Mucosa-associated lymphoid tissue lymphoma translocation protein 1 (MALT1), also known as paracaspase 1, is a ubiquitous protease with homology to caspases.1 The function of MALT1 is best understood in immune cells, in particular lymphocytes, in which MALT1 controls signaling downstream of antigen receptors, for example, nuclear-factor-kappa-B (NF-κB) and mitogen-activated protein kinase pathways. Activation of MALT1 paracaspase activity has been shown to require the assembly of a tripartite signaling complex termed CBM (CARD11/BCL10/MALT1), which is formed following the phosphorylation and conformational change of caspase recruitment domain 11 (CARD11) that is induced by antigen-receptor stimulation. This complex then recruits the E3 ligase tumor necrosis factor receptor-associated factor 6 (TRAF6), which leads to the activation of the inhibitor-of-kappa-B kinase (IκK) complex, an essential step in the release of transcriptionally active NF-κB. Now, according to recent studies, there might be alternative mechanisms for MALT1 activation that do not rely on the recruitment into CBM complexes. In the first study, Li and colleagues show that the OX40 signaling pathway in invariant natural killer T (iNKT) cells activates caspase-1 by recruiting MALT1 in a TRAF6-dependent manner that might bypass CBM formation.2 In the second study, Thome and colleagues show that two Kaposi’s sarcoma-associated herpes virus (KSHV) proteins promote NF-κB activation via binding to MALT1 and activating its paracaspase activity, likely in a CBM-independent manner.3 These findings are highlighted below and show how emerging concepts continue to push the current boundaries of our understanding of the function of MALT1.
MALT1 was discovered some 20 years ago as a proto-oncogenic translocation product that accounted for antibiotic resistance in MALT lymphoma patients.4 Subsequently, the CARMA protein family was identified, and MALT1 was shown to be an essential component of so-called CBM complexes composed of CARMA1, also known as CARD11, B-cell lymphoma 10 (BCL10) and MALT1, which assemble upon antigen-receptor-driven stimulation in lymphocytes.5 In addition to CARMA1, other CARD containing proteins, for example, CARD9, CARMA2 (CARD14) and CARMA3 (CARD10), have been shown to build similar CBM complexes in response to various ligands in several cell types. They are involved, either downstream of receptors/co-receptors displaying immune-receptor tyrosine-based activation motifs in their cytoplasmic domain, through a cascade of phosphorylation-induced recruitment of signaling molecules, or downstream of G-protein-coupled receptors by unknown mechanisms. In 2008, the long elusive catalytic function of MALT1 was finally elucidated.6 MALT1 was identified as a Cys-dependent, Arg-specific protease, leading to the discovery of several MALT1 proteolytic substrates.5 Furthermore, constitutive MALT1 protease activity was discovered in diffuse large B-cell lymphomas (DLBCL) of the activated B-cell (ABC) subtype, which are characterized by chronic stimulation of the B-cell receptor pathway, as a result of somatic mutations in some of the signaling components. In particular, CARD11 gain-of-function mutations were characterized,7 which contributed to the establishment that CBM assembly is a keystone for MALT1 protease activation (Figure 1).
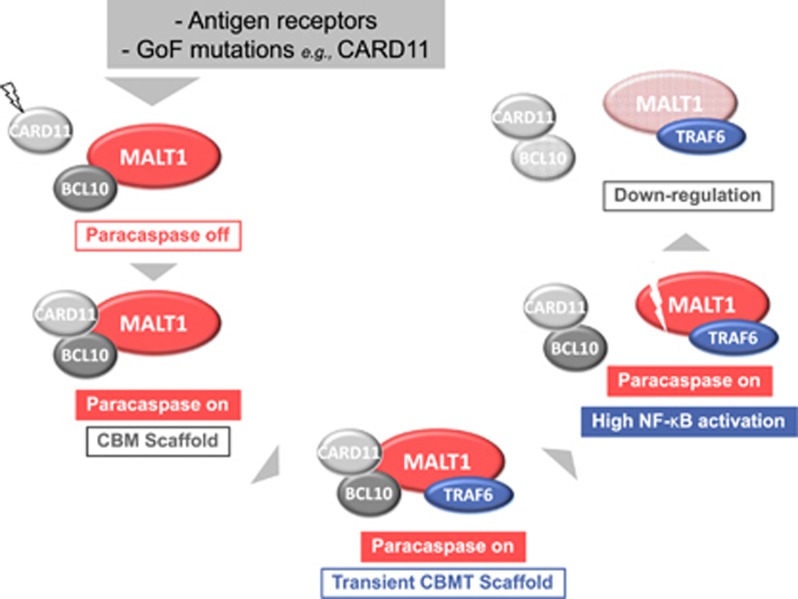
Figure 1.
The waves of MALT1 activation. MALT1 is recruited into CARD/BCL10/MALT1 (CBM) complexes after stimulation of antigen receptors or under chronic stimulatory conditions resulting from mutations in signaling components of the pathway, for example, gain-of-function (GoF) mutations in CARD11. CBM assembly triggers MALT1 paracaspase activity. MALT1 cleaves several substrates including BCL10. MALT1 can also auto-cleave, particularly at R149,8 which is promoted by TRAF6.9 This process represents a feed-forward mechanism that releases a highly functional MALT1 species. MALT1 auto proteolysis, and cleavage of BCL10 by MALT1 may contribute to downregulation of the pathway.9
The recent work by Li and colleagues, published in the June issue of The Journal of Clinical Investigation,2 showed that OX40, a TNF superfamily receptor (TNFRSF4), can activate the MALT1 protease in iNKT cells. Although normally associated with T-cell survival, effector differentiation and memory generation, this study uncovered that OX40 signaling in iNKT cells instead leads to caspase-1-dependent programmed cell death, also known as pyroptosis. Furthermore, in TRAF6-deficient iNKT cells, OX40 failed to induce caspase-1 activation, as shown by the absence of caspase-1 cleavage using immunoblotting and flow cytometry methods. Next, using an immunoprecipitation approach with FACS-sorted iNKT cells stimulated with OX40 ligand in vitro, the authors identified BCL10 and MALT1 as TRAF6 interactors. By overexpressing TRAF6, MALT1 and caspase-1 in 293T cells, they observed that TRAF6 fails to co-immunoprecipitate with caspase-1 in the absence of MALT1, suggesting that MALT1 is a critical component for TRAF6-mediated activation of caspase-1. Binding of BCL10 to MALT1 also appears to be key because deletion of the N-terminal region of MALT1—a region previously shown to contain key determinants of BCL10 binding—abrogated recruitment of caspase-1 into the MALT1-TRAF6 complex. Additionally, a MALT1 protease inhibitor could block the cleavage of caspase-1 in a concentration-dependent manner, thus suggesting the involvement of MALT1 paracaspase activity in caspase-1 activation. Collectively, these data suggested that in iNKT cells, activation of the OX40 pathway recruits MALT1-BCL10 through TRAF6, and MALT1 then activates caspase-1 to induce cellular pyroptosis. Whether cleavage of caspase-1 is directly performed by MALT1 or if there is an intermediate regulator, however, remains to be clarified.
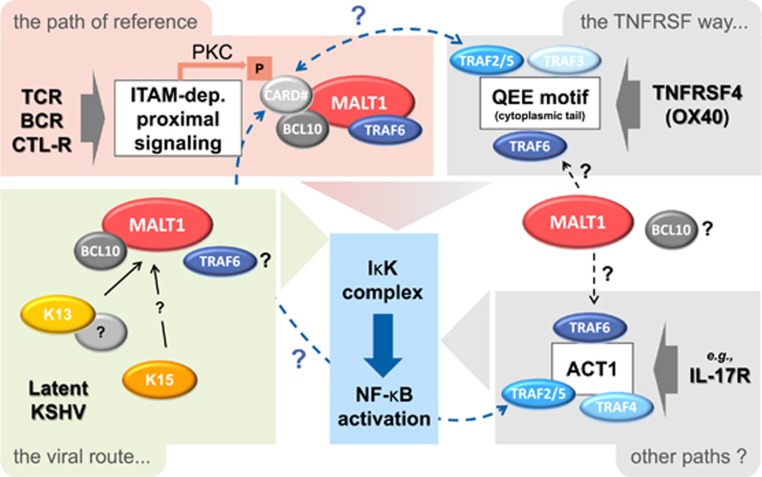
This study is the first report of a TNF superfamily receptor that can trigger MALT1 paracaspase activity. Notably, the cytoplasmic domain of OX40 bears TRAF2 recruitment motifs,10 and, therefore, classical CBM complex assembly appears unlikely. OX40-induced recruitment of protein kinase C together with CBM molecules into a TRAF2 complex was proposed previously;11 however, the mechanism has remained incompletely characterized. In the meantime, new insights have been obtained. First, shorter isoforms of CARD proteins were reported to be able to interact with TRAF2.12 Second, the E3 ligase activity of TRAF6 was shown to be activated downstream of OX40.10 Third, a recent report indicated that TRAF6 induces self-cleavage of MALT1, which has an impact on the activation cycle of MALT1 (Figure 1). That study also raised the possibility that TRAF6 might be able to activate the MALT1 protease directly, independently of CBM complex formation.9 Together, these recent insights suggest that MALT1, either directly or after release from assembly into a CBM complex, or even as part of a CBM complex—perhaps involving a short CARD isoform12 —might be able to reach signaling hubs coated with TRAF proteins, such as those downstream of TNF ligand family receptors, such as OX40.10 Expanding along these lines, other pathways might be able to recruit MALT1. For instance, the IL-17 receptor pathway represents an interesting case to investigate because it is known to recruit several TRAF isoforms via its scaffold protein, ACT1 (NF-κB-activating protein 1), including TRAF2 and TRAF6(ref. 13) (Figure 2).
Figure 2.
Toward novel ways of MALT1 activation?. ‘The path of reference’ represents the classical pathway of MALT1 activation as depicted in Figure 1. TCR, T-cell receptor; BCR, B-cell receptor; CTL-R, C-type lectin receptor. ‘The TNFRSF way…’ is based on an understanding of and questions about signaling and NF-κB activation in the context of the OX40 pathway. OX40 stimulation leads to the recruitment of TRAF proteins at the cytoplasmic tail of the receptor,10 which might enable recruitment of a CBM complex11 via binding of a CARD protein to TRAF2(ref. 12) or lead to recruitment of MALT1 by TRAF6, perhaps together with BCL10.2, 9 ‘Other paths?’ refers to pathways relying on signaling hubs able to recruit TRAF proteins, such as the IL-17R pathway via the protein, ACT1, which could potentially attract MALT1 in similar ways as proposed for the OX40 pathway. Finally, ‘the viral route’ summarizes the recent findings3 that two viral proteins, K13 and K15, from KSHV can activate MALT1 in a BCL10-dependent and likely CARD-independent manner—K13 binds to MALT1, possibly indirectly, whereas K15 does not—thus representing potential novel MALT1 activation pathways. CARD# represents CARD11 for antigen receptor (TCR/BCR) signaling; CARD9 for C-type-lectin (CTL)-receptor signaling and potentially stands for the four CARD/CARMA family proteins (CARD9, CARD10, CARD11, CARD14) or isoforms thereof, in case of the hypothesized signaling crosstalks depicted in the figure.
Another recent study by Thome and colleagues,3 published in the March issue of Leukemia, unveiled a key role for MALT1 in primary effusion lymphoma (PEL), which is a subtype of non-Hodgkin’s B-cell lymphoma caused by KSHV. Inhibiting the constitutive protease function of MALT1 in PEL induced a switch from the latent to the lytic stage of viral infection, leading to PEL cell death in vitro and to reduced tumor size in vivo using a xenograft model. Remarkably, PEL cell lines do not express Bruton tyrosine kinase (BTK) and, consistently, were not sensitive to the BTK inhibitor ibrutinib, in contrast to HBL-1 cells, which are an example of an ABC-DLBCL lymphoma cell line that responds to both BTK and MALT1 inhibition. Furthermore, these cell lines do not express detectable amounts of CARMA1, CARMA3 or CARD9. Together, this finding led the authors propose that MALT1 activation in PEL likely occurs independently of the BTK-CARMA axis. To identify mechanisms that activate MALT1 in latently infected PEL cells, they screened an expression library of 86 open reading frames (ORFs) encoded by the KSHV genome and found ORFs K13 and K15, which are two known NF-κB-inducing proteins expressed during viral latency, to be the most potent hits. Both K13 and K15 promoted MALT1 activation in a concentration-dependent manner and induced MALT1 mono-ubiquitination, which was previously shown to positively correlate with paracaspase activity.14 Using a pull-down approach, they provided evidence that the cytoplasmic K13 protein activates MALT1 and consequently NF-κB via binding to its protease domain, either directly or via an additional binding partner. The transmembrane K15 protein, which does not bind MALT1, most likely activates it via recruitment of additional signaling proteins through its cytoplasmic SH2-binding motif. How K13 and K15, respectively, activate MALT1 remains to be further studied; however, it is possible that these proteins are able, directly or indirectly, to induce a conformational change in the paracaspase domain of MALT1 that promotes activation. Both viral proteins are known to activate NF-κB via IκK components. Because MALT1 was proposed to physically recruit and activate the IκK complex, there is a possibility that signaling complexes recruited by K13/K15 might contain MALT1 and IκK components together. Additionally, given the key role of the TRAF6 E3 ligase to connect MALT1 and IκK, together with the reported importance of TRAF6 in PEL,15 it remains possible that TRAF6 is part of the IκK activation complexes nucleated by the K13 and K15 proteins. Overall, even if the mechanism requires further elucidation, the findings by Thome and colleagues clearly point to novel ways of MALT1 activation (Figure 2).
Beyond the classical CBM-mediated pathway, the emerging evidence summarized here has suggested the existence of alternative mechanisms to trigger or regulate MALT1 paracaspase activity. Clearly, MALT1 as a scaffold protein has still a lot to reveal in terms of a potential interactome. Either directly, through its death, protease, or Ig-like domains, or indirectly, via its key binding partners, for example, CARD/CARMA proteins, BCL10 and TRAF6, MALT1 appears to be poised for interactions with signaling platforms and for providing synergistic input through its paracaspase activity. Unraveling the signaling network of MALT1 will be valuable to better understand the impact of MALT1 protease inhibition on pathophysiological mechanisms.
Acknowledgments
The authors thank Christopher Farady for his critical reading of the manuscript.
Footnotes
The authors declare no conflict of interest.
References
- Hulpiau P, Driege Y, Staal J, Beyaert R. MALT1 is not alone after all: Identification of novel paracaspases. Cell Mol Life Sci 2016; 73: 1103–1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lan P, Fan Y, Zhao Y, Lou X, Monsour HP, Zhang X et al. TNF superfamily receptor OX40 triggers invariant NKT cell pyroptosis and liver injury. J Clin Invest 2017; 37: 524–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonsignore L, Passelli K, Pelzer C, Perroud M, Konrad A, Thurau M et al. A role for MALT1 activity in Kaposi’s sarcoma-associated herpes virus latency and growth of primary effusion lymphoma. Leukemia 2017; 31: 614–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du MQ. MALT lymphoma: genetic abnormalities, immunological stimulation and molecular mechanism. Best Pract Res Clin Haematol 2017; 30: 13–23. [DOI] [PubMed] [Google Scholar]
- Meininger I, Krappmann D. Lymphocyte signaling and activation by the CARMA1-BCL10-MALT1 signalosome. Biol Chem 2016; 397: 1315–1333. [DOI] [PubMed] [Google Scholar]
- McAllister-Lucas LM, Lucas PC. Finally, MALT1 is a protease!. Nat Immunol 2008; 9: 231–233. [DOI] [PubMed] [Google Scholar]
- Lenz G, Davis RE, Ngo VN, Lam L, George TC, Wright GW et al. Oncogenic CARD11 mutations in human diffuse large B cell lymphoma. Science 2008; 319: 1676–1679. [DOI] [PubMed] [Google Scholar]
- Baens M, Bonsignore L, Somers R, Vanderheydt C, Weeks SD, Gunnarsson J et al. MALT1 auto-proteolysis is essential for NF- κB B-dependent gene transcription in activated lymphocytes. PLoS One 2014; 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginster S, Bardet M, Unterreiner A, Malinverni C, Renner F, Lam S et al. Two antagonistic MALT1 auto-cleavage mechanisms reveal a role for TRAF6 to unleash MALT1 activation. PLoS ONE 2017; 12: e0169026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willoughby J, Griffiths J, Tews I, Cragg MS. OX40: structure and function—what questions remain? Mol Immunol 2017; 83: 13–22. [DOI] [PubMed] [Google Scholar]
- So T, Croft M. Regulation of the PKCθ-NF-κB axis in T lymphocytes by the tumor necrosis factor receptor family member OX40. Front Immunol 2012; 3: 133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scudiero I, Zotti T, Ferravante A, Vessichelli M, Vito P, Stilo R. Alternative splicing of CARMA2/CARD14 transcripts generates protein variants with differential effect on NF-??B activation and endoplasmic reticulum stress-induced cell death. J Cell Physiol 2011; 226: 3121–3131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amatya N, Garg AV, Gaffen SL. IL-17 signaling: the yin and the yang. Trends Immunol 2017; 38: 310–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelzer C, Cabalzar K, Wolf A, Lenz G, Thome M, Gonzalez M et al. The protease activity of the paracaspase MALT1 is controlled by monoubiquitination. Nat Immunol 2013; 14: 337–345. [DOI] [PubMed] [Google Scholar]
- Shigemi Z, Furukawa Y, Hosokawa K, Minami S, Matsuhiro J, Nakata S et al. Diallyl trisulfide induces apoptosis by suppressing NF-B signaling through destabilization of TRAF6 in primary effusion lymphoma. Int J Oncol 2016; 48: 293–304. [DOI] [PubMed] [Google Scholar]