Abstract
Aim: The association of social networks with cardiovascular disease (CVD) has been demonstrated through various studies. This study aimed to examine the association between social network betweenness–a network position of mediating between diverse social groups–and coronary artery calcium.
Methods: The data of 1,384 participants from the Cardiovascular and Metabolic Disease Etiology Research Center–High Risk Cohort, a prospective cohort study enrolling patients with a high risk of developing CVD (clinicaltrials.gov: NCT02003781), were analyzed. The deficiency in social network betweenness was measured in two ways: only-family networks, in which a respondent had networks with only family members, and no-cutpoint networks, in which the respondent does not function as a point of bridging between two or more social groups that are not directly connected.
Results: Participants who had higher coronary artery calcium scores (CACSs) were likely to have a smaller network size (p < 0.001), only-family networks (p < 0.001), and no-cutpoint networks (p < 0.001). Multiple logistic regression analyses revealed no significant association between network size and CACS. Only no-cutpoint networks had a significant relationship with CACS > 400 (odds ratio, 1.72; 95% confidence interval, 1.07–2.77; p = 0.026). The association was stronger among older (age > 60 years) and female respondents.
Conclusion: Deficiency in social network betweenness is closely related to coronary calcium in participants with a high risk of CVD. To generalize these results to a general population, further study should be performed.
Keywords: Coronary calcium score, Social networks, Cardiovascular disease, Risk factor
See editorial vol. 25: 124–125
Introduction
Social networks have been considered as an important social factor associated with cardiovascular disease (CVD) in terms of social contacts, social support, or social isolation1). A recent meta-analysis showed that the function of social networks (content provided by social networks, such as emotional or instrumental support) strongly affected the onset and development of CVD; however, there is little evidence on the effects of the structure of social networks (objective features of social networks, such as frequency of contacts or network size)2). Despite the varied results concerning network structure, investigation of the detailed features of network structure has been consistently demanded because these determine the potential role and function of social networks3).
Social network betweenness is a network structure in which a member can indirectly bridge between two or more social actors or groups that have no direct social connections to each other4). For example, a person who maintains intimate relationships with the two social groups of neighbors and university alumni can better take advantage of social networks than those connected with only neighbors or only alumni, because this person can (i) draw more diverse resources and information from people of two different backgrounds, and (ii) feel a sense of freedom from crossing over various social groups5). Whereas a few studies have examined the social determinants of coronary artery calcium, such as psychosocial stress6) or marital status7), there were no research that explicitly examined the relationship to structural features of social networks. By adopting an elaborate social network module that reveals thorough information about a person's important social network members, we investigated the association between social network structure and coronary artery calcium, with a focus on the limitations in social network betweenness.
Methods
Study Population
This study analyzed the data from Cardiovascular and Metabolic Disease Etiology Research Center–High Risk Cohort (CMERC-HI). Briefly, CMERC-HI is a prospective cohort study aimed at developing more specific preventive strategies for patients with a high risk of CVD (clinicaltrials.gov NCT02003781). The inclusion criteria of the cohort were as follows: high-risk patients with hypertension [estimated glomerular filtration rate (eGFR) > 60 mL/min/1.73 m2) with target organ damage, or eGFR ≤ 60 mL/min/1.73 m2]; patients with diabetes mellitus with albuminuria; anuric patients with end-stage renal disease (ESRD) who were undergoing dialysis; relatives of patients with acute myocardial infarction (men < 55 years old; women < 65 years old); patients with asymptomatic atherosclerotic CVD (abdominal aorta diameter ≥ 3 cm or ankle-brachial index < 0.9, or carotid plaque or carotid intima-media thickness ≥ 0.9 mm, or asymptomatic old cerebrovascular accident, or > 30% stenosis in at least one major coronary artery); patients with rheumatoid arthritis aged > 40 years and taking methotrexate and steroid; patients with atrial fibrillation with CHA2DS2-VASc score ≥ 1; and kidney transplant recipients at > 3 months after transplantation. People aged > 20 years who met at least one of the inclusion criteria were enrolled. The exclusion criteria were as follows: a history of acute coronary syndrome; symptomatic coronary artery disease or symptomatic peripheral; heart failure; with a life expectancy of < 6 months; pregnant women; a history of contrast allergy and related adverse effects. A total of 1,958 participants were enrolled from November 2013 to May 2016 at the Severance Hospital in Seoul, Republic of Korea. The Institutional Review Board of the Yonsei University Health System Clinical Trial Center approved the study protocol (4-2013-0581), and written informed consent was obtained from all participants. Among the participants, 312 did not undergo a coronary artery calcium scanning, and 16 did not participate in the social network survey or provided incomplete information about their networks. After excluding 23 participants with missing values in socio-economic status, 20 in health behaviors or medical history, and 213 in laboratory analyses (203 with missing lipid profile data), we examined 1,384 participants in the final analyses.
Social Network Betweenness
The CMERC adopted a social network module called name generator from a nationwide study in the United States8). The Korean version of name generator has been used in nationwide social surveys in South Korea9), and proved to capture important network properties for health in a comparative study of the USA and South Korea10). The module started as follows: “From time to time, most people discuss things that are important to them with others. For example, these may include good or bad things that happen to you, problems you are having, or important concerns you may have. Looking back over the last 12 months, who are the people with whom you most often discussed things that were important to you?” The participants listed the real names of up to five people, and reported the type of relationship with each person (e.g., spouse, child, neighbor). The participants also reported the emotional closeness between network members within each pair (“How emotionally close are NAME1 and NAME2 to each other?”) on a five-level scale (do not know each other, not close, somewhat close, very close, or very much close).
Fig. 1 illustrates two possible networks, where circles represent participants, squares represent social network members from a family (e.g., parent, child, relative), diamonds represent non-family network members (e.g., friend, neighbor), and lines show the social connections. Network size was defined as the total number of social network members. A and B have five network members each; thus, their network size is 5. The deficiency in social network betweenness was measured by using two binary indicators. First, if a participant did not enumerate any non-family members in his or her network list, he or she was considered to have only-family (OF) networks. Compared with A's networks of three family members [a1, a2, a3] and two non-family members [a4, a5], B's networks are limited in the family. Participants who listed no social network member were assumed to have OF networks in this study. Second, if a respondent did not function as a cutpoint of his or her networks, he or she was considered to have no-cutpoint (NC) networks. In network theory, a cutpoint is a person whose deletion breaks up the remaining group into two or more disconnected pieces11). A's networks show an example of NC networks: A's network members are all connected to at least one other network member even when respondent A is missing, whereas B's networks are divided into the two groups of [b1, b5] and [b2, b3, b4] when respondent B is deleted. Participants who listed no or only one social network member cannot act as a cutpoint so were categorized into a NC network group. When counting the number of groups in networks, we only considered very close or very much close social connections among network members. Those who have OF or NC networks are expected to have little diversity in their social interactions, and little potential to draw resources from different social pools.
Fig. 1.
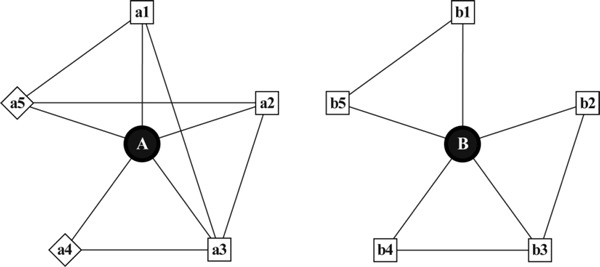
Two possible social networks. Circles represent participants, squares represent social network members from a family (e.g., parent, child, relative), diamonds represent non-family network members (e.g., friend, neighbor), and lines show the social connections. Network size was defined as the total number of social network members. Only-family networks (OF) do not include any non-family member. Compared to A's networks, B's networks are limited in the family. A cutpoint is a person whose deletion breaks up the remaining group into two or more disconnected pieces. If a respondent did not function as a cutpoint of his or her networks, he or she was considered to have no-cutpoint (NC) networks. A's networks show an example of NC networks: A's network members are all connected to at least one other network member even when respondent A is missing, whereas B's networks are divided into the two groups of [b1, b5] and [b2, b3, b4] when respondent B is deleted.
Acquisition of Computed Tomographic Images for Coronary Artery Calcium and Image Analysis
The patients were scanned by using a 320-detector row computed tomography (CT) scanner (Aquillion ONE; Toshiba Medical Systems Corporation, Tokyo, Japan). A non-enhanced prospective electrocardiogramgated CT scan was performed to measure the coronary artery calcium score (CACS) with the following parameters: rotation time 275 ms, slice collimation 0.5 mm, slice thickness 3.0 mm, tube voltage 100 kV, and automatic tube current modulation (SURE Exposure 3D standard; Toshiba Medical Systems Corporation, Otawara, Japan). Images were analyzed in a core workstation by using dedicated software (TeraRecon V. 4.4.11.82.3430.Beta, Foster City, CA, USA). CACS was calculated by using the Agatston method12, 13).
Statistical Analysis
The participants were divided into four groups according to CACS, as follows: (i) 0, (ii) 1–100, (iii) 101–400, and (iv) > 400. Bivariate relationships were considered among CACS and various characteristics. Continuous variables were expressed as mean ± SD, and compared by using one-way analysis of variance (ANOVA). Categorical variables were expressed as number and percentage, and compared with the chisquare test. In multiple logistic regression analyses, the odds of CACS > 400 were computed according to network size and deficiency in network betweenness with covariates of age, sex, smoking, history of hypertension, history of diabetes, ESRD, exercise assessed by using the International Physical Activity Questionnaire14), depression assessed with Beck Depression Inventory15), statin use, body mass index (BMI), systolic blood pressure (SBP), low-density lipoprotein (LDL) cholesterol, triglyceride, fasting glucose, eGFR, level of education, household income, working status, marital status, and number of co-habitants. Five models were examined with different sets of social network variables: model 1 with network size; model 2 with network size and OF networks; model 3 with network size and NC networks; model 4 with network size, OF, and NC networks; and model 5 with three dummy variables for those who had OF networks alone, NC networks alone, and both OF and NC networks. Based on the results from model 5, we also did the Wald test (H0: βOF alone + βNC alone = β OF + NC) to examine if there was a multiplicative association of OF and NC networks. If the sum of coefficients for OF alone and NC alone is significantly larger than that for both OF and NC, the association can be considered multiplicative. Using subsamples of age ≤ 60 years, age > 60 years, male, or female, we re-examined models 2 and 3 and reported the ORs for OF networks and NC networks as figures. Additionally, we considered several models to address the robustness of the results. First, as problems in the coronary artery could reversely affect social networks, we considered only long-lasting social networks and re-examined the associations between CACS and the deficiency in social network betweenness in model As and Bs. Based on the information about how many years the participants had known their social network members, we eliminated recently-formed social networks and re-calculated network size and betweenness using only long-lasting network members based on two different thresholds (≥ 5 years or ≥ 10 years), and tested if the associations of network betweenness were sustained. By removing those young networks, we aimed to rule out the associations due to the network changes caused by the present health condition from our prediction. Second, for a more accurate assessment of causal effects, we adopted the coarsened exact matching (CEM) method in Model Cs16). Unlike other matching methods based on propensity scores, CEM matches observations with those with “exactly” the same values of covariates, and performs regression analyses using a subsample of matched observations where the treated and untreated groups are weighted to have the same sample size. Since it is hard to find observations with exactly the same covariates in a given sample, CEM “coarsens” covariates to a small number of categories before matching. Under the assumption that this set of variables determine the present social networks, we can consider the associations between CACS and networks from CEM as causal. As it was hard to retain enough sample size for statistical inference when treating with multivalued treatment, we did not test a CEM model with three dummy variables for network betweenness. In this analysis, continuous variables were coarsened into three groups, and categorical variables were adopted as original categories. As covariates for matching, we examined those that had significant bivariate relationships with network betweenness (age, diabetes, depression, SBP, LDL-cholesterol, glucose, eGFR, education, income, working, and marriage). When doing regression analyses after finding a subsample of matched observations, we used the same set of covariates as other multiple logistic regression analyses except that the categorical variables that were not coarsened during matching were excluded. Third, we restricted our sample to those with social network size > 1 and performed the same logistic regression analyses in Model Ds. Since social network betweenness can arise from at least two social network members, some sociologists emphasized a qualitative difference between those who have so small networks (≤ 1) to cultivate network betweenness and the others with big networks17). By restricting our sample to those with social network size > 1, we could focus on the disadvantage of deficiency in network betweenness among participants whose networks were big enough to have network betweenness. The analyses were performed by using STATA 14 (StataCorp LP, College Station, TX, USA).
Results
Table 1 shows the clinical characteristics of participants according to CACS. Participants who were included in a higher CACS group were more likely to be older, male, currently smoking, having diabetes, a sedentary lifestyle, ESRD or a history of receiving kidney transplantation, higher SBP, lower DBP, and higher level of fasting plasma glucose. These participants had lower serum cholesterol, possibly because more statin users were included in the higher CACS group. Concerning socio-economic status, participants with higher CACS were less educated, not married, and living with fewer household members; however, household income and working status were significantly different across CACS categories with no consistent patterns. Concerning social network characteristics, participants with higher CACS had significantly smaller (p < 0.001) OF (p < 0.001) and NC (p < 0.001) networks.
Table 1. Characteristics of participants by coronary artery calcium score (n = 1384).
| Variable | Category | Coronary calcium score (AU) |
||||
|---|---|---|---|---|---|---|
| 0 (n = 545) | 1–100 (n = 364) | 101–400 (n = 266) | > 400 (n = 209) | P | ||
| Age, year | 54.9 ± 412.0 | 61.1 ± 10 | 63.9 ± 10.2 | 63.3 ± 10.6 | < 0.001 | |
| Sex, n (%) | Male | 259 (48%) | 212 (58%) | 144 (54%) | 145 (69%) | < 0.001 |
| Female | 286 (52%) | 152 (42%) | 122 (46%) | 64 (31%) | ||
| Current smoker, n (%) | 213 (39%) | 172 (47%) | 130 (49%) | 119 (57%) | < 0.001 | |
| Hypertension, n (%) | 456 (84%) | 307 (84%) | 229 (86%) | 184 (88%) | 0.451 | |
| Diabetes, n (%) | 153 (28%) | 150 (41%) | 139 (52%) | 119 (57%) | < 0.001 | |
| End-stage renal disease, n (%) | 84 (15%) | 47 (13%) | 34 (13%) | 58 (28%) | < 0.001 | |
| Kidney transplantation, n (%) | 36 (7%) | 19 (5%) | 19 (7%) | 30 (14%) | 0.001 | |
| Exercise, MET minute/week | 1928.6 ± 2493.9 | 2224.2 ± 3211.8 | 1887.0 ± 2747.6 | 1535.5 ± 2155.1 | 0.032 | |
| Depression, n (%) | 34 (6%) | 27 (7%) | 24 (9%) | 24 (11%) | 0.096 | |
| Statin use, n (%) | 235 (43%) | 188 (52%) | 154 (58%) | 119 (57%) | < 0.001 | |
| Body mass index, kg/m2 | 25.0 ± 3.8 | 25.5 ± 3.6 | 25.3 ± 3.4 | 24.8 ± 3.9 | 0.079 | |
| Systolic blood pressure, mmHg | 123.7 ± 14.8 | 129.1 ± 16.4 | 130.7 ± 18.1 | 132.2 ± 21.8 | < 0.001 | |
| Diastolic blood pressure, mmHg | 76.8 ± 10.3 | 77.2 ± 10.4 | 74.3 ± 9.5 | 73.9 ± 10.1 | < 0.001 | |
| Total cholesterol, mg/dL | 179.7 ± 35.3 | 172.9 ± 35.7 | 166.5 ± 35.9 | 162.7 ± 34.5 | < 0.001 | |
| HDL-cholesterol, mg/dL | 50.9 ± 13.2 | 48.0 ± 12.5 | 48.5 ± 22 | 45.6 ± 11.9 | < 0.001 | |
| LDL-cholesterol, mg/dL | 101.0 ± 30.5 | 95.1 ± 28.8 | 90.1 ± 27.6 | 86.6 ± 27.9 | < 0.001 | |
| Triglyceride, mg/dL | 133.7 ± 71.5 | 140.8 ± 76.9 | 144.7 ± 104.7 | 142.3 ± 83.5 | 0.251 | |
| Fasting glucose, mg/dL | 107.2 ± 28.5 | 112.6 ± 29.6 | 116.5 ± 31 | 120.7 ± 41.4 | < 0.001 | |
| Estimated GFR, ml/min/1.73 m2 | 68.4 ± 36.1 | 66.2 ± 33.6 | 64.2 ± 30.9 | 53.0 ± 32.5 | < 0.001 | |
| Education, n (%) | ≤Middle school | 132 (24%) | 111 (30%) | 94 (35%) | 71 (34%) | |
| High school | 192 (35%) | 110 (30%) | 82 (31%) | 71 (34%) | 0.013 | |
| ≥College | 221 (41%) | 143 (39%) | 90 (34%) | 67 (32%) | ||
| Household income, n (%) | < US$3000 | 64 (12%) | 50 (14%) | 52 (20%) | 37 (18%) | |
| US$3001–6000 | 140 (26%) | 75 (21%) | 66 (25%) | 39 (19%) | 0.013 | |
| ≥US$6000 | 122 (22%) | 94 (26%) | 46 (17%) | 40 (19%) | ||
| DK or refusal | 219 (40%) | 145 (40%) | 102 (38%) | 93 (44%) | ||
| Current worker, n (%) | 298 (55%) | 180 (49%) | 104 (39%) | 93 (44%) | < 0.001 | |
| Married, n (%) | 432 (79%) | 304 (84%) | 220 (83%) | 155 (74%) | 0.034 | |
| Number of household members | 1.3 ± 1.3 | 1.2 ± 1.2 | 1.0 ± 1.2 | 1.0 ± 1.2 | < 0.001 | |
| Network size | 2.2 ± 1.4 | 2.0 ± 1.4 | 1.9 ± 1.4 | 1.7 ± 1.3 | < 0.001 | |
| Only-family networks, n (%) | 283 (52%) | 214 (59%) | 180 (68%) | 154 (74%) | < 0.001 | |
| No-cutpoint networks, n (%) | 332 (61%) | 242 (66%) | 198 (74%) | 173 (83%) | < 0.001 | |
Data are presented as mean (SD) for continuous variables or n (%) for categorical variables. The p-values are from ANOVA tests for continuous variables or chi-square tests for categorical variables.
AU, Agatston unit; MET, metabolic equivalent of task; DK, do not know.
Table 2 shows the association between deficiency of social network betweenness and other covariates. Participants with OF or NC networks were more likely to be older and have diabetes, depression, higher SBP, higher total cholesterol, lower HDL-cholesterol, lower LDL-cholesterol, and higher fasting plasma glucose levels. eGFR was positively associated with OF networks, whereas current smokers were more likely to have NC networks. Concerning socio-economic status, deficiency in both types of social network betweenness was related to a lower level of education, lower household income, and not working status. Married participants were more likely to have OF networks but less likely to have NC networks. Those who had smaller networks were more likely to have both OF and NC networks.
Table 2. Characteristics of participants by social network betweenness (n = 1384).
| Variable | Category | Only-family networks |
No-cutpoint networks |
||||
|---|---|---|---|---|---|---|---|
| No (n = 553) | Yes (n = 831) | P | No (n = 439) | Yes (n = 945) | P | ||
| Coronary calcium score (AU) | 176.3 ± 527.0 | 270.6 ± 565.0 | 0.002 | 146.3 ± 485.7 | 273.2 ± 575.9 | < 0.001 | |
| Age, year | 55.5 ± 11.8 | 62.2 ± 10.7 | < 0.001 | 55.1 ± 11.4 | 61.6 ± 11.1 | < 0.001 | |
| Sex, n (%) | Male | 299 (54%) | 461 (55%) | 0.606 | 231 (53%) | 529 (56%) | 0.242 |
| Female | 254 (46%) | 370 (45%) | 208 (47%) | 416 (44%) | |||
| Current smoker, n (%) | 254 (46%) | 380 (46%) | 0.941 | 190 (43%) | 444 (47%) | 0.198 | |
| Hypertension, n (%) | 459 (83%) | 717 (86%) | 0.094 | 368 (84%) | 808 (86%) | 0.417 | |
| Diabetes, n (%) | 166 (30%) | 395 (48%) | < 0.001 | 139 (32%) | 422 (45%) | < 0.001 | |
| End-stage renal disease, n (%) | 89 (16%) | 134 (16%) | 0.988 | 69 (16%) | 154 (16%) | 0.785 | |
| Kidney transplantation, n (%) | 43 (8%) | 61 (7%) | 0.764 | 34 (8%) | 70 (7%) | 0.825 | |
| Exercise, MET minute/week | 2067.7 ± 2620.11853.3 ± 2766.9 | 0.150 | 1887.3 ± 2451.71963.0 ± 2823.3 | 0.629 | |||
| Depression, n (%) | 32 (6%) | 77 (9%) | 0.019 | 24 (5%) | 85 (9%) | 0.023 | |
| Statin use, n (%) | 285 (52%) | 411 (49%) | 0.449 | 220 (50%) | 476 (50%) | 0.929 | |
| Body mass index, kg/m2 | 25.2 ± 3.7 | 25.1 ± 3.7 | 0.498 | 25.1 ± 3.7 | 25.2 ± 3.7 | 0.869 | |
| Systolic blood pressure, mmHg | 125.5 ± 15.6 | 129.2 ± 18.4 | < 0.001 | 125.0 ± 15.3 | 129.0 ± 18.2 | < 0.001 | |
| Diastolic blood pressure, mmHg | 77.1 ± 10.3 | 75.2 ± 10.1 | 0.001 | 76.7 ± 10.4 | 75.6 ± 10.2 | 0.059 | |
| Total cholesterol, mg/dL | 177.9 ± 35.9 | 169.4 ± 35.6 | < 0.001 | 179.6 ± 36.9 | 169.7 ± 35.1 | < 0.001 | |
| HDL-cholesterol, mg/dL | 50.7 ± 17.7 | 47.7 ± 12.9 | < 0.001 | 51.0 ± 18.6 | 47.9 ± 12.9 | < 0.001 | |
| LDL-cholesterol, mg/dL | 98.1 ± 29.6 | 93.2 ± 29.5 | 0.003 | 99.1 ± 29.9 | 93.3 ± 29.3 | 0.001 | |
| Triglyceride, mg/dL | 140.6 ± 88 | 137.9 ± 77.9 | 0.549 | 140.3 ± 86.6 | 138.4 ± 79.9 | 0.693 | |
| Fasting glucose, mg/dL | 107.5 ± 24.7 | 115.7 ± 35.5 | < 0.001 | 106.7 ± 23 | 115.1 ± 34.9 | < 0.001 | |
| Estimated GFR, ml/min/1.73 m2 | 68.0 ± 34.9 | 62.5 ± 33.8 | 0.003 | 67.1 ± 34.4 | 63.5 ± 34.3 | 0.069 | |
| Education, n (%) | ≤ Middle school | 107 (19%) | 301 (36%) | 85 (19%) | 323 (34%) | ||
| High school | 174 (31%) | 281 (34%) | < 0.001 | 128 (29%) | 327 (35%) | < 0.001 | |
| ≥College | 272 (49%) | 249 (30%) | 226 (51%) | 295 (31%) | |||
| Household income, n (%) | < US$3000 | 62 (11%) | 141 (17%) | 50 (11%) | 153 (16%) | ||
| US$3001–6000 | 148 (27%) | 172 (21%) | < 0.001 | 125 (28%) | 195 (21%) | < 0.001 | |
| ≥US$6000 | 165 (30%) | 137 (16%) | 142 (32%) | 160 (17%) | |||
| DK or refusal | 178 (32%) | 381 (46%) | 122 (28%) | 437 (46%) | |||
| Current worker, n (%) | 311 (56%) | 364 (44%) | < 0.001 | 246 (56%) | 429 (45%) | < 0.001 | |
| Married, n (%) | 427 (77%) | 684 (82%) | 0.020 | 369 (84%) | 742 (79%) | 0.016 | |
| Number of household members | 1.2 ± 1.1 | 1.2 ± 1.3 | 0.569 | 1.3 ± 1.1 | 1.1 ± 1.3 | 0.054 | |
| Network size | 3.0 ± 1.2 | 1.3 ± 1.1 | < 0.001 | 3.2 ± 1.1 | 1.5 ± 1.2 | < 0.001 | |
Data are presented as mean ± SD for continuous variables or n (%) for categorical variables. The p-values are from ANOVA tests for continuous variables or chi-square tests for categorical variables.
AU, Agatston unit; MET, metabolic equivalent of task; DK, do not know.
Table 3 shows the results of multiple logistic regression analyses for identifying whether each social network component was a determinant for CACS > 400. The association between CACS and network size (odds ratio [OR], 0.95; 95% confidence interval [CI], 0.83–1.08; p = 0.412) or OF networks (OR, 1.50; 95% CI, 0.95–2.35; p = 0.080) was not statistically significant at the 0.05 level; however, NC networks had significant association with CACS > 400 when separately considered in model 3 (OR, 1.72; 95% CI, 1.07–2.77; p = 0.026). When including two types of deficiency in network betweenness together in model 4, both had p-values > 0.05. When examining three dummy variables (OF networks alone, NC networks alone, and both OF and NC networks) in model 5, participants who had both OF and NC networks had significantly greater odds of CACS > 400 than those with no deficiency in network betweenness (OR, 1.88; 95% CI, 1.10–3.23; p = 0.022). Even though we did not find any evidence for the multiplicative association between OF and NC networks from the Wald test (χ2 = 0.00, p = 0.98), we could observe that the ORs for those with both OF and NC networks was the largest among three types of deficiency in network betweenness.
Table 3. Multiple logistic regression analyses of coronary artery calcium score > 400 (N = 1384).
| Variable | Model 1 |
Model 2 |
Model 3 |
Model 4 |
Model 5 |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | P | OR | P | OR | P | OR | P | OR | P | |
| (95% CI) | (95% CI) | (95% CI) | (95% CI) | (95% CI) | ||||||
| Network size | 0.95 | 0.412 | 1.03 | 0.730 | 1.03 | 0.690 | 1.05 | 0.510 | 1.06 | 0.509 |
| (0.83–1.08) | (0.88–1.20) | (0.89–1.19) | (0.90–1.24) | (0.90–1.24) | ||||||
| No deficiency+ | 1.00 | – | 1.00 | – | ||||||
| NC alone (n = 553) | (reference) | (reference) | ||||||||
| OF (n = 831) | 1.50 | 0.080 | 1.21 | 0.467 | ||||||
| (0.95–2.35) | (0.72–2.03) | |||||||||
| No deficiency+ | 1.00 | – | 1.00 | – | ||||||
| OF alone (n = 439) | (reference) | (reference) | ||||||||
| NC (n = 945) | 1.72 | 0.026 | 1.56 | 0.114 | ||||||
| (1.07–2.77) | (0.90–2.69) | |||||||||
| No deficiency | 1.00 | – | ||||||||
| (n = 383) | (reference) | |||||||||
| OF alone (n = 56) | 1.19 | 0.755 | ||||||||
| (0.39–3.68) | ||||||||||
| NC alone (n = 170) | 1.55 | 0.166 | ||||||||
| (0.83–2.88) | ||||||||||
| OF + NC (n = 775) | 1.88 | 0.022 | ||||||||
| (1.10–3.23) | ||||||||||
All models were controlled for age, sex, smoking, hypertension, diabetes, ESRD, exercise, depression, statin use, BMI, SBP, LDL-cholesterol, glucose, eGFR, education, income, working, marriage, and number of co-habitants.
Model 1 evaluated the association of network size. Model 2 included network size and OF. No deficiency + NC alone was reference of OF. Model 3 included network size and NC. No deficiency + OF alone was a reference to NC. Model 4 included network size, OF, and NC. No deficiency + NC alone was a reference to OF. No deficiency+OF alone was a reference to NC. Model 5 used three dummy variables for social network betweenness (OF alone, NC alone, and OF + NC) comparing with “no deficiency” as reference.
OF, only-family networks; NC, no-cutpoint networks
The results of robustness checks are shown in Table 4. First, when considering social networks known for ≥ 5 years in model A-1 to A-3, OF networks (OR, 1.65; 95% CI, 1.05–2.60; p = 0.030), NC networks (OR, 1.98; 95% CI, 1.22–3.24; p = 0.006), and both OF and NC networks (OR, 2.24; 95% CI, 1.28–3.90; p = 0.004) showed significant associations with CACS > 400. When adopting the threshold of ≥ 10 years in model B-1 to B-3, we also observed significant associations of OF networks (OR, 1.67; 95% CI, 1.06–2.64; p = 0.028), NC networks (OR, 1.98; 95% CI, 1.20–3.26; p = 0.007), and both OF and NC networks (OR, 2.26; 95% CI, 1.28–3.98; p = 0.005). Second, according to the CEM analyses in model C-1 to C-2, the p-value for OF networks reached > 0.05 (OR, 1.60; 95% CI, 0.96–2.66; p = 0.070), whereas NC networks (OR, 2.78; 95% CI, 1.53–5.05; p = 0.001) were significantly associated with CACS > 400. Lastly, in model D-1 to D-3 in which those with no or only one network member were excluded, OF networks (OR, 1.41; 95% CI, 0.80–2.48; p = 0.239) and both OF and NC networks (OR, 1.77; 95% CI, 0.92–3.38; p = 0.086) did not show significant associations with CACS > 400, whereas NC networks (OR, 1.74; 95% CI, 1.02–2.99; p = 0.044) were significantly associated with CACS > 400 in model D-2.
Table 4. Robustness checks for the multiple logistic regression analyses of coronary artery calcium score > 400.
| Networks known for ≥ 5 years |
Networks known for ≥ 10 years |
Coarsened-exact-matching analysis |
Network size > 1 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | OR | P | n | OR | P | n | OR | P | n | OR | P | |
| (95% CI) | (95% CI) | (95% CI) | (95% CI) | |||||||||
| Model A-1 (n = 1,384) | Model B-1 (n = 1,384) | Model C-1 (n = 933) | Model D-1 (n = 694) | |||||||||
| No deficiency+ NC alone | 553 | 1.00 | – | 553 | 1.00 | – | 393 | 1.00 | – | 553 | 1.00 | – |
| (reference) | (reference) | (reference) | (reference) | |||||||||
| OF | 831 | 1.65 | 0.030 | 831 | 1.67 | 0.028 | 540 | 1.60 | 0.070 | 831 | 1.41 | 0.239 |
| (1.05–2.60) | (1.06–2.64) | (0.96–2.66) | (0.80–2.48) | |||||||||
| Model A-2 (n = 1,384) | Model B-2 (n = 1,384) | Model C-2 (n = 920) | Model D-2 (n = 694) | |||||||||
| No deficiency+ OF alone | 439 | 1.00 | – | 439 | 1.00 | – | 332 | 1.00 | – | 439 | 1.00 | – |
| (reference) | (reference) | (reference) | (reference) | |||||||||
| NC | 945 | 1.98 | 0.006 | 945 | 1.98 | 0.007 | 588 | 2.78 | 0.001 | 945 | 1.74 | 0.044 |
| (1.22–3.24) | (1.20–3.26) | (1.53–5.05) | (1.02–2.99) | |||||||||
| Model A-3 (n = 1,384) | Model B-3 (n = 1,384) | Model D-3 (n = 694) | ||||||||||
| No deficiency | 383 | 1.00 | – | 383 | 1.00 | – | 383 | 1.00 | – | |||
| (reference) | (reference) | (reference) | ||||||||||
| OF alone | 56 | 1.22 | 0.728 | 56 | 1.23 | 0.724 | 56 | 1.64 | 0.427 | |||
| (0.39–3.80) | (0.39–3.85) | (0.49–5.50) | ||||||||||
| NC alone | 170 | 1.73 | 0.090 | 170 | 1.69 | 0.110 | 170 | 1.93 | 0.062 | |||
| (0.92–3.25) | (0.89–3.22) | (0.97–3.83) | ||||||||||
| OF+NC | 775 | 2.24 | 0.004 | 775 | 2.26 | 0.005 | 775 | 1.77 | 0.086 | |||
| (1.28–3.90) | (1.28–3.98) | (0.92–3.38) | ||||||||||
All models were controlled for age, sex, smoking, hypertension, diabetes, ESRD, exercise, depression, statin use, BMI, SBP, LDL-cholesterol, glucose, eGFR, education, income, working, marriage, and number of co-habitants.
Model As used 5 years and model Bs used 10 years as thresholds of network duration, respectively. In Model Cs using the coarsened-exact-matching method, observations were matched based on age, diabetes, depression, SBP, LDL-cholesterol, glucose, eGFR, education, income, working, and marriage. Continuous variables were coarsened into three groups, and categorical variables were adopted as original categories. Model Ds were logistic regressions which used subsamples with social network size > 1.
OF, only-family networks; NC, no-cutpoint networks
To examine the difference by age and sex, we reassessed models 2 and 3 in Table 3 by using subsamples of age ≤ 60 years, age > 60 years, male, or female. As seen in Fig. 2, there was no difference in the associations of OF networks by age and sex. However, NC networks were more disadvantageous for older (OR, 2.64; 95% CI, 1.27–5.51; p = 0.009) and female (OR, 6.34; 95% CI, 2.02–19.96; p = 0.002) participants.
Fig. 2.
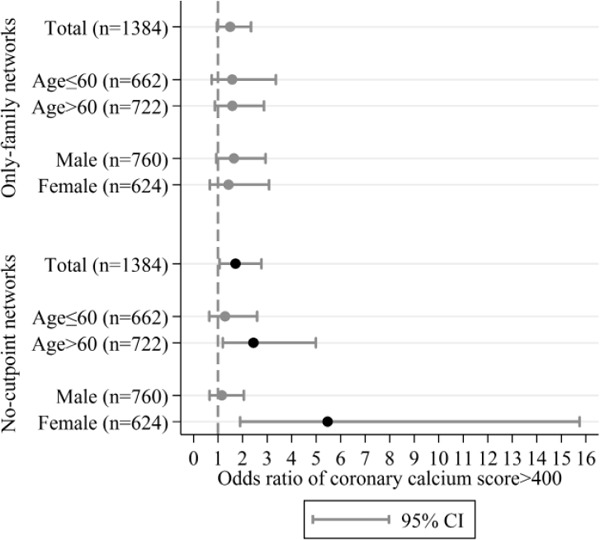
ORs and 95% CIs for only-family networks and nocutpoint network from multiple logistic regression analyses of coronary calcium score > 400 in total participants and subgroups. We predicted ORs for only-family networks or no-cutpoint networks after controlling for age, sex, smoking, hypertension, diabetes, ESRD, exercise, depression, statin use, BMI, SBP, LDL-cholesterol, glucose, eGFR, education, income, working, marriage, number of co-habitants, and network size.
Discussion
The key findings from this study were as follows: (i) social network betweenness was closely related with health and socio-economic status; (ii) no-cutpoint networks, in which network members form a connected group even when excluding a respondent, were significantly associated with a higher risk of CACS > 400; and (iii) the disadvantage of no-cutpoint networks was larger for older and female participants. While previous studies have investigated whether biomarkers such as pulse wave velocity or inflammatory markers were associated with the presence of subclinical atherosclerosis18, 19), the novelty of this study is that sociological factors may be closely related with subclinical atherosclerosis, characterized by coronary artery calcification.
In previous studies, the disadvantage of poor social networks was considered to parallel the deficiency in social support, which could directly cause the onset and progression of CVD20), or have indirect effects through buffering the negative influence of acute stress21) and depressive symptoms22). In this study, more detailed properties of social networks were investigated by adopting the network structure of betweenness. First, network betweenness captures the accessibility to diverse origins of social resources, which is a different aspect from the content or size of networks. For example, diverse networks more effectively provide medical information and first-hand experience about certain diseases, and are known to have special importance for those with health problems23). Considering that the sample of this study was at a high risk of CVD, the strong disadvantage for those without network betweenness is not surprising. Second, various sources represent the diversity in the activities they perform with their network members. Network betweenness allows the potential to enjoy at least two different activities and thoughts, which affords a stronger sense of freedom and accomplishment than being confined to a narrow social space. Those benefits are reported to have more importance for the subjective well-being of the older population5), as retirement status and little participation in organizational activities make them more dependent on selective interpersonal relationships24). The strong correlation between network betweenness and depression, and the stronger associations of betweenness with the CACS older adults observed in this study are consistent with previous findings.
Among the two types of deficiency in social network, between and no-cutpoint networks had stronger and more robust associations with CACS than only-family networks. Even though these two had no significant associations with CACS at a level of 0.05 when included together in the same model due to a strong correlation between themselves (χ2 = 599.24, p < 0.001), no-cutpoint networks were significantly associated with CACS in all models for robustness checks, whereas only-family networks showed little evidence of associations in the models using the CEM method and the subsample with two or more social networks. Considering that family members are the first sources of immediate support for people with health problems25), the associations of only-family networks could largely originate from the previous health status, which was partly proved in the results from the matching analyses. Furthermore, the results from the subsample with network size > 1 implicate that the disadvantage of only-family networks is not critical among those who have big networks, but mixed with the fundamental restriction of small network size. The robust results from the analyses of no-cutpoint networks, on the other hand, show that they could be more strong indicators for CACS than only-family networks. Additionally, no-cutpoint networks were more accurate in detecting the bridging potential of participants, as these are based on direct information about the social network structure. Despite its importance, there are few studies on the relationship between network betweenness and CVD because of the shortage of data about the details of network structure3). While a recent study showed that older women are more likely to establish their social autonomy via social network betweenness26), we observed a similar pattern that no-cutpoint networks were more unfavorable for the CACS of older and female participants. Cumulative findings from future studies on network structure and CVD may provide a clearer explanation about the sex difference in the associations of network betweenness.
This study has several limitations. First, owing to the cross-sectional design, we do not know the causality of social network betweenness with the progression of coronary artery calcium and/or the development of cardiovascular disease. For addressing this issue, we recalculated network indices using only long-lasting social networks and observed robust associations between CACS and both types of deficiency in social network betweenness. If we assume that the formation of longlasting social networks precedes the progression of coronary artery calcification, the results possibly implicate the causal effects of network betweenness. In addition, we also found the significant associations of no-cutpoint networks from the CEM analyses. However, these results cannot fully support our causal inference since we do not have the accurate information about the temporal order among variables, and examined the outcome and covariates at the same time point. As CMERC-HI is a prospective cohort study, the prognostic implications of social network betweenness in this cohort can be clarified in the future. Second, as the study population comprised subjects with a relatively high risk of developing CVD, the results of this study are vulnerable to generalizability. Third, the results showed that age and socio-economic status were different according to CACS. Considering that age and income had strong associations with both social network betweenness and cardiovascular outcome, we could expect that our estimates could be biased from residual confounding. Even though we controlled for age and income in all multiple regression models, 1) there could be some omitted information such as medical access which might be limited to those with younger age and higher income, and 2) our indicators for income could be crude to sufficiently capture variations in economic status. Future studies are required to collect more thorough data of economic and medical backgrounds for unbiased estimates of network effects on CVD. Fourth, this study assumed that CACS > 400 is a surrogate marker of CVD. Although higher CACS is closely correlated with having more other cardiovascular risk factors and CACS > 400 is known as a good predictor of future CVD in the western population, clinical implication of CACS > 400 needs to be further validated in the Asian population27).
Conclusion
Participants who had higher coronary artery calcium score were likely to have a smaller network size and deficiencies in social network betweenness (only-family network, and no-cutpoint network). Especially, no-cutpoint networks had a significant and robust relationship with CACS > 400, a powerful surrogate marker of future CVD.
Funding
This research was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute funded by the Ministry of Health and Welfare, Republic of Korea (grant no. HI13C0715), and the National Research Foundation of Korea Grant funded by the Korean Government (NRF-2014S1A3A2044496).
Conflict of Interest
The authors have no conflict of interest to disclose.
References
- 1). Valtorta NK, Kanaan M, Gilbody S, Ronzi S, Hanratty B: Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart, 2016; 102: 1009-1016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2). Barth J, Schneider S, von Känel R: Lack of social support in the etiology and the prognosis of coronary heart disease: a systematic review and meta-analysis. Psychosomatic medicine, 2010; 72: 229-238 [DOI] [PubMed] [Google Scholar]
- 3). Berkman LF, Glass T, Brissette I, Seeman TE: From social integration to health: Durkheim in the new millennium. Social Science & Medicine, 2000; 51: 843-857 [DOI] [PubMed] [Google Scholar]
- 4). Burt RS: Structural holes: the social structure of competition, Harvard University Press, Cambridge, MA, 1992 [Google Scholar]
- 5). Cornwell B: Good health and the bridging of structural holes. Social Networks, 2009; 31: 92-103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6). Janssen I, Powell LH, Jasielec MS, Matthews KA, Hollenberg SM, Sutton-Tyrrell K, Everson-Rose SA: Progression of coronary artery calcification in black and white women: do the stresses and rewards of multiple roles matter? Annals of Behavioral Medicine, 2012; 43: 39-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7). Smith TW, Uchino BN, Florsheim P, Berg CA, Butner J, Hawkins M, Henry NJ, Beveridge RM, Pearce G, Hopkins PN: Affiliation and control during marital disagreement, history of divorce, and asymptomatic coronary artery calcification in older couples. Psychosomatic Medicine, 2011; 73:350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8). Burt RS: Network items and the general social survey. Social Networks, 1984; 6: 293-339 [Google Scholar]
- 9). Kim J, Kim S, Kim H: Korean General Social Survey 2003–2014, Sungkyunkwan University Press, Seoul, 2016 [Google Scholar]
- 10). Youm Y, Laumann EO, Ferraro KF, Waite LJ, Kim HC, Park Y-r, Chu SH, Joo W-t, Lee JA: Social network properties and self-rated health in later life: comparisons from the Korean social life, health, and aging project and the national social life, health and aging project. BMC geriatrics, 2014; 14: 102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11). Wasserman S: Social network analysis: Methods and applications, Cambridge university press, 1994 [Google Scholar]
- 12). Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Detrano R: Quantification of coronary artery calcium using ultrafast computed tomography. Journal of the American College of Cardiology, 1990; 15: 827-832 [DOI] [PubMed] [Google Scholar]
- 13). Nakazato R, Dey D, Gutstein A, Le Meunier L, Cheng VY, Pimentel R, Paz W, Hayes SW, Thomson LE, Friedman JD: Coronary artery calcium scoring using a reduced tube voltage and radiation dose protocol with dual-source computed tomography. Journal of Cardiovascular Computed Tomography, 2009; 3: 394-400 [DOI] [PubMed] [Google Scholar]
- 14). Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF: International physical activity questionnaire: 12-country reliability and validity. Medicine & Science in Sports & Exercise, 2003; 35: 1381-1395 [DOI] [PubMed] [Google Scholar]
- 15). Jo SA, Park MH, Jo I, Ryu SH, Han C: Usefulness of Beck Depression Inventory (BDI) in the Korean elderly population. International Journal of Geriatric Psychiatry, 2007; 22: 218-223 [DOI] [PubMed] [Google Scholar]
- 16). Iacus SM, King G, Porro G: Causal inference without balance checking: Coarsened exact matching. Political Analysis, 2012: 1-24 [Google Scholar]
- 17). Cornwell B, Laumann EO: Network Position and Sexual Dysfunction: Implications of Partner Betweenness for Men. American journal of sociology, 2011; 117: 172-208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18). Nagasawa SY, Ohkubo T, Masaki K, Barinas-Mitchell E, Miura K, Seto T, El-Saed A, Kadowaki T, Willcox BJ, Edmundowicz D, Kadota A, Evans RW, Kadowaki S, Fujiyoshi A, Hisamatsu T, Bertolet MH, Okamura T, Nakamura Y, Kuller LH, Ueshima H, Sekikawa A: Associations between Inflammatory Markers and Subclinical Atherosclerosis in Middle-aged White, Japanese-American and Japanese Men: The ERA-JUMP Study. J Atheroscler Thromb, 2015; 22: 590-598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19). Torii S, Arima H, Ohkubo T, Fujiyoshi A, Kadota A, Takashima N, Kadowaki S, Hisamatsu T, Saito Y, Miyagawa N, Zaid M, Murakami Y, Abbott RD, Horie M, Miura K, Ueshima H: Association between Pulse Wave Velocity and Coronary Artery Calcification in Japanese men. J Atheroscler Thromb, 2015; 22: 1266-1277 [DOI] [PubMed] [Google Scholar]
- 20). Rosengren A, Wilhelmsen L, Orth-Gomér K: Coronary disease in relation to social support and social class in Swedish men. European Heart Journal, 2004; 25: 56-63 [DOI] [PubMed] [Google Scholar]
- 21). Uchino BN, Garvey TS: The availability of social support reduces cardiovascular reactivity to acute psychological stress. Journal of Behavioral Medicine, 1997; 20: 15-27 [DOI] [PubMed] [Google Scholar]
- 22). Frasure-Smith N, Lespérance F, Gravel G, Masson A, Juneau M, Talajic M, Bourassa MG: Social support, depression, and mortality during the first year after myocardial infarction. Circulation, 2000; 101: 1919-1924 [DOI] [PubMed] [Google Scholar]
- 23). Thoits PA: Mechanisms linking social ties and support to physical and mental health. Journal of Health and Social Behavior, 2011; 52: 145-161 [DOI] [PubMed] [Google Scholar]
- 24). Fredrickson BL, Carstensen LL: Choosing social partners: how old age and anticipated endings make people more selective. Psychology and Aging, 1990; 5: 335-347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25). Schulz R, Quittner AL: Caregiving for children and adults with chronic conditions: introduction to the special issue. Health Psychology, 1998; 17: 107. [PubMed] [Google Scholar]
- 26). Cornwell B: Independence through social networks: Bridging potential among older women and men. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 2011; 66: 782-794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27). Zaid M, Fujiyoshi A, Kadota A, Abbott RD, Miura K: Coronary Artery Calcium and Carotid Artery Intima Media Thickness and Plaque: Clinical Use in Need of Clarification. J Atheroscler Thromb, 2017; 24: 227-239 [DOI] [PMC free article] [PubMed] [Google Scholar]


