Abstract
Child abuse is a sensitive topic among many medical practitioners and the diagnosis of this entity requires awareness about conditions which can mimic physical child abuse. Here, the authors present a case of a 13-year-old school non-attendee who was referred due to multiple scars, over areas prone to accidental as well as non-accidental injury, who underwent medicolegal examination due to suspicion of physical child abuse. On further inquiry, it was discovered that she had easy bruising and poor wound healing. A diagnosis of Ehlers-Danlos syndrome was established and physical child abuse was excluded. This case emphasizes the importance of identifying conditions which may confound the diagnosis of physical child abuse. This is of utmost importance in avoiding adverse legal and psycho-social implications on the child, family and society.
Keywords: Child Maltreatment, Child Neglect, Ehlers Danlos Disease
INTRODUCTION
Child abuse is a global problem affecting millions of children, varying from neglect and abandonment to physical and sexual abuse. The skin has been identified as the commonest organ to sustain injuries during childhood, whether it be through accidental or non-accidental means.1 Differentiating between accidental and non-accidental injuries requires understanding various injury patterns and recognizing warning (“red flag”) signs in the history provided by the parents/ guardians.
CASE REPORT
A 13-year-old girl presented to the surgical casualty ward with a large wound on the anterior aspect of her right leg, which was associated with pain and swelling of one week duration. The leg was swollen, tender and erythematous at the upper margin of the knee. A large wound was noted over the anterior tibial border, with necrotic tissue filling the wound’s floor. She also had fever with chills and rigors, suggestive of systemic involvement. She appeared unwell and miserable. A clinical diagnosis of complicated cellulitis was made and intravenous antibiotics were promptly initiated, after taking blood samples for culture. The clinical diagnosis was supported by laboratory investigations, including neutrophil leukocytosis and an elevated C-reactive protein level, and blood culture was positive for group A beta hemolytic streptococci. Antibiotics were changed according to antibiotic sensitivity. The wound was cleaned and dressed every other day and the leg was kept elevated.
The history revealed that she was an only child, abandoned by the father at the age of six. The mother had also left to work as a house maid in a Middle Eastern country, due to financial reasons. The child was in the care of the grandparents who were manual laborers. Due to financial difficulties, the child had dropped out of school. She was alone at home during the day when the grandparents were at work.
On inquiry, she had denied any form of abuse, physical or sexual, but admitted that she missed school and her friends. However, because of the delay in seeking medical treatment for the current condition and the appearance of multiple scars, receding hairline, and sparse hair which together suggested traumatic alopecia, the surgical team began to suspect physical child abuse (PCA) and neglect. Therefore, the child was referred for clinical forensic examination.
The informed consent was signed by the patient and her guardian.
The child was co-operative and was accompanied by her grandmother. She was 153 cm tall and thinly built, weighing 35 kg. Her BMI was calculated as 15, which is lower than a -2 z-score and was classified as thinness according to WHO growth charts. There were multiple atrophic scars over areas of the body prone to accidental and non-accidental injuries, including forehead and face, knees, shins, posterior trunk, and forearms (Figures 1, 2 and 3). The scars were at different stages of healing. Inquiry revealed that she had poor wound healing and that skin would appear thin and wrinkled after healing.
Figure 1. Front (A) and right (B) side of the face. Multiple thin scares with different stage of healing on non-accidental area, fine hair and hair lose, receding hairline.

Figure 2. Front aspect of right lower leg (A) close-up and front aspect of both lower legs (B). Abnormal scaring with wrinkling, chronic wound with poor healing.

Figure 3. Back aspect of both forearms (A) and left forearm (B) close-up. Thin abnormal scars on accidental and non-accidental areas.

She stated that she was prone to bruising easily including following a minor trauma and sometimes spontaneously, as well.
The unusual injury pattern prompted a dermatological referral, where she was noted to have velvety skin with normal recoil, mild to moderate hypermobility of joints (Figure 4) and “cigarette paper” scars over knees and legs, which are characteristic of Ehlers-Danlos syndrome (EDS) (Figure 5).
Figure 4. Left wrist (A) and left wrist & carpophalageal joints (B). Hypermobility of joints.
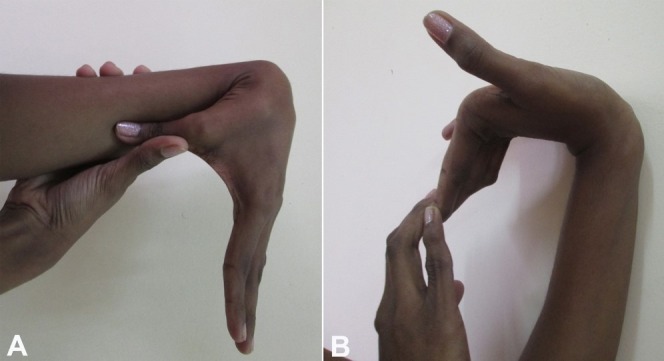
Figure 5. Flat/depressed large scares with evidence of underlying bruising (dark color).

Other differential diagnoses such as vasculidites and coagulopathies were excluded. Inquiry into the family history revealed the presence of lax skin and hyper-extensible joints in the paternal side of the family. The diagnosis of EDS was made and PCA was excluded.
The radiology referrals, to screen for skeletal abnormalities and PCA, and the venereology referrals, to screen for sexual abuse and sexually transmitted diseases, were negative. It was confirmed by the pediatricians that there was no evidence of nutritional deficiencies or bleeding disorders, and that her growth and development were normal. Her weight and height were between the 5th and 25th centiles. However, some degree of mental retardation was suspected and a psychiatric referral was made. She was deemed to have a low IQ level, which was possibly due to school non-attendance and the non-stimulating environment in which she lived.
Subsequently, a case conference was conducted and a decision was made to provide financial assistance to the family through the department of social services and to re- integrate the child back into a school environment.
DISCUSSION
We present the case of a 13-year-old girl suspected to be the subject of PCA based on cutaneous manifestations and socio-demographic factors. As in many other developing countries, Sri Lanka lacks adequate data regarding child abuse, probably due to under-detection as well as inadequate reporting and surveillance. In 2013, a study conducted in Kenya2 revealed that 18.2% of females and 24.5% of males were abused before attaining the age of 18 years. A majority of the reported cases involved sexual and physical abuse. Abandonment and neglect were also common types of abuse reported in this study, with 21.9% of children having been subjected to neglect by their parents/guardians. About 90% of PCA victims present with cutaneous manifestations, including bruises, lacerations, abrasions, burns, oral trauma, bite marks and traumatic alopecia. With bruises being the most common finding, it is mandatory to differentiate injuries following accidental and non-accidental trauma. Two characteristics that help differentiate an accidental from a non-accidental bruise include the location and pattern of the bruise, with distribution of bruises depending on the age and developmental stage of the child.5 Injury to areas including the face, ears, neck, trunk, upper arms, hands, inner and back aspect of upper legs, and genitalia should raise suspicion for child abuse, whereas involvement of knees, anterior tibial area, and overlying other bony prominences is commonly caused by accidental trauma.6 Furthermore, non-accidental bruises tend to be larger, multiple and occur in clusters. They may be of uniform shape and are commonly seen away from bony prominences, with some carrying the imprint of the offending object.7
Even though individuals with intellectual disabilities and a low intelligence quotient (IQ) are more prone to experience sexual abuse,8 there was no evidence of such a link in our reported patient. The presence of thinness and low IQ in a child should raise the suspicion of child abuse in the form of neglect, however with a multidisciplinary approach we were able to arrive at a diagnosis of EDS, avoiding the incorrect diagnosis of PCA, which could have resulted in catastrophic social, psychological and legal consequences.9
EDS is a heritable generalized connective tissue disorder, characterized by easy bruising and bleeding.10 The first comprehensive description of the syndrome was published in 189211 and according to the 2017 international classification of Ehlers-Danlos syndromes, 13 subtypes are recognized.3,4 Classic EDS, also known as EDS 1 and 2, commonly affects the joints and the skin. Hypermobility of joints affects both small and large joints.12 However, a cohort study done by Ritelli et al.13 demonstrated that joint hypermobility was absent in 20% cases of classic EDS. Classic EDS, with a prevalence of 1 in 20,000, can be diagnosed accurately with family history and clinical examination alone.14 The cutaneous manifestations seen in classic EDS are multiple, with the most common being smooth, velvety, fragile and hyper-extensible skin with easy bruising15 and atrophic scars,16 as were observed in our patient. Genetic mutations of COL5A1 and COL5A2, resulting in deficiency of type 5 collagen,17,18 have been identified to be responsible for around 50% of cases of classic EDS, with approximately 50% representing de novo mutations.19
As case reports with a diagnosis of EDS during evaluation for PCA are scarce in international literature, we believe this case report will emphasize the importance of being aware of natural disease such as EDS that can mimic injuries of PCA among medical practitioners. They should consider accidental non-accidental etiologies of observed bruises, and appreciate the importance of seeking referral to a multidisciplinary team when considering PCA.20,21
The manuscript has the approval /ethical clearance from the ethical review committee of the University of Peradeniya, Sri Lanka.
CONCLUSIONS AND RECOMMENDATIONS
A child with multiple scars and bruises was diagnosed with EDS and PCA was excluded.
This case highlights the need to:
-
i
Improve awareness among health professionals about natural diseases that can mimic injuries arising from PCA;
-
ii
Consider performing molecular testing for diagnosis of any condition or disease like EDS;
-
iii
Create access to a multi-disciplinary approach when evaluating suspected cases of PCA.
Footnotes
How to cite: Vadysinghe AN, Wickramashinghe CU, Nanayakkara DN, Kaluarachchi CI. Suspicious scars: physical child abuse vs Ehlers-Danlos syndrome. Autops Case Rep [Internet]. 2018;8(1):e2018008. http://dx.doi.org/10.4322/acr.2018.008
Financial support: None
REFERENCES
- 1.Coulter K. Bruising and skin trauma. Pediatr Rev. 2000;21(1):34-5. http://dx.doi.org/10.1542/pir.21-1-34. [DOI] [PubMed] [Google Scholar]
- 2.Unite for Children . Violence against children in Kenya: Findings from a 2010 National Survey. Kenya: United Nations Children’s Fund Kenya Country Office, Division of Violence Prevention, National Center for Injury Prevention and Control, U.S. Centers for Disease Control and Prevention, Kenya National Bureau of Statistics; 2012. [Google Scholar]
- 3.Malfait F, Francomano C, Byers P, et al. The 2017 international classification of the Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet. 2017;175(1):8-26. http://dx.doi.org/10.1002/ajmg.c.31552. [DOI] [PubMed] [Google Scholar]
- 4.Malfait F, Wenstrup RJ, De Paepe A. Clinical and genetic aspects of Ehlers-Danlos syndrome, classic type. Genet Med. 2010;12(10):597-605. http://dx.doi.org/10.1097/GIM.0b013e3181eed412. [DOI] [PubMed] [Google Scholar]
- 5.Reece RM, Christian CW, editors. Child abuse medical diagnosis and management. 3rd ed. Elk Grove Village: American Academy of Pediatrics; 2009. [Google Scholar]
- 6.Kos L, Shwayder T. Cutaneous manifestations of child abuse. Pediatr Dermatol. 2006;23(4):311-20. http://dx.doi.org/10.1111/j.1525-1470.2006.00266.x. [DOI] [PubMed] [Google Scholar]
- 7.Jenny C. Child abuse and neglect: diagnosis, treatment and evidence. St. Louis: Saunders/Elsevier; 2011. [Google Scholar]
- 8.Vadysinghe AN, Dassanayaka PB, Sivasubramanium M, Senasinghe DPP, Samaranayake AN, Wickramasinghe WMMHP. A study on sexual violence inflicted on individuals with intellectual developmental disorder. Disabil Health J. 2017;10(3):451-4. http://dx.doi.org/10.1016/j.dhjo.2016.12.010. [DOI] [PubMed] [Google Scholar]
- 9.Male I, Kenney I, Appleyard C, Evans N. Neoplasia masquerading as physical abuse. Child Abuse Rev. 2000;9(2):142-7. http://dx.doi.org/10.1002/1099-0852(200003/04)9:2<142::AID-CAR602>3.0.CO;2-E. [Google Scholar]
- 10.De Paepe A, Malfait F. The Ehlers Danlos syndrome, a disorder with many faces. Clin Genet. 2012;82(1):1-11. http://dx.doi.org/10.1111/j.1399-0004.2012.01858.x. [DOI] [PubMed] [Google Scholar]
- 11.Tschernogobow A. Cutis laxa. Mhft Prakt Dermatol. 1892;14:76. [Google Scholar]
- 12.De Paepe A, Malfait F. Bleeding and bruising in patients with Ehlers-Danlos syndrome and other collagen vascular disorders. Br J Haematol. 2004;127(5):491-500. http://dx.doi.org/10.1111/j.1365-2141.2004.05220.x. [DOI] [PubMed] [Google Scholar]
- 13.Ritelli M, Dordoni C, Venturini M, et al. Clinical and molecular characterization of 40 patients with classic Ehlers–Danlos syndrome: identification of 18 COL5A1 and 2 COL5A2 novel mutations. Orphanet J Rare Dis. 2013;8(1):58. http://dx.doi.org/10.1186/1750-1172-8-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Malfait F, Wenstrup R, De Paepe A. Ehlers-Danlos syndrome, Classic Type. Updated 2011 Aug 18 In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews®. Seattle: University of Washington; 2007. [cited 2017 Sept 20]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1244/ [Google Scholar]
- 15.Pourazizi M, Abtahi-Naeini B, Shapouri J, Masjedi M, Saffaei A. Unexplained facial scar: child abuse or Ehlers-Danlos syndrome? N Am J Med Sci. 2014;6(11):595-8. http://dx.doi.org/10.4103/1947-2714.145482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bursztejn AC, Baumann M, Lipsker D. Ehlers-Danlos syndrome related toFKBP14mutations: detailed cutaneousphenotype. Clin Exp Dermatol. 2017;42(1):64-7. http://dx.doi.org/10.1111/ced.12983. [DOI] [PubMed] [Google Scholar]
- 17.Walter SM. Case report: Ehlers-Danlos syndrome in an adolescent presenting with chronic daily headache. Surg Neurol Int. 2014;5(13, Suppl 13):S475-8. http://dx.doi.org/10.4103/2152-7806.144629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Paepe A, Nuytinck L, Hausser I, Anton-Lamprecht I, Naeyaert JM. Mutations in the COL5A1 gene are causal in the Ehlers-Danlos syndromes I and II. Am J Hum Genet. 1997;60(3):547-54. [PMC free article] [PubMed] [Google Scholar]
- 19.Pauker SP, Stoler JM. Clinical manifestations and diagnosis of Ehlers-Danlos syndromes. UpTtoDate; 2016. [cited 2017 Sept 20]. Available from: https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-ehlers-danlos-syndromes [Google Scholar]
- 20.Onyon C, Rabb L, Debelle G. Non-accidental injury and bone fragility disorders: the need for a multidisciplinary perspective. Child Abuse Rev. 2009;18(5):346-53. http://dx.doi.org/10.1002/car.1086. [Google Scholar]
- 21.Thain J. Child protection, public health and nursing. Nurs Child Young People. 2017;29(3):18 http://dx.doi.org/10.7748/ncyp.29.3.18.s21. [Google Scholar]


