Abstract
Current evidence pertaining to the effectiveness of flossing and caries prevention is potentially being misinterpreted by health oversight bodies, which may have significant implications for current and future public flossing guidelines. We identify and discuss several methodological deficiencies including the lack of validated measures of flossing skill, over-reliance on self-reported flossing behavior and the lack of current guidelines on how to interpret and apply evidence-based findings to specific clinical scenarios that are present in the studies of flossing effectiveness included in the Cochran Review. As such, we argue that it is premature for health oversight bodies to conclude that flossing is ineffective in the prevention of dental caries. Our research group, which is funded by the National Institutes of Health, is developing valid and reliable provider-observed measure of tooth brushing and flossing skill that may help promote higher quality flossing evidence in the future.
Keywords: flossing, oral hygiene, interpreting evidence, self-report, behavior change
Introduction
Recently publicized meta-analytic data-analyses/Cochran Reviews 1, 2 have been used to advance the argument that flossing (aka cleaning well between the teeth) does not reduce the risk of developing dental caries and periodontal diseases (Saint Louis, NYT, Aug 2, 2016). Has the interpretation of these data been appropriate in the media? Will simplistic sound bites lead the lay public then conclude that cleaning between the teeth is unnecessary? With regard to the effectiveness of flossing, there are several points to consider. Importantly, it should be noted that none of the studies used in either Cochrane Review examined dental caries as an outcome variable. Also, one Cochrane Review (Sambunjak et al, 2012) examined 12 studies and the other (Poklepovic et al, 2013) was based on only 7 studies—this is not a reflection on the Cochran Review authors, but on the limitations of currently available evidence 1, 2. In fact, the work (Sambunjak et al, 2012) that was referenced by the NYT article(s), actually stated: “The trials [used in their review] were of poor quality and conclusions must be viewed as unreliable.”1 Despite this disclaimer, the decision was made to remove the recommendation of flossing (to promote oral health—within the context of other oral health recommendations) from the Dietary Guidelines for Americans, 2015–2020 [https://health.gov/dietaryguidelines/2015/guidelines/]. We ask: might such an interpretation of the currently available evidence on flossing be premature?
A Critique of Current Evidence
First (1), how can we assess flossing effectiveness when the frequency of flossing was self-reported (at best, by people keeping an activity log) 1 and there were no actual measures of flossing skill? Second (2), how can meta-data findings—based on a limited number of studies (many with significant potential for bias)—be generalized to patients with unique or complex dentition? Finally (3), how should we interpret and apply evidence based findings—especially ones with serious limitations—to clinical care? Herein lies the rub.
Background
Dental caries are known to be driven by factors such as excess exposure to sugars [fermentable carbohydrates] 3, a lack of exposure to fluoride 4, and a lack of regular and ongoing annual comprehensive dental visits for the purposes of prevention, cleaning and early treatment. The social determinants of disease (e.g., access to dental care, insurance coverage, environmental factors related to socioeconomic status, etc.) also factor heavily into the prevalence of dental caries 5, 6. As such, the development (and subsequent prevention and/or treatment) of dental caries should be viewed as a complex, multifactorial process7. The issue of periodontal diseases (not directly addressed herein) is similarly complex and the interpretation of currently available evidence is likewise nuanced.
Clinical Example #1
With regard to the meta-analyses and their external validity—we ask: to what degree can these findings be appropriately applied to the general population? Specifically, what information, if any, do these meta-analyses provide about flossing outcomes among high-risk patients? Practicing clinicians recognize that the current [lack of] evidence regarding flossing certainly pose challenges when applied to a specific clinical case. For example, some individuals cannot reach and/or appropriately floss between certain teeth (e.g., posterior teeth, like between #2 and #3). In such a patient, there may be a “food trap” (build-up of food particles and dense plaque between teeth) adjacent to a wide and tight interproximal contact—in addition to some gingival recession between these teeth. If ignored over time, interproximal tooth decay could easily develop in this area which could even lead to tooth loss 8. Ideally, a person would both floss and use an appropriately-sized proxy brush in this area. Use of either cleaning aid can be technically challenging and requires professional guidance. If such a patient had been seen regularly by a dentist and the dentist had effectively informed the patient that they had a food trap between specific teeth and that it would be helpful for the patient tofloss (and use an interproximal cleaning aid in) this area daily to keep it free from food and dental plaque—and if the patient took such corrective action, then the likelihood of developing dental caries in this area could be significantly reduced. Further, substantial dental caries (increase in concentration and quantity of Streptococcus mutans 3) in the areas of #2 and #3 could then increase the likelihood of caries in #30 and/or #31, the area where the upper and lower arch occlude when eating or swallowing. In such situations, timely and individualized prevention-focused interventions are recommended 9, 10.
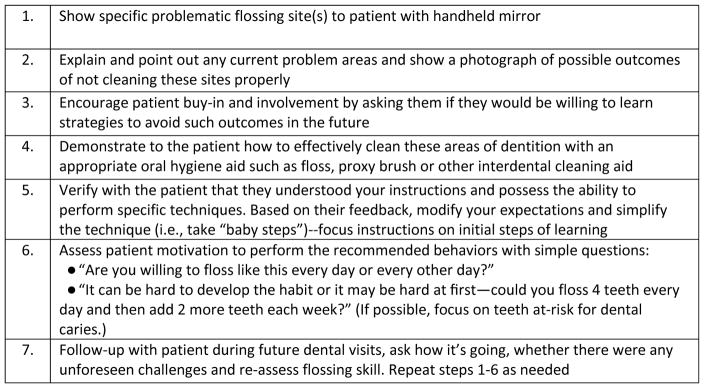
Many dental patients have a unique and/or challenging dentition that may require modifications to how they floss and/or use dental cleaning aids. Here, the challenge may be how the practice of flossing is communicated to the individual patient. Below are a set of recommended strategies for communicating with patients about flossing that are based upon existing heath theory9 (Figure 1)
Figure 1.
Strategies for Communicating Flossing to Patients
Such a comprehensive, healthy theory-informed approach to communicating with the patient about flossing/interproximal cleaning may help increase such oral hygiene behavior [tailored to high-risk teeth] and this could, in turn, help reduce caries risk—as compared to simply telling the patient, “You should floss every day.” Admittedly, the individualized or tailored approach described above can be time-consuming; thus, the use of adjunct technologies (i.e., the use of smart phone apps. selfies, and video training) may be required 11 to make such an approach viable and cost effective.
Clinical Example #2
Here is another example: consider a 3-year-old child (with some risk factors for dental caries) who has three areas in his or her mouth where two teeth touch each other (as we know, typically there is space between most teeth in younger children). We would argue that a parent should floss between specific teeth that touch (e.g., tooth E and F) and have plaque build-up on them because the enamel is very thin on deciduous teeth and caries can develop quickly. One could argue that with regular dental cleanings, limited [added or processed] sugar intake and an increase in topical fluoride exposure could help prevent dental caries—but such expectation may not be realistic with all parents of young children—especially if essential details (why/when and how) of flossing were not adequately communicated by oral health professionals. Therefore, flossing information and skill training (provided to parents of young children) would need to be tailored specifically to the needs of the individual child. In a systematic review by Hujoel et al, 2005 (anauthor whose own comments were quoted in the August 12, 2016 NYT article), professional flossing performed during school on young children was associated with a 40% risk reduction for dental caries (relative risk, 0.60; (% CI 0.48–0.76, p<0.001), implying that, when done regularly and skillfully, flossing significantly reduced risk for dental caries in children 12.
Evidence for Flossing versus Interdental Brushes—are Past Studies Nuanced Enough?
Recently, the European Federation of Periodontology (EFP) has recommended interdental brushes (IBDs), but could not recommend flossing (except in where contacts are too tight for IBDs to be used without possibility of trauma), for the removal of interdental plaque to manage gingivitis 13, 14. The authors’ recommendations, while aimed at managing periodontal diseases, are based largely upon low quality evidence plagued by many of the same methodological issues as studies that we critique herein. Briefly, among the limited number of studies comparing the effectiveness of flossing versus IBDs, there again was little emphasis on evaluating whether participants’ flossing skill was effective; as well, the frequency of flossing was typically assessed using a form of self-reported data (e.g., journals, logs, or daily diaries)2. Additionally, for interproximal sites where IBDs did not fit, these areas were typically excluded from study assessment2. Further, the durations of all (7) studies cited as evidence for the effectiveness of IBDs were relatively short (≤12 weeks) with some studies limited to just one month 2. The above would seem to be serious limitations worth further consideration. Finally, we ask how the lay public as well as oral health providers will interpret simplified recommendations (https://prevention.efp.org/wp-content/uploads/2015/12/Prevention-of-periodontal-diseases-general-guidance1.pdf) that preferentially recommend IBDs over flossing (bullet point #5 on this webpage)? While we fully endorse thorough plaque removal using effective tooth brushing and other techniques, could the recommendation to promote gingival health stressing IBD use (if taken out of context) be conflated with the prevention of dental caries by some providers and/or the media? Or, could there be other unintended consequences linked to interpretation and/or implementation of such statements?
Our two major concerns in regard to the EFP recommendations [specifically related to IBD use] are: 1) interproximal caries can occur where two teeth touch (tightly); this is an area where IBDs generally cannot clean, and 2) studies showing favorable results for IBD use (without proper flossing instruction) may largely be demonstrating that IBD use is easier and more intuitive (as compared to flossing). It is possible that participants had greater compliance and thus greater effect with IBDs on the basis of these factors. It is important to note that, in our critique, we are advocating for enhanced cleaning between the teeth. While this goal may be accomplished using IBDs and/or effective flossing, there are specific situations (see case #1 and #2, above) in which flossing is likely the most effective oral hygiene option currently available. However, in defense of the EFP guidelines, if most people prefer and find IDB use easier than flossing (which is technique sensitive), than IDB use would certainly be preferred over no interdental cleaning whatsoever [i.e., avoiding flossing because it is challenging to learn].
A Health Theory-informed Approach to Promote Flossing and IDB Use
By highlighting these two specific examples, above, we advocate that oral health providers tailor their oral health advice—(including flossing and IBD use), based on the clinical presentation, caries risk assessment of the patient 15, and possibly other personal/socio-demographic factors 6, 7. Adequately tailoring patient recommendations would likely lead to greater flossing adoption and ongoing maintenance. Further, such prevention-focused behaviors would likely lower the risk for dental caries (as issues such as diet, effective tooth brushing/fluoride exposure and access to care can, of course, trump any one single oral hygiene practice).
For many, flossing (and even IBD use in posterior teeth) can be a challenging skill to properly master16, and therein lies another rub: are dentists and other oral health providers adequately trained to help their patients change their behavior? To our knowledge, this has not been well studied.
Specifically, what percentage of dentists/oral health providers has received the appropriate training to conduct such assessments and then tailor their advice to specific patient needs? Presumably, with effective training, practitioners may feel more capable and motivated to implement time-limited, prevention-focused strategies. However, realistically, there would need to be greater economic incentives—given the overhead costs incurred in private practice and the current insurance reimbursements that focus on procedures. These are not minor hurdles, but there are options and strategies that could be implemented if there were sufficient will to do so.
Thus, we believe,, based on our current evidence, that to conclude that flossing is ineffective [against dental caries] may be a premature conclusion, and one that, quite possibly, may be seriously flawed. Most of the studies included in the Cochran review assessed flossing habits using patient self-report. To the best of our knowledge, directly-observed measures (of how well individuals flossed their teeth) were not used. While, at present, one such measures exists (e.g., Niederman and Sullivan, 1981) it is rarely used17, 18. Issues of patient recall, question framing and personal biases to report greater flossing frequency can all significantly limit the accuracy and utility of patients’ self-reported habits and must be carefully accounted for prior to implementing self-report outcome based studies 19. Additional assessments of flossing quality and frequency are needed components of future studies to ensure valid and reliable study findings.
Current NIH-Funded Research
Our group has developed a directly-observed measure of how well a person brushes teeth and flosses their teeth—termed the Oral Hygiene Skills Mastery (OHSIM). This new measure is designed to assess key oral hygiene competencies in order to guide the tailored coaching of specific technical skills. While intended primarily to address flossing in relation to periodontal diseases, OHSIM—once deemed reliable and provisionally valid—could also be used in future clinical studies to address flossing and risk for developing dental caries.
Future Implications
The future use of OHSIM may help the dental community to take a more methodologically rigorous approach to studying the effect of improved oral hygiene on clinical oral health outcomes. For example, longitudinal, within-person, pre-and post-interventional studies can help identify for whom flossing (in addition to tooth brushing) is essential and at what frequency (times per week), duration (minutes or seconds per time flossing), area (which teeth) and skill level is needed for specific individuals (based on, for example, age, access to care, and current oral condition) in order to achieve and maintain their desired level of oral health.
Acknowledgments
This work was funded by the National Institutes of Health: R21 DE023740 and had no involvement in writing this manuscript. Conflict of interests: None.
Contributor Information
Lance T. Vernon, Case Western Reserve University School of Dental Medicine, Department of Pediatric Dentistry and Community Dentistry; 10900 Euclid Avenue, Cleveland, Ohio USA 44106-4905.
Jason D. Seacat, Western New England University, Department of Psychology, 1215 Wilbraham Road, Springfield, MA 01119.
References
- 1.Sambunjak D, Nickerson JW, Poklepovic T, et al. Flossing for the management of periodontal diseases and dental caries in adults. Cochrane Database Syst Rev. 2011:CD008829. doi: 10.1002/14651858.CD008829.pub2. [DOI] [PubMed] [Google Scholar]
- 2.Poklepovic T, Worthington HV, Johnson TM, et al. Interdental brushing for the prevention and control of periodontal diseases and dental caries in adults. Cochrane Database Syst Rev. 2013:CD009857. doi: 10.1002/14651858.CD009857.pub2. [DOI] [PubMed] [Google Scholar]
- 3.Featherstone JD. The caries balance: the basis for caries management by risk assessment. Oral Health Prev Dent. 2004;2(Suppl 1):259–264. [PubMed] [Google Scholar]
- 4.Featherstone JD. The continuum of dental caries--evidence for a dynamic disease process. J Dent Res. 2004;83(Spec No C):C39–42. doi: 10.1177/154405910408301s08. [DOI] [PubMed] [Google Scholar]
- 5.Marmot M, Bell R. Social determinants and dental health. Adv Dent Res. 2011;23:201–206. doi: 10.1177/0022034511402079. [DOI] [PubMed] [Google Scholar]
- 6.Watt RG. Social determinants of oral health inequalities: implications for action. Community Dent Oral Epidemiol. 2012;40(Suppl 2):44–48. doi: 10.1111/j.1600-0528.2012.00719.x. [DOI] [PubMed] [Google Scholar]
- 7.Fisher-Owens SA, Gansky SA, Platt LJ, et al. Influences on children’s oral health: a conceptual model. Pediatrics. 2007;120:e510–520. doi: 10.1542/peds.2006-3084. [DOI] [PubMed] [Google Scholar]
- 8.Bignozzi I, Crea A, Capri D, Littarru C, Lajolo C, Tatakis DN. Root caries: a periodontal perspective. J Periodontal Res. 2014;49:143–163. doi: 10.1111/jre.12094. [DOI] [PubMed] [Google Scholar]
- 9.Chapple ILC, Hill K. Getting the message across to periodontitis patients: the role of personalized biofeedback. International Dental Journal. 2008;58:294–306. [Google Scholar]
- 10.Vernon L, Howard A. Advancing Health Promotion in Dentistry: Articulating an Integrative Approach to Coaching Oral Health Behavior Change in the Dental Setting. Curr Oral Health Rep. 2015;2:111–122. doi: 10.1007/s40496-015-0056-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Madan Kumar PD, Mohandoss AA, Walls T, Rooban T, Vernon LT. Using smartphone video “selfies” to monitor change in toothbrushing behavior after a brief intervention: A pilot study. Indian journal of dental research: official publication of Indian Society for Dental Research. 2016;27:268–277. doi: 10.4103/0970-9290.186241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hujoel PP, Cunha-Cruz J, Loesche WJ, Robertson PB. Personal oral hygiene and chronic periodontitis: a systematic review. Periodontol 2000. 2005;37:29–34. doi: 10.1111/j.1600-0757.2004.03795.x. [DOI] [PubMed] [Google Scholar]
- 13.Chapple IL, Van der Weijden F, Doerfer C, et al. Primary prevention of periodontitis: managing gingivitis. J Clin Periodontol. 2015;42(Suppl 16):S71–76. doi: 10.1111/jcpe.12366. [DOI] [PubMed] [Google Scholar]
- 14.Salzer S, Slot DE, Van der Weijden FA, Dorfer CE. Efficacy of inter-dental mechanical plaque control in managing gingivitis--a meta-review. J Clin Periodontol. 2015;42(Suppl 16):S92–105. doi: 10.1111/jcpe.12363. [DOI] [PubMed] [Google Scholar]
- 15.Featherstone JD, Domejean-Orliaguet S, Jenson L, Wolff M, Young DA. Caries risk assessment in practice for age 6 through adult. J Calif Dent Assoc. 2007;35:703–707. 710–703. [PubMed] [Google Scholar]
- 16.Thavarajah R, Kumar M, Mohandoss AA, Vernon LT. Drilling Deeper into tooth brushing skills: Is proactive interference an under-recognized factor in oral hygiene behavior change? Curr Oral Health Rep. 2015;2:123–128. doi: 10.1007/s40496-015-0053-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Niederman R, Sullivan TM. Oral Hygiene Skill Achievement Index I. J Periodontol. 1981;52:143–149. doi: 10.1902/jop.1981.52.3.143. [DOI] [PubMed] [Google Scholar]
- 18.Niederman R, Sullivan TM, Weiss D, Morhart R, Robbins W, Maier D. Oral Hygiene Skill Achievement Index II. J Periodontol. 1981;52:150–154. doi: 10.1902/jop.1981.52.3.150. [DOI] [PubMed] [Google Scholar]
- 19.Loftus EF. Suggestion, imagination, and the transformation of reality. In: Stone A, Tukkan JS, CA, BHS, KVC, editors. The science of self-report, implications for research and practice. New Jersey, USA: Lawrence Erlbaum Associates; 2000. pp. 201–210. [Google Scholar]