Abstract
Introduction
Hepatobiliary cystadenomas are rare cystic tumours that can arise from any portion of the biliary tract but most commonly develop intrahepatically. They typically cause non-specific symptoms and are often detected incidentally. Cystadenomas can be mistaken for simple hepatic cysts on radiological imaging, which leads to inadequate treatment. Hepatobiliary cystadenomas have a malignant predisposition and a high recurrence rate. Complete excision including hepatic resection is therefore generally recommended.
Methods
Three cases of hepatobiliary cystadenoma were identified at one unit over a six-month period. Their clinical details and management are reported.
Results
Three female patients are described aged 25, 37 and 73 years. One patient presented because of recurrent infection, one presented because of pressure related symptoms and one lesion was identified incidentally. All patients were investigated by ultrasonography and computed tomography (CT), two additionally had magnetic resonance imaging (MRI) and one had a liver biopsy. The tumours were 4–16cm in size and all lesions were excised by non-anatomical, parenchyma sparing resections. Histology revealed mixed epithelium with underlying ovarian-like stroma.
Conclusions
The management of hepatic cystadenomas as well as operative and pathological findings are discussed. Preoperative ultrasonography, CT and MRI is recommended, and early referral for specialist hepatobiliary review is advised. Operative resection is also recommended and complete excision was achieved in these cases. This strategy is supported by the current literature and recurrence has been shown to be unlikely.
Keywords: Hepatobiliary cystadenoma, Hepatobiliary tumour, Hepatobiliary cystic lesion
Hepatobiliary cystadenomas are rare benign tumours of the liver and account for 5% of hepatic cystic lesions.1 These cyst forming neoplasms do not usually contain a communication with the bile ducts and are associated with ovarian-type subepithelial stroma.2 They can arise in any portion of the biliary tree although most are identified in the hepatic parenchyma.3–5 Hepatobiliary cystadenomas occur most frequently in middle aged women (80–90%) and present typically with non-specific symptoms such as abdominal pain and fullness, nausea and anorexia.1,3,6–9 Many are found incidentally on abdominal imaging1–3,4,7–9 and liver function tests are generally normal unless there is compression of the biliary tree. Diagnosis is often made radiologically using ultrasonography, computed tomography (CT), magnetic resonance imaging (MRI) or magnetic retrograde cholangiopancreatography (MRCP).1,3–5,7,10–14
Hepatobiliary cystadenomas should be excised completely to prevent recurrence (up to 90% following incomplete excision) and because of their malignant potential (30% become invasive).1,3,5,7–10,12 Prognosis following complete excision is excellent due to the benign nature of the lesions.1,3,5–10,12 Pathological examination reveals a smooth cystic macroscopic appearance while histological assessment may reveal the presence of ovarian stroma in the tumour wall.2,6,15,16
We report three patients with hepatobiliary cystadenomas treated at our unit, and describe their presentation, management and operative histology.
Case histories
Three patients with histologically confirmed diagnoses of hepatobiliary cystadenoma were identified at our institution over a six-month period (February – July 2012).
Case 1
A 25-year-old woman had an incidental solitary 4cm cystic lesion in the left side of the liver detected on CT. Haematological investigations including hydatid serology and tumour markers were unremarkable. Subsequent MRI (Fig 1) showed that the cystic lesion contained proteinaceous fluid or blood and a liver biopsy revealed a hepatobiliary cystadenoma.
Figure 1.
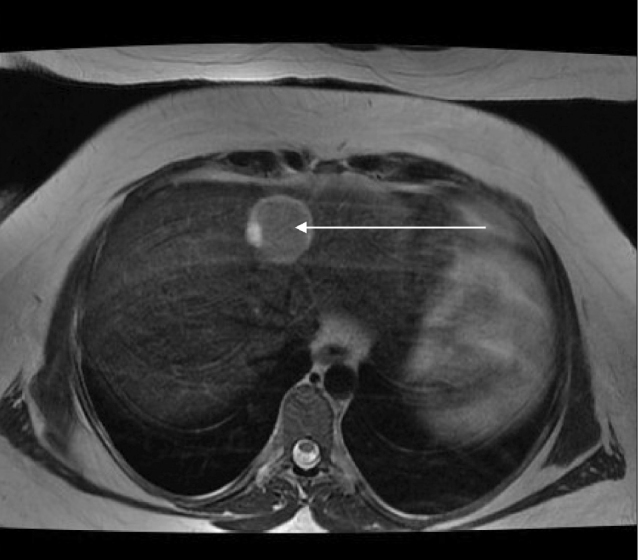
Magnetic resonance imaging with hepatobiliary contrast showing a left-sided 4cm hepatic cystic lesion containing proteinaceous fluid or blood (arrow)
A single smooth 4cm cystic lesion was identified at operation and confirmed on intraoperative ultrasonography at the border of segments 2 and 4 of the liver. As there was no evidence of local invasion, a wedge resection was performed and the patient recovered well. Histology confirmed a cystadenoma, with the cyst locules ranging from flattened to cuboid to columnar mucinous epithelium. Ovarian-like stroma was seen but there was no evidence of malignant invasion.
Case 2
A 37-year-old fit and well woman presented with a 3-month history of right upper quadrant abdominal pain associated with an epigastric mass. Routine haematological investigations including hydatid and amoebic serology were normal apart from a mildly elevated carbohydrate antigen (CA) 19-9 of 45iu/ml (normal <35iu/ml). Ultrasonography revealed a large central haemorrhagic hepatic cyst and subsequent CT confirmed a large central hepatic cyst (Fig 2a), with two satellite lesions in the right inferior aspect of the liver. The inferior portion of the cyst splayed open the inflow to the right and left sides of the liver (Fig 2b). Subsequent MRI revealed that the cyst had a solid component with papillary projections, which had been misinterpreted as haemorrhage on ultrasonography. These features were consistent with hepatic cystadenoma and operative excision was planned.
Figure 2.
Computed tomography showing a 16cm central hepatic cystic lesion (A), and the cyst splaying the right and left portal vein branches (B), and intraoperative photographs showing large central hepatic cystic lesion before excision (C)
At operation, a 16cm central hepatic cystic lesion was identified, which splayed the inflow to the left and right lobes of the liver (Fig 2c). Intraoperative ultrasonography showed the lesion to be thin walled, without a solid component, and no invasive features could be demonstrated. Local excision was therefore undertaken, which was facilitated by cautious decompression of the lesion. A small bile leak from the left hepatic duct was noted and repaired although this later required biliary decompression via endoscopic retrograde cholangiopancreatography (ERCP) for persistent bile leakage. Macroscopic examination revealed a 16cm unilocular cystic lesion, with evidence of haemorrhage into the cyst. Histological investigation demonstrated bland columnar mucinous-type epithelium, with a band of spindle cell ovarian-like stroma underlying it, consistent with a hepatic cystadenoma.
Case 3
A 74-year-old woman was referred following multiple episodes of hepatic cyst infection. She had presented initially with a liver abscess more than ten years earlier and CT revealed a septated lesion with areas of calcification. Over the preceding two years, she had two further episodes of recurrent bacteraemia (Enterobacter cloacae and Escherichia coli) that responded to antibiotics and radiological drainage. Routine haematological investigations including hydatid serology were unremarkable but her CA19-9 was elevated at 243iu/ml (normal <35iu/ml). CT showed a complex 8cm septated cyst in the left lobe of the liver (Fig 3), which was close to the proximity of the right portal inflow and consistent with a cystadenoma. Despite awareness that operative intervention would be difficult and likely to require a formal left hemihepatectomy, resection was advised to prevent septic episodes.
Figure 3.
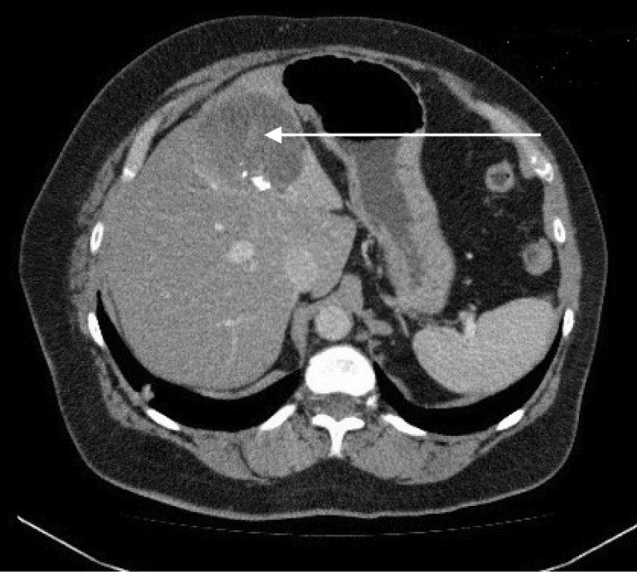
Computed tomography showing a complex 8cm septated cyst in the left lobe of the liver (arrow)
At operation, a large solitary cyst was identified in the left lateral sector of the liver in close proximity to the inflow structures, which was confirmed by intraoperative ultrasonography. A formal left lateral sectorectomy (segments 2 and 3) was undertaken and the patient made an uncomplicated recovery. Pathological examination identified a multilocular cyst measuring 70mm in maximal diameter. Histological examination revealed a smooth inner lining to each of the cyst locules, which ranged from flattened epithelium to cuboid to columnar mucinous cells. The underlying stroma showed focal ovarian-type change consistent with a hepatobiliary cystadenoma and there was no evidence of invasive malignancy.
Discussion
Hepatobiliary cystadenomas are rare, slow growing tumours that can arise from any portion of the biliary tree although there is a predominance for the intrahepatic component (80–90%).1,13,16 Of these intrahepatic lesions, 55% arise in the right lobe, 29% in the left lobe and 16% are bilobar.17 They account for less than 5% of all biliary neoplasms1 and are more than 1,000 times rarer than simple hepatic cysts.14,16 The vast majority of cystadenomas (80–90%) are found in middle aged women, with a mean age at presentation of 50 years,1,7–9 suggesting a possible hormonal pathogenesis of these lesions.10
Hepatobiliary cystadenomas are typically asymptomatic and often large at diagnosis.10,11 They may cause mass effect symptoms including pain, fullness in the upper abdomen and nausea.3,7,9–11,17 The tumours may occasionally lead to biliary obstruction, with resulting jaundice and cholangitis,17 and they can rarely rupture, haemorrhage, become infected (as in Case 3) or even cause vena caval obstruction.4 Haematological and biochemical investigations are rarely diagnostic but anti-Echinococcus and antiamoebic serology can assist in diagnosis.14,17 Serum tumour markers are usually normal although carcinoembryonic antigen and CA19-9 levels in cyst fluid may be elevated.12
Radiological assessment is usually diagnostic although there are similarities with other hepatic cystic lesions including simple cysts, hydatid lesions, liver abscesses and malignant cystic lesions, Caroli’s disease, post-traumatic cysts and polycystic disease.8,10,15,17 Ultrasonography and CT are most commonly used to characterise the lesion and any involvement of the biliary tree or hepatic vasculature. The use of supplemental MRI in cases of diagnostic uncertainty is increasing.5,10,17
Typical radiological features include the presence of multiloculated cystic lesions with internal septa, containing mucin or blood.14,17 The wall of the lesion is often thickened and irregular, with papillary protrusions and calcium deposits.5,17 Distinguishing between benign and malignant lesions on radiological imaging can be difficult although the presence of a solid component increases the likelihood of malignancy (cystadenocarcinoma). In the presence of malignant lesions, both ERCP and MRCP can provide assessments of the biliary and pancreatic ducts for possible tumour invasion, with MRCP additionally giving information about the biliary tree proximal to any obstruction.14
Diagnostic accuracy is critical prior to definitive treatment as incomplete excision of these lesions is associated with frequent local recurrence (90%) and a high rate of progression to malignancy (30%).1,16 Complete excision is recommended to prevent malignant degeneration either via a formal liver resection10,13,17 or a more conservative resection if disease free resection margins can be achieved.13,17 Misdiagnosis resulting in simple de-roofing of the cyst should result in reoperation and radical resection to achieve clearance. The prognosis after complete removal of a cystadenoma is excellent while cystadenocarcinomas have a survival profile comparable with intrahepatic cholangiocarcinomas, with specific survival dependent on tumour grade, lymph node status and the degree of involvement of the resection margin.13,17
Macroscopically, the lesions are globular with a smooth external surface and they consist of multiloculated cavities that contain mucinous fluid.8–10,16 Microscopically, they are lined with columnar or cuboid, non-ciliated cells and are generally (85–90%) surrounded by a dense ‘ovarian-like’ stroma.7,8,10,11 The presence of this ovarian-like stroma has been accepted recently as a prerequisite for diagnosis for cystadenomas, helping to differentiate from intraductal papillary neoplasms.6 Invasion through the basement membrane is diagnostic of a cystadenocarcinoma.7 Immunohistochemical staining for biliary immunophenotypes should be positive for cytokeratin (CK) 7; expression of CK20, mucin (MUC) 2, MUC5AC and MUC6 is seen in borderline tumours, and MUC1 expression is seen in malignancy.6
The histogenesis of these lesions is not fully understood. The presence of a stroma reminiscent of a fetal gallbladder suggests the lesions may originate from remnants of primitive hepatobiliary tissue4,7,8 while the expression of oestrogen or progesterone receptors in the ovarian-like stroma suggests that female hormones may affect tumourogenesis.6
Conclusions
Hepatobiliary cystadenomas are uncommon and frequently misdiagnosed hepatic cystic lesions. They can be mistaken for other hepatic cystic lesions and may subsequently be treated inadequately by de-roofing. Complete resection is the optimal treatment to prevent recurrence and later malignant transformation. Although uncommon, a diagnosis of hepatobiliary cystadenoma should be considered preoperatively in all patients with atypical hepatic cystic lesions. If diagnostic uncertainty exists, radical excision is advised.
References
- 1.Ishak KG, Willis GW, Cummins SD, Bullock AA. Biliary cystadenoma and cystadenocarcinoma: report of 14 cases and review of the literature. Cancer 1977; 39: 322–338. [DOI] [PubMed] [Google Scholar]
- 2.Tsui WM, Adsay NV, Crawford JM et al. . Mucinous Cystic Neoplasms of the Liver. In: Bosman FT, Carnerio F, Hruban RH, Theise ND. WHO Classification of Tumours of the Digestive System. Geneva: WHO Press; 2010. pp236–238. [Google Scholar]
- 3.Kim K, Choi J, Park Y et al. . Biliary cystadenoma of the liver. J Hepatobiliary Pancreat Surg 1998; 5: 348–352. [DOI] [PubMed] [Google Scholar]
- 4.Lewin M, Mourra N, Honigman I et al. . Assessment of MRI and MRCP in diagnosis of biliary cystadenoma and cystadenocarcinoma. Eur Radiol 2006; 16: 407–413. [DOI] [PubMed] [Google Scholar]
- 5.Ratti F, Ferla F, Paganelli M et al. . Biliary cystadenoma: short- and long-term outcome after radical hepatic resection. Updates Surg 2010; 64: 13–18. [DOI] [PubMed] [Google Scholar]
- 6.Zen Y, Pedica F, Patcha VR et al. . Mucinous cystic neoplasms of the liver: a clinicopatholigcal study and comparison with intraductal papillary neoplasms of the bile duct. Mod Pathol 2011; 24: 1,079–1,089. [DOI] [PubMed] [Google Scholar]
- 7.Gadzijev E, Ferlan-Marolt V, Grkman J. Hepatobiliary cystadenomas and cystadenocarcinoma. Report of five cases. HPB Surg 1996; 9: 83–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Subramony C, Herrera GA, Turbat-Herrera EA. Hepatobiliary cystadenoma. A study of five cases with reference to histogenesis. Arch Pathol Lab Med 1993; 117: 1,036–1,042. [PubMed] [Google Scholar]
- 9.Davies W, Chow M, Nagorney D. Extrahepatic biliary cystadenomas and cystadenocarcinoma. Ann Surg 1995; 222: 619–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thomas KT, Welch D, Trueblood A et al. . Effective treatment of biliary cystadenoma. Ann Surg 2005; 241: 769–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Palacios E, Shannon M, Solomon C, Guzman M. Biliary cystadenoma: ultrasound, CT, and MRI. Gastrointest Radiol 1990; 15: 313–316. [DOI] [PubMed] [Google Scholar]
- 12.Lewis WD, Jenkins RL, Rossi RL et al. . Surgical treatment of biliary cystadenoma. Arch Surg 1988; 123: 563–568. [DOI] [PubMed] [Google Scholar]
- 13.Mortelé KJ, Ros PR. Cystic focal liver lesions in the adult: differential CT and MR imaging features. Radiographics 2001; 21: 895–910. [DOI] [PubMed] [Google Scholar]
- 14.Buetow PC, Buck JL, Pantongrag-Brown L et al. . Biliary cystadenoma and cystadenocarcinoma: clinical-imaging-pathologic correlations with emphasis on the importance of ovarian stroma. Radiology 1995; 196: 805–810. [DOI] [PubMed] [Google Scholar]
- 15.Teoh AY, Ng SS, Lee KF, Lai PB. Biliary cystadenoma and other complicated cystic lesions of the liver: diagnostic and therapeutic challenges. World J Surg 2006; 30: 1.560–1,566. [DOI] [PubMed] [Google Scholar]
- 16.Devaney K, Goodman ZD, Ishak KG. Hepatobiliary cystadenoma and cystadenocarcinoma. A light microscopic and immunohistochemical study of 70 patients. Am J Surg Pathol 1994; 18: 1,078–1,091. [PubMed] [Google Scholar]
- 17.Koffron A, Rao S, Ferrario M, Abecassis M. Intrahepatic biliary cystadenoma: role of cyst fluid analysis and surgical management in the laparoscopic era. Surgery 2004; 136: 926–936. [DOI] [PubMed] [Google Scholar]



