Abstract
The NK group 2 member D (NKG2D) immune receptor is implicated in both human and mouse autoimmune diabetes. However, the significance of NKG2D in diabetes pathogenesis has been unclear due to conflicting reports as to the importance of this receptor in the NOD mouse model. In this study we demonstrate that NKG2D expression affects NOD diabetes development by at least two previously undescribed, and opposing, mechanisms. First, we demonstrate that the NKG2D ligand H60a is induced on activated NOD T cells, and that NKG2D–H60a interaction during CD8+ T cell differentiation into CTLs generally decreases the subsequent CTL effector cytokine response. This corresponds to an increase in diabetes development in NKG2D-deficient compared with wild-type NOD mice under microbiota-depleted conditions. Second, we demonstrate that NKG2D promotes NOD diabetes development through interaction with the microbiota. Together these findings reveal a previously undescribed role for NKG2D ligand expression by activated T cells in CTL development. Further, they demonstrate that NKG2D has both diabetogenic and antidiabetogenic roles in NOD diabetes development.
INTRODUCTION
Type 1 diabetes is an autoimmune disease occurring with increasing frequency worldwide (1). In type 1 diabetes the insulin-producing β cells in pancreatic islets are destroyed by the immune system, resulting in a lifelong dependence on supplemental insulin therapy and reduced life expectancy (2). The cause of type 1 diabetes remains unknown; however, it is clear that many factors contribute to disease development. T cells are believed to play a significant role in type 1 diabetes development, with CD8+ T cells being critical to β cell destruction (3–6). Mouse studies implicate the NK group 2 member D (NKG2D) immune receptor in this diabetogenic CD8+ response (7–9). Further, genetic linkage studies suggest an association between polymorphismin the gene encoding one of the human NKG2D ligands, MHC class I chain–related A (MICA), and type 1 diabetes (7, 8, 10).
NKG2D, encoded by the gene Klrk1, is expressed on all human and mouse NK cells, all human CD8+ T cells, activated (but not naive) mouse CD8+ T cells, γδ T cells, NKT cells, and rare CD4+ T cells in both human and mouse (11–17). NKG2D binds to a number of ligands that are not normally expressed by most healthy tissues, but rather are induced by cellular stress (18). In humans, the NKG2D ligands are MICA, MICB, and the retinoic acid early transcript 1 family members (also known as the UL16-binding proteins, or ULBP1–6) (11, 19–21). The mouse NKG2D ligands are murine ULBP-like transcript 1, the RAE1 protein family (RAE1α-ε), and H60 proteins (H60a–c) (22–26). All ligands induce similar signaling through NKG2D, which in NK cells triggers granule release and cytokine production (27). The function of NKG2D engagement in CD8+ T cells is less well understood, with both costimulatory as well as TCR-independent functions, for NKG2D engagement on T cells described (8, 11, 20, 21, 28–31).
In a previous study with the NOD mouse model, expression of RAE1 was observed in the pancreatic islets, and Ab blockade of NKG2D was found to inhibit CD8+ T cell infiltration and prevent diabetes development (7). We subsequently showed that transgenic expression of RAE1ε by pancreatic β cells in nonautoimmune C57BL/6 mice caused recruitment of activated CD8+ T cells to pancreatic islets (8). This suggested a mechanism by which NKG2D ligand expression in the islets enhances diabetes development in NOD mice. However, RAE1 gene expression was not detected at any time during diabetes development in NOD pancreatic islets in two other studies (32, 33). Additionally, diabetes development in NOD mice genetically deficient in NKG2D was reported to be similar to that of wild-type NOD mice (34). These conflicting results suggest that NKG2D may play a more complex role in autoimmune diabetes development than originally proposed, affecting disease development through multiple mechanisms.
In the current study, we compared effector CTL responses and diabetes development between NOD mice genetically deficient in NKG2D expression (Klrk1−/−) and wild-type NOD mice. In contrast to what was previously reported (7), we detected the NKG2D ligand H60a, rather than RAE1, in the pancreatic islets of NOD mice. This expression was not on islet cells, but on infiltrating T cells. We also found that both H60a and NKG2D were expressed on NOD CD8+ T cells following activation, and that NKG2D–H60a interaction via homotypic CD8+ T cell contact during NOD CTL differentiation decreased effector cytokine production by the CTL in vitro. This corresponded with increased effector cytokine production by Klrk1−/− NOD CTL in vivo and increased diabetes development in microbiota-depleted Klrk1−/− NOD mice. By contrast, microbiota-replete Klrk1−/− mice had reduced diabetes development compared with wild-type mice, showing a separate effect resulting from interactions between NKG2D and the microbiota. Taken together, these results demonstrate that NKG2D influences NOD diabetes development by at least two separate, opposing mechanisms; NKG2D–ligand interaction during CTL generation dampens the diabetogenic CTL response, whereas NKG2D signaling induced by interaction with the microbiota promotes diabetogenesis.
MATERIALS AND METHODS
Mice
NOD mice were purchased from the Jackson Laboratory. Klrk1−/− mice on the C57BL/6 background have been previously described (35). The Klrk1−/− allele was moved from the C57BL/6 to the NOD genetic background using the speed congenics service of the Washington University School of Medicine to generate Klrk1−/− NOD mice. By single nucleotide polymorphism analysis (performed by DartMouse), these mice are 98% NOD, with the only observed genomic region containing a continuous interval of non–NOD-like single nucleotide polymorphisms found at the expected site of the Klrk1 knockout allele. Experiments were performed with Klrk1+/+ (wild-type) and Klrk1−/− NOD littermates from Klrk1+/− NOD interbreeding. Mice were housed under specific pathogen-free (SPF) conditions in the Washington University School of Medicine or University of Kansas Medical Center animal facilities in accordance with institutional guidelines.
Abs
Unconjugated anti-CD28 (Clone 37.51), anti-CD3ε (Clone 2C11), anti–mCD8-APC, anti–mCD4-BV786, anti–CD3ε-PE-Cy7, anti-mCD107 (LAMP1)-PE, anti–DX5-FITC, and anti-mCD45 were purchased from BD Biosciences. Anti–H60-PE, anti–mNKG2D-PE, rat IgG2a-PE, and rat IgG2b-PE were purchased from R&D Systems.
Pancreatic islet isolation
Islets were purified with a Ficoll-Paque gradient by published methods (36). Pancreata were minced and digested with collagenase IV (20 mg/ml) (Sigma-Aldrich). The digested pancreata were spun through a Ficoll-Paque gradient and the islets harvested.
RT-PCR
Single-cell suspensions were generated from whole pancreas, purified islets, or from cells separated into CD45+ and CD45− fractions via magnetic bead separation (Invitrogen). Total RNA was isolated with Trizol (Invitrogen) followed by the RNeasy Mini Kit (Qiagen) according to the manufacturers’ protocols. Reverse transcription was performed with the SABiosciences RT2 First Strand Kit (QIAGEN). Real-time quantitative PCR was performed using the Power SYBR Green PCR Master Mix (Applied Biosystems) and an ABI 7500 (Applied Biosystems) instrument, according to the manufacturers’ instructions. Transcript levels were normalized to 18S. The sequence of the primers used were: RAE1 (all isoforms): forward 5′-CCACCTGGGAATTCAACA-3′ TC; reverse 5′-TGA TCT TGG CTT TTC CTT GG-3′; H60a: forward 5′-TGC CTG ATT CTG AGC CTT TTC-3′ A; reverse 5′-ATT CAC TGA GCA CTG TCC ATG TAG-3′ AT; 18S: forward 5′-CCGCAGCTAGGAATAATGGAA-3′; reverse 5′-CGAACCTCC GAC TTT CGT TCT-3′.
In vitro CTL generation
All cells were grown in IMDM (Cellgro) supplemented with 10% defined FBS (HyClone), penicillin-streptomycin-glutamine (Life Technologies), and β-mercaptoethanol (Sigma-Aldrich). For activation of total splenocytes, spleens were harvested from 6 to 8 wk old SPF-housed NOD mice, passed through a 40 µm cell strainer, and plated in a six-well dish at 1.5 × 107 cells per well in 3 ml media and 1 µg/ml of plate-bound anti-CD3ε (2C11). For purified CD8+ T cells, cells were harvested from spleens and lymph nodes of 6–8 wk old NOD mice, and enriched by negative selection using magnetic beads (BD Biosciences) according to the manufacturer’s protocol. CD8+ T cells were then plated at 3–5 × 106 cells per well in a six-well dish with 1 µg/ml plate-bound anti-C3ε (2C11) and soluble anti-CD28 (37.51). The cells were allowed to expand for 5 d and split as needed.
Cytokine analysis
In vitro
CTL were harvested and plated at 1 × 105 cells per well in 100 µl of fresh media in 96-well plates precoated with anti-CD3 (2C11) at the stated concentrations. Cells were incubated at 37°C for 20 h. Supernatant was then collected and cytokines were analyzed using the Mouse Inflammation Cytometric Bead Array kit (BD Biosciences) and an LSR II (BD Biosciences). Data were quantified using FCAP array software (BD Biosciences).
In vivo
Total CD8+ T cells were purified from spleens and lymph nodes of 6–8wk old Klrk1−/− or wild-type NOD mice by negative selection using magnetic beads (BD Biosciences) according to the manufacturer’s protocol. Isolated Klrk1−/− and wild-type CD8+ T cells were then labeled with eFluor 670 (eBioscience) and CFSE (Thermo Fisher Scientific), respectively. The labeled cells were then mixed 1:1 and adoptively transferred via retro orbital injection into 6–8 wk old wild-type NOD recipient mice (Supplemental Fig. 2A). Total splenocytes were harvested after 7 d, incubated for 4–6 h in complete media with GolgiPlug protein transport inhibitor (BD Biosciences), followed by fixation and permeabilization using BD Cytofix/Cytoperm (BD Biosciences) according to the manufacturer’s directions. Cells were then stained overnight at 4°C with anti-mouse TNF-α (BD Pharmingen), anti-mouse IFN-γ (BD Pharmingen), and anti-mouse CD8 (BioLegend), and analyzed by flow cytometry. Transferred CD8+ T cells were analyzed by gating on live lymphocytes based on forward and side scatter, CD8+ cells, then either eFluor 670+ or CFSE+ cells.
Lamp-1 granule release analysis
CTL were plated at 1 × 105 in 100 µl fresh media in 96-well plates precoated with anti-CD3ε (2C11) at the stated concentrations. Before plating, PE-conjugated anti-CD107a was added to the cells at 4 µl/ml. Cells were incubated at 37°C for 3 h before being washed, fixed in 2% paraformaldehyde, and assessed for LAMP1 staining by flow cytometry.
Antibiotic treatment of mice
A solution of 0.5 g/l vancomycin (Sigma-Aldrich), 1 g/l neomycin (Sigma-Aldrich), 1 g/l ampicillin (Sigma-Aldrich), and 1 g/l metronidazole (Sigma-Aldrich) was made in grape KoolAid. This solution was mixed with Dietgel Boost (ClearH2O) and crushed food pellets.
Klrk1−/− and wild-type NOD littermates were exclusively fed this antibiotic mixture beginning at weaning until euthanasia. Sequencing of the 16S rRNA genes present in feces confirmed that the Firmicutes and Bacteroidetes populations, the two predominant bacteria phyla present in the intestine, were reduced 94–99% within 4 wk of antibiotic treatment.
Diabetes determination
In all experiments the age of diabetes development was defined as the age at which the first of two consecutive blood glucose measurements ≥250 mg/dl was obtained.
Statistical analysis
Data were analyzed using a two-tailed unpaired Mann–Whitney U test, one-tailed Wilcoxon test, or two-way ANOVA as described in the figure legends. All statistical analyses were performed using GraphPad Prism.
RESULTS
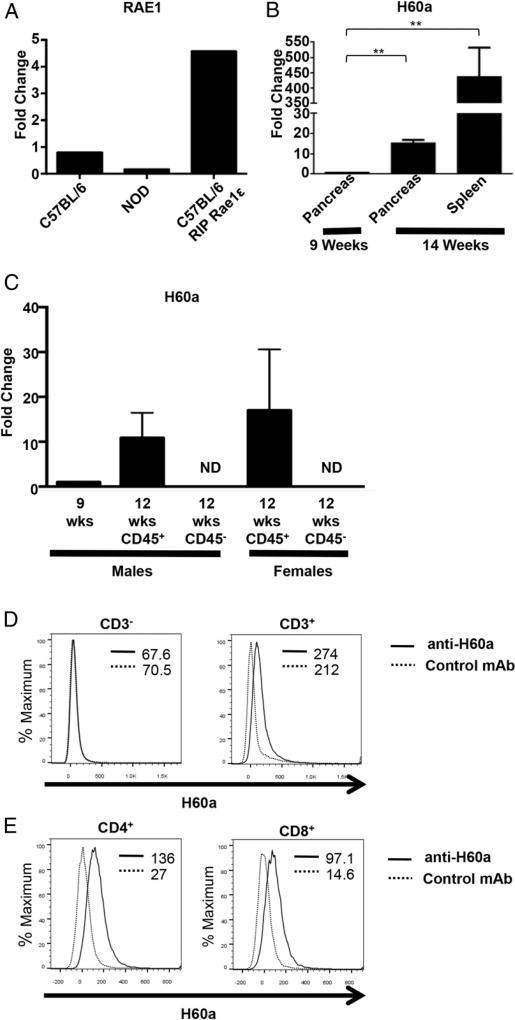
The NKG2D ligand H60a is expressed on infiltrating T cells within the pancreas of NOD mice
We set out to better characterize the role of NKG2D and its ligands in NOD diabetes. We first examined wild-type NOD pancreatic islets for NKG2D ligand expression. A previous report described the expression of RAE1 family members in the pancreatic β-islet cells of NOD mice, and suggested that this expression targeted β-islet cells for autoimmune destruction (7). Therefore, we first looked for RAE1 mRNA expression in the pancreatic islets of our NOD mice. We used RIP-RAE1ε mice, which constitutively express RAE1ε in the pancreatic islets (8), as a positive control. However, we were unable to detect RAE1 mRNA in the pancreatic islets of wild-type NOD mice in our colony (Fig. 1A). We next looked for expression of the other NKG2D ligand expressed in NOD mice, H60a. We found significant expression of H60a mRNA in both the pancreas and spleen of NOD mice by 12 wk of age (Fig. 1B, 1C).
FIGURE 1. T cells within the pancreas of NOD mice express the NKG2D ligand H60a.
(A) Relative expression of RAE1 mRNA levels in isolated pancreatic islets from 20 wk old C57BL/6, NOD, or RIP-RAE1ε (8) mice. (B) Relative expression of H60a mRNA in the pancreas and spleen of 9 (expression set as 1-fold) and 14 wk old NOD mice (mean ± STD). (C) Relative expression of H60a mRNA in CD45+ and CD45− cells purified from isolated NOD pancreatic islets (mean ± STD). The housekeeping gene 18S was used in all experiments. (D) H60a expression on CD3− and CD3+ cells within the pancreas of a 12 wk old NOD mouse. (E) H60a expression on CD4+ and CD8+ T cells within the pancreas of a 12 wk old NOD mouse. The mean fluorescence intensity of staining is shown. Data are representative of at least three independent experiments. **p ≤ 0.01 in two-tailed unpaired Mann–Whitney U test. ND, not detected.
To determine whether H60a was expressed within pancreatic islets, as well as which cells expressed H60a, we compared H60a mRNA levels between immune (CD45+) and nonimmune (CD45−) cells present within isolated islets from 12 wk old mice. These analyses revealed H60a mRNA was expressed in the CD45+ immune cells, but not the CD45− islet cells (Fig. 1C). Finally, we determined by flow cytometric analysis that the major cells expressing H60a were pancreas-infiltrating T cells (Figs. 1D, 1E).
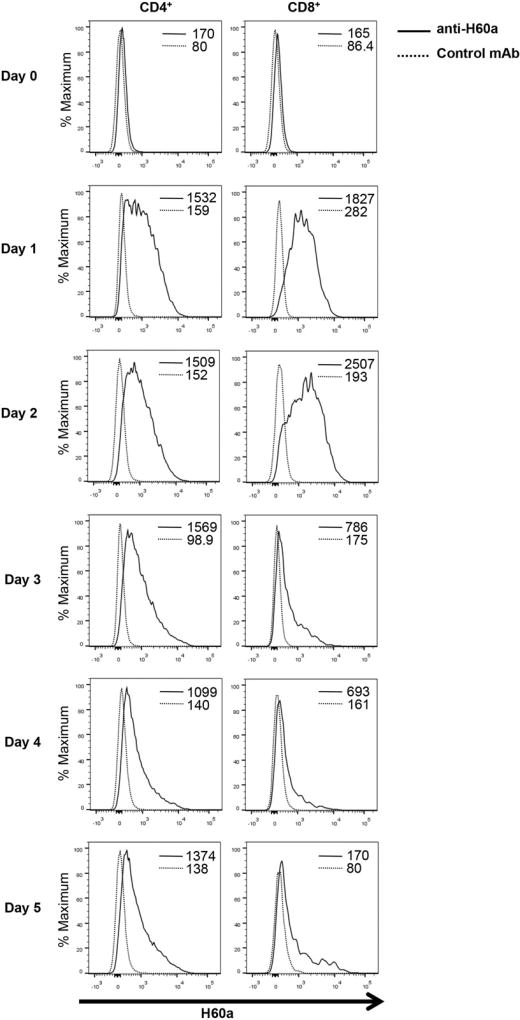
NOD CD8+ T cells express NKG2D and H60a upon activation
We next set out to determine the role of H60a expression by NOD T cells. We first characterized the expression of H60a on splenic T cells in young (6–8 wk old) NOD mice. We observed low but detectable H60a expression on freshly isolated splenic T cells (Fig. 2). We tested whether activation would increase this expression by stimulating NOD splenocytes in vitro with anti-CD3 Ab. H60a expression increased substantially on both CD4+ and CD8+ T cells following activation and remained elevated through day 5 of culture (Fig. 2).
FIGURE 2. NOD T cells express H60a upon activation.
H60a expression on CD4+ and CD8+ T cells following activation of NOD splenocytes with anti-CD3ε Ab. The mean fluorescence intensity of staining is shown. H60a expression was assessed on CD4+ and CD8+ gated live cells. Data are representative of at least four independent experiments.
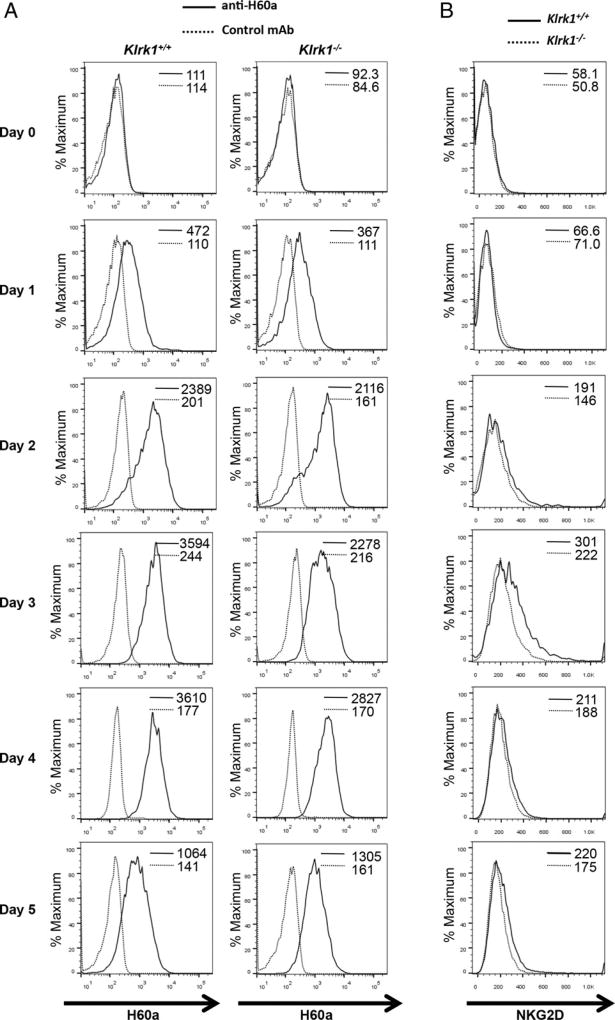
In addition to H60a, activated NOD CD8+ T cells express NKG2D (7). Therefore, we determined the time course of both H60a and NKG2D expression after initial TCR activation of NOD CD8+ T cells in vitro. CD8+ T cells were purified from the spleens and lymph nodes of 6–8 wk old Klrk1−/− and wild-type NOD mice. NKG2D and H60a expression was assessed at the time of cell isolation and daily following activation with anti-CD3 and anti-CD28 Abs. Similar to what we observed with whole splenocytes (Fig. 2), a low level of H60a was detected directly ex vivo, increased after TCR activation, and continued through day 5 (Fig. 3A). This expression was unaffected by Klrk1 (Fig. 3A). In wild-type mice, NKG2D became detectable on day 2 and persisted through day 5 (Fig. 3B).
FIGURE 3. NOD CD8+ T cells express both H60a and NKG2D upon activation.
Expression of (A) H60a and (B) NKG2D on CD8+ T cells purified from 6 to 8 wk old Klrk1−/− and wild-type NOD mice activated with anti-CD3ε and anti-CD28 Abs. Mean fluorescence intensity of staining is shown. Data are representative of at least four independent experiments.
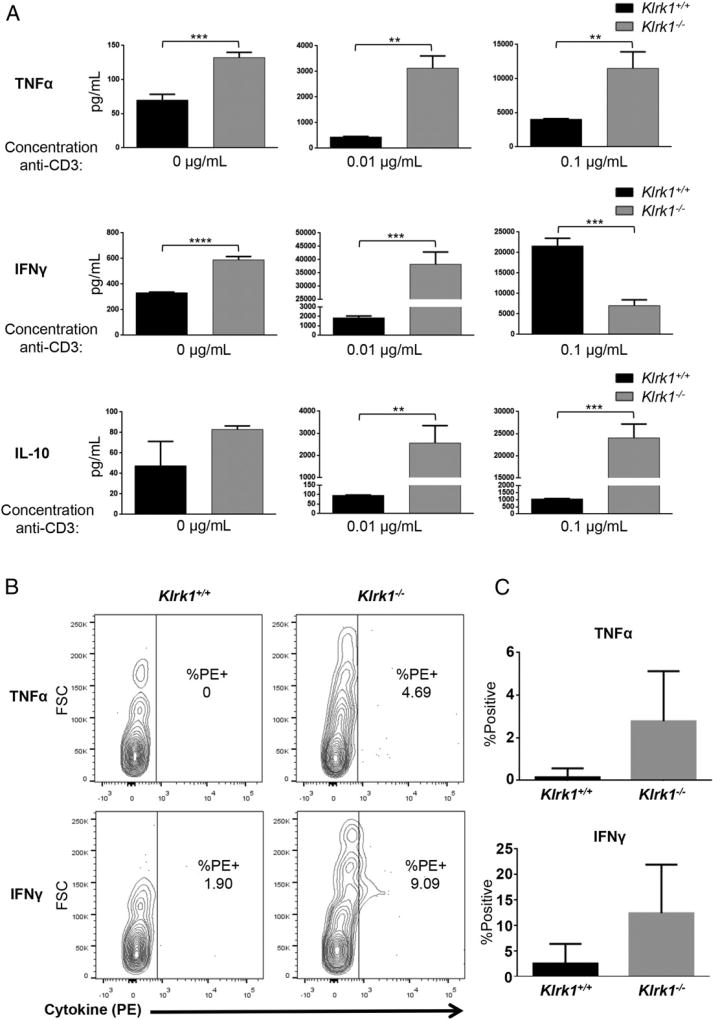
NKG2D expression alters NOD CTL effector cytokine responses in vitro and in vivo
NKG2D engagement by ligands expressed on target cells enhances CTL effector function induced by TCR engagement by Ag expressed on the same target cells (11, 28). Given our finding that NOD CTL coexpress NKG2D and the NKG2D ligand H60a, we hypothesized NKG2D–H60a interaction via homotypic CD8+ T cell contact could similarly alter NOD CTL effector function. To test this, we activated purified Klrk1−/− and wild-type NOD CD8+ T cells with anti-CD3 and anti-CD28 Abs in vitro and allowed them to differentiate for 5 d. Cytokine production and lytic granule release by the CTL were then assessed after restimulation with various concentrations of plate-bound anti-CD3 Ab to mimic target cell recognition.
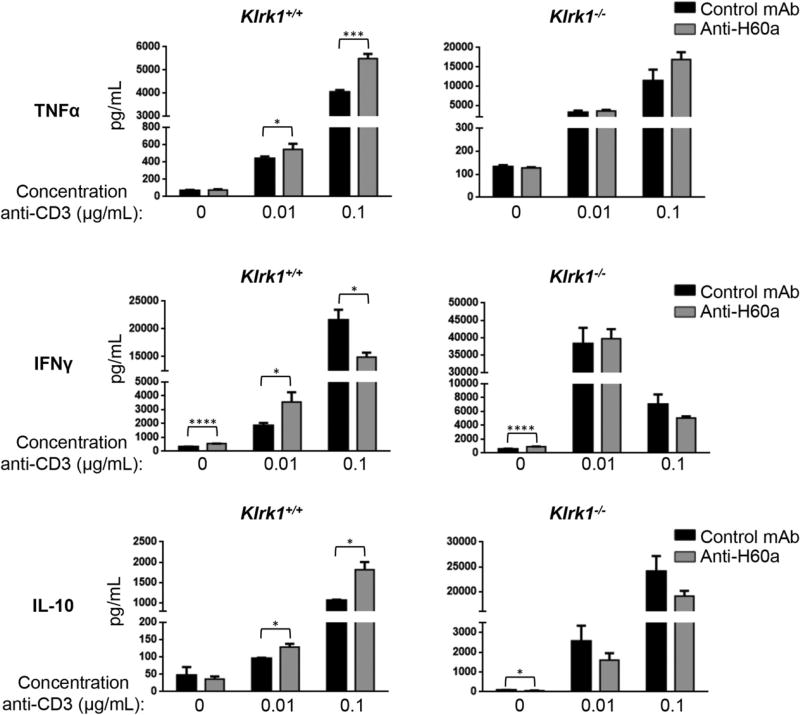
In the absence of stimulation, or with a low concentration of anti-CD3 Ab, Klrk1−/− CTL produced significantly more IFN-γ, TNF-α, and IL-10 compared with wild-type CTL (Fig. 4A, Supplemental Fig. 1A). With a higher concentration of anti-CD3 Ab, Klrk1−/− CTL also produced greater amounts of TNF-α and IL-10 (Fig. 4A, Supplemental Fig. 1A). At this higher level of stimulation, IFN-γ production by Klrk1−/− CTL was lower in some experiments compared with wild-type CTL; however, this did not reach statistical significance when data from multiple experiments were combined (Fig. 4A, Supplemental Fig. 1A). In contrast to this effect on cytokine production, no change in lytic granule release was observed (Supplemental Fig. 1B). To determine if NKG2D expression similarly affected NOD CD8+ T cell cytokine production in vivo, we purified CD8+ T cells from Klrk1−/− or wild-type NOD mice and labeled them with eFluor 670 or CFSE, respectively. Without providing exogenous TCR activation, we adoptively transferred a 1:1 mixture of these cells into wild-type NOD recipient mice (Supplemental Fig. 2A). After 1 wk, Klrk1−/− cells recovered from the spleen produced more TNF-α and IFN-γ than wild-type cells recovered from the same spleen (Fig. 4B, 4C). Together, these results demonstrate that expression of NKG2D by NOD CD8+ T cells generally reduces effector cytokine production by these cells.
FIGURE 4. Altered cytokine production by Klrk1−/− NOD CTL.
(A) Secretion of TNF-α, IFN-γ, and IL-10 (mean ± STD) by in vitro–generated Klrk1−/− and wild-type CTL stimulated with the indicated concentrations of anti-CD3ε Ab. Data are representative of at least six independent experiments. (B) Representative flow cytometry plots showing intracellular staining of TNF-α and IFN-γ in Klrk1−/− and wild-type NOD CD8+ T cells 1 wk after cotransfer into a wild-type NOD adoptive transfer recipient mouse. (C) Combined results (mean ± SEM) from transfers into eight mice from three independent experiments showing the percent TNF-α or IFN-γ positive Klrk1−/− and wild-type NOD CD8+ T cells 1 wk after cotransfer into wild-type NOD adoptive transfer recipient mice. **p ≤ 0.01, ***p ≤ 0.001, ****p ≤ 0.0001 in two-tailed unpaired Mann–Whitney U test.
NKG2D–H60a interaction during NOD CTL differentiation dampens diabetogenic cytokine production
To assess whether the increased cytokine production by Klrk1−/− CTL was the result of a loss of NKG2D interaction with H60a during the effector response, we included a blocking Ab against H60a during effector CTL stimulation. However, this blockade did not affect cytokine secretion by any of the CTLs (Supplemental Fig. 3A, 3B). This led us to hypothesize that NKG2D–H60a interaction during CTL differentiation, rather than during the effector CTL response, was responsible for the altered cytokine production by Klrk1−/− CTL. To test this, we added anti-H60a blocking Ab at the beginning of the T cell culture. This resulted in increased TNF-α, IL-10, and IFN-γ by wild-type CTL when the cells were stimulated with a low concentration of anti-CD3 Ab (Fig. 5, Supplemental Fig. 4). With a higher concentration of anti-CD3 Ab, H60a blockade also resulted in greater production of TNF-α and IL-10, but lower or similar production of IFN-γ, by wild-type CTLs (Fig. 5, Supplemental Fig. 4). Confirming this effect of H60a blockade was dependent on NKG2D expression, no difference in cytokine production was observed between CD3-stimulated anti–H60a-and isotype control-treated Klrk1−/− CTL (Fig. 5, Supplemental Fig. 4). The similar effect of NKG2D deficiency (Fig. 4A, Supplemental Fig. 1A) and H60a blockade during CTL differentiation (Fig. 5, Supplemental Fig. 4) demonstrates that NKG2D–H60a interaction via homotypic CD8+ T cell contact during CTL differentiation alters the NOD CTL effector cytokine response, generally reducing production.
FIGURE 5. Blockade of NKG2D–H60a interaction during NOD CTL differentiation results in increased CTL effector cytokine production.
Secretion of TNF-α, IFN-γ, and IL-10 by in vitro–generated Klrk1−/− and wild-type CTL stimulated with the indicated concentrations of anti-CD3ε Ab in the presence of an anti-H60a or isotype control Ab. Data are representative of at least six independent experiments. *p ≤ 0.05, ***p ≤ 0.001, ****p ≤ 0.0001 in two-tailed unpaired Mann–Whitney U test.
NKG2D enhances diabetes development in SPF-housed NOD mice
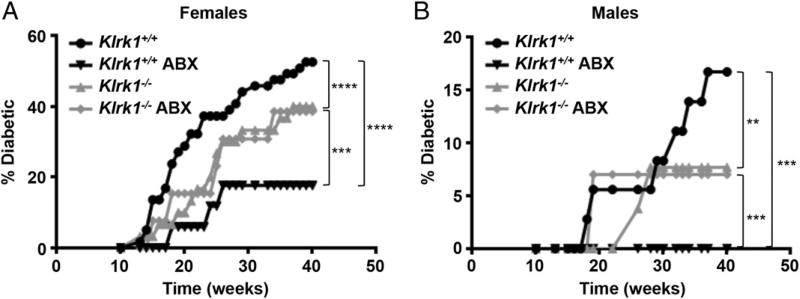
Expression of TNF-α, IFN-γ, and IL-10 within the islets all enhance NOD insulitis and diabetes development (37). Given the increased production of these cytokines by Klrk1−/− CTL, we predicted that NKG2D expression would have a protective role in NOD diabetes development. To test this, we first compared diabetes development between Klrk1−/− and wild-type NOD littermates housed under SPF conditions. As is well characterized in the NOD model (38–40), there was greater diabetes development in the female compared with the male mice. However, in both sexes, the Klrk1−/− mice exhibited slower diabetes development compared with wild-type mice (Fig. 6).
FIGURE 6. NKG2D expression affects NOD diabetes development and is protective in microbiota-depleted NOD mice.
Cumulative diabetes incidence in (A) female wild-type (n = 59), antibiotic (ABX)-treated wild-type (n = 17), Klrk1−/− (n = 30), ABX-treated Klrk1−/− (n = 13) and (B) male wild-type (n = 36), ABX-treated wild-type (n = 10), and Klrk1−/− (n = 26) and ABX-treated Klrk1−/− (n = 14) NOD mice. **p ≤ 0.002, ***p ≤ 0.001, ****p ≤ 0.0001 in two-way ANOVA.
NKG2D decreases diabetes in NOD mice treated with broad-spectrum antibiotics
The reduced diabetes development in Klrk1−/− NOD mice was inconsistent with our finding that NKG2D–H60a interaction decreases CTL effector function. This suggested there is an additional prodiabetic role for NKG2D signaling in disease development. We hypothesized that this role may be via interaction with the microbiota. This was based on the fact that Klrk1−/− mice are deficient in B1a B cells (41), which are believed to play a major role in shaping the microbiota composition via IgA production (24), and that NOD diabetes development is sensitive to microbiota alterations (40, 42–44). To test this hypothesis, we compared the effect on diabetes development of an antibiotic treatment that largely depletes the intestinal microbiota (45–47). Compared with SPF-housed wild-type mice, antibiotic-treated wild-type NOD mice exhibited reduced diabetes development (Fig. 6). By contrast, diabetes development in Klrk1−/− mice was unchanged by antibiotic treatment (Fig. 6). These results demonstrate that an interaction exists between NKG2D and the microbiota present in our SPF mouse colony, which enhances NOD diabetes incidence. By contrast, with antibiotic treatment, diabetes development was enhanced in Klrk1−/− compared with wild-type NOD mice (Fig. 6). Similar to SPF-housed mice, adoptively transferred Klrk1−/− cells recovered from the spleen of antibiotic-treated wild-type mice produced more TNF-α and IFN-γ compared with adoptively transferred wild-type cells (Supplemental Fig. 2B). These results support our findings that NKG2D plays a protective role during NOD diabetes development via interaction with H60a during CTL differentiation.
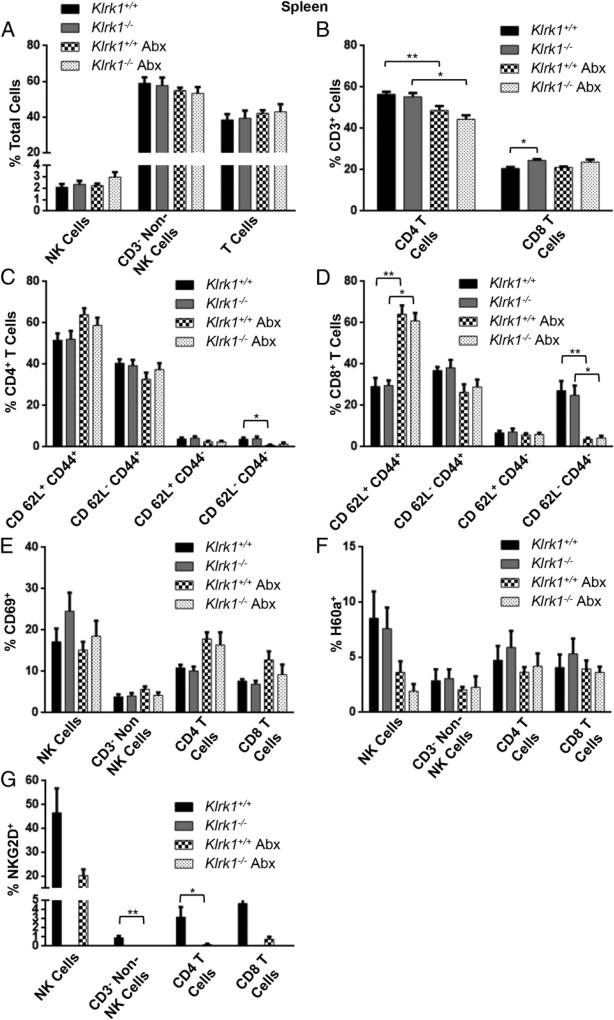
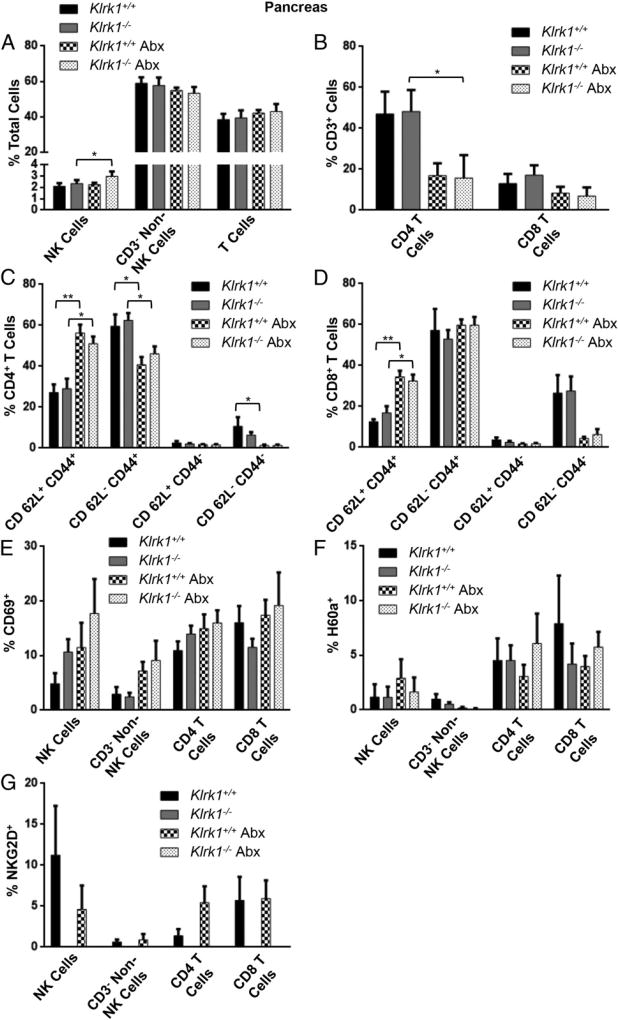
We next compared the immune cell populations present in the spleen and pancreas of wild-type and Klrk1−/− mice under both SPF and antibiotic-treated conditions. Antibiotic treatment did not significantly change NKG2D or H60a expression (Figs. 7G, 8G), and there was no difference in CD69 expression on immune cells in the pancreas or spleen between wild-type and Klrk1−/− mice under either condition (Figs. 7E, 8E). Antibiotic treatment did result in a decrease in CD4+ T cells in both the pancreas and spleen (Figs. 7B, 8B), and altered the ratio of effector to central memory CD4+ T cells in the pancreas (Fig. 8C). Specifically, with antibiotics there were fewer effector CD4+ T cells (CD44+CD62L−) and more central memory CD4+ T cells (CD44+CD62L+) in the pancreas in both wild-type and Klrk1−/− mice (Fig. 8C). There was a similar increase in central memory CD8+ T cells in the pancreas; however, unlike the CD4+ T cell population, there was no corresponding decrease in effector CD8+ T cells (Fig. 8D). These data demonstrate that there were fewer effector T cells in the pancreas of the antibiotic-treated mice. This corresponds with the reduced diabetes development in these mice compared with SPF-housed wild-type mice (Fig. 6), as well as the increased ability to observe the protective role of NKG2D in antibiotic-treated mice (Fig. 6).
FIGURE 7. Immune cell populations, activation, and NKG2D and H60a expression in the spleen of untreated and antibiotic-treated Klrk1+/+ and Klrk1−/− NOD mice.
(A) Percentage of total splenocytes in 12 wk old wild-type and Klrk1−/− NOD mice with or without antibiotic that were CD3− CD49b+ (NK cells), CD3− CD49b− (non-T or NK cells), or CD3+ (T cells). (B) Percentage of splenic T cells in (A) that were CD4+ and CD8+. (C) CD62L and CD44 expression by splenic CD4+ T cells in (A). (D) CD62L and CD44 expression by splenic CD8+ T cells in (A). (E–G) Percentage of splenic populations in (A) and (B) that expressed (E) CD69, (F) H60a, or (G) NKG2D. Data are combined results (mean ± SEM) of at least four mice per group. *p ≤ 0.05, **p ≤ 0.01 in two-tailed unpaired Mann–Whitney U test.
FIGURE 8. Immune cell populations, activation, and NKG2D and H60a expression in the pancreata of untreated and antibiotic-treated Klrk1+/+ and Klrk1−/− NOD mice.
(A) Percentage of cells isolated from the pancreata of 12 wk old wild-type and Klrk1−/− NOD mice with or without antibiotic that were CD3− CD49b+ (NK cells), CD3− CD49b− (non-T or NK cells), or CD3+ (T cells). (B) Percentage of T cells in (A) that were CD4+ and CD8+. (C) CD62L and CD44 expression by CD4+ T cells in (A). (D) CD62L and CD44 expression by CD8+ T cells in (A). (E–G) Percentage of populations in (A) and (B) that expressed (E) CD69, (F) H60a, or (G) NKG2D. Data are combined results (mean ± SEM) of at least four mice per group. *p ≤ 0.05, **p ≤ 0.01 in two-tailed unpaired Mann–Whitney U test.
DISCUSSION
In this study we demonstrate that NKG2D expression affects NOD diabetes development via two previously undescribed mechanisms. First, we demonstrate that interaction between NKG2D and H60a, both expressed on differentiating CTL, reduces the production of effector cytokines by NOD CTL. This corresponds with decreased diabetes development in antibiotic-treated Klrk1−/− NOD mice. Second, we showed that NKG2D influences NOD diabetes development via interaction with the microbiota.
NKG2D is implicated in the development of autoimmune diabetes in both humans and mice (7–10); however, a definitive role for NKG2D in this disease has not been established. Much of this uncertainty has been due to seemingly conflicting results in the NOD mouse model. Previous reports have demonstrated that NKG2D either promotes NOD diabetes (7) or has little effect (34). In particular, Ogasawara et al. (7) suggested that expression of the NKG2D ligand RAE1 in pancreatic islets targets islet β cells for NKG2D-mediated destruction. Our later finding that transgenic expression of RAE1 by islet β cells drove immune cell infiltration of pancreatic islets in the non-autoimmune C57BL/6 background seemed to support the feasibility of this model (8). In the current study, however, we did not detect expression of RAE1 mRNA, or any other NKG2D ligand, by CD45− cells in pancreatic islets. This finding is consistent with other reports that found no RAE1 mRNA (32, 33), or protein (33) expressed by NOD islet cells. These differing reports of RAE1 expression may be a result of variance between NOD mouse colonies due to gut microbial influence or genetic drift (40, 42, 48). A report by Adlercreutz et al. (49) did show expression of H60a mRNA in the pancreatic islets of 13 wk old NOD and BALB/c mice, but did not distinguish between immune and nonimmune cells. This is consistent with the H60a mRNA expression observed in our study.
Our observation of robust H60a expression by activated NOD CD8+ T cells was not anticipated, but is consistent with earlier reports. H60a mRNA was previously shown to be expressed in healthy NOD tissues and by NOD NK cells (49, 50). Similar to the NOD mouse, BALB/c immune cells express H60a (23, 25, 51), and mRNA encoding this NKG2D ligand was shown to be upregulated in BALB/c T cells upon activation (52). Likewise, human T cells also express NKG2D ligands upon activation (53–55).
Constitutive NKG2D ligand expression decreases NKG2D surface expression on NK and CD8+ T cells (18, 56, 57). Poor NKG2D expression has been previously reported on NOD NK cells (50), which correlated with RAE1 expression by these cells (50). Similarly, the high level of H60a expression on NOD CD8+ T cells is likely responsible for the low surface expression of NKG2D we observed on these cells. However, our results clearly show that this low NKG2D expression has functional relevance to CTL differentiation.
To date, the function of NKG2D in CD8+ T cells has largely been studied in differentiated CTLs. These studies have generally shown a costimulatory role for NKG2D, enhancing TCR-stimulated effector function (11, 28, 58) or memory formation (59, 60). The effects of NKG2D signaling in the absence of TCR engagement are not well understood, but have been shown to induce immune synapse formation by mouse CTLs (28) and MHC-unrestricted killing by cytokine-activated human CTLs (61). Therefore, our finding that there is a role for NKG2D–H60a interaction during CD8+ T cell differentiation into CTL describes a new mode of NKG2D–ligand interaction, which dampens, rather than enhances, later CTL responses.
In our in vitro experiments, there was a consistent decrease in TNF-α, IL-10, and IFN-γ production by CTL with either genetic knockout of NKG2D or Ab blockade of H60a with low levels of stimulation. At the highest level of stimulation, IFN-γ production was significantly decreased in a number of experiments (Figs. 4, 5). This decrease could potentially reflect a different cytokine response at very high levels of TCR stimulation. However, because this decrease was not significant when data from all experiments were combined (Supplemental Figs. 1, 3), we did not investigate this further. Additionally, the consistently enhanced production of IFN-γ by Klrk1−/− adoptively transferred CD8+ T cells in vivo (Fig. 4B, 4C) suggests that low to medium levels of TCR stimulation more closely reflect in vivo conditions.
When we assessed diabetes incidence in Klrk1−/− and wild-type NOD mice, our results indicated a different effect of NKG2D genotype on diabetes incidence depending upon whether the mice were treated with microbiota-depleting antibiotics. Under SPF housing conditions, we found a detrimental role for NKG2D in NOD diabetes development. By contrast, when animals were treated with antibiotics, wild-type NOD mice had delayed disease compared with Klrk1−/− mice. This differential effect revealed a separate protective role for NKG2D. In addition, the lack of an effect of antibiotic treatment on disease incidence in Klrk1−/− mice provides evidence for NKG2D genotype–dependent changes in the microbiota affecting NOD diabetes incidence. Antibiotic-treatment resulted in a decrease in effector T cells in the pancreas. This is a probable mechanism by which diabetes development was decreased in antibiotic-treated compared with SPF-housed wild-type mice. Further, it is likely that this decrease in effector T cells is responsible for the increased ability to observe the protective role of NKG2D in diabetes development with antibiotic treatment. Taken together, our results lead us to propose a detrimental influence of NKG2D on diabetes development in the gut, which involves the microbiota, and a separate effect independent of microbiota in which NKG2D dampens the NOD CTL cytokine response.
We observed the well-established sexual dimorphism in NOD diabetes incidence, with increased rates of diabetes in females compared with males (38–40). Within SPF-housed or antibiotic-treated groups, however, the effect of NKG2D was consistent between males and females. The mechanism by which NKG2D promotes NOD diabetes through interactions with microbiota was not explored in the current study, but warrants further investigation. This may be due to a lack of B1a cells in these mice (41), or interaction of other immune cells with NKG2D ligands, which are constitutively expressed by intestinal epithelial cells (62–65). Additionally, further work remains to conclusively attribute the protective effect of NKG2D genotype in antibiotic-treated animals to the effects of NKG2D–H60a interactions between CD8+ T cells. Although our data do support this hypothesis, a definitive answer awaits the generation of a NOD H60a−/− mouse, as well as CD8+ T cell conditional NOD NKG2D−/− and NOD H60a−/− animals. Finally, our model of opposing pro- and antidiabetic effects of NKG2D suggests that a lack of consensus from previous studies concerning the role of NKG2D in NOD diabetes may be the result of variation in cohousing practices and differences in microbiota between mouse colonies.
In summary, we found that NKG2D–H60a interaction between CD8+ T cells during NOD CTL differentiation in vitro resulted in decreased production of diabetogenic cytokines upon subsequent CTL activation. To our knowledge, this is the first report of a role for NKG2D–NKG2D ligand interaction during differentiation of mouse CD8+ T cells into CTL rather than during the effector phase of differentiated CTL. Furthermore, these results describe a functional role for NKG2D ligand expression by healthy murine CD8+ T cells. Finding that NKG2D is protective in animals with depleted microbiota correlates with NKG2D signaling resulting in reduced cytokine production by NOD CTL. The additional observation that microbiota-depleting antibiotics profoundly affected NOD diabetes development in wild-type, but not Klrk1−/−, animals demonstrates a separate effect in which NKG2D-dependent alterations in the microbiota promote disease development. Additionally, these data may have broader implications for the role of NKG2D–ligand interaction between T cells in modulating CD8+ T cell responses in both mice and humans.
Supplementary Material
Acknowledgments
This work was supported by Washington University Diabetes Research Center Grant P30 DK020579 (to M.A.M.), American Diabetes Association Grant 1-12-JF-41 (to M.A.M.), National Institutes of Health Centers of Biomedical Research Excellence Grant P20GM104936 (to M.A.M.), the American Association of Immunologists Careers in Immunology Fellowship Program (to N.S. and M.A.M.), and National Institutes of Health/Integrated Grants Management System Grant P30 GM103326 (flow cytometry core).
Abbreviations used in this article
- MICA
MHC class I chain–related A
- NKG2D
NK group 2 member D
- SPF
specific pathogen-free.
Footnotes
The online version of this article contains supplemental material.
DISCLOSURES
The authors have no financial conflicts of interest.
References
- 1.Heinonen MT, Moulder R, Lahesmaa R. New insights and biomarkers for type 1 diabetes: review for Scandinavian Journal of Immunology. Scand. J. Immunol. 2015;82:244–253. doi: 10.1111/sji.12338. [DOI] [PubMed] [Google Scholar]
- 2.van Belle TL, Coppieters KT, von Herrath MG. Type 1 diabetes: etiology, immunology, and therapeutic strategies. Physiol. Rev. 2011;91:79–118. doi: 10.1152/physrev.00003.2010. [DOI] [PubMed] [Google Scholar]
- 3.Pinkse GG, Tysma OH, Bergen CA, Kester MG, Ossendorp F, van Veelen PA, Keymeulen B, Pipeleers D, Drijfhout JW, Roep BO. Autoreactive CD8 T cells associated with beta cell destruction in type 1 diabetes. Proc. Natl. Acad. Sci. USA. 2005;102:18425–18430. doi: 10.1073/pnas.0508621102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderson MS, Bluestone JA. The NOD mouse: a model of immune dysregulation. Annu. Rev. Immunol. 2005;23:447–485. doi: 10.1146/annurev.immunol.23.021704.115643. [DOI] [PubMed] [Google Scholar]
- 5.Mallone R, Martinuzzi E, Blancou P, Novelli G, Afonso G, Dolz M, Bruno G, Chaillous L, Chatenoud L, Bach JM, van Endert P. CD8+ T-cell responses identify beta-cell autoimmunity in human type 1 diabetes. Diabetes. 2007;56:613–621. doi: 10.2337/db06-1419. [DOI] [PubMed] [Google Scholar]
- 6.Roep BO, Peakman M. Antigen targets of type 1 diabetes autoimmunity. Cold Spring Harb. Perspect. Med. 2012;2:a007781. doi: 10.1101/cshperspect.a007781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ogasawara K, Hamerman JA, Ehrlich LR, Bour-Jordan H, Santamaria P, Bluestone JA, Lanier LL. NKG2D blockade prevents autoimmune diabetes in NOD mice. Immunity. 2004;20:757–767. doi: 10.1016/j.immuni.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 8.Markiewicz MA, Wise EL, Buchwald ZS, Pinto AK, Zafirova B, Polic B, Shaw AS. RAE1ε ligand expressed on pancreatic islets recruits NKG2D receptor-expressing cytotoxic T cells independent of T cell receptor recognition. Immunity. 2012;36:132–141. doi: 10.1016/j.immuni.2011.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van Belle TL, Ling E, Haase C, Bresson D, Ursø B, von Herrath MG. NKG2D blockade facilitates diabetes prevention by antigen-specific Tregs in a virus-induced model of diabetes. J. Autoimmun. 2013;40:66–73. doi: 10.1016/j.jaut.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 10.Gambelunghe G, Brozzetti A, Ghaderi M, Candeloro P, Tortoioli C, Falorni A. MICA gene polymorphism in the pathogenesis of type 1 diabetes. Ann. N. Y. Acad. Sci. 2007;1110:92–98. doi: 10.1196/annals.1423.011. [DOI] [PubMed] [Google Scholar]
- 11.Bauer S, Groh V, Wu J, Steinle A, Phillips JH, Lanier LL, Spies T. Activation of NK cells and T cells by NKG2D, a receptor for stress-inducible MICA. Science. 1999;285:727–729. doi: 10.1126/science.285.5428.727. [DOI] [PubMed] [Google Scholar]
- 12.Wu J, Song Y, Bakker AB, Bauer S, Spies T, Lanier LL, Phillips JH. An activating immunoreceptor complex formed by NKG2D and DAP10. Science. 1999;285:730–732. doi: 10.1126/science.285.5428.730. [DOI] [PubMed] [Google Scholar]
- 13.Dai Z, Turtle CJ, Booth GC, Riddell SR, Gooley TA, Stevens AM, Spies T, Groh V. Normally occurring NKG2D +CD4+ T cells are immunosuppressive and inversely correlated with disease activity in juvenile-onset lupus. J. Exp. Med. 2009;206:793–805. doi: 10.1084/jem.20081648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Groh V, Bruhl A, El-Gabalawy H, Nelson JL, Spies T. Stimulation of T cell autoreactivity by anomalous expression of NKG2D and its MIC ligands in rheumatoid arthritis. Proc. Natl. Acad. Sci. USA. 2003;100:9452–9457. doi: 10.1073/pnas.1632807100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Groh V, Smythe K, Dai Z, Spies T. Fas-ligand-mediated paracrine T cell regulation by the receptor NKG2D in tumor immunity. Nat. Immunol. 2006;7:755–762. doi: 10.1038/ni1350. [DOI] [PubMed] [Google Scholar]
- 16.Jamieson AM, Diefenbach A, McMahon CW, Xiong N, Carlyle JR, Raulet DH. The role of the NKG2D immunoreceptor in immune cell activation and natural killing. Immunity. 2002;17:19–29. doi: 10.1016/s1074-7613(02)00333-3. [DOI] [PubMed] [Google Scholar]
- 17.Hyka-Nouspikel N, Lucian L, Murphy E, McClanahan T, Phillips JH. DAP10 deficiency breaks the immune tolerance against transplantable syngeneic melanoma. J. Immunol. 2007;179:3763–3771. doi: 10.4049/jimmunol.179.6.3763. [DOI] [PubMed] [Google Scholar]
- 18.Champsaur M, Lanier LL. Effect of NKG2D ligand expression on host immune responses. Immunol. Rev. 2010;235:267–285. doi: 10.1111/j.0105-2896.2010.00893.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bacon L, Eagle RA, Meyer M, Easom N, Young NT, Trowsdale J. Two human ULBP/RAET1 molecules with transmembrane regions are ligands for NKG2D. J. Immunol. 2004;173:1078–1084. doi: 10.4049/jimmunol.173.2.1078. [DOI] [PubMed] [Google Scholar]
- 20.Cosman D, Müllberg J, Sutherland CL, Chin W, Armitage R, Fanslow W, Kubin M, Chalupny NJ. ULBPs, novel MHC class I-related molecules, bind to CMV glycoprotein UL16 and stimulate NK cytotoxicity through the NKG2D receptor. Immunity. 2001;14:123–133. doi: 10.1016/s1074-7613(01)00095-4. [DOI] [PubMed] [Google Scholar]
- 21.Chalupny NJ, Sutherland CL, Lawrence WA, Rein-Weston A, Cosman D. ULBP4 is a novel ligand for human NKG2D. Biochem. Biophys. Res. Commun. 2003;305:129–135. doi: 10.1016/s0006-291x(03)00714-9. [DOI] [PubMed] [Google Scholar]
- 22.Carayannopoulos LN, Naidenko OV, Kinder J, Ho EL, Fremont DH, Yokoyama W. Ligands for murine NKG2D display heterogeneous binding behavior. Eur. J. Immunol. 2002;32:597–605. doi: 10.1002/1521-4141(200203)32:3<597::aid-immu597>3.3.co;2-5. [DOI] [PubMed] [Google Scholar]
- 23.Cerwenka A, Bakker AB, McClanahan T, Wagner J, Wu J, Phillips JH, Lanier LL. Retinoic acid early inducible genes define a ligand family for the activating NKG2D receptor in mice. Immunity. 2000;12:721–727. doi: 10.1016/s1074-7613(00)80222-8. [DOI] [PubMed] [Google Scholar]
- 24.Diefenbach A, Hsia JK, Hsiung MY, Raulet DH. A novel ligand for the NKG2D receptor activates NK cells and macrophages and induces tumor immunity. Eur. J. Immunol. 2003;33:381–391. doi: 10.1002/immu.200310012. [DOI] [PubMed] [Google Scholar]
- 25.Takada A, Yoshida S, Kajikawa M, Miyatake Y, Tomaru U, Sakai M, Chiba H, Maenaka K, Kohda D, Fugo K, Kasahara M. Two novel NKG2D ligands of the mouse H60 family with differential expression patterns and binding affinities to NKG2D. J. Immunol. 2008;180:1678–1685. doi: 10.4049/jimmunol.180.3.1678. [DOI] [PubMed] [Google Scholar]
- 26.Whang MI, Guerra N, Raulet DH. Costimulation of dendritic epidermal gammadelta T cells by a new NKG2D ligand expressed specifically in the skin. J. Immunol. 2009;182:4557–4564. doi: 10.4049/jimmunol.0802439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Le Bert N, Gasser S. Advances in NKG2D ligand recognition and responses by NK cells. Immunol. Cell Biol. 2014;92:230–236. doi: 10.1038/icb.2013.111. [DOI] [PubMed] [Google Scholar]
- 28.Markiewicz MA, Carayannopoulos LN, Naidenko OV, Matsui K, Burack WR, Wise EL, Fremont DH, Allen PM, Yokoyama WM, Colonna M, Shaw AS. Costimulation through NKG2D enhances murine CD8+ CTL function: similarities and differences between NKG2D and CD28 costimulation. J. Immunol. 2005;175:2825–2833. doi: 10.4049/jimmunol.175.5.2825. [DOI] [PubMed] [Google Scholar]
- 29.Diefenbach A, Jamieson AM, Liu SD, Shastri N, Raulet DH. Ligands for the murine NKG2D receptor: expression by tumor cells and activation of NK cells and macrophages. Nat. Immunol. 2000;1:119–126. doi: 10.1038/77793. [DOI] [PubMed] [Google Scholar]
- 30.Sutherland CL, Chalupny NJ, Schooley K, VandenBos T, Kubin M, Cosman D. UL16-binding proteins, novel MHC class I-related proteins, bind to NKG2D and activate multiple signaling pathways in primary NK cells. J. Immunol. 2002;168:671–679. doi: 10.4049/jimmunol.168.2.671. [DOI] [PubMed] [Google Scholar]
- 31.Meresse B, Chen Z, Ciszewski C, Tretiakova M, Bhagat G, Krausz TN, Raulet DH, Lanier LL, Groh V, Spies T, et al. Coordinated induction by IL15 of a TCR-independent NKG2D signaling pathway converts CTL into lymphokine-activated killer cells in celiac disease. Immunity. 2004;21:357–366. doi: 10.1016/j.immuni.2004.06.020. [DOI] [PubMed] [Google Scholar]
- 32.Carrero JA, Calderon B, Towfic F, Artyomov MN, Unanue ER. Defining the transcriptional and cellular landscape of type 1 diabetes in the NOD mouse [Published erratum appears in 2014 PLoS One 9.] PLoS One. 2013;8:e59701. doi: 10.1371/journal.pone.0059701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Angstetra E, Graham KL, Zhao Y, Irvin AE, Elkerbout L, Santamaria P, Slattery RM, Kay TW, Thomas HE. An indirect role for NK cells in a CD4(+) T-cell-dependent mouse model of type I diabetes. Immunol. Cell Biol. 2012;90:243–247. doi: 10.1038/icb.2011.16. [DOI] [PubMed] [Google Scholar]
- 34.Guerra N, Pestal K, Juarez T, Beck J, Tkach K, Wang L, Raulet DH. A selective role of NKG2D in inflammatory and autoimmune diseases. Clin. Immunol. 2013;149:432–439. doi: 10.1016/j.clim.2013.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zafirova B, Mandarić S, Antulov R, Krmpotić A, Jonsson H, Yokoyama WM, Jonjić S, Polić B. Altered NK cell development and enhanced NK cell-mediated resistance to mouse cytomegalovirus in NKG2D-deficient mice. Immunity. 2009;31:270–282. doi: 10.1016/j.immuni.2009.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kelly CB, Blair LA, Corbett JA, Scarim AL. Isolation of islets of Langerhans from rodent pancreas. Methods Mol. Med. 2003;83:3–14. doi: 10.1385/1-59259-377-1:003. [DOI] [PubMed] [Google Scholar]
- 37.Rabinovitch A. An update on cytokines in the pathogenesis of insulin-dependent diabetes mellitus. Diabetes Metab. Rev. 1998;14:129–151. doi: 10.1002/(sici)1099-0895(199806)14:2<129::aid-dmr208>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 38.Makino S, Kunimoto K, Muraoka Y, Katagiri K. Effect of castration on the appearance of diabetes in NOD mouse. Jikken Dobutsu. 1981;30:137–140. doi: 10.1538/expanim1978.30.2_137. [DOI] [PubMed] [Google Scholar]
- 39.Kikutani H, Makino S. The murine autoimmune diabetes model: NOD and related strains. Adv. Immunol. 1992;51:285–322. doi: 10.1016/s0065-2776(08)60490-3. [DOI] [PubMed] [Google Scholar]
- 40.Pozzilli P, Signore A, Williams AJ, Beales PE. NOD mouse colonies around the world–recent facts and figures. Immunol. Today. 1993;14:193–196. doi: 10.1016/0167-5699(93)90160-M. [DOI] [PubMed] [Google Scholar]
- 41.Lenartić M, Jelenčić V, Zafirova B, Ožanič M, Marečić V, Jurković S, Sexl V, Šantić M, Wensveen FM, Polić B. NKG2D promotes B1a cell development and protection against bacterial infection. J. Immunol. 2017;198:1531–1542. doi: 10.4049/jimmunol.1600461. [DOI] [PubMed] [Google Scholar]
- 42.Yurkovetskiy L, Burrows M, Khan AA, Graham L, Volchkov P, Becker L, Antonopoulos D, Umesaki Y, Chervonsky AV. Gender bias in autoimmunity is influenced by microbiota. Immunity. 2013;39:400–412. doi: 10.1016/j.immuni.2013.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mathis D, Benoist C. Microbiota and autoimmune disease: the hosted self. Cell Host Microbe. 2011;10:297–301. doi: 10.1016/j.chom.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 44.King C, Sarvetnick N. The incidence of type-1 diabetes in NOD mice is modulated by restricted flora not germ-free conditions. PLoS One. 2011;6:e17049. doi: 10.1371/journal.pone.0017049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rakoff-Nahoum S, Paglino J, Eslami-Varzaneh F, Edberg S, Medzhitov R. Recognition of commensal microflora by toll-like receptors is required for intestinal homeostasis. Cell. 2004;118:229–241. doi: 10.1016/j.cell.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 46.Ubeda C, Pamer EG. Antibiotics, microbiota, and immune defense. Trends Immunol. 2012;33:459–466. doi: 10.1016/j.it.2012.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Willing BP, Russell SL, Finlay BB. Shifting the balance: antibiotic effects on host-microbiota mutualism. Nat. Rev. Microbiol. 2011;9:233–243. doi: 10.1038/nrmicro2536. [DOI] [PubMed] [Google Scholar]
- 48.Simecek P, Churchill GA, Yang H, Rowe LB, Herberg L, Serreze DV, Leiter EH. Genetic analysis of substrain divergence in non-obese diabetic (NOD) mice. G3. 2015;5:771–775. doi: 10.1534/g3.115.017046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Adlercreutz EH, Weile C, Larsen J, Engkilde K, Agardh D, Buschard K, Antvorskov JC. A gluten-free diet lowers NKG2D and ligand expression in BALB/c and non-obese diabetic (NOD) mice. Clin. Exp. Immunol. 2014;177:391–403. doi: 10.1111/cei.12340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ogasawara K, Hamerman JA, Hsin H, Chikuma S, Bour-Jordan H, Chen T, Pertel T, Carnaud C, Bluestone JA, Lanier LL. Impairment of NK cell function by NKG2D modulation in NOD mice. Immunity. 2003;18:41–51. doi: 10.1016/s1074-7613(02)00505-8. [DOI] [PubMed] [Google Scholar]
- 51.Ogasawara K, Lanier LL. NKG2D in NK and T cell-mediated immunity. J. Clin. Immunol. 2005;25:534–540. doi: 10.1007/s10875-005-8786-4. [DOI] [PubMed] [Google Scholar]
- 52.Rabinovich BA, Li J, Shannon J, Hurren R, Chalupny J, Cosman D, Miller RG. Activated, but not resting, T cells can be recognized and killed by syngeneic NK cells. J. Immunol. 2003;170:3572–3576. doi: 10.4049/jimmunol.170.7.3572. [DOI] [PubMed] [Google Scholar]
- 53.Cerboni C, Zingoni A, Cippitelli M, Piccoli M, Frati L, Santoni A. Antigen-activated human T lymphocytes express cell-surface NKG2D ligands via an ATM/ATR-dependent mechanism and become susceptible to autologous NK- cell lysis. Blood. 2007;110:606–615. doi: 10.1182/blood-2006-10-052720. [DOI] [PubMed] [Google Scholar]
- 54.Molinero LL, Fuertes MB, Rabinovich GA, Fainboim L, Zwirner NW. Activation-induced expression of MICA on T lymphocytes involves engagement of CD3 and CD28. J. Leukoc. Biol. 2002;71:791–797. [PubMed] [Google Scholar]
- 55.Zwirner NW, Fernández-Viña MA, Stastny P. MICA, a new polymorphic HLA-related antigen, is expressed mainly by keratinocytes, endothelial cells, and monocytes. Immunogenetics. 1998;47:139–148. doi: 10.1007/s002510050339. [DOI] [PubMed] [Google Scholar]
- 56.Wiemann K, Mittrücker HW, Feger U, Welte SA, Yokoyama WM, Spies T, Rammensee HG, Steinle A. Systemic NKG2D down-regulation impairs NK and CD8 T cell responses in vivo. J. Immunol. 2005;175:720–729. doi: 10.4049/jimmunol.175.2.720. [DOI] [PubMed] [Google Scholar]
- 57.Coudert JD, Zimmer J, Tomasello E, Cebecauer M, Colonna M, Vivier E, Held W. Altered NKG2D function in NK cells induced by chronic exposure to NKG2D ligand-expressing tumor cells. Blood. 2005;106:1711–1717. doi: 10.1182/blood-2005-03-0918. [DOI] [PubMed] [Google Scholar]
- 58.Groh V, Rhinehart R, Randolph-Habecker J, Topp MS, Riddell SR, Spies T. Costimulation of CD8alphabeta T cells by NKG2D via engagement by MIC induced on virus-infected cells. Nat. Immunol. 2001;2:255–260. doi: 10.1038/85321. [DOI] [PubMed] [Google Scholar]
- 59.Zloza A, Kohlhapp FJ, Lyons GE, Schenkel JM, Moore TV, Lacek AT, O’Sullivan JA, Varanasi V, Williams JW, Jagoda MC, et al. NKG2D signaling on CD8+ T cells represses T-bet and rescues CD4-unhelped CD8+ T cell memory recall but not effector responses. Nat. Med. 2012;18:422–428. doi: 10.1038/nm.2683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wensveen FM, Lenartic M, Jelencic V, Lemmermann NA, ten Brinke A, Jonjic S, Polic B. NKG2D induces Mcl-1 expression and mediates survival of CD8 memory T cell precursors via phosphatidylinositol 3-kinase. J. Immunol. 2013;191:1307–1315. doi: 10.4049/jimmunol.1300670. [DOI] [PubMed] [Google Scholar]
- 61.Verneris MR, Karimi M, Baker J, Jayaswal A, Negrin RS. Role of NKG2D signaling in the cytotoxicity of activated and expanded CD8+ T cells [Published erratum appears in 2015 Blood 125: 2583] Blood. 2004;103:3065–3072. doi: 10.1182/blood-2003-06-2125. [DOI] [PubMed] [Google Scholar]
- 62.Hansen CH, Holm TL, Krych Ł, Andresen L, Nielsen DS, Rune I, Hansen AK, Skov S. Gut microbiota regulates NKG2D ligand expression on intestinal epithelial cells. Eur. J. Immunol. 2013;43:447–457. doi: 10.1002/eji.201242462. [DOI] [PubMed] [Google Scholar]
- 63.Hüe S, Mention JJ, Monteiro RC, Zhang S, Cellier C, Schmitz J, Verkarre V, Fodil N, Bahram S, Cerf-Bensussan N, Caillat-Zucman S. A direct role for NKG2D/MICA interaction in villous atrophy during celiac disease. Immunity. 2004;21:367–377. doi: 10.1016/j.immuni.2004.06.018. [DOI] [PubMed] [Google Scholar]
- 64.Allez M, Tieng V, Nakazawa A, Treton X, Pacault V, Dulphy N, Caillat-Zucman S, Paul P, Gornet JM, Douay C, et al. CD4+NKG2D+ T cells in Crohn’s disease mediate inflammatory and cytotoxic responses through MICA interactions. Gastroenterology. 2007;132:2346–2358. doi: 10.1053/j.gastro.2007.03.025. [DOI] [PubMed] [Google Scholar]
- 65.Eagle RA, Jafferji I, Barrow AD. Beyond stressed self: evidence for NKG2D ligand expression on healthy cells. Curr. Immunol. Rev. 2009;5:22–34. doi: 10.2174/157339509787314369. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.