Sir,
Endobronchial Ultrasound-guided Transbronchial Needle Aspiration (EBUS-TBNA) has evolved into a standard of care modality for evaluation of mediastinal lymphadenopathy and is usually performed through the oral route under moderate sedation.[1] If required, it can also be performed under general anaesthesia through a supraglottic airway or an endotracheal tube. The larger diameter of the EBUS scope (6.9–7.4 mm) than that of the flexible bronchoscope (4.9–6.0 mm, adult bronchoscope and 2.8–4.9 mm, paediatric bronchoscope) limits its utility in the paediatric population. Nonetheless, a few studies have described the utilisation of EBUS-TBNA in paediatric population.[2,3,4] Issues peculiar to children for performing EBUS include the choice of anaesthesia as well as airway management. We describe the utilisation of EBUS-TBNA in a child, primarily focussing on the anaesthetic issues encountered.
An 8-year-old child with subcarinal lymphadenopathy was planned for EBUS-TBNA. The EBUS bronchoscope (BF-UC 180F, Olympus Medical Systems, Japan, diameter 6.9 mm) has a convex-shaped ultrasound transducer with 30° forward oblique vision as compared to 0° view in flexible bronchoscope. It was decided to ventilate the lungs using I-gel™ that would also allow smooth passage of the EBUS bronchoscope. Anaesthesia was induced with inhalational sevoflurane, and neuromuscular blockade was achieved with intravenous atracurium (0.5 mg/kg) followed by insertion of a size 2 I-gel™. Anaesthesia was maintained with sevoflurane and O2:air (50:50) mixture. Low tidal volume ventilation (6 mL/kg with a respiratory rate of 14–16/min) was initiated using anaesthesia circuit and a catheter mount. A triradiate incision was ade over the catheter mount opening to allow the smooth passage of EBUS bronchoscope [Figure 1a]. After applying sufficient lubricating jelly, the EBUS scope was introduced through the I-gel™ [Figure 1b]. However, due to the forward oblique view, the bronchoscope could not be negotiated through vocal cords with I-gel™ in place [Figure 1c]. The I-gel™ was withdrawn by 3 cm after removing the securing tapes to release the pressure on larynx [Figure 1d]. This manoeuvre allowed for easy displacement of epiglottis upward by the bronchoscope and it was easily passed into the trachea. After the bronchoscope had reached the mid-tracheal lumen, the I-gel™ was advanced back to its original position and secured. An enlarged subcarinal lymph node was identified and three EBUS-TBNA aspirates were obtained. Intermittent removal of the EBUS bronchoscope between the passes was performed to facilitate ventilation. Following procedure completion, neuromuscular blockade was reversed and I-gel™ was removed once the patient regained spontaneous breathing.
Figure 1.
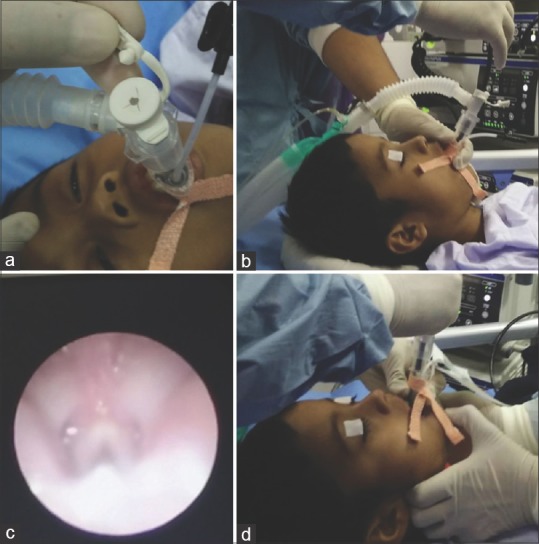
(a) Triradiate incision is made on the opening of catheter mount to allow smooth passage of large size endobronchial ultrasound-guided bronchoscope. (b) Endobronchial ultrasound scope being inserted through the supraglottic airway. (c) Image demonstrating the difficulty in negotiating the vocal cords through the supraglottic airway. (d) For passage of scope through vocal cords, the supraglottic airway had to be withdrawn 2 cm proximally after removing the fixing tapes
The utilisation of EBUS-TBNA in paediatric population has been slow paced. As the EBUS bronchoscope can occupy a large part of paediatric airway, it is important for the anaesthetist to monitor for hypoventilation during the procedure. End-tidal carbon dioxide (EtCO2) monitoring is a useful tool in these cases. If EtCO2 monitoring is not available, removal of EBUS bronchoscope in between passes may help in preventing hypoventilation. The usual approach to airway entry during EBUS-TBNA performed under general anaesthesia is placement of an airway conduit followed by EBUS bronchoscope insertion through the conduit. This technique may result in difficulty in airway access (as in our case), as in children, the epiglottis is longer, narrower, and posteriorly angled. We propose that EBUS bronchoscope-guided airway insertion (I-gel mounted over the EBUS bronchoscope) will solve this problem. With this technique, both airway entry for bronchoscope and artificial airway placement can be done quickly.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Madan K, Mohan A, Ayub II, Jain D, Hadda V, Khilnani GC, et al. Initial experience with endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) from a tuberculosis endemic population. J Bronchology Interv Pulmonol. 2014;21:208–14. doi: 10.1097/LBR.0000000000000080. [DOI] [PubMed] [Google Scholar]
- 2.Dhooria S, Madan K, Pattabhiraman V, Sehgal IS, Mehta R, Vishwanath G, et al. Amulticenter study on the utility and safety of EBUS-TBNA and EUS-B-FNA in children. Pediatr Pulmonol. 2016;51:1031–9. doi: 10.1002/ppul.23415. [DOI] [PubMed] [Google Scholar]
- 3.Gilbert CR, Chen A, Akulian JA, Lee HJ, Wahidi M, Argento AC, et al. The use of convex probe endobronchial ultrasound-guided transbronchial needle aspiration in a pediatric population: A multicenter study. Pediatr Pulmonol. 2014;49:807–15. doi: 10.1002/ppul.22887. [DOI] [PubMed] [Google Scholar]
- 4.Madan K, Ayub II, Mohan A, Jain D, Guleria R, Kabra SK, et al. Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) in mediastinal lymphadenopathy. Indian J Pediatr. 2015;82:378–80. doi: 10.1007/s12098-014-1665-3. [DOI] [PubMed] [Google Scholar]


