Multidrug-resistant organisms (MDROs) are increasingly prevalent in post–acute care (PAC) facilities.1,2 Increased contact between health care workers, the environment, and patients in PAC facilities can increase the risk of MDRO cross-transmission3,4 because PAC patients may need assistance with activities of daily living and are encouraged to be mobile outside of their room for rehabilitation, dining, and other recreational activities. Much more than other anatomic sites, patients’ hands are more likely to come in contact with environmental surfaces, health care workers’ hands, and other patients in PAC facilities. Our objective was to evaluate baseline, new acquisition, and duration of MDRO hand carriage among patients newly admitted to PAC facilities from acute care hospitals.
Methods
This prospective observational cohort study in 6 PAC facilities in metropolitan Detroit and Southeast Michigan was approved by the institutional review board of the University of Michigan. After obtaining written informed consent, the dominant hands of newly admitted PAC patients were sampled. We swabbed the palm, fingers, and around nails of patients’ hands. Samples were collected at baseline (day of enrollment), day 14, and monthly for up to 180 days or until discharge from the facility. Methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus (VRE), and resistant gram-negative bacilli (RGNB) were identified using standard microbiological methods. Gram-negative bacilli resistant to either ceftazidime, ciprofloxacin, or imipenem were defined as RGNB.
Results
Of 826 consecutive eligible PAC patients approached for the study, 357 (43.2%) agreed to participate and were followed for 806 visits (mean, 2.3 visits; range, 1–8 visits). Most participants were female (54.9%), with a mean age of 75.8years.
Nearly one-quarter (86 of 357 [24.1%]) had at least 1 MDRO on their hands on discharge from an acute care hospital and admission to the PAC facility (Table). Baseline hand carriage rates of VRE, MRSA, and RGNB were 13.7%, 10.9%, and 2.8%, respectively. During follow-up (Figure), 34.2% of patients’ hands (122 of 357) were colonized with an MDRO, with 10.1% of patients (36 of 357) newly acquiring 1 or more MDROs. Specifically, 7.1% (22 of 308 at risk), 6.3% (20 of 318 at risk), and 3.1% (11 of 347 at risk) of patients newly acquired VRE, MRSA, and RGNB colonization, respectively. MRSA and VRE colonization were more likely to be persistent, with 37.3% (22 of 59) and 22.5% (16 of 71) of patients colonized at multiple visits, whereas RGNB colonization on the same patient’s hand was never obtained at follow-up. Overall, 67.2% of MDRO-colonized patients (82 of 122) remained colonized at discharge.
Table.
Baseline Patient Hand Carriage of MDROs in 6 Post–Acute Care Facilities
| Facility (Patients, No.) | Organisms, No. (%) | |||
|---|---|---|---|---|
| MRSA | VRE | RGNB | Any MDROa | |
| 1 (81) | 8 (9.9) | 7 (8.6) | 2 (2.5) | 16 (19.8) |
| 2 (47) | 6 (12.8) | 6 (12.8) | 1 (2.1) | 12 (25.5) |
| 3 (85) | 9 (10.6) | 9 (10.6) | 2 (2.4) | 19 (22.4) |
| 4 (81) | 8 (9.9) | 16 (19.8) | 2 (2.5) | 21 (25.9) |
| 5 (26) | 3 (11.5) | 5 (19.2) | 3 (11.5) | 8 (30.8) |
| 6 (37) | 5 (13.5) | 6 (16.2) | 0 | 10 (27.0) |
| Total (357) | 39(10.9) | 49 (13.7) | 10 (2.8) | 86 (24.1) |
Abbreviations: MDRO, multidrug resistant organism; MRSA, methicillin-resistant Staphylococcus aureus; RGNB, resistant-gram negative bacilli; VRE, vancomycin-resistant Enterococcus.
At least 1 MDRO.
Figure. Patient Hand Carriage of Organisms at Baseline and Follow-up.
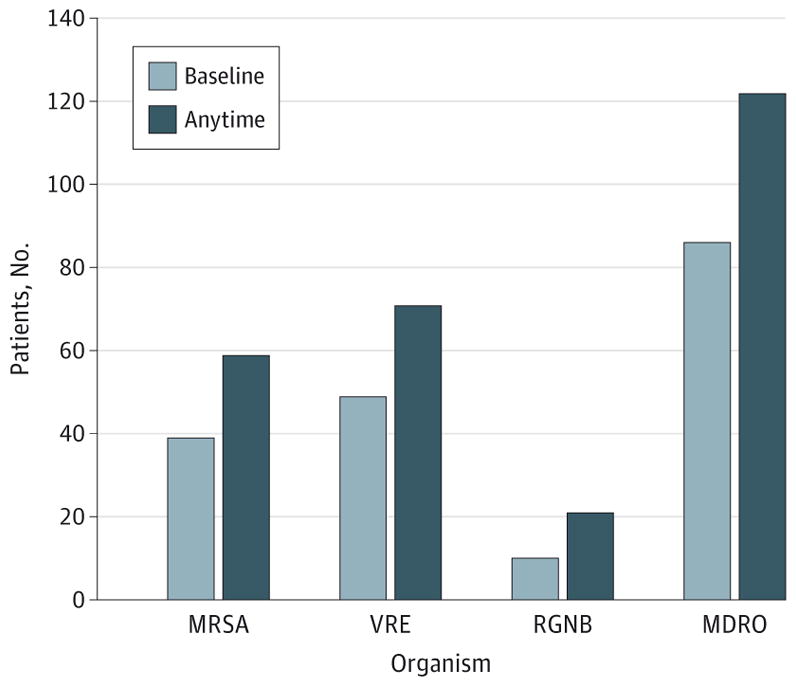
MDRO indicates multidrug resistant organism; MRSA, methicillin-resistant Staphylococcus aureus; RGNB, resistant-gram negative bacilli; and VRE, vancomycin-resistant Enterococcus. During the entire follow-up period, 34.2% (122 of 357) patients were colonized by at least 1 MDRO. MRSA, VRE, and RGNB were colonized on patients hands at rates of 16.5%(59 of 357), 19.9%(71 of 357), and 5.9% (21 of 357), respectively.
Discussion
Our study shows that patients commonly bring MDROs on their hands on discharge from an acute care hospital and acquire more during their stay at the PAC facility. This, combined with frequent antibiotic use in PAC patients, increases the probability that MDROs introduced to a PAC facility will be transmitted to other frail patients and to health care workers—and, most important, that the MDRO will persist in the facility. Current quality measures that address infection prevention fail to adequately address patient hand hygiene. Despite concerns raised by some recent studies,5–7 patient hand washing is not a routine practice in hospitals to date. Owing to PAC patients’ increased mobility and interaction with the environment, health care workers, and other patients, we believe that it is even more important to implement routines that enforce washing of patients’ hands than in the acute care setting.1
We did not conduct molecular typing for MDROs, and our analysis was limited to patients who were newly admitted to PAC facilities. Therefore, our estimates do not reflect the patients who were already residing in the facility, some of them long-term, and may under estimate the magnitude of hand colonization and its impact on transmission.
Our study provides critical and emerging evidence that patient hand hygiene is a greatly under appreciated strategy for MDRO reduction efforts in PAC facilities as well as acute care hospitals. Further interventions and development of performance measures to address this issue are overdue.
Acknowledgments
Funding/Support: This research was supported by National Institute on Aging grant R01AG032298 (Dr Mody), grant R01AG041780 (Drs Min, Foxman, and Mody), and grant K24AG050685 (Dr Mody).
Footnotes
Conflict of Interest Disclosures: None reported.
Previous Presentation: Preliminary data from this article were presented at the Annual Scientific Meeting of the American Geriatrics Society; May 15, 2015; National Harbor, Maryland.
Additional Contributions: We thank all the post–acute care facilities, health care workers, and patients for their participation.
Author Contributions: Dr Mody had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Cao, Lansing, Mody.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Cao, Mody.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Cao, Mody.
Obtained funding: Mody.
Administrative, technical, or material support: Lansing, Mody.
Study supervision: Min, Mody.
Role of the Funder/Sponsor: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
References
- 1.Mody L, Krein SL, Saint S, et al. A targeted infection prevention intervention in nursing home residents with indwelling devices: a randomized clinical trial. JAMA Intern Med. 2015;175(5):714–723. doi: 10.1001/jamainternmed.2015.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pittet D, Allegranzi B, Storr J, Donaldson L. “Clean Care is Safer Care”: the global patient safety challenge 2005–2006. Int J Infect Dis. 2006;10(6):419–424. doi: 10.1016/j.ijid.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 3.O’Donnell M, Harris T, Horn T, et al. Sustained increase in resident meal time hand hygiene through an interdisciplinary intervention engaging long-term care facility residents and staff. Am J Infect Control. 2015;43(2):162–164. doi: 10.1016/j.ajic.2014.10.018. [DOI] [PubMed] [Google Scholar]
- 4.Murphy CR, Eells SJ, Quan V, et al. Methicillin-resistant Staphylococcus aureus burden in nursing homes associated with environmental contamination of common areas. J AmGeriatr Soc. 2012;60(6):1012–1018. doi: 10.1111/j.1532-5415.2012.03978.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Istenes N, Bingham J, Hazelett S, Fleming E, Kirk J. Patients’ potential role in the transmission of health care-associated infections: prevalence of contamination with bacterial pathogens and patient attitudes toward hand hygiene. Am J Infect Control. 2013;41(9):793–798. doi: 10.1016/j.ajic.2012.11.012. [DOI] [PubMed] [Google Scholar]
- 6.Kundrapu S, Sunkesula V, Jury I, Deshpande A, Donskey CJ. A randomized trial of soap and water hand wash versus alcohol hand rub for removal of Clostridium difficile spores from hands of patients. Infect Control Hosp Epidemiol. 2014;35(2):204–206. doi: 10.1086/674859. [DOI] [PubMed] [Google Scholar]
- 7.Kim MK, Nam EY, Na SH, et al. Discrepancy in perceptions regarding patient participation in hand hygiene between patients and health care workers. Am J Infect Control. 2015;43(5):510–515. doi: 10.1016/j.ajic.2015.01.018. [DOI] [PubMed] [Google Scholar]


