhalation, carbon dioxide, monitoring, physiologic
1. Introduction:
Capnometry, measuring the concentration of carbon dioxide (CO2) in the atmosphere, was used for the first time during World War II as a tool for monitoring the internal environment (1). It was used in medicine for the first time in 1950 to measure the amount of CO2 exhaled during anesthesia. However, it was not used in practice until the early 1980s and with development of smaller machines, capnometry officially entered the anesthesia field (2, 3).
There are two types of capnograph, “side stream” and “mainstream” (4) . In the “mainstream” technique, sampling window is in the ventilator circuit and measures CO2, while in the “side stream”, the gas analyzer is located out of the ventilator circuit. In both types, gas analyzer uses infrared radiation, mass or Raman spectra and a photo acoustic spectra technology (1, 4). Flow measurement equipment is used in volumetric capnograph.
Colorimetric CO2 detector is an example of mainstream form. These devices have a pH sensitive indicator, which changes color in inspiration and expiration. These color changes are in response to CO2 concentration changes. In the presence of a small amount of CO2, the device has a base color, which changes gradually with increase in CO2 concentration (5).
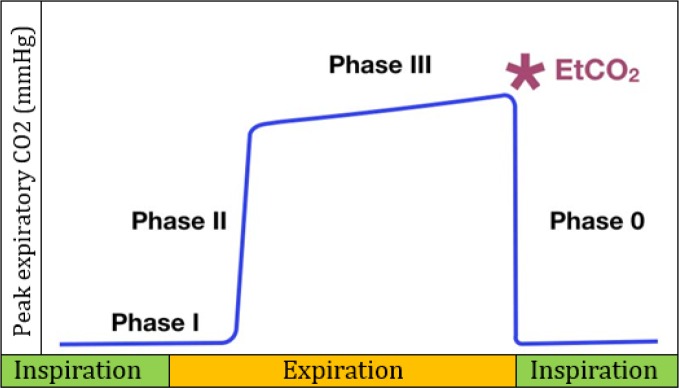
A normal capnograph (Figure 1) has a square-wave pattern, which begins in inspiratory phase (peak expiratory CO2 (PECO2) = 0 mmHg) and will continue until the expiratory phase (6).
Figure 1.
Diagram of a normal capnogram that includes the inspiratory and expiratory phase.
Phase 0 (inspiratory phase): Happens suddenly with an inspiration.
The expiration phase includes three-phases:
Phase I (latency phase): Beginning of expiration, represents anatomical dead space of the respiratory tract and is not discernible from the inspiratory phase before it (PECO2 = 0 mmHg),
Phase II: A very rapid increase in PECO2, which represents exhalation of mixed air.
Phase III (Plateau phase): Reflects the alveolar expiratory flow (a small increase in PECO2), which happens the peak at the end of tidal expiration (ETCO2). In this phase PECO2 is close to alveolar carbon dioxide tension (PACO2).
Emergency physicians are always looking for a non-invasive, reliable instrument to detect life-threatening conditions in patients. One of the methods that have been suggested recently in the emergency department is capnography or ETCO2 monitoring. This study aimed to review the applications of ETCO2 monitoring in emergency department.
2. Evidence Acquisition
A review of the literature was performed in November 2017 to find all previously published articles that included ETCO2 application in the emergency department. The review was done in multiple electronic databases (PubMed, Google Scholar, Scopus, Index Copernicus, EBSCO and Cochrane Database) using key words including ETCO2, emergency department monitoring, and critical monitoring, searching for articles published between 1966 and 2017. In addition, all references cited in these studies were searched for the keywords. All clinical trials, case reports, case series and meta-analyses were reviewed regarding their content. In the initial search, 386 articles were found and 65 articles were eligible to be included in this review
3. ETCO2 Applications
3.1. Cardio Pulmonary Resuscitation (CPR)
ETCO2 concentration is a reliable index of effective heart compression during CPR, which is associated with cardiac output (7, 8). The first sign of the return of spontaneous circulation (ROSC) during CPR is increase in ETCO2, therefore monitoring of ETCO2 provides very useful information to guide treatment during CPR (8-10). ETCO2 is a reliable indicator with a high prognostic value in determining the CPR outcome (11, 12) . Studies have shown that in patients who had ETCO2 of 10 mmHg or less, cardiac arrest was associated with death (13, 14). After 20 minutes of CPR, death occurs if ETCO2 is consistently below 10 mmHg, with 100% sensitivity and specificity (15). ETco2 is more sensitive than cerebral oxygen saturations (rSO2) in ROSC prediction (16).
3.2. Airway assessment
Confirmation of endotracheal intubation is vital in airway management in the emergency department, while there is no definitive diagnostic tool to verify correct intubation in emergency rooms (17). Recently, capnography was used as the gold standard for confirming the correct location of the endotracheal tube (18, 19). Colorimetric ETCO2 is a safe, reliable, simple and portable tool to determine the proper placement of endotracheal tube in patients with stable hemodynamic and it is very useful when a capnograph is not available (20) . However, when patients have a bag or mask ventilation or consume carbonated beverages or antacids it can cause a false positive result, yet it usually indicates the true result after 6 breaths (21). The use of sodium bicarbonate leads to a higher level of ETCO2 for 5 to 10 minutes (22). During a cardiac arrest, which leads to decrease in tissue-pulmonary CO2 transportation, capnography can show a correct intubation as a wrong one (false negative)(23).
3.3. Procedural sedation and analgesia
Capnography is an effective method to diagnose early respiratory depression and airway disorders, especially during sedation, leading to a reduction in serious complications (23, 24). Capnography provided more safety in monitoring patients during sedation. Oxygen prescription does not have an effect on respiratory function parameters evaluated by capnography (25). It shows impaired airway function sooner than any other device, 5 to 240 seconds earlier than pulse oximetry (26, 27). Capnography is more sensitive than clinical evaluation in diagnosis of respiratory dysfunction, for instance, in many cases where apnea was experienced during sedation, doctors at the bedside did not recognize the apnea but capnography could identify it (28).
3.4. Pulmonary disease
3.4.1. Obstructive pulmonary disease
In obstructive airway diseases, hypoventilation can cause shortness of breath and hypercarbia (29). There is a relationship between ETCO2 and partial arterial carbon dioxide (PaCO2) in patients with acute asthma in the emergency department (30, 31). Capnography is dynamic monitoring of patients with acute respiratory distress conditions such as asthma, chronic obstructive pulmonary disease (COPD), bronchiolitis, and heart failure (32). Bronchospasm is associated with a prolonged expiratory phase (E1, E2, E3) in capnogram (Figure 1) in patients with obstructive diseases such as COPD (32, 33). Changes in ETCO2 and expiratory phase slope correlated with (E1, E2, E3) forced expiratory volume in 1 second (FEV1) and Peak expiratory flow rate (PEFR) (32, 34). ETCO2 is an indispensable tool in assessing the severity of obstructive respiratory disease in the emergency department. ETCO2 is higher in patients with COPD exacerbation who are admitted to the hospital compared to those who are discharged from the emergency department (35).
3.4.2. Pulmonary embolism
In thromboembolism, ETCO2 is significantly lower than normal due to the reduction of pulmonary perfusion and increased alveolar dead space that reduces the amount of CO2 exhaled from the lungs, so venous carbon dioxide pressure (PvCO2) increases and all of these changes lead to an increase in arterial CO2-ETCO2 gradient (36). This helps in correctly diagnosing pulmonary embolism, especially silent pulmonary embolism (37). Volumetric capnography is used for monitoring of thrombolysis in large pulmonary embolism (38). The average value of ETCO2 and decrease in PCO2 / PO2 pressure for 30 seconds correlates with clinical probability or rule out of pulmonary embolism (39).
3.5. Heart failure
Rapid differentiation of heart failure as the cause of dyspnea from other respiratory causes, is very important for choosing an appropriate therapy (40). Sometimes distinguishing COPD / asthma exacerbation and acute heart failure is very difficult, especially when both exist together, and treatment decisions in this situation are very complex (41). ETCO2 in patients with cardiac causes is markedly different from patients with respiratory distress due to obstructive causes. ETC02 level > 37 mmHg was not observed in any patient with heart failure, although ETC02 level > 37 mmHg has a slight sensitivity for diagnosis of COPD / asthma (42, 43). ETCO2 level during cardiopulmonary exercise testing in patients with heart failure has high prognostic value for cardiac events (44, 45). N-Terminal Pro- brain Natriuretic Peptide on the side of quantitative capnography is very useful in early diagnosis and treatment of patients with acute dyspnea (respiratory or cardiac causes) in emergency departments. The widespread use of quantitative capnography can be beneficial in everyday work for emergency physicians (46).
3.6. Shock
Hypotensive shock is a clinical feature for many diseases and is related to high mortality rate in emergency departments. Emergency physicians continuously strive to find new ways to diagnose early-stage shock to start treatment as soon as possible (47). Capnography is considered as a simple and non-invasive method to detect and estimate shock intensity in the early stage (48, 49). ETCO2 is known to be decreased in volume-related hypotensive states (50). ETCO2 has a correlation with blood pressure, serum lactate and base excess. In early-stage shock that is linked to reduced cardiac output, the amount of ETCO2 significantly decreases. This is due to decreased blood flow in the pulmonary artery during the cardiac output reduction, which disrupts ventilation perfusion ratio. With increase in shunt ETCO2 level decreases, while PaCO2 does not change (51, 52). With decrease in blood pressure, ETCO2 drops and PaCO2-ETCO2 gradient increases (53, 54). There is a correlation between the amount of dehydration and the amount of sodium bicarbonate and ETCO2, and ETCO2 can be used as a simple and non-invasive indicator for determination of dehydration (55).
3.7. Metabolic disorder
Carbon dioxide (CO2) is one of the final products of metabolism and is transferred to lungs through the blood circulation and transmitted through respiratory system, so exhaling CO2 reflects the body’s metabolic status (56, 57). ETCO2 is a fast, inexpensive and non-invasive indicator to estimate the amount of HCO3- bicarbonate and PaCO2 in emergency and critical situations (58). Due to the direct connection between ETCO2 and HCO3, ETCO2 is a predictor of metabolic acidosis and mortality, so capnograph as a screening tool for metabolic acidosis is very useful in the emergency department (59) . ETCO2 can be recommended as a noninvasive method for determination of metabolic acidosis and can be used to detect early metabolic acidosis in patients with spontaneous breathing, however, ABG should be used as the gold standard for diagnosis and management of treatment (60).
3.7.1. Diabetic keto acidosis (DKA)
Patients with diabetes mellitus are at increased risk of major and disabling complications, one of the most important of which is DKA (61). The Direct linear relationship between ETCO2 and HCO3 is useful in prediction of acidosis. It was shown that there is no DKA diagnosis when ETCO2 ˃ 36, and there is DKA diagnosis when ETCO2 ≤ 29. ETCO2 30 to 35 is considered as the cut –point, so it is clinically useful in diagnosis of acidosis (62, 63). In addition, a low PaCO2 level is correlated with increased risk of cerebral edema in children with DKA (64). Thus, according to the relationship between ETCO2 and PaCO2, capnography can be used to identify individuals with high risk of cerebral edema (62). When the patient's glucose is above 550 mg/dl, ETCO2 is a useful tool to rule out the DKA (65).
3.7.2. Gastroenteritis
Among children with diarrhea and vomiting, ETCO2 is independently correlated with serum HCO3 concentration. This is a non-invasive index for measuring the severity of acidosis in patients with gastroenteritis (66). ETCO2 can be used to estimate HCO3 in many emergency situations(58).
3.8. Trauma
End-tidal carbon dioxide cannot be used to rule out severe injury in patients meeting the criteria for trauma care. ETCO2 ≤30 mmHg may be associated with increased risk of traumatic severe injury (67).
There is a reverse relationship between pre-hospital ETCO2 and traumatic mortality rates, so ETCO2 can be used to improve triage and also helps the emergency medical service staff in planning for the transfer of patients to the appropriate trauma center (68).
Low ETCO2 has a strong association with shock in patients with trauma and suggests the severity of the patient's condition in the first 6 hours of admission (69).
4. Conclusion:
ETCO2 is used in the emergency department as an indicator for measurement in many clinical situations. Capnography is a non-invasive and accurate method to measure ETCO2 and can help emergency physicians in some critical situations. Although this is not used in many emergency situations and it is not used routinely in the emergency department, its application is increasing in many emergency situations, such as patients undergoing mechanical ventilation, procedural sedation and analgesia, pulmonary disease, heat failure, shock, metabolic disorder and trauma. This means that capnography must be considered as an essential tool in emergency department, however, more researches are needed to evaluate its application in specific clinical conditions and diseases.
Acknowledgment
None
Author’ Contributions
Conception and design, collection of data and writing of the manuscript: Hamed Aminiahidashti; Conception and design, and data interpretation: Mohammad Sazgar and Sajad Shafiee; Conception and design, and critical revision of the manuscript: Alieh Zamani Kiasari.
Funding:
None
Conflict of interest
We declare no conflict of interest with any financial organization regarding the material discussed in the manuscript.
References
- 1.O'Flaherty . Capnography: principles and practice. London: BMJ Publishing Group; 1994. [Google Scholar]
- 2.Smalhout B KZ. An atlas of capnography. Amsterdam: Kerchebosch-Zeist; 1981. [Google Scholar]
- 3.M W. Respiratory monitoring: a ten year perspective. J Clin Monit. 1990;6:217. doi: 10.1007/BF02832150. [DOI] [PubMed] [Google Scholar]
- 4.Block FE, Jr MJ. Sidestream versus mainstream carbon dioxide analyzers. J Clin Monit. 1992;8(2):139–41. doi: 10.1007/BF01617434. [DOI] [PubMed] [Google Scholar]
- 5.Garey DM WR, Rich W, Heldt G, Leone T, Finer NN. T idal volume threshold for colorimetric carbon dioxide detectors available for use in neonates. Pediatrics . 2008;21(6):1524–7. doi: 10.1542/peds.2007-2708. [DOI] [PubMed] [Google Scholar]
- 6.Berengo A C. Single-breath analysis of carbon dioxide concentration records. J Appl Physiol. 1961;16:522–30. [Google Scholar]
- 7.Falk JL RE, Weil MH. End-tidal carbon dioxide concentration during cardiopulmonary resuscitation. N Engl J Med. 1989;318:607–11. doi: 10.1056/NEJM198803103181005. [DOI] [PubMed] [Google Scholar]
- 8.Garnett AR OJ, Gonzalez ER, Johnson EB. End-tidal carbon dioxide monitoring during cardiopulmonary resuscitation. JAMA. 1987;257:512–5. [PubMed] [Google Scholar]
- 9.Ahrens T ea. End-tidal carbon dioxide measurements as a prognostic indicator of outcome in cardiac arrest. Am J Crit Care. 2001;10:391–8. [PubMed] [Google Scholar]
- 10.Ornato JP GE, Garnett AR, Levine RL, McClung BK. Effect of cardiopulmonary resuscitation compression rate on end-tidal carbon dioxide concentration and arterial pressure in man. Crit Care Med. 1988;16:241–5. doi: 10.1097/00003246-198803000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Cantineau JP ea. End-tidal carbon dioxide during cardiopulmonary resuscitation in humans presenting mostly with asystole: A predictor of outcome. Crit Care Med. 1996;24:791–6. doi: 10.1097/00003246-199605000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Pokorná M AM, Necas E. End tidal CO2 monitoring in condition of constant ventilation: a useful guide during advanced cardiac life support. Prague Med Rep. 2006;107(3):317–26. [PubMed] [Google Scholar]
- 13.Callaham M BC. Prediction of outcome of cardiopulmonary resuscitation from end-tidal carbon dioxide concentration. Crit Care Med. 1990;18:358–62. doi: 10.1097/00003246-199004000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Cantineau JP MP, Lambert Y, Sorkine M, Bertrand C, Duvaldestin P. Effect of epinephrine on end-tidal carbon dioxide pressure during prehospital cardiopulmonary resuscitation. Am J Emerg Med. 1994;12:267–70. doi: 10.1016/0735-6757(94)90136-8. [DOI] [PubMed] [Google Scholar]
- 15.Levine RL WM, Miller CC. End-tidal carbon dioxide and outcome of out-of-hospital cardiac arrest. N Engl J Med. 1997;337:301–6. doi: 10.1056/NEJM199707313370503. [DOI] [PubMed] [Google Scholar]
- 16.Cournoyer A, Iseppon M, Chauny JM, Denault A, Cossette S, Notebaert É. Near‐infrared Spectroscopy Monitoring During Cardiac Arrest: A Systematic Review and Meta‐analysis. Academic Emergency Medicine. 2016;23(8):851–62. doi: 10.1111/acem.12980. [DOI] [PubMed] [Google Scholar]
- 17.Ma G DD, Schmitt J, Vilke GM, Chan TC, Hayden SR. the sensitivity and specificity of transcricothyroid ultrasonography to confirm endotracheal tube placement in a cadaver model. J Emerg Med. 2007 ;32(4):405–7. doi: 10.1016/j.jemermed.2006.08.023. [DOI] [PubMed] [Google Scholar]
- 18.Turle S SP, Nicholson S, Callaghan T, Shepherd SJ. Availability and use of capnography for in-hospital cardiac arrests in the United Kingdom. Resuscitation. 2015 ;94:80–4. doi: 10.1016/j.resuscitation.2015.06.025. [DOI] [PubMed] [Google Scholar]
- 19.Š G. Comparison of three different methods to confirm tracheal tube placement in emergency intubation. Intensive Care Med. 2002;28:701–4. doi: 10.1007/s00134-002-1290-x. [DOI] [PubMed] [Google Scholar]
- 20.Goldberg JS RP, Zehnder JL, Sladen RN. Colorimetric end-tidal carbon dioxide monitoring for tracheal intubation. Anesth Analg. 1990 ;70(2):191–4. doi: 10.1213/00000539-199002000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Garnett AR GC, Gervin AS. Capnographic waveforms in esophageal intubation: Effect of carbonated beverages. Ann Emerg Med. 1989;18:387–90. doi: 10.1016/s0196-0644(89)80576-1. [DOI] [PubMed] [Google Scholar]
- 22.Okamoto H HS, Kawasaki T, Okuyama T, Takahashi S. Changes in end-tidal carbon dioxide tension following sodium bicarbonate administration: Correlation with cardiac output and haemoglobin concentration. Acta Anaesthesiol Scand. 1995;39:79–84. doi: 10.1111/j.1399-6576.1995.tb05596.x. [DOI] [PubMed] [Google Scholar]
- 23.B K. Capnography as a rapid assessment and triage tool for chemical terrorism. Pediatr Emerg Care. 2005;21:493–7. doi: 10.1097/01.pec.0000173345.07530.c0. [DOI] [PubMed] [Google Scholar]
- 24.Adams L BS, Spurlock D Jr. Capnography (ETCO2), respiratory depression, and nursing interventions in moderately sedated adults undergoing transesophageal echocardiography (TEE) J Perianesth Nurs. 2015 ;30(1):14–22. doi: 10.1016/j.jopan.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 25.Mora Capín A MNC, López López R, Marañón Pardillo R. Usefulness of capnography for monitoring sedoanalgesia: influence of oxygen on the parameters monitored. An Pediatr (Barc) 2014;80(1):41–6. doi: 10.1016/j.anpedi.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 26.Burton JH HJ, Germann CA, Dillon DC. Does end-tidal carbon dioxide monitoring detect respiratory events prior to current sedation monitoring practices? Acad Emerg Med. 2006;13:500–504. doi: 10.1197/j.aem.2005.12.017. [DOI] [PubMed] [Google Scholar]
- 27.Deitch K MJ, Chudnofsky CR, Dominici P, Latta D. Does end tidal CO2 monitoring during emergency department procedural sedation and analgesia with propofol decrease the incidence of hypoxic events? A randomized, controlled trial. Ann Emerg Med. 2010;55:258–264. doi: 10.1016/j.annemergmed.2009.07.030. [DOI] [PubMed] [Google Scholar]
- 28.Soto RG FE, Vila H Jr, Miguel RV. Capnography accurately detects apnea during monitored anesthesia care. Anesth Analg. 2004;99:379–82. doi: 10.1213/01.ANE.0000131964.67524.E7. [DOI] [PubMed] [Google Scholar]
- 29.Hawkins NM PM, Pardeep SJ, et al. Heart failure and chronic obstructive pulmonary disease: diagnostic pitfalls and epidemiology. Eur J Heart Failure. 2009;11:130–9. doi: 10.1093/eurjhf/hfn013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Corbo J BP, Lahn M, et al. Concordance between capnography and arterial blood gas measurements of carbon dioxide in acute asthma. Ann Emerg Med. 2005;46:323–327. doi: 10.1016/j.annemergmed.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 31.Cinar O AY, Arziman I, et al. Can mainstream end-tidal carbon dioxide measurement accurately predict the arterial carbon dioxide level of patients with acute dyspnea in ED. Am J Emerg Med. 2012;30:358–361. doi: 10.1016/j.ajem.2010.12.014. [DOI] [PubMed] [Google Scholar]
- 32.Krauss B ea. Capnogram shape in obstructive lung disease. Anesth Analg. 2005;100:884–8. doi: 10.1213/01.ANE.0000146520.90393.91. [DOI] [PubMed] [Google Scholar]
- 33.Krauss B HD. Capnography for procedural sedation and analgesia in the emergency department. Ann Emerg Med. 2007;50:172–81. doi: 10.1016/j.annemergmed.2006.10.016. [DOI] [PubMed] [Google Scholar]
- 34.Yaron M PP, Hutsinpiller M, Cairns CB. Utility of the expiratory capnogram in the assessment of bronchospasm. Ann Emerg Med. 1996;28:403–7. doi: 10.1016/s0196-0644(96)70005-7. [DOI] [PubMed] [Google Scholar]
- 35.Doğan NÖ ŞA, Günaydın GP, İçme F, Çelik GK, Kavaklı HŞ, Temrel TA. T he accuracy of mainstream end-tidal carbon dioxide levels to predict the severity of chronic obstructive pulmonary disease exacerbations presented to the ED. Am J Emerg Med. 2014 ;32(5):408–11. doi: 10.1016/j.ajem.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 36.Anderson C T BPH. Carbon dioxide kinetics and capnography during critical care. Crit Care Med. 2000;4:207–15. doi: 10.1186/cc696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Taniguchi S IK, Sakaguchi Y, et al. Capnometry as a tool to unmask silent pulmonary embolism. Tohoku J Exp Med. 1997;183(4):263–71. doi: 10.1620/tjem.183.263. [DOI] [PubMed] [Google Scholar]
- 38.Verschuren F HE, Clause D, Roeseler J, Thys F, Meert P, Marion E, El Gariani A, Col J, Reynaert M, Liistro G. Volumetric capnography as a bedside monitoring of thrombolysis in major pulmonary embolism. Intensive Care Med. 2004 ;30(11):2129–32. doi: 10.1007/s00134-004-2444-9. [DOI] [PubMed] [Google Scholar]
- 39.Kline JA HM. Measurement of expired carbon dioxide, oxygen and volume in conjunction with pretest probability estimation as a method to diagnose and exclude pulmonary venous thromboembolism. Clin Physiol Funct Imaging. 2006 ;26(4):212–9. doi: 10.1111/j.1475-097X.2006.00672.x. [DOI] [PubMed] [Google Scholar]
- 40.Stiell IG SD, Field B, Nesbitt LP, Munkley D, Maloney J, Dreyer J, Toohey LL, Campeau T, Dagnone E, Lyver M, Wells GA OPALS Study Group, authors. Advanced life support for out-of-hospital respiratory distress. N Engl J Med. 2007;356(21):2156–64. doi: 10.1056/NEJMoa060334. [DOI] [PubMed] [Google Scholar]
- 41.Macchia A MS, Romero M, D'Ettorre A, Tognoni G. The prognostic influence of chronic obstructive pulmonary disease in patients hospitalised for chronic heart failure. Eur J Heart Fail. 2007;9(9):942–8. doi: 10.1016/j.ejheart.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 42.Brown LH GJ, Seim RH. Can quantitative capnometry differentiate between cardiac and obstructive causes of respiratory distress? Chest. 1998;113(2):323–6. doi: 10.1378/chest.113.2.323. [DOI] [PubMed] [Google Scholar]
- 43.Grmec Š GM, Klemen P, Cander D. Utility of the quantitative capnometry (QC) and rapid bedside test for N-terminal pro-brain natriuretic peptide (pro-BNP) in the evaluation of respiratory distress in prehospital setting - preliminary results. J Emerg Med. 2007;33(3):322. [Google Scholar]
- 44.Arena R GM, Myers J. Prognostic value of end-tidal carbon dioxide during exercise testing in heart failure. Int J Cardiol. 2007;117(1):103–8. doi: 10.1016/j.ijcard.2006.04.058. [DOI] [PubMed] [Google Scholar]
- 45.Arena R GM, Myers J, Chase P, Bensimhon D, Cahalin LP, Peberdy MA, Ashley E, West E, Forman Prognostic value of capnography during rest and exercise in patients with heart failure. Congest Heart Fail. 2012;18(6):230–307. doi: 10.1111/j.1751-7133.2012.00296.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Klemen P GM, Grmec S. Combination of quantitative capnometry, N-terminal pro-brain natriuretic peptide, and clinical assessment in differentiating acute heart failure from pulmonary disease as cause of acute dyspnea in pre-hospital emergency setting: study of diagnostic accuracy. Croat Med J. 2009 50(2):133–42. doi: 10.3325/cmj.2009.50.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Emanuel RM P, Bryant Nguyenn H. A Comprehensive Study Guide. In: Tintinalli JE KG SJ, editor. Emergency Medicine. New York: McGraw-Hill, Inc; 2004. [Google Scholar]
- 48.Weil MH NY, Tang W, Sato Y, Ercoli F, Finegan R, Grayman G, Bisera J. Sublingual capnometry: a new noninvasive measurement for diagnosis and quantitation of severity of circulatory shock. Crit Care Med. 1999 27(7):1225–9. doi: 10.1097/00003246-199907000-00001. [DOI] [PubMed] [Google Scholar]
- 49.Rackow EC ONP, Astiz ME, Carpati CMS. ublingual capnometry and indexes of tissue perfusion in patients with circulatory failure. Chest. 2001;120(5):1633–88. doi: 10.1378/chest.120.5.1633. [DOI] [PubMed] [Google Scholar]
- 50.Hemnes AR NA, Rosenbaum B, Barrett TW, Zhou C, Rice TW, Newman JH. Bedside end tidal CO2 as a screening tool to exclude pulmonary embolism. EurRespir J. 2010;35(4):735–41. doi: 10.1183/09031936.00084709. [DOI] [PubMed] [Google Scholar]
- 51.Kheng CP RN. The use of end-tidal carbon dioxide monitoring in patients with hypotension in the emergency department. International Journal of Emergency Medicine. 2012;5(1):31. doi: 10.1186/1865-1380-5-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.DMello J BM. Capnography. Indian J Anesth. 2002;46(4):269–78. [Google Scholar]
- 53.Syed Shujat A AD, Abdul Raheem al Gattan. The relationship between end tidal carboon dioxide and urterial carbon dioxide during controlled hypotensice anesthesia. Med principles pact. 2002;11:35–7. doi: 10.1159/000048658. [DOI] [PubMed] [Google Scholar]
- 54.Mahoori A HE, Mehdizadeh H, Nanbakhsh N. the effects of blood pressure variations on end-tidal and arterial CO2 pressure differences in patients undergoing coronary artery bypass graft. Journal of Iranian Society of Anesthesiology and Intensive Care. 2014;36(85):3–9. [Google Scholar]
- 55.Yang HW, Jeon W, Min YG, Lee JS. Usefulness of end-tidal carbon dioxide as an indicator of dehydration in pediatric emergency departments: A retrospective observational study. Medicine. 2017;96(35) doi: 10.1097/MD.0000000000007881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.BS K. Capnography outside the operating rooms. Anesthesiology. 2013;118:192–201. doi: 10.1097/ALN.0b013e318278c8b6. [DOI] [PubMed] [Google Scholar]
- 57.Rafael O CC, Sora K, et al. Monitoring Ventilation with Capnography. N Eng J Med. 2012:367. doi: 10.1056/NEJMvcm1105237. [DOI] [PubMed] [Google Scholar]
- 58.Pishbin E AG, Sharifi MD, Deloei MT, Shamloo AS, Reihani H. The correlation between end-tidal carbon dioxide and arterial blood gas parameters in patients evaluated for metabolic acid-base disorders. Electron Physician. 2015;7(3):1095–101. doi: 10.14661/2015.1095-1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kartal M EO, Rinnert S, Goksu E, Bektas F, Eken C. ETCO₂. a predictive tool for excluding metabolic disturbances in nonintubated patients. Am J Emerg Med;29(1):65–9. doi: 10.1016/j.ajem.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 60.Taghizadieh A, Pouraghaei M, Moharamzadeh P, Ala A, Rahmani F, Sofiani KB. Comparison of end-tidal carbon dioxide and arterial blood bicarbonate levels in patients with metabolic acidosis referred to emergency medicine. Journal of cardiovascular and thoracic research. 2016;8(3):98. doi: 10.15171/jcvtr.2016.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Losman ED, Weakness . In: Rosen’s Emergency Medicine. A MJ, editor. Philadelphia: Mosby; 2010. pp. 87–92. [Google Scholar]
- 62.Fearon DM SD. End-tidal carbon dioxide predicts the presence and severity of acidosis in children with diabetes. Acad Emerg Med. 2002 (12):1373–8. doi: 10.1111/j.1553-2712.2002.tb01605.x. [DOI] [PubMed] [Google Scholar]
- 63.Soleimanpour H TA, Niafar M, Rahmani F, Golzari SE, Esfanjani RM. Predictive value of capnography for suspected diabetic ketoacidosis in the emergency department. West J Emerg Med. 2013;14(6):590–4. doi: 10.5811/westjem.2013.4.14296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Glaser NS BP, McCaslin I, et al. Risk factors for cerebral edema in children with diabetic ketoacidosis. N Engl J Med. 2001;344:264–9. doi: 10.1056/NEJM200101253440404. [DOI] [PubMed] [Google Scholar]
- 65.Chebl RB, Madden B, Belsky J, Harmouche E, Yessayan L. Diagnostic value of end tidal capnography in patients with hyperglycemia in the emergency department. BMC emergency medicine. 2016;16(1) doi: 10.1186/s12873-016-0072-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nagler J WR, Krauss B. End-tidal carbon dioxide as a measure of acidosis among children with gastroenteritis. Pediatrics. 2006;118(1):260–7. doi: 10.1542/peds.2005-2723. [DOI] [PubMed] [Google Scholar]
- 67.Williams DJ, Guirgis FW, Morrissey TK, Wilkerson J, Wears RL, Kalynych C, et al. End-tidal carbon dioxide and occult injury in trauma patients: ETCO2 does not rule out severe injury. The American journal of emergency medicine. 2016;34(11):2146–9. doi: 10.1016/j.ajem.2016.08.007. [DOI] [PubMed] [Google Scholar]
- 68.Childress K, Arnold K, Hunter C, Ralls G, Papa L, Silvestri S. Prehospital End-tidal Carbon Dioxide Predicts Mortality in Trauma Patients. Prehospital Emergency Care. 2017:1–5. doi: 10.1080/10903127.2017.1356409. [DOI] [PubMed] [Google Scholar]
- 69.Stone ME, Kalata S, Liveris A, Adorno Z, Yellin S, Chao E, et al. End-tidal CO 2 on admission is associated with hemorrhagic shock and predicts the need for massive transfusion as defined by the critical administration threshold: A pilot study. Injury. 2017;48(1):51–7. doi: 10.1016/j.injury.2016.07.007. [DOI] [PubMed] [Google Scholar]