Abstract
Melanosis vesica is a rare condition and thought to be benign. We report the case of a 50-year-old man who presented with haematuria and was found to have a diffusely pigmented bladder on cystoscopy and high grade transitional cell carcinoma of his upper and lower renal tract. This required a laparoscopic nephroureterectomy and pathology confirmed a diagnosis of melanosis vesica. Melanosis vesica has only been associated with high grade transitional cell carcinoma in one previous case. We recommend that any patient presenting with bladder melanosis is monitored for the development of upper or lower urinary tract transitional cell carcinoma.
Keywords: Urinary tract, Carcinoma, Bladder - Melanosis
Melanosis of the bladder (or melanosis vesica) is a rare condition. Fewer than 20 cases have been reported in the literature to date. It is thought to be a benign condition1 and has only once been reported in association with high grade transitional cell carcinoma (TCC) of the bladder.2 It is important to distinguish from malignant melanoma of the bladder, which may look similar cystoscopically. This is again rare, with only 19 reported cases of primary melanoma to date.3
Melanosis occurs when there are excessive deposits of melanin in bladder tissue. It has rarely been reported in the genitourinary system but commonly affects the skin and oral mucosa.
Case history
A 50-year-old man was referred to clinic with loin pain and haematuria. He had no other medical problems apart from hypertension, for which he was taking routine medication. Computed tomography (CT) was performed and he was found to have a duplex right kidney containing renal calculi and a thickened right renal pelvis. This was thought to be due to the recent passage of stones. However, a tumour could not be ruled out.
Following a discussion in clinic, the patient declined a cystoscopy and renal ultrasonography confirmed stones but no other obvious pathology. Outpatient CT urography was arranged and on this he was found to have a tumour in the right renal pelvis and distal right ureter. Cystoscopy and ureteroscopy revealed a diffusely pigmented bladder as well as a right ureteric TCC. Biopsies were taken from the right ureter and the bladder.
After the biopsy results, a right laparoscopic nephroureterectomy with an open lower end was performed to remove the renal and ureteric tumour. At the time of surgery pictures were taken of the bladder cystoscopically (Fig 1) and when the bladder was opened (Fig 2), clearly showing deposits of brown pigment.
Figure 1.
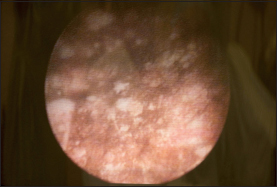
Melanin deposits seen in the bladder at cystoscopy
Figure 2.
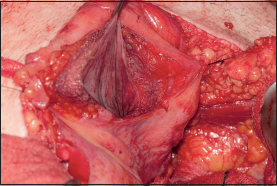
Melanin deposits seen in the bladder during open surgery
Histopathology results of the initial bladder biopsy using haematoxylin and eosin (H&E) staining revealed dark brown granular deposits of intracytoplasmic pigment within urothelial cells at all levels (Fig 3). Perls’ Prussian blue stain was negative, excluding haemosiderin, but the pigment stained positive with Schmorl’s stain (Fig 4), confirming that it was melanin. In addition, immunocytochemistry was performed for S100 and Melan-A, which revealed no evidence of malignant melanoma or other melanocytic lesion. From this, a diagnosis of melanosis vesica was made.
Figure 3.
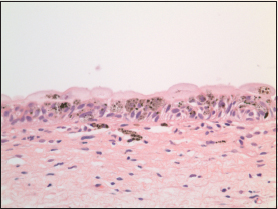
Haematoxylin and eosin stain (40x magnification): The melanin deposits appear dark brown on staining.
Figure 4.
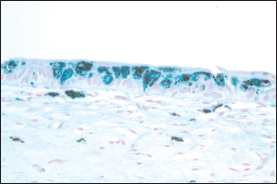
Schmorl’s stain (40x magnification): The melanin deposits appear blue-green on staining.
The initial right ureteric biopsy demonstrated an invasive TCC. Histological examination of the subsequent nephroureterectomy specimen confirmed a grade 3 invasive TCC arising in one of the two ureters and invading into the wall of this ureter (pT2).
Discussion
Melanosis of the bladder is a rare condition first reported in 19864 and its incidence is unknown. A PubMed search was performed looking at all English literature with the keywords ‘melanosis’, ‘bladder’, ‘melanosis vesica’ and ‘genito-urinary melanosis’. Fewer than 20 cases were found.
In the majority of cases, patients report symptoms including haematuria, dysuria, difficulty voiding, cystitis and/or urinary incontinence.5 Uncertainty remains as to whether the melanin deposits contribute to the symptoms or whether they are an incidental finding. It has been reported in men and woman of ages ranging from 43 to 86 years.2
On cystoscopy, the bladder is found to be dark brown in appearance, the affected area is often multifocal and deposits can be found at any location in the bladder.2,5 This dark colour can be due to melanosis, melanoma, haemosiderin or lipochrome deposits and these can be differentiated by histological examination.
Histologically, standard H&E staining does not distinguish reliably between melanin and other possible types of dark pigment. Melanin deposits stain dark blue-green with Schmorl’s stain. A Fontana–Masson stain can also be used and will stain melanin black.
The most important differential diagnosis for melanosis vesica is malignant melanoma. While this is again rare, biopsies must be taken to rule out this serious pathology.
Whether melanosis of the bladder is a benign condition remains under debate. Only one case has been reported where melanosis vesica has been associated with the development of a high grade papillary bladder TCC (pT1N0M0).2 This patient underwent complete endoscopic resection. Following this, she underwent bacilli Calmette–Guérin therapy and is under regular surveillance for recurrence. Our case is the second that has been associated with high grade TCC of the urinary tract affecting the kidney and the ureter. This suggests that melanosis vesica may be a premalignant condition and that patients with melanosis vesica are at risk of developing cancer in their urinary tract. We plan to follow up our patient with regular surveillance, both cystoscopically and radiologically, for tumour recurrence.
Conclusions
Melanosis of the bladder is a rare condition. This is the second reported case in which it has been associated with high grade TCC of the urinary tract and the first case in a patient who has been found to have renal and ureteric TCC. Our recommendation is that patients with this condition should be monitored for development of malignancy in the lower and upper urinary tract.
References
- 1.Jin B, Zaidi SY, Hollowell M et al. A unique case of urinary bladder simple melanosis: a case report and review of the literature. Diagn Pathol 2009; 4: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sanborn L, MacLennan G, Cooney MM et al. High-grade transitional cell carcinoma and melanosis of the urinary bladder: case report and review of the literature. Urology 2009; 73: 928.e13–928.e15. [DOI] [PubMed] [Google Scholar]
- 3.Siroy AE, MacLennan GT. Primary melanoma of the bladder. J Urol 2011; 185: 1,096–1,097. [DOI] [PubMed] [Google Scholar]
- 4.Alroy J, Ucci AA, Heaney JA et al. Multifocal pigmentation of prostatic and bladder urothelium. J Urol 1986; 136: 96–97. [DOI] [PubMed] [Google Scholar]
- 5.Talmon GA, Khan AU, Koerber RK, Johansson SL. Simple melanosis of the bladder: a rare entity. Int J Surg Pathol 2010; 18: 547–549. [DOI] [PubMed] [Google Scholar]


