Abstract
A cluster-randomized trial evaluating the effectiveness of chlorhexidine glucotiate-impregnated wipes against skin and soft tissue infections (SSTIs) and colonization with methicillin-resistant Staphylococcus aureas (MRSA) was conducted among military recruits attending Officer Candidate School at Marine Corps Base Quantico, Virginia. Participants were instructed to use the wipes thrice weekly and were monitored daily for SSTI. Surveys assessed frequency of wipe use as well as knowledge and attitudes regarding MRSA SSTI. Use of chlorhexidine gluconate-impregnated wipes failed to prevent SSTI; however, study adherence was moderate. Adherence with the study regimen (defined as use of ≥50% of the wipes) was 65% at week 2 and declined to 49% by week 6. Adherence was ~59% in the first two classes and declined in later classes. One-third felt that use of the wipes was disruptive. Participants were knowledgeable about MRSA SSTI prevention measures. However, only 53% agreed that MRSA commonly causes skin infections in military training facilities. Understanding adherence and its determinants is needed to optimize prevention strategies that require self-administration. Future efforts should address barriers to adherence with prevention strategies in recruit training settings.
INTRODUCTION
Skin and soft tissue infections (SSTIs), particularly those because of methicillin-resistant Staphylococcus aureus (MRSA), are a recognized health threat among military trainees.1 MRSA colonization of skin and mucous membranes plays a role in SSTI pathogenesis; so, decolonization methods (e.g., intranasal application of mupirocin, use of chlorhexidine-based cleansers, etc.) have been incorporated into SSTI prevention strategies among military trainees and other high-risk groups.2,3 However, data on the effectiveness of decolonization are limited.
A cluster-randomized controlled trial among Officer Candidate School (OCS) recruits at Marine Corps Base Quantico, Virginia, assessed the effectiveness of chlorhexidine gluconate (CHG)-impregnated body wipes in preventing SSTI and MRSA colonization.4 Use of the wipes, self-applied thrice weekly, did not reduce rates of SSTI. Furthermore, MRSA colonization rates increased in both study groups, albeit to a lesser extent in groups randomized to receive CHG. Although the trial outcome has brought into question the effectiveness of CHG in a community setting, a major limitation of the study was moderate adherence with the study intervention. Self-reported rates of adherence (defined as use of ≥50% of the wipes) were 65% in week 2 of the study and declined to 49% by week 6.
Adherence with personal protective and hygiene measures among military populations has been studied for other infectious diseases, including malaria chemoprophylaxis and hand washing to prevent acute respiratory infection.5–8 Understanding adherence and its determinants is important in the design and implementation of disease prevention strategies. Herein, we evaluate recruit adherence with a self-administered, hygiene-based intervention in a cluster-randomized controlled trial to prevent SSTI and MRSA colonization. Knowledge gained here may ultimately improve the quality of health communication strategies in this and other high-risk populations.
METHODS
Description of the Study Setting and Population
Details of the study design and population have previously been reported.4 In brief, from May to November 2007, a cluster-randomized controlled trial was conducted among OCS recruits at Marine Corps Base Quantico to evaluate the effectiveness of thrice weekly application of CHG in preventing SSTI and MRSA colonization. Recruits were assigned to platoons of 40 to 60 individuals upon arrival and had minimal interaction with members of other platoons during training (either a 6- or 10-week class). Platoons had dedicated training instructors and corpsmen that remained with the same platoon for the duration of training.
Description of the Study Procedures
On the first day of training, study investigators briefed recruits on the study purpose and procedures, its risk and benefits, as well as the voluntary nature of participation in the study. In addition, the study investigators briefed recruits on the recognition and prevention of MRSA SSTI. Consenting recruits were randomized by platoon to receive either 2% CHG wipes9 or Comfort Bath wipes10 in similar packaging. Packets were dispensed thrice weekly by platoon corpsmen in the morning before personal hygiene time. The thrice-weekly regimen was selected based on clinical evidence that CHG has residual antimicrobial activity up to 24 hours11 and because it was felt the regimen could be incorporated into a highly structured environment with minimal disruption of activities. Participants were instructed to use the wipes on their entire body after showering, avoiding application to their face, genitalia, and any areas with open wounds. Instruction on proper application of the wipes was reinforced at biweekly follow-up visits. As part of standard OCS procedure, platoon corpsmen performed daily checks on recruits for SSTI and referred possible cases to the OCS clinic for evaluation.
Participants completed an enrollment survey capturing demographic and medical information, including history of SSTI/”staph” infection and recent antibiotic use before OCS. Biweekly follow-up surveys captured recent antibiotic use, frequency of showers, frequency of use of body wipes, and changes in skin condition related to wipe use. Adherence with wipes in the prior 2 weeks was categorized as (1) all the packets, (2) half or more of the packets, (3) less than half of the packets, or (4) none of the packets. The survey captured the areas of the body (neck, chest, arms, hands, legs, groin, and armpits) on which the wipes were applied as well as any side effects (irritation, burning, itching, redness, or rash) from wipe use. The final survey, completed at week 6, assessed participant knowledge and attitudes regarding MRSA, SSTI, and wipe use. Survey items included “Using the wipes was disruptive to my day” and “I did not like using the wipes.” Responses were recorded on a 5-point Likert scale ranging from “strongly agree” to “strongly disagree.”
Participating recruits provided written informed consent. This study was approved by the Uniformed Services University Institutional Review Board (Protocol No. IDCRP-001).
Analysis
Frequencies were computed for survey data, including reported wipe use at 2, 4 and 6 weeks and questions at study completion. To evaluate factors associated with regimen adherence, we compared the distribution of reported wipe use at 6 weeks by age, gender, race, training class, medical history, and participant knowledge and attitudes. Significance was assessed by χ2 tests. Graphical displays of study completion questions are presented with the middle category “neutral” (i.e., neither agree nor disagree) removed. SAS software version 9.2 (SAS Institute, Cary, North Carolina) was used for all analyses. Statistical significance was set at p < 0.05, and two-tailed testing was used for all analysis.
RESULTS
Of the 2,572 OCS recruits, 1,562 (60.7%) were enrolled; 781 recruits were assigned to platoons randomized to CHG and 781 were assigned to platoons randomized to Comfort Bath (Fig. 1). Participants were young (mean 22.4 years, SD ± 2.8), predominantly male (95.0%), and Caucasian (83.9%). Of the 1,562 recruits enrolled in the trial, 1,355 (86.7%), 1,189 (76.1%), and 1,035 (66.3%) completed the 2-, 4- and 6-week follow-up surveys, respectively. Of those who withdrew from the study, approximately one-half withdrew from OCS altogether and the remainder withdrew from the study only. Withdrawal rates did not differ significantly by age or race, or by study group but were higher among females than males (65.1% vs. 30.5%).
FIGURE 1.
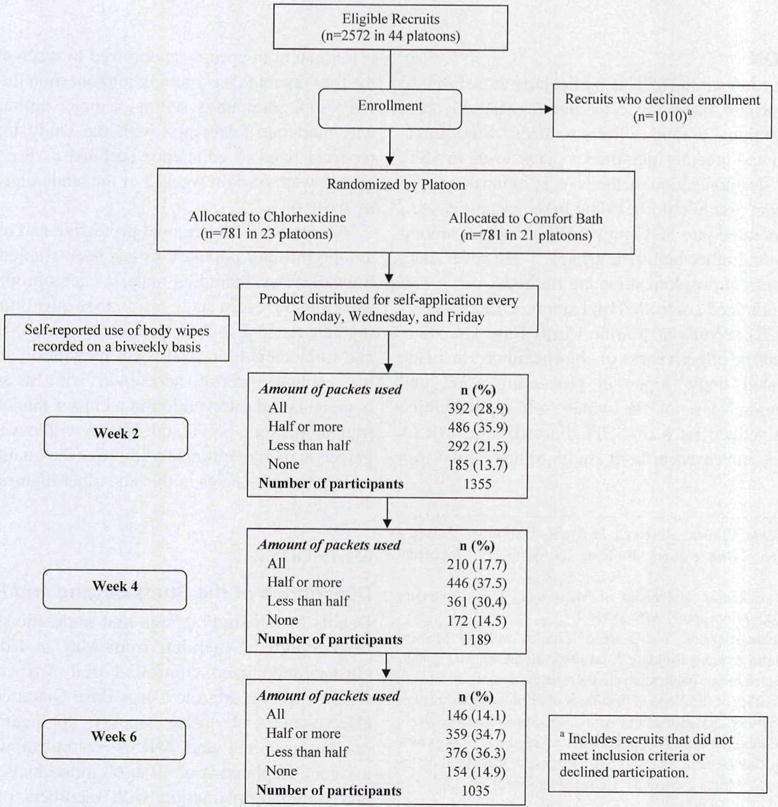
Participation and progress of OCS platoons and recruits in a cluster-randomized controlled trial to prevent SSTIs.
Self-reported wipe use was similar between study groups, therefore results were combined. At week 2, frequency of use in the previous 2 week period was as follows: 28.9% used all the packets, 35.9% used half or more of the packets, 21.5% used less than half of the packets, and 13.7% did not use any of the packets (Fig. 1). Adherence decreased over the course of the study. In particular, the percentage reporting use of all the packets decreased from 28.9% at week 2 to 14.1% at week 6. There was a corresponding increase in the percent using less than half of the packets. The percent that reported using half or more of the packets remained fairly constant (37.5% at week 4 and 34.7% at week 6). Similarly, the percent of participants that reported no use remained constant over the course of the study (range 13.7%–14.9%). Figure 2 presents rates of adherence at weeks 4 and 6, stratified by rates of adherence at week 2. Participants that reported use of all the wipes at week 2 continued to use half or more of the wipes consistently for the study duration (86.0% at week 4 and 77.0% at week 6). Those that used half or more of the wipes at week 2 showed the most dramatic shift in use to less than half of the wipes at week 4 (40.6%) and week 6 (54.1%). A small percentage of participants that reported using less than half or none of the wipes at week 2 were compliant (use of ≥50% of the wipes) at week 4 (30.1% and 28.5%, respectively) and week 6 (28.5% and 22.3%, respectively). At 6 weeks, participants reported using the wipes most frequently on the arms and legs (80%–82%), followed by the neck, chest, hands, and armpits (71%–76%), and then the groin (54%). This pattern was similar at other biweekly assessments.
FIGURE 2.
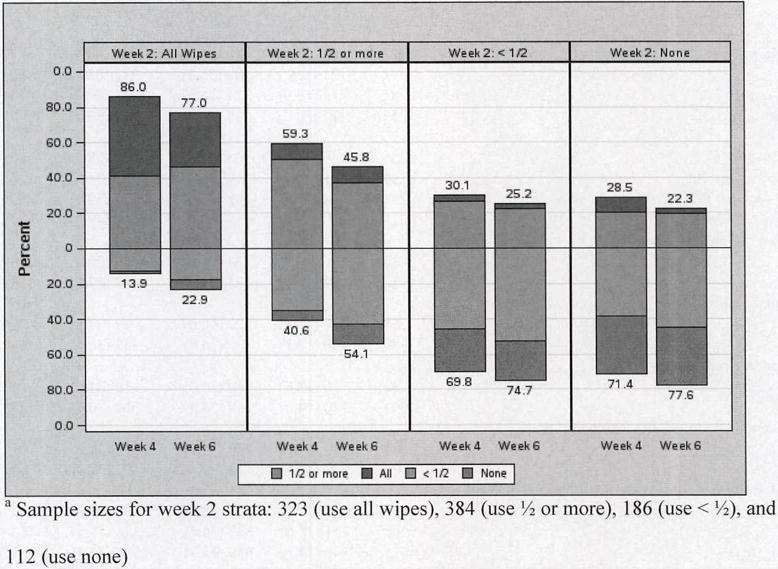
Reported use of body wipes at weeks 4 and 6, stratified by reported adherence at week 2.
Factors associated with reported adherence were evaluated (Table I). Female participants had a higher level of adherence than their male counterparts (64.7% vs. 47.9%, respectively; p < 0.01). Frequency of use did not vary by age and race. Rates of adherence were highest among the first and second training classes and declined in subsequent classes (p < 0.01). Having had a previous SSTI/ “staph” infection did not impact adherence. Similarly, no difference in adherence was observed among participants who had a history of recurrent skin infections before training. A small percentage (3.1%) of participants previously worked in a hospital or clinic; adherence among these individuals did not differ from participants without this experience. Adherence did not differ between the ~6% that reported changes (i.e., irritation or burning, itching. redness, or rash) in skin condition compared to those that did not; this was true both overall and in the subgroup of participants in CHG-randomized groups.
TABLE I.
Factors Associated With Reported Use of Body Wipes at Week 6
| Number of Participants | All the Packets | Half or More of the Packets | Less Than Half of the Packets | None of the Packets | p-Valuea | |
|---|---|---|---|---|---|---|
| Age | 0.39 | |||||
| <20 | 106 | 14 (13.2) | 46 (43.4) | 35 (33.0) | 11 (10.4) | |
| 20–24 | 720 | 105 (14.6) | 243 (33.8) | 257 (35.7) | 115 (16.0) | |
| 25+ | 209 | 27 (12.9) | 70 (33.5) | 84 (40.2) | 28 (13.4) | |
| Gender | <0.01 | |||||
| Male | 984 | 135 (13.7) | 337 (34.2) | 361 (36.7) | 151 (15.3) | |
| Female | 51 | 11 (21.6) | 22 (43.1) | 15 (29.4) | 3 (5.9) | |
| Race | 0.27 | |||||
| African-American | 27 | 1 (3.7) | 10 (37.0) | 12 (44.4) | 4 (14.8) | |
| Caucasian | 871 | 121 (13.9) | 309 (35.5) | 311 (35.7) | 130 (14.9) | |
| Hispanic | 82 | 13 (15.9) | 21 (25.6) | 33 (40.2) | 15 (18.3) | |
| Other/Unknown | 55 | 11 (20.0) | 19 (34.5) | 20 (36.4) | 5 (9.1) | |
| Training Class | <0.01 | |||||
| Class 1 (May 26–July 6) | 256 | 46 (18.0) | 105 (41.0) | 73 (28.5) | 32 (12.5) | |
| Class 2 (June 2–August 10) | 259 | 37 (14.3) | 114 (44.0) | 89 (34.4) | 19 (7.3) | |
| Class 3 (July 7–August 17) | 297 | 34 (11.4) | 83 (27.9) | 117 (39.4) | 63 (21.2) | |
| Class 4 (September 2–November 4) | 223 | 29 (13.0) | 57 (25.6) | 97 (43.5) | 40 (17.9) | |
| Baseline—Previous “staph” Infection | 0.63 | |||||
| Yes | 83 | 9 (10.8) | 34 (41.0) | 24 (28.9) | 16 (19.3) | |
| No | 952 | 137 (14.4) | .325 (34.1) | 352 (37.0) | 138 (14.5) | |
| Baseline—Repeated Skin Infection | 0.95 | |||||
| Yes | 55 | 6 (10.9) | 22 (40.0) | 19 (34.5) | 8 (14.5) | |
| No | 980 | 140 (14.3) | 337 (34.4) | 357 (36.4) | 146 (14.9) | |
| Baseline—Worked in Hospital | 0.90 | |||||
| Yes | 32 | 6 (18.8) | 10 (31.3) | 10 (31.3) | 6 (18.8) | |
| No | 1,003 | 140 (14.0) | 349 (34.8) | 366 (36.5) | 148 (14.8) | |
| During Study—Wounds From Injuries Through 6 Weeks | 0.93 | |||||
| Yes | 835 | 119 (14.3) | 288 (34.5) | 302 (36.2) | 126 (15.1) | |
| No | 200 | 27 (13.5) | 71 (35.5) | 74 (37.0) | 28 (14.0) | |
| During Study—Skin Burning, Itching, or Rash Through 6 Weeks | 0.98 | |||||
| Yes | 67 | 5 (7.5) | 26 (38.8) | 32 (47.8) | 4 (6.0) | |
| No | 968 | 141 (14.6) | 333 (34.4) | 344 (35.5) | 150 (15.5) | |
| Number of Participants | 1,035 | 146 (14.1) | 359 (34.7) | 376 (36.3) | 154 (14.9) |
Number and percent are shown as N (%).
p-Values are χ2 tests for trend.
Survey questions assessed participants’ attitudes regarding wipe use; 34.5% felt using the wipes was disruptive to their day, 33% did not, and 32.5% were neutral. In response to the statement “I did not like using the wipes,” 22.8% agreed, 38.7% disagreed, and 38.5% were neutral. These responses were strongly associated with adherence. Only a small percentage of those that used all the wipes felt that they were disruptive (13.6%) and disliked using them (6.1%), in contrast to those that did not use any of the wipes (disruptive: 54.3%, dislike: 42.3%) (Fig. 3). Of note, although 61.6% of the participants either did not like using the wipes or were indifferent, 68.6% thought that future recruits should use wipes to prevent skin infections.
FIGURE 3.
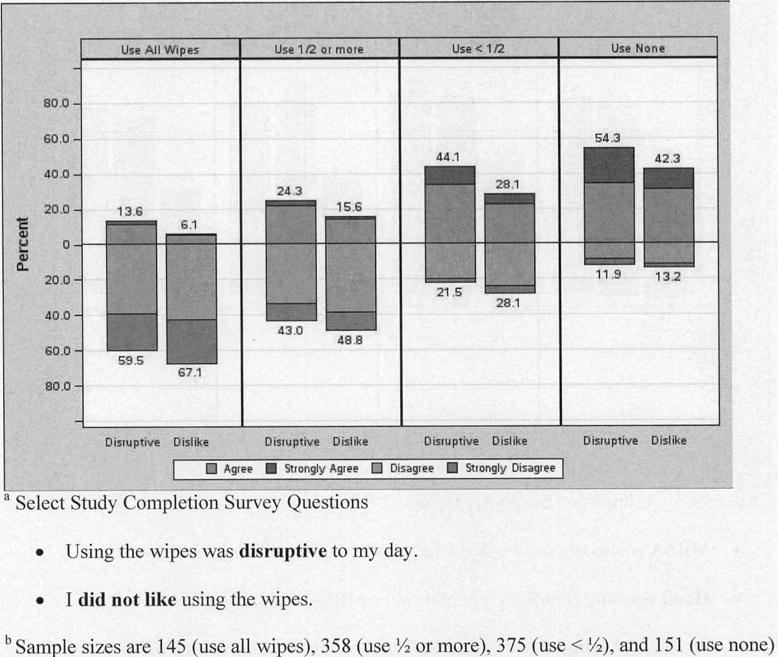
Attitudes of participants regarding use of body wipes, stratified by reported rates of adherence at week 6a.
When assessing level of knowledge of MRSA SSTI, 52.7% of participants agreed (2.3% disagreed and 45.0% were neutral) that the organism commonly causes SSTI in military training facilities. Overall, participants were very knowledgeable about appropriate hygiene measures to prevent skin infections. Eighty-five percent agreed (0.6% disagreed and 13.9% were neutral) that hand washing was important in preventing MRSA skin infections. Similarly, 86.9% of participants also agreed (0.5% disagreed and 12.6% were neutral) that not sharing of personal items (e.g., towels) was important in preventing MRSA skin infections. Although levels of knowledge were high, only 33.5% of participants agreed that skin infections are a big problem in the military. Unlike the questions on attitudes toward product use, participants’ level of knowledge was similar by level of adherence (Fig. 4).
FIGURE 4.
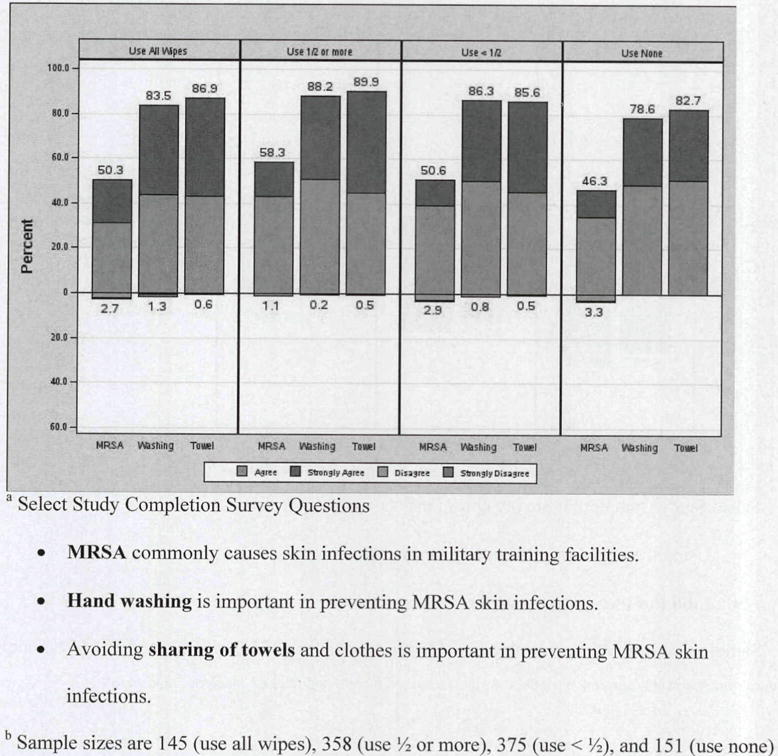
Knowledge of participants regarding MRSA .skin infections, stratified by reported rates of adherence at week 6a.
DISCUSSION
In a cluster-randomized trial evaluating the effectiveness of CHG against SSTI, rates of infection did not differ between CHG and control groups.4 Rates of MRSA colonization increased in both groups, although acquisition was significantly lower in CHG-randomized groups. Interpretation of trial outcomes must take into account participant adherence with the study regimen. Self-reported adherence was 65% after 2 weeks, and 49% after 6 weeks. Only 14% of participants reported use of all the wipes. Selection of the regimen was based on the prolonged residual antiseptic effect of CHG on the skin11 as well as taking into consideration the rigorous training schedule. It is possible that thrice weekly application may not have been sufficient to reduce MRSA colonization and SSTI. Further study is needed to determine the optimal use of CHG in the community setting.
Adherence with wipe use varied over the duration of the trial; adherence was significantly higher in the training classes beginning in May and June compared to the classes beginning in July and September. With regard to participants’ attitudes on wipe use, one-third felt that use of the product was disruptive and ~20% did not like using the wipes. Although the majority were knowledgeable about MRSA SSTI prevention measures (i.e., hand washing, not sharing personal items, etc.), nearly half were neutral on whether MRSA commonly causes skin infections in military training facilities.
Full adherence with the study regimen (reported use of 100% of the wipes) was lower than levels of adherence with command-directed prevention measures, such as hand washing for prevention of respiratory and gastrointestinal illness (49%)6 and use of repellent (45%) and chemoprophylaxis for malaria (55%).7,12 This could be due in part to the investigational nature of our study, whereas the others assessed adherence with personal protective and hygiene measures that are known to be effective in preventing disease. Our findings highlight the numerous challenges in conducting prevention trials in a military setting and underscore the difficulty in communicating disease risk and ensuring adherence with personal protective measures in military populations.
We examined possible barriers to adherence. It is likely that personal knowledge and attitudes regarding SSTI, MRSA, and/or ease of use of the wipes were the primary adherence determinants. The investigational nature of the study may have also influenced use; however, this was not assessed on follow-up surveys. When surveyed, a significant percentage of participants not only felt that wipe use was disruptive, they also disliked using the wipes. Some felt that the wipes were sticky and left a residue on their skin, whereas others reported skin irritation, itching, redness, or rash. Participants demonstrated high levels of knowledge about means to prevent MRSA SSTI, but nearly half were neutral on whether MRSA was a common cause of skin infections in military training facilities.
Although the survey did not permit an exhaustive examination of participants’ perceived threat and susceptibility to MRSA SSTI, the findings suggest it was low. Because awareness of one’s own risk for disease is a critical component of adopting and maintaining positive health behaviors,13,14 the focus of SSTI prevention strategies must be on educating new recruits of their increased risk for MRSA infection. This message might be best delivered via various means, such as in-person briefings and posting of information in common areas. Mott et al reported implementation of a hand hygiene intervention in soldiers. In addition to increased access to hand sanitizer, the program included hygiene education, posters, and weekly reminders to drill sergeants and was effective in reducing lost duty time to illnesses likely caused by communicable diseases.15 In our study, investigators briefed recruits on recognition and prevention of MRSA SSTI, however no other educational tools were employed. It is possible that supplemental materials, such as educational briefs, posters, pocket cards, email and text reminders, may have improved adherence levels in our study.
It is likely that the additional requirements of trial participation, including biweekly surveys and collection of swabs for surveillance purposes, may have interfered with concurrent recruit responsibilities, and that adherence may have been negatively affected as a result. When informally queried, a number of participants that voluntarily withdrew from the study cited lack of time as a reason for discontinuation. The difficulty of maintaining disease prevention strategies in military training environments has been described elsewhere.6 In a study of respiratory illness prevention among military trainees, approximately half of the survey respondents reported challenges with hand washing during training cycles. The most common reason was limited time. Further evaluation of barriers to adherence is needed. Convening focus groups of trial participants, before and at the conclusion of the trial, may be useful in this regard.
Adherence levels may have been influenced by instructors, platoon corpsmen, and fellow recruits as not all recruits enrolled in the study. Although command leadership was supportive of the trial, it is possible that platoon level instructors may have felt that study participation interfered with training activities, thus limiting their positive reinforcement of continued recruit participation in the trial. It is unknown whether the possibility of waning support for the trial activities from platoon leadership over the course of the study accounted for the lower levels of adherence observed in later training classes. Platoon corpsmen, responsible for the distribution of the study product on Monday, Wednesday, and Friday mornings during recruits’ medical assessment, were initially trained by study personnel on proper application of the wipes. If, however, time to answer questions about the study or distribute the product hindered or delayed their medical assessment, again, the continued positive reinforcement of recruit participation may have been compromised.
There are limitations to the current study. Adherence levels were assessed by self-administered biweekly questionnaires. Inaccurate recall of the quantity of wipes used may have led to misclassification of participants’ level of adherence. Unused packets were collected from platoon corpsmen; however, this only provided reassurance that the packets were dispensed, rather than used properly, if at all. We did not assess reasons why participants felt wipe use was disruptive or why participants disliked using the wipes. Finally, although the questionnaires were self-administered, it is possible that respondents overestimated their use of the wipes, tending towards survey responses they perceived to be acceptable to the study investigators.
For investigational studies that assess the effectiveness of self-administered personal protective measures, more direct measures of participant adherence need to be applied. Direct observation of product use, while time- and resource-intensive and more likely to interfere with routine training activities, would ensure a more accurate measure of participant adherence and more precise estimates of product effectiveness. If direct observation is not feasible, self-administered questionnaires should be supplemented with quantitative indicators of adherence, such as numbers of used or unused products collected at regular intervals. For trials utilizing self-administered interventions over an extended duration, measures of participant adherence should be collected and analyzed in real time so that reinforcement of study procedures can be targeted appropriately and delivered immediately.
Findings from this study of adherence, conducted in the context of a randomized trial for the prevention of SSTI among military recruits, underscore the importance of a multifaceted approach to disease prevention and health promotion in military settings.8 Assessing personal knowledge and attitudes regarding risk and severity of disease is critical in the development of effective health communication strategies targeted to individuals. In addition, the influence of military leadership in communicating disease risk and advocating disease prevention methods among personnel should be evaluated. Prevention strategies in military settings must also consider the ease or difficulty of execution such that minimal deviation from other activities is required. This is of paramount importance for military populations where protective measures are often self-administered, require sustained use, and are conducted in the face of other rigorous and time-consuming tasks central to military operations.
Acknowledgments
This work (IDCRP-001) was supported by the Infectious Disease Clinical Research Program (IDCRP), a Department of Defense (DoD) program executed through the Uniformed Services University. This project has been funded in whole, or in part, with federal funds from the National Institute of Allergy and Infectious Diseases, National Institutes of Health, under Inter-Agency Agreement Yl-Al-5072.
Footnotes
The views expressed in this publication are those of the authors and do not reflect the official policies of the National Institutes of Health. Department of Health and Human Services, Department of Army, Department of Defense, or U.S. Government. Mention of trade names, commercial products, or organizations does not imply endorsement by the U.S. Government. Reviewed by the Walter Reed National Military Medical Center Public Affairs Office in December 2011.
References
- 1.Army Medical Surveillance Activity. Cellulitis and abscess, active components, US armed forces, 2002–2005. MSMR. 2006;12(4):2–9. [Google Scholar]
- 2.Ellis MW, Griffith ME, Dooley DP, et al. Targeted intranasal mupirocin to prevent colonization and infection by community-associated methicillin-resistant Staphylococcus aureus strains in soldiers: a cluster randomized controlled trial. Antimicrob Agents Chemother. 2007;51(10):3591–8. doi: 10.1128/AAC.01086-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wootton SH, Arnold K, Hill HA, et al. Intervention to reduce the incidence of methicillin-resistant Staphylococcus aureus skin infections in a correctional facility in Georgia. Infect Control Hosp Epidemiol. 2004;25(5):402–7. doi: 10.1086/502413. [DOI] [PubMed] [Google Scholar]
- 4.Whitman TJ, Herlihy RK. Chlorhexidine-impregnated cloths to prevent skin and soft-tissue infection in Marine recruits: a cluster-randomized, double-blind, controlled effectiveness trial. Infect Control Hosp Epidemiol. 2010;31(12):1207–15. doi: 10.1086/657136. [DOI] [PubMed] [Google Scholar]
- 5.Gambel JM, Brundage JF, Kuschner RA, Kelley PW. Deployed US Anny soldiers’ knowledge and use of personal protection measures to prevent arthropod-related casualties. J Travel Med. 1998;5(4):217–20. doi: 10.1111/j.1708-8305.1998.tb00511.x. [DOI] [PubMed] [Google Scholar]
- 6.Ryan MA, Christian RS, Wohlrabe J. Handwashing and respiratory illness among young adults in military training. Am J Prev Med. 2001;21(2):79–83. doi: 10.1016/s0749-3797(01)00323-3. [DOI] [PubMed] [Google Scholar]
- 7.Kotwal RS, Wenzel RB, Sterling RA, Porter WD, Jordan NN, Petruccelli BP. An outbreak of malaria in US Army Rangers returning from Afghanistan. JAMA. 2005;293(2):212–6. doi: 10.1001/jama.293.2.212. [DOI] [PubMed] [Google Scholar]
- 8.Mott PJ, Sisk BW, Arbogast JW, Femizzano-Yaussy C, Bondi CA, Sheehan JJ. Alcohol-based instant hand sanitizer use in military settings; a prospective cohort study of Army basic trainees. Mil Med. 2007;172(11):1170–6. doi: 10.7205/milmed.172.11.1170. [DOI] [PubMed] [Google Scholar]
- 9.HALO 2% Chlorhexidine Gluconate Cloth [package insert] Cary, IL: Sage Products Inc.; Available at http://www.sageproducts.com/lit/21077B_CHG_cloths_product_info_sheet.pdf; accessed June 21, 2012. [Google Scholar]
- 10.Comfort Bath [package insert] Cary, IL: Sage Products Inc.; Available at http://www.sageprodticts.com/lit/20258D_Comfort_Bath_product_information_sheet.pdf; accessed June 21, 2012. [Google Scholar]
- 11.Hibbard JS. Analyses comparing the antimicrobial activity and safety of current antiseptic agents: a review. J Infus Nurs. 2005;28(3):194–207. doi: 10.1097/00129804-200505000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Whitman TJ, Coyne PE, Magill AJ, et al. An outbreak of Plasmodium falciparum malaria in U.S. Marines deployed to Liberia. Am J Trop Med Hyg. 2010;83(2):258–65. doi: 10.4269/ajtmh.2010.09-0774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosenstock IM. Why people use health services. Milbank Mem Fund Q. 1966;44(3 Suppl):94–127. [PubMed] [Google Scholar]
- 14.Wong TY, Seet B. A behavioral analysis of eye protection use by soldiers. Mil Med. 1997;162(11):744–8. [PubMed] [Google Scholar]
- 15.Mott P, Sisk B, Arbogast JW, Ferrazzano-Yaussy C, Sheehan J. Reducing Lost Training Time in IET: A Comprehensive Hand Hygiene Approach at Fort Sill, OK. UCLA Faculty Center; 2005. (Christopher S Foote Memorial Poster Session). Available at http://www.chem.ucla.edu/research/org/FOOTE-MEMORIAL/Poster_Titles.html: accessed March 20. 2012. [Google Scholar]


