Abstract
This study introduces a computerized clinical decision-support tool, the Fluid Outpatient Rehabilitation Treatment (FORT), that incorporates individual and ever-evolving patient needs to guide clinicians in developing and updating treatment decisions in real-time. In this proof-of-concept feasibility pilot, FORT was compared against traditional treatment planning using similar behavioral therapies in 52 adults with severe mental illness attending community-based day treatment. At post and follow-up, group differences and moderate to large effect sizes favoring FORT were detected in social function, work readiness, self-esteem, working memory, processing speed, and mental flexibility. Of participants who identified obtaining a GED as their primary goal, 73% in FORT passed the exam compared to 18% in traditional treatment planning. FORT was also associated with higher agency cost-effectiveness and a better average benefit-cost ratio, even when considering diagnosis, baseline symptoms, and education. While the comparison groups were not completely equivalent, the findings suggest computerized decision support systems that collaborate with human decision-makers to personalize psychiatric rehabilitation and address critical decisions may have a role in improving treatment effectiveness and efficiency.
Keywords: Computerized decision support system, schizophrenia, personalized treatment, health informatics, clinical decision-making
Introduction
Adults with serious mental illness face significant challenges as they learn skills for a productive and satisfying life (McGurk et al., 2010; Tsang et al., 2010), with profound cognitive and social deficits interfering with the ability to navigate the job market and community resources (Bowie et al., 2012; Twamley et al., 2012; Reddy et al., 2014). These individuals may be referred to day treatment programs that tend to rely on traditional modes of treatment planning, where treatment providers decide on a ‘course’ of treatment and create a treatment plan that may be updated at only 6-month intervals, if then, and may not contain an evaluation of treatment effectiveness. These plans rely on a set treatment course over a period of months with only minimal tailoring to the changing needs of the patient (Essock and Hogan, 2011). In addition, behavioral therapies offered at many day treatment programs are manualized and delivered in such a way that a patient progresses through the same set of lessons, at the same pace as everyone else every week, regardless of his or her response to those lessons. Hence, while the actual treatments administered may be evidence-based, one could argue that advancing participants through the lessons even when they have not adequately learned the previous lesson is not evidence-based practice (Dixon et al., 2010). This “one-size-fits-all” approach does not take into consideration the significant variability in the longitudinal recovery of neurocognitive, social, symptom, and everyday functioning, leading to sub-optimal outcomes for many (Liu et al, 2011).
Personalizing treatments can be a complex process that entails not only collecting and synthesizing large amounts of individual data, but also continually updating these datasets with new information as it becomes available over the course of treatment. How one organizes and uses this information to inform treatment is the field of decisional informatics. Within the focused area of serious mental illnesses, Spaulding and Deogun (2011) have been at the forefront of championing the introduction of decisional informatics into treatment planning. As this is a relatively new emphasis area within treatments for individuals diagnosed with serious mental illness, to date there are no published studies using decisional informatics in psychosocial treatment planning.
In this article, we introduce a computerized clinical decision support system called Fluid Outpatient Rehabilitation Treatment (FORT) that provides clinicians with tailored treatment planning, based on the patient’s current performance and rehabilitation needs. Baseline individual profile data are entered into FORT, which then outputs the most appropriate treatment plan, given the individual’s strengths, weaknesses, and treatment goals. Weekly, FORT reformulates the treatment plan for the upcoming week based on updated information about treatment progress. In cases where individuals fail to learn lesson content, the FORT algorithm identifies potential psychological, social functioning, cognitive or symptom variables that may have impacted this, and adjusts the treatment accordingly, in most cases to re-focus the treatment on variables that are associated with lack of treatment progress and that must be remediated before the previously set course of treatment is resumed. With FORT, treatment content for each individual is continually adjusted to maximize the efficacy of each treatment lesson presented, while minimizing exposure to sessions the participant does not learn from and that may negatively impact motivation to continue in the treatment as a whole. The resulting rehabilitation program is highly personalized.
We report the results from a pilot study that tested this mode of computerized clinical decision support against traditional treatment planning occurring in the context of a day treatment program for people with serious mental illnesses. The lesson plan and content were comprised of behavioral feedback and cognitive and social cognitive therapies, some of which were computer-based interventions. The primary question we asked was whether compared to traditional treatment planning, FORT would lead to better outcomes and greater cost-effectiveness. More specifically, we hypothesized that FORT would be related to better social function and work-readiness compared to traditional treatment planning.
Methods
Participants
Fifty-two adults with serious mental illness referred to a day treatment program in New York City were enrolled. Informed consent of the participants was obtained after the nature of the procedures had been fully explained. Immediately following informed consent and prior to any assessments, they were randomized to receive either traditional treatment planning or FORT using a simple randomization technique (flipping a coin). All participants received medication management and were enrolled in a weekly incentive work therapy program for 2 to 4 hours through the day treatment program. Those randomized to FORT received psychosocial interventions at a nearby clinical research office, which was one floor below the day treatment program, due to limitation in treatment space in the day treatment program. Assessments were conducted at baseline, end of the 4 month active phase, and at a 2-month follow-up by doctoral-level trainees not blind to group allocation. While we attempted to conduct a single-blind study, it became apparent that post-assessment and follow-up questions and interviews about social and work outcome could not be completed without disclosing information about treatments received during the active phase. The study was approved by the local institutional review board and conducted in accordance with the Helsinki Declaration as revised in 1989. Data was collected from August 2010 to October 2014.
Procedures
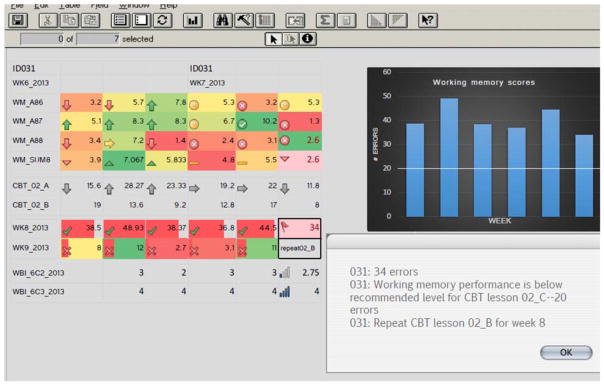
FORT took four distinct psychological therapies and modularized them into hierarchically structured, progressive lessons. Each lesson was individualized based on underlying cognitive resources needed to attend to and consolidate content, the prerequisite knowledge of therapy lesson content, comparable content and goals to concurrent therapies, and baseline profiles of symptom, work history, social functioning, and cognition. Data from weekly brief questionnaires, therapy lesson post-tests, updated cognitive training results, and the stored baseline profiles were entered into FORT’s computer algorithm using a data entry program similar to an Excel spreadsheet (Microsoft Access) to produce the lessons for the following week. FORT was developed by author JC and the algorithm is a programmed code of decisional kernels of cognitive, social cognitive, and group therapy performances that establishes relationships between these kernels to produce a suggested course of action. For instance, if patient 031 had not achieved at least a low average level of working memory ability during week 7, then that patient did not move on to cognitive-behavioral lessons that required at least low-average working memory, but would instead review and re-do previous lessons while continuing to shore up working memory skills in cognitive remediation. After calculating performance in cognitive remediation and CBT lesson post-tests, treatment suggestions were: continue to the next CBT lesson, re-do the lesson, or skip forward past the next lesson. A user-friendly output was generated by Microsoft Access for the treatment team at the end of the week suggesting the next course of action for next week’s lesson. This output listed the participant, week number in the study, the recommended therapy lesson for each category, and the reason for it (see Figure 1).
Figure 1.
Screenshot of decisional support tool (FORT) that shows patient 031 has not reached at least a low average level of working memory during week 7 and should not move on to the next CBT lesson that requires at least low average working memory (left side). This was presented in a user-friendly output (right side, bottom) that relayed the treatment suggestion and reason (too many working memory errors during cognitive training/testing that week). Microsoft Access with conditional formatting and icon sets.
FORT’s algorithm was similar to other computerized decisional support systems in that a hierarchy of rules was needed to establish relationships between decisional kernels on cognitive, social, and group therapy performance. Rules included prerequisite knowledge of therapy content for the next session, comparable content and goal with other concurrent therapies, and baseline cognitive ability. For example, this decisional rule on baseline cognitive ability was based on underlying cognitive resources needed to attend to and consolidate group therapy content. As alluded to in the example above, certain group sessions required a level of cognitive ability that was ascertained by baseline cognitive assessment. Each therapy session was assigned a cognitive load value of low, moderate, or high depending on how much content was expected to be learned. A CBT session that covered multi-step lessons in rephrasing negative thoughts was deemed “high cognitive load for working memory,” while a CBT lesson that was more experiential rather than learning was deemed a “low working memory load.” Subsequently, a high working memory load session required at least a low average range of working memory ability while a low working memory load session was permissible for any participant including those with impaired working memory. In this way, a cut-off of low average ability in working memory (24th percentile) was needed for any high working memory load group session.
While the ideal treatment algorithm would allow a participant to repeat cognitive training sessions to shore up working memory skills until a low average range was reached, in this proof-of-concept study, the number of times a cognitive training lesson could be repeated was limited to three. This was the number of times a participant could repeat a session without falling so far behind that the participant’s algorithm was beyond the following week’s schedule accommodating the groups. That is, a participant needed to cover a CBT or social cognition lesson regardless of their working memory skills within 4 weeks’ time in order for the group as a whole to gradually move forward. As FORT is further honed, we will need to explore the therapeutic value of repeating a lesson or advancing the participant regardless of more than 3 repeats in so much as to reduce the risk of frustration and disengagement that may arise from continual repetition.
While a decisional informatics system is simply a tool to create a fluid treatment plan and can use can be applied to most therapies or combinations of therapies, it does require that these treatments can be “taken apart” to provide distinct modules, so that individual treatment decision trees can be developed along with the necessary informatics algorithms. Unfortunately, we were not allowed to do so with the therapies offered through the comparator condition, the existing community-based traditional day treatment program. Hence, we sought to identify treatments that were similar to those offered in the traditional day treatment program and that could be modularized to provided discrete lessons that built upon each other, along with an opportunity to measure learning. The following four therapies were modularized for this particular demonstration of FORT: (1) Incentive Work Therapy (IWT) (Bell and Lysaker, 1997), 2 to 4 hours per week of paid work activity throughout the medical center (e.g. mailroom, janitorial service) including a weekly 50-minute session on performance feedback and goal setting, (2) Indianapolis Vocational Intervention Program (Lysaker et al., 2009), a weekly 50-minute cognitive behavioral therapy group that focused on modifying negative expectations about vocational issues, (3) computer-based social cognitive drill and practice training called Understanding Social Situations (Fiszdon et al., 2016) that targets attributional bias and theory of mind, and (4) a tablet-based cognitive remediation program for psychosis (Choi et al., 2016) designed to improve processing speed and working memory.
Participants randomized to traditional treatment planning engaged in vocational counseling, along with behavioral interventions common to community-based programs, including CBT for symptoms, social skills training, family support, and/or a computer skills class. Both FORT and traditional treatment planning groups consisted of 4 therapists providing 4 parallel behavioral therapies each week. While FORT required additional time to collect data from weekly brief questionnaires (10–15 min) and therapy lesson post-tests (5 min), and staff entering the data into FORT’s database (30–45 min) at the end of the week, traditional treatment planning consisted of hour-long weekly team meetings discussing the patient’s progress.
Instruments
Outcome measures were established instruments of social functioning, work-readiness, basic cognition, and symptoms. Primary outcomes were social functioning, which was measured using the Social Functioning Scale (SFS; Birchwood et al., 1990), and work-readiness, which was assessed using the Work Behavior Inventory (WBI; Bryson et al., 1997) to tap into work-appropriate behavior. Secondary work outcome was captured using the Employment Attitude Survey (EAS; Priebe et al., 1998) inquiring about receptiveness to finding employment, along with the Work Motivation Scale (WMS; Cook et al., 2008; Pickett et al., 1997) which measured motivation for employment. Tertiary outcomes included cost-effectiveness analysis (described in the data analysis section) and educational goal attainment as measured by the percentage of those who obtained their GED among those listing GED as their primary goal.
Other measures included overall self-esteem measured using the Rosenberg Self-esteem Scale (RSE; Rosenberg, 1965) and a range of cognitive and symptom measures. Attention and working memory were assessed respectively with the Digit Span subtest and Working Memory Index from Wechsler Adult Intelligence Scale-Third Edition (WASI-III; Wechsler, 1997). Speeded response was measured by the Minnesota Clerical Test (MCT; Andrew et al., 1979), a paper and pencil clerical test requiring minimal manual dexterity, while Trailmaking Test B (TMT B; Reitan, 1992) was used to measure speeded mental flexibility. Verbal memory was gauged with the Hopkins Verbal Learning Test-Revised (HVLT-R) delayed recall (Brandt, J., & Benedict, 2001). Abstract reasoning was assessed using the total number of errors on the Wisconsin Card Sorting Test (WCST; Heaton, 1993). In terms of symptoms, the Positive and Negative Syndrome Scale (PANSS; Kay et al., 1987) measured general psychopathology, while the Scale for the Assessment of Negative Symptoms (SANS; Andreasen, 1989) specifically measured the presence of negative symptoms. The level of depression was recorded using the Hamilton Depression Rating Scale (HDRS; Hamilton, 1960).
Data Analysis
An intent-to-treat analysis included all enrolled participants. FORT and traditional treatment planning groups were compared at baseline on demographic and clinical characteristics using independent sample t-tests. Despite careful randomization procedures, the FORT group had greater baseline PANSS and SANS scores, which dictated our subsequent analysis of covariance (ANCOVA) strategy. In a series of one-way ANCOVAs, group (FORT or traditional treatment planning) was the between-subjects variable, post-treatment, and 2-month follow-up scores on the SFS and WBI were the dependent measures, and baseline PANSS and SANS scores were used as covariates. We also performed another series of ANCOVAs for the secondary outcome measures, again using PANSS and SANS as covariates, to compare the two groups at post and follow-up in work motivation and attitude, self-esteem, cognition, and symptoms.
We also computed effect sizes (Hedges’ g) between FORT and traditional treatment planning at post and two months after treatment ended to generate between-group effect sizes for FORT. We tallied the success rate of those who identified obtaining a GED as their primary educational goal, and examined FORT’s productive efficiency using cost-effectiveness analysis (CEA). An agency perspective CEA was computed for each participant using hospital use and costs per unit of community treatment services for a 4-month period. Outpatient costs were based on 2010 Medicare cost reports for hospitals in the service areas of New York City. Total service costs for all time periods were computed for each participant by multiplying unit costs by service units provided. Estimated service costs for FORT and traditional treatment planning were compared using t-tests and multiple regression, with gender, education, baseline symptoms, diagnosis, and work history (hours worked in past 2 years) as covariates. Finally, while we did not obtain acceptability ratings for the two conditions, we did examine attrition rates among them.
Results
Of the 52 participants enrolled in the study, 42% were females, mean age was 35.3±10.2, and education level was 10.7±2.9 in the FORT group and 11.1±3.0 in the traditional treatment planning group. Participants were ethnically diverse, with 38% Caucasians, 28% African Americans, 28% Hispanics, and 6% Pacific Islanders. The majority was on atypical antipsychotics (93%), and diagnoses were schizophrenia (55%), schizoaffective disorder (27%), and bipolar type I (18%). While there were no baseline group differences in demographics and diagnosis, the FORT group had higher psychosis-related symptom severity on the PANSS and SANS at baseline (Table 1)(t[50]=8.43–10.47, p<0.01). Attrition at 2-month follow-up was 7% for FORT (27/29) and 14% for traditional treatment planning (20/23).
Table 1.
Baseline, post, and 2-month follow-up performance on outcome measures, by group, along with change scores from baseline, ANCOVA p-values, and between group effect sizes at post and follow-up.
| FORT (n=29) Mean (SD) | Change scores | Traditional Treatment Planning (n=23) Mean (SD) | Change scores | ANCOVA Significance (p-value) | Effect Size | |
|---|---|---|---|---|---|---|
| Social functioning | ||||||
| Baseline | 90.37 (17.48) | -- | 97.27 (14.65) | -- | -- | -- |
| Post (4mo) | 105.38 (10.11) | 15.01 | 102.43 (12.17) | 5.16 | 0.010 | 0.65 |
| Follow-up (6mo) | 103.42 (12.63) | 13.05 | 101.21 (13.47) | 3.94 | 0.019 | 0.56 |
| Work-related behavior | ||||||
| Baseline | 124.45 (14.27) | -- | 129.34 (12.42) | -- | -- | -- |
| Post (4mo) | 135.01 (12.03) | 10.56 | 130.96 (16.39) | 1.62 | 0.008 | 0.67 |
| Follow-up (6mo) | 134.77 (12.49) | 10.32 | 131.27 (15.72) | 1.93 | 0.009 | 0.62 |
| Employment attitude | ||||||
| Baseline | 20.23 (6.11) | -- | 22.76 (6.39) | -- | -- | -- |
| Post (4mo) | 26.57 (4.05) | 6.34 | 24.53 (6.88) | 1.77 | 0.002 | 0.88 |
| Follow-up (6mo) | 24.25 (6.19) | 4.02 | 23.34 (8.18) | 0.58 | 0.007 | 0.56 |
| Work motivation | ||||||
| Baseline | 21.25 (7.84) | -- | 24.32 (7.29) | -- | -- | |
| Post (4mo) | 26.02 (5.04) | 4.77 | 26.91 (5.81) | 2.59 | 0.045 | 0.33 |
| Follow-up (6mo) | 27.21 (4.29) | 5.96 | 26.43 (5.31) | 2.11 | 0.031 | 0.61 |
| Self-esteem | ||||||
| Baseline | 20.53 (5.29) | -- | 21.07 (7.27) | -- | -- | -- |
| Post (4mo) | 26.68 (5.03) | 6.15 | 24.02 (6.89) | 2.95 | 0.019 | 0.76 |
| Follow-up (6mo) | 25.63 (6.17) | 5.10 | 23.25 (6.18) | 2.18 | 0.020 | 0.56 |
| Attention | ||||||
| Baseline | 8.12 (2.17) | -- | 8.02 (2.34) | -- | -- | -- |
| Post (4mo) | 9.84 (1.73) | 1.72 | 9.69 (2.15) | 1.67 | 0.391 | 0.13 |
| Follow-up (6mo) | 8.94 (2.39) | 0.82 | 8.57 (2.95) | 0.55 | 0.322 | 0.15 |
| Working memory | ||||||
| Baseline | 86.28 (14.21) | -- | 89.53 (13.77) | -- | -- | -- |
| Post (4mo) | 94.71 (15.22) | 8.43 | 93.94 (16.52) | 4.41 | 0.048 | 0.30 |
| Follow-up (6mo) | 92.32 (14.27) | 6.04 | 91.44 (17.29) | 1.91 | 0.033 | 0.31 |
| Processing speed | ||||||
| Baseline | 34.67 (13.26) | -- | 36.18 (14.52) | -- | -- | -- |
| Post (4mo) | 46.94 (6.88) | 12.27 | 36.13 (15.77) | -0.05 | 0.000 | 1.14 |
| Follow-up (6mo) | 44.42 (9.27) | 9.75 | 37.63 (15.30) | 1.45 | 0.001 | 0.74 |
| Verbal memory | ||||||
| Baseline | 34.28 (11.29) | -- | 33.17 (10.29) | -- | -- | -- |
| Post (4mo) | 35.14 (10.38) | 0.86 | 35.11 (9.20) | 1.94 | 0.099 | −0.12 |
| Follow-up (6mo) | 34.83 (9.92) | 0.55 | 34.53 (9.55) | 1.36 | 0.162 | −0.08 |
| Abstract reasoning | ||||||
| Baseline | 32.17 (8.28) | -- | 33.53 (7.21) | -- | -- | -- |
| Post (4mo) | 38.45 (7.27) | 6.28 | 35.18 (5.33) | 1.65 | 0.019 | 0.54 |
| Follow-up (6mo) | 37.36 (5.27) | 5.19 | 34.69 (8.30) | 1.16 | 0.011 | 0.59 |
| Speeded mental flexibility | ||||||
| Baseline | 37.29 (5.30) | -- | 36.17 (6.39) | -- | -- | -- |
| Post (4mo) | 40.05 (4.47) | 2.76 | 36.40 (5.62) | 0.23 | 0.005 | 0.52 |
| Follow-up (6mo) | 39.96 (7.18) | 2.68 | 35.97 (6.41) | −0.20 | 0.001 | 0.45 |
| PANSS | ||||||
| Baseline | 87.83 (6.49) | -- | 71.84 (7.17) | -- | -- | -- |
| Post (4mo) | 80.31 (11.07) | −7.52 | 66.27 (11.64) | −5.57 | 0.089 | −0.25 |
| Follow-up (6mo) | 83.46 (10.78) | −4.37 | 67.52 (9.25) | −4.32 | 0.466 | −0.03 |
| SANS | ||||||
| Baseline | 39.26 (6.28) | -- | 22.03 (5.36) | -- | -- | -- |
| Post (4mo) | 38.85 (5.21) | −0.41 | 23.74 (7.79) | 1.71 | 0.078 | 0.32 |
| Follow-up (6mo) | 38.97 (7.73) | −0.29 | 22.23 (6.67) | 0.20 | 0.203 | 0.08 |
| Depression | ||||||
| Baseline | 10.27 (5.18) | -- | 11.31 (6.73) | -- | -- | -- |
| Post (4mo) | 10.16 (2.05) | −0.11 | 10.71 (5.45) | −0.60 | 0.197 | 0.07 |
| Follow-up (6mo) | 8.94 (4.29) | −1.33 | 10.42 (5.33) | −0.89 | 0.190 | 0.13 |
Note: PANSS-Positive and Negative Syndrome Scale; SANS-Scale for the Assessment of Negative Symptoms
ANCOVAs comparing the two groups at post treatment and 2-month follow-up (covarying for baseline PANSS and SANS) revealed a significant group difference on the SFS and WBI at post, F(2, 50)=7.41–8.04, p’s≤0.01, as well as follow-up, F(2, 50)=6.15–6.49, p’s <0.02, with the FORT group experiencing better social function and demonstrating better work readiness. A similar pattern emerged on secondary work outcome measures of work motivation and employment attitudes, as the FORT group reported more motivation for work and greater receptiveness to looking for employment in the community at post and follow-up (p’s<.05). Group differences favoring FORT at post and follow-up were also noted in self-esteem (p’s<0.02), working memory (p’s<0.05), processing speed (p’s<.0.001), speeded mental flexibility (p’s<0.005), and abstract reasoning (p’s<0.02). Differences from baseline to post to follow-up were not different between the groups in attention, verbal memory, symptoms, or depression (p’s>0.08) (Table 1).
In terms of effect sizes, results immediately following the intervention showed moderate to large between-group effects for FORT in social functioning, work readiness, self-esteem, executive ability, and particularly processing speed. A small effect at post was also noted in negative symptoms, but it disappeared at follow-up. Two months following the end the of the 16 week intervention, smaller but still moderate between-group effect size differences favoring FORT were still detected in social functioning, work readiness, self-esteem, and abstract reasoning (Table 1), thus showing a persistence of effects. In addition, of participants who identified obtaining a GED as their primary goal, 11 of 15 in FORT passed the exam (73%), compared to only 2 of 11 in traditional treatment planning (18%). Ordinary least squares regression analyses from the CEA showed that FORT had better average benefit-cost ratio from an agency perspective (14.67 vs 8.84; t(50)=7.78, p<0.01) even when considering FORT had patients who were more symptomatic at baseline (LSR=2.09, p=0.01).
Discussion
Compared to traditional treatment planning, the computerized clinical decision support system called FORT was associated with greater improvements in social functioning, executive ability, and domains related to work readiness. Importantly, a greater percentage of those enrolled in FORT met their primary goal of obtaining a GED. FORT was also more cost-effective than traditional treatment planning. This effect occurred in spite of individuals in the FORT group being more symptomatic—a factor usually associated with less improvement in outpatient treatment (Kurtz, 2015).
In this initial proof-of-concept pilot trial of FORT, we did not tease out the decisional informatics element from the treatment element. That is, we did not compare traditional treatment planning to FORT in the context of the same menu of treatment options. The traditional treatment planning comparison condition was a setting of convenience--an existing, community-based traditional day treatment program. Given the commingling of FORT with therapies that were somewhat different than those offered within the traditional day treatment program, at this point we can only speculate that the benefits seen from FORT were a combination of the psychotherapies used in FORT along with the decisional informatics treatment plan, and are unable to definitively conclude that they were solely due to the personalized nature of the rehabilitation program. The effect sizes reported were also based on change scores. Despite randomization, the participants in the FORT arm were doing more poorly at baseline in terms of symptoms. As such, it is possible that clinical improvements might reflect a greater opportunity to improve (regression towards the mean). However, greater SANS-measured negative schizophrenia symptomatology would be expected to hinder motivation and therapeutic engagement, resulting in worse outcome. The opposite was observed. Moreover, because treatment did not appreciably impact SANS scores in either study group by follow-up, it suggests that FORT benefits were independent of this baseline clinical difference. Another argument in support of the validity of FORT gains is the observations that clinical benefits were seen across multiple measures, the combination of which is unlikely to have occurred by chance. So while the simple randomization done at enrollment (a flip of the coin) unfortunately did not result in study groups with fully equivalent clinical symptomatology, our use of ANCOVA to statistical control for these differences lends confidence in the results. Future research should employ a stratified randomization procedure more likely to yield fully comparable groups. Additional limitations of the current trial include the use of different sets of treatment providers for the two conditions, along with lack of blinding for outcome assessors. Collectively, these limitations indicate the initial results of this field test are only meant to provide preliminary, broad-strokes information for the feasibility, potential efficacy and cost-effectiveness of a decisional informatics approach to personalized treatment. We are currently in the process of running a larger, more rigorously-controlled replication study that will compare FORT to traditional treatment planning in the same therapeutic setting, with the same menu of treatment options, and a more in-depth methodology that studies how the treatment team interacts with computer-based decisional programs in patient care.
Clinical decision support systems that collaborate with human decision makers to personalize psychiatric rehabilitation and address critical decisions may have a role in improving treatment effectiveness and efficiency. If such is the case, it will also be important to address potential barriers to making available FORT-based modifications to treatment, such as state mandates as to content and structure of treatment or perceptions of computer-generated treatment algorithms by rehabilitation professionals. The goal of personalizing psychiatric rehabilitation through collaboration with intelligent computer-based decisional tools is to offer the treatment team access to a continually updating clinical database that tracks patient status, the use of which may lead to better outcomes. In the near future, we expect the field will see more of these prototype systems that collaborate with human decision makers to personalize psychiatric rehabilitation and optimize outcomes.
Conclusion
To our knowledge, this is the first report on the use of a clinical decision support system to inform behavioral treatment planning for serious mental illness by personalizing the timing, content, and application of interventions.
Acknowledgments
We would like to thank Susan Essock, Ph.D., for her support and guidance. We would also like to thank Marcela Horvitz-Lennon, M.D., M.P.H., for her detailed comments and assistance with the manuscript. Finally, we would like to acknowledge the project coordinators, Jackie Helcer, M.S., and Carol Pauls, M.A., for their tireless efforts in managing the project.
Source of Funding
This study was funded in part by NIMH K23MH086755 to Dr. Choi.
Footnotes
Conflicts of Interest
Conflicts of interest: none declared.
References
- Andreasen NC. Scale for the Assessment of Negative Symptoms (SANS) Brit J Psychiat. 1989;155(7):53–58. [PubMed] [Google Scholar]
- Andrew DM, Paterson DG, Longstaff HP. Minnesota clerical test. Psychological Corporation, Harcourt Brace & Company; 1979. [Google Scholar]
- Bell MD, Lysaker PH. Clinical benefits of paid work activity in schizophrenia: 1-year followup. Schizophr Bull. 1997;23:317–328. doi: 10.1093/schbul/23.2.317. [DOI] [PubMed] [Google Scholar]
- Birchwood M, Smith JO, Cochrane R, Wetton S, Copestake SONJ. The Social Functioning Scale. The development and validation of a new scale of social adjustment for use in family intervention programmes with schizophrenic patients. Brit J Psychiat. 1990;157(6):853–859. doi: 10.1192/bjp.157.6.853. [DOI] [PubMed] [Google Scholar]
- Bowie CR, McGurk SR, Mausbach B, Patterson TL, Harvey PD. Combined cognitive remediation and functional skills training for schizophrenia: effects on cognition, functional competence, and real-world behavior. Am J Psychiat. 2012;169(7):710–718. doi: 10.1176/appi.ajp.2012.11091337. [DOI] [PubMed] [Google Scholar]
- Brandt J, Benedict RH. Hopkins verbal learning test, revised: professional manual. Psychological Assessment Resources; 2001. [Google Scholar]
- Bryson G, Bell MD, Lysaker P, Zito W. The Work Behavior Inventory: A scale for the assessment of work behavior for people with severe mental illness. Psychiatr Rehabil J. 1997;20(4):47–55. [Google Scholar]
- Choi J, Corcoran CM, Fiszdon JM, Stevens M, Javitt DC, Haber LC, Dewberry MJ, Pearlson GD. Pupillometer-based neurofeedback cognitive training to improve processing speed and social functioning in psychosis. Psychiatr Rehabil J. 2016 doi: 10.1037/prj0000217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook J, Blyler C, Burke-Miller J, McFarlane W, Leff H, Mueser K, Donegan K. Effectiveness of supported employment for individuals with schizophrenia: Results of a multi-site, randomized trial. Clin Schizophr Relat Psychoses. 2008;2(1):37–46. [Google Scholar]
- Dixon LB, Dickerson F, Bellack AS, et al. The 2009 schizophrenia PORT psychosocial treatment recommendations and summary statements. Schizophr Bull. 2010;36:48–70. doi: 10.1093/schbul/sbp115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essock SM, Hogan MF. Looking into the health reform crystal ball: Seeing more constructive, less expensive management scenarios. Am J Psychiat. 2011;168:449–51. doi: 10.1176/appi.ajp.2011.11020205. [DOI] [PubMed] [Google Scholar]
- Fiszdon JM, Roberts DL, Penn DL, Choi KH, Tek C, Choi J, Bell MD. Understanding Social Situations (USS): A Proof-of-Concept Social-Cognitive Intervention Targeting Theory of Mind and Attributional Bias in Individuals With Psychosis. Psychiatr Rehabil J. 2016 doi: 10.1037/prj0000190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery & Psychiatry. 1960;23(1):56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heaton RK. Wisconsin card sorting test: computer version 2. Odessa: Psychological Assessment Resources; 1993. [Google Scholar]
- Kay SR, Flszbein A, Opfer LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Kurtz MM. Schizophrenia and Its Treatment: Where is the Progress? Oxford University Press; New York: 2015. [Google Scholar]
- Liu NH, Choi K-H, Reddy F, et al. Heterogeneity and the longitudinal recovery of functioning during inpatient psychiatric rehabilitation for treatment-refractory severe mental illness. Am J Psychiatr Rehabil. 2011;14:55–75. [Google Scholar]
- Lysaker PH, Davis LW, Bryson GJ, Bell MD. Effects of cognitive behavioral therapy on work outcomes in vocational rehabilitation for participants with schizophrenia spectrum disorders. Schizophr Res. 2009;107:186–191. doi: 10.1016/j.schres.2008.10.018. [DOI] [PubMed] [Google Scholar]
- McGurk SR, Schiano D, Mueser KT, et al. Implementation of the thinking skills for work program in a psychosocial clubhouse. Psychiatr Rehabil J. 2010;33:190–9. doi: 10.2975/33.3.2010.190.199. [DOI] [PubMed] [Google Scholar]
- Pickett SA, Cook JA, Carey MA. Report to the Steering Committee, Employment Intervention Demonstration Program (EIDP) University of Illinois; Chicago: 1997. Creating and testing a work motivation scale for a multi-site vocational study. [Google Scholar]
- Priebe S, Warner R, Hubschmid T, Eckle I. Employment, attitudes toward work, and quality of life among people with schizophrenia in three countries. Schizophr Bull. 1998;24:469–477. doi: 10.1093/oxfordjournals.schbul.a033341. [DOI] [PubMed] [Google Scholar]
- Twamley EW, Vella L, Burton CZ, et al. The efficacy of supported employment for middle-aged and older people with schizophrenia. Schizophr Res. 2010;135:100–104. doi: 10.1016/j.schres.2011.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddy LF, Horan WP, Jahshan C, Green MF. Cognitive remediation for schizophrenia: a review of recent findings. Curr Treat Options Psychiatry. 2014;1(2):121–133. [Google Scholar]
- Reitan RM. Trail Making Test: Manual for administration and scoring. Reitan Neuropsychology Laboratory; 1992. [Google Scholar]
- Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton Press; 1965. [Google Scholar]
- Spaulding W, Deogun J. A pathway to personalization of integrated treatment: informatics and decision science in psychiatric rehabilitation. Schizophr Bull. 2011;37:S129–S37. doi: 10.1093/schbul/sbr080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsang HW, Leung AY, Chung RC, Bell M, Cheung WM. Review on vocational predictors: a systematic review of predictors of vocational outcomes among individuals with schizophrenia: an update since 1998. Aust N Z J Psychiatry. 2010;44(6):495–504. doi: 10.3109/00048671003785716. [DOI] [PubMed] [Google Scholar]
- Wechsler D. WAIS-III: Administration and scoring manual: Wechsler adult intelligence scale. Psychological Corporation; 1997. [Google Scholar]