Abstract
Objective
High rates of sexually transmitted infections (STIs) and unintended pregnancy suggest a role for multipurpose prevention technologies (MPTs) designed to combine contraception and infection prophylaxis into one unified method. This study aims to determine factors associated with interest in MPTs among U.S. women.
Study Design
We administered a national cross-sectional survey via MTurk. Eligibility criteria included female gender, age 18–29 years, residence in the U.S., and sexual activity with a male partner in the past three months. In total, 835 surveys were suitable for analysis. Bivariable and multivariable logistic regressions were performed to determine factors associated with interest in MPTs.
Results
Eighty-three percent of women were interested in MPTs. Factors associated with interest included oral sex in the past three months (aOR 1.87, 95% CI 1.07, 3.53), recent use of oral contraceptive pills (OCPs; aOR 1.78, 95% CI 1.08, 2.93), HIV test within one year (aOR 2.10, 95% CI 1.29, 3.40), and increased STI worry score (aOR 1.98, 95% CI 1.36, 2.86). No use of contraception in the past three months was associated with decreased interest in MPTs (aOR 0.31, 95% CI 0.17, 0.58). HIV risk factors including race were not associated with MPT interest.
Conclusion
Our data show that young, sexually active, U.S. women are interested in MPTs. Women who used contraception, specifically OCPs, or evidenced concern for infection were most likely to be interested in such a product. Women reporting unsafe sexual habits were less likely to be interested, highlighting the importance of HIV/STI prevention education.
Keywords: multipurpose prevention technologies, HIV prophylaxis, STIs, contraception
1. Introduction
Globally, women face sexual and reproductive health risks including unintended pregnancy and human immunodeficiency virus (HIV) infection. In the United States (U.S.) in 2011, nearly half of pregnancies were unintended, with the highest rate among 18-24 year-olds[1]. The Centers for Disease Control and Prevention (CDC) reported an estimated rate of 645.5 new cases of chlamydia, 107.2 new cases of gonorrhea, and 5.4 new cases of HIV per 100,000 women in the U.S. in 2015[2, 3]. Most new HIV infections occurred in women aged 25-34 with African American women at highest risk[3].
High rates of sexually transmitted infections (STIs) and unintended pregnancy among U.S. women suggest a role for multipurpose prevention technologies (MPTs), dual-purpose products designed to combine contraception and HIV/STI infection prophylaxis into one unified delivery method[4]. Condoms are currently the most basic form of MPT. However, typical condom use leads to pregnancy rates as high as 18 to 21% per year as use is often inconsistent, and women are not always able to advocate for condom usage[5-7]. Therefore, MPT development is aimed at woman-controlled products to reduce the need for partner negotiation[8]. Currently, intravaginal rings and diaphragms combined with a dual action spermicide/antimicrobial gel are under investigation[9]. In the future, MPTs may be available in various other forms, including pills, implants, and injectables[10].
Despite the potential of MPTs to protect women worldwide, only one study explicitly assessing interest has been published to date, and no research has been done among women in the U.S[11]. Studies have shown that some U.S. women are interested in a daily pill used as preexposure prophylaxis (PrEP) for protection against HIV infection[12-14]. We hypothesize that women with similar demographic and behavioral characteristics as those who expressed interest in HIV prophylaxis via PrEP may be interested in MPTs. Specifically, we hypothesize that African American women will be more interested in MPTs than Caucasian women, as previous research shows that African American women have higher interest in PrEP for HIV prophylaxis[14]. Therefore, this study aimed to determine if U.S. women are interested in MPTs and to identify demographic and behavioral characteristics associated with MPT interest.
2. Materials and Methods
2.1 Data Collection
This is a cross-sectional online survey. Subjects were recruited using Amazon's Mechanical Turk (MTurk), an online marketplace that allows workers to perform various tasks, including research surveys, for a nominal fee. It has been used extensively in social science research[15]. Analysis of the MTurk participant pool found that subjects are more demographically diverse than standard internet samples and the data collected are equally reliable compared to traditional methods[16]. We determined subject eligibility prior to survey initiation. Eligibility criteria included: self-identified female gender, age 18 to 29 years, living in the U.S., and sexually active with a male partner in the past three months. If eligible, subjects gave consent, continued to the survey and were compensated $3 for their participation. We received approval from the Emory University Institutional Review Board to conduct this study.
We aimed to recruit 850 participants in order to detect a 50% increase in interest in MPTs among African American compared to Caucasian women with 80% power (alpha of 0.05). We chose a priori to oversample African American women from the MTurk population to achieve the 3:1 ratio (White/Caucasian and Other: Black/African American) used in our power calculation. To this end, we paused enrollment once 647 “White/Caucasian” or “Other” women had completed the survey. At this point, “Black/African American” became an eligibility criterion.
2.2 Measures
Our primary outcome was interest in MPTs. We asked, “Are you interested in a form of birth control (other than a condom) that protects you against both unplanned pregnancy and infection with the HIV virus?” Using the same question stem, we inquired about interest in a similar product for protection against STIs other than HIV. We also assessed interest in contraception and HIV prophylaxis in order to compare interest in single-purpose products versus dual-purpose MPTs.
Predictor variables included demographics such as age, race, education, and zip code[17-19]. We examined sexual behavior by inquiring about relationship status, recent vaginal, oral, and anal intercourse, and frequency and type of contraception used within the past three months.
We assessed risk for HIV infection by inquiring about high-risk sexual behaviors as defined by the CDC: lack of condom at last sex, sex with a casual partner, greater than one sexual partner in the past three months, sex with a known HIV-positive male partner and anal sex without a condom[20].We used the Worry About Sexual Outcomes (WASO) scale adapted from Sales et al. to measure self-perceived risk of infection with HIV, STIs and unplanned pregnancy[21]. Our version of the WASO scale consisted of two items from each of three risk categories (worry about unintended pregnancy, HIV, and other STIs). Category scores ranged from 2 (lowest) to 8 (highest self-perceived risk) and were analyzed as continuous variables. Women were asked about a history of STIs or unintended pregnancy and whether they had been tested for HIV in the past year.
We piloted the survey for length and comprehensibility among seven women from various educational and geographic backgrounds prior to study initiation.
2.3 Statistical Analysis
Demographic and behavioral characteristics were characterized using descriptive statistics including frequencies and means with standard deviation.
To determine differences in MPT interest between groups, we analyzed dichotomous predictor variables using odds ratios (OR) and Pearson chi-square analysis, along with Fisher's exact test where appropriate. Categorical and continuous variables were evaluated using bivariable logistic regression. Variables with low levels of endorsement (fewer than 2% of the total survey population) were excluded. We examined the differences in the proportions of women interested in MPTs vs. contraception and HIV prophylaxis as well as the difference in the proportions interested in MPTs for HIV vs. other STIs using the McNemar test.
We assessed factors associated with interest in MPTs for HIV and MPTs for other STIs separately. As few specific differences were identified, we completed the remainder of the analysis using a composite variable reflecting interest in MPTs for either HIV or STIs.
We performed a multivariable logistic regression evaluating interest in MPTs including all predictor variables found to be significant at p < 0.05 in the bivariable analysis. We evaluated colinearity, selecting the strongest model with VIF < 2.5 and tolerance > 0.5. Adjusted ORs (aOR) with 95% confidence intervals (CI) are presented. We repeated this multivariable process for interest in contraception and HIV prophylaxis. The statistical analysis was completed using SPSS for Macintosh, Version 23[22].
3. Results
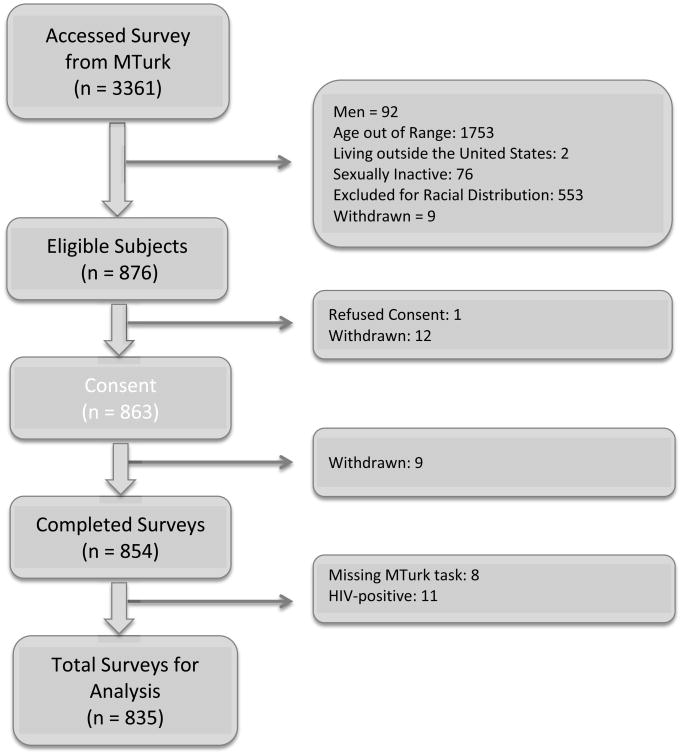
A total of 3,361 people followed the link from MTurk and answered the first eligibility question. Stepwise exclusion and withdrawal of respondents is detailed in Figure 1. Ultimately, 854 eligible women completed the survey; 8 were excluded due to lack of corresponding task completed in MTurk and 11 were HIV-positive, leaving 835 surveys suitable for analysis.
Figure 1. Subject Recruitment, Eligibility Determination, and Survey Completion.
Sequential exclusion of participants based on study inclusion criteria; withdrawn indicates subject(s) chose to terminate their participation prior to completing the indicated step in the enrollment procedure; exclusion based on race only after Black or African American was made an inclusion criteria to achieve the predetermined 3:1 ratio of “White/Caucasian” and “Other” to “Black/African American” subjects; completed surveys were excluded if they a. lacked a corresponding task completed in MTurk or if b. subject reported HIV-positive status; MTurk = Mechanical Turk; HIV = human immunodeficiency virus.
The demographic characteristics of the survey respondents are shown in Table 1. Sexual and contraceptive behaviors are recorded in Table 2. The mean age was 25.4 years. Two-thirds of women identified as White/Caucasian (65.7%) while nearly one quarter (23.6%) identified as Black/African American. More than half had engaged in HIV risk behaviors in the past three months. A small proportion (16.3%) had a lifetime history of an STI. Nearly a quarter (23.8%) reported an unintended pregnancy. The median worry scores for STIs, HIV, and pregnancy were 2, 2, and 3, respectively.
Table 1. Demographic Characteristics of the Study Population.
| Demographic Characteristics | |
|---|---|
| Age in years – mean (SD) | 25.4 (2.63) |
| Age Range – no. (%) | |
| 18-21 years | 76 (9.1) |
| 22-25 years | 329 (39.4) |
| 26-29 years | 430 (51.5) |
| Race or Ethnicity – no. (%) | |
| White/Caucasian | 549 (65.7) |
| Black/African American | 197 (23.6) |
| Other | 89 (10.7) |
| Hispanic/Latino (n = 833) | 71 (8.5) |
| Highest Level of Education – no. (%) | |
| Less than Bachelors degree | 401 (48.0) |
| Bachelors degree or higher | 434 (52.0) |
| United States Region* (n = 788) – no. (%) | |
| Northeast | 76 (9.8) |
| South | 329 (42.3) |
| Midwest | 174 (22.4) |
| West | 199 (25.6) |
| Type of Community* (n = 759) – no. (%) | |
| Urban | 699 (92.1) |
| Rural | 60 (7.9) |
Zip codes were categorized into regions and coded as urban vs. rural based on 2010 US. Census Bureau data;
SD = standard deviation; n = 835 unless otherwise specified.
Table 2. Sexual Behaviors, Contraceptive Use, HIV Risk Behaviors, and History of Unintended Sexual and Reproductive Health Outcomes Among the Study Population.
| No. (%) | |
|---|---|
| Relationship Status | |
| Single | 169 (20.2) |
| In a Relationship | 666 (79.8) |
| Sexual activity with a male partner | |
| Oral sex (n = 831) | 731 (88.0) |
| Anal sex (n = 833) | 221 (26.5) |
| Frequency of any contraception during sex (n = 833) | |
| All of the time | 462 (55.5) |
| Some of the time | 238 (28.6) |
| Never | 133 (16.0) |
| Frequency of condoms used during sex (n = 834) | |
| All of the time | 203 (24.3) |
| Some of the time | 307 (36.8) |
| Never | 324 (38.8) |
| Forms of birth control used | |
| Condoms | 487 (58.3) |
| Diaphragm | 13 (1.6) |
| Vaginal Ring | 31 (3.7) |
| Pills | 367 (44.0) |
| Patch | 13 (1.6) |
| Injections | 32 (3.8) |
| Implant | 41 (4.9) |
| IUD | 57 (6.8) |
| None | 122 (14.6) |
| HIV Risk Behaviors | |
| Condom at last sex (n = 833) | 348 (41.8) |
| Sexual partners > 1 | 158 (18.9) |
| Casual partner (n = 832) | 218 (26.2) |
| Known HIV+ male partner (n = 831) | 21 (2.5) |
| Anal sex without a condom (n = 833) | 175 (21.0) |
| Lifetime history of unintended pregnancy (n = 833) | 199 (23.8) |
| Lifetime history of STI(s) | 136 (16.3) |
| HIV test in the past year (n = 832) | 275 (33.1) |
Reported behaviors in the past three months except history of unintended pregnancy and STIs; HIV = human immunodeficiency virus; STI = sexually transmitted infection; n = 835 unless otherwise specified.
3.1 Interest in MPTs
The majority of women (82.9%) were interested in an MPT to protect against unplanned pregnancy and either HIV or other STIs. A slightly higher proportion of women were interested in MPTs protecting against STIs other than HIV (82.2%) compared to MPTs protecting against HIV (79.8%, p <0.001). Of 168 women not interested in MPTs for HIV, 26 (15.5%) were interested in MPTs for other STIs. More women were interested in dual-purpose MPTs than in single-purpose contraception (76.3%, p < 0.001) or HIV prophylaxis (68.0%, p < 0.001). Of 198 women not interested in contraception and 267 not interested in HIV prophylaxis, 100 (50.5%) and 163 (60.7%) were interested in MPTs, respectively.
Among the 13 factors found to be significant (p < 0.05) in the bivariable analysis of interest in MPTs, five continued to be significant in the multivariable analysis (Table 3.) Oral sex (aOR 1.87, 95% CI 1.07, 3.53) and use of oral contraceptive pills (OCPs) in the past three months (aOR 1.78, 95% CI 1.08, 2.93), HIV test within the past year (aOR 2.10, 95% CI 1.29, 3.40), and higher WASO STI scores (aOR 1.98, 95% CI 1.36, 2.86) were associated with higher interest in MPTs. Conversely, women who never (vs. always) used contraception within the past three months were less likely to be interested in MPTs (aOR 0.31, 95% CI 0.17, 0.58).
Table 3. Factors Predicting Interest in MPTs in the Bivariable and Multivariable Analyses.
| Characteristic | Interest | No Interest | OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|---|---|
| Age (in years) | -- | -- | 0.98 (0.92, 1.04) | |
| Race or ethnicity: | ||||
| White/Caucasian | 452 (82.3) | 97 (17.7) | ||
| Black/African American | 160 (81.2) | 37 (18.8) | 0.93 (0.61, 1.41) | |
| Other | 80 (89.9) | 9 (10.1) | 1.91 (0.93, 3.93) | |
| Highest level of education: | ||||
| Less than Bachelors Degree | 321 (80.0) | 80 (20.0) | 0.68 (0.47, 0.98)* | 0.78 (0.54, 1.19) |
| Bachelors Degree or higher | 371 (85.5) | 62 (14.5) | ||
| Geographic location: (n = 778) | ||||
| Northeast | 68 (89.5) | 8 (10.5) | -- | |
| South | 275 (83.6) | 54 (16.4) | 0.60 (0.27, 1.32) | |
| Midwest | 141 (81.0) | 33 (19.0) | 0.50 (0.22, 1.15) | |
| West | 165 (82.9) | 34 (17.1) | 0.57 (0.25, 1.30) | |
| Type of Community: (n = 759) | ||||
| Urban | 584 (83.5) | 115 (16.5) | 1.41 (0.74, 2.68) | |
| Rural | 47 (78.3) | 13 (21.7) | ||
| Relationship status: | ||||
| Single | 150 (88.8) | 19 (11.2) | 1.81 (1.08, 3.03)* | 1.43 (0.79, 2.62) |
| In a Relationship | 542 (81.4) | 124 (18.6) | ||
| Oral Sexual Activity | ||||
| Yes | 615 (84.1) | 116 (15.9) | 1.86 (1.14, 3.04)* | 1.87 (1.07, 3.53)* |
| No | 74 (74.0) | 26 (26.0) | ||
| Anal Sexual Activity | ||||
| Yes | 191 (86.4) | 30 (13.6) | 1.43 (0.92, 2.21) | |
| No | 691 (83.0) | 142 (17.0) | ||
| Frequency of use of contraception: | ||||
| All the time | 413 (89.4) | 49 (10.6) | -- | |
| Some of the time | 198 (83.2) | 40 (16.8) | 0.59 (0.37, 0.92)* | 0.63 (0.37, 1.08) |
| Never | 80 (60.2) | 53 (39.8) | 0.18 (0.11, 0.28)** | 0.31 (0.17, 0.58)** |
| Condoms (male and female) | ||||
| Yes | 417 (85.6) | 70 (14.4) | 1.58 (1.10, 2.27)* | 0.82 (0.45, 1.51) |
| No | 275 (79.0) | 73 (21.0) | ||
| Vaginal Ring | ||||
| Yes | 26 (83.9) | 5 (16.1) | 1.08 (0.41, 2.86) | |
| No | 666 (82.8) | 138 (17.2) | ||
| Oral Contraceptive Pills | ||||
| Yes | 331 (90.2) | 36 (9.8) | 2.73 (1.82, 4.09)** | 1.78 (1.08, 2.93)* |
| No | 361 (77.1) | 107 (22.9) | ||
| Injections | ||||
| Yes | 29 (90.6) | 3 (9.4) | 2.04 (0.61, 6.80) | |
| No | 663 (82.6) | 140 (17.4) | ||
| Implant | ||||
| Yes | 33 (80.5) | 8 (19.5) | 0.84 (0.38, 1.87) | |
| No | 659 (83.0) | 135 (17.0) | ||
| Intrauterine Device | ||||
| Yes | 54 (94.7) | 3 (5.3) | 3.95 (1.22, 12.81)* | 3.39 (0.95, 12.10) |
| No | 638 (82.0) | 140 (18.0) | ||
| Any Form of Contraception | ||||
| Yes | 620 (87.0) | 93 (13.0) | 4.63 (3.31, 7.06)** | Excluded from model |
| No | 72 (59.0) | 50 (41.0) | ||
| Condom at last sex | ||||
| Yes | 302 (86.8) | 46 (13.2) | 1.62 (1.11, 2.38)* | 1.48 (0.81, 2.69) |
| No | 389 (80.2) | 96 (19.8) | ||
| >1 sexual partner | ||||
| Yes | 135 (85.4) | 23 (14.6) | 1.27 (0.78, 2.05) | |
| No | 557 (82.3) | 120 (17.7) | ||
| Sex with casual partner | ||||
| Yes | 187 (85.8) | 31 (14.2) | 1.33 (0.86, 2.05) | |
| No | 503 (81.9) | 111 (18.1) | ||
| Sex with HIV+ partner | ||||
| Yes | 14 (66.7) | 7 (33.3) | 0.40 (0.16, 1.02) | |
| No | 674 (83.2) | 136 (16.8) | ||
| Anal sex without a condom | ||||
| Yes | 152 (86.9) | 23 (13.1) | 1.46 (0.90, 2.36) | |
| No | 539 (81.9) | 119 (18.1) | ||
| WASO Scale: HIV (2 to 8) | -- | -- | 1.24 (0.94, 1.64) | |
| HIV test within the past year (n = 807) | ||||
| Yes | 246 (89.5) | 29 (10.5) | 2.16 (1.39, 3.35)** | 2.10 (1.29, 3.40)* |
| No | 424 (79.7) | 108 (20.3) | ||
| WASO Scale: STI (2 to 8) | -- | -- | 2.12 (1.54, 2.93)** | 1.98 (1.36, 2.86)** |
| History of infection with an STI | ||||
| Yes | 122 (89.7) | 14 (10.3) | 1.97 (1.10, 3.54)* | 1.89 (0.93, 3.85) |
| No | 570 (81.5) | 129 (18.5) | ||
| WASO Scale: Pregnancy (2 to 8) | -- | -- | 1.18 (1.01, 1.39)* | 1.14 (0.95, 1.37) |
| History of unintended pregnancy | ||||
| Yes | 162 (81.4) | 37 (18.6) | 0.88 (0.58, 1.33) | |
| No | 528 (83.3) | 106 (16.7) |
Odds ratios calculated in bivariable analysis with n = 830 to 835 except where otherwise specified; Adjusted odds ratios calculated using multivariable logistic regression with n = 788; Reported behaviors in the past three months except history of unintended pregnancy and STIs; CI = confidence interval; OR = odds ratio; HIV = human immunodeficiency virus; STI = sexually transmitted infection; WASO = worry about sexual outcomes score;
Significant to 0.05;
Significant to 0.001.
We compared the multivariable predictors of interest in MPTs with factors associated with interest in contraception and HIV prophylaxis (Table 4.) Frequency of use of contraception was significant in all three models; subjects who never used contraception were less likely to be interested in all three products. Use of OCPs was associated with an increased interest in MPTs and contraception, while use of condoms was associated with interest in HIV prophylaxis. WASO STI score was related to interest in MPTs and HIV prophylaxis but not in contraception.
Table 4. Multivariable Associations Predicting Interest in MPTs, Contraception, and HIV Prophylaxis.
| MPTs aOR (95% CI) | Contraception aOR (95% CI) | HIV Prophylaxis aOR (95% CI) | |
|---|---|---|---|
| Single relationship status | --- | --- | 2.76 (1.50, 5.08)** |
| Oral sexual activity | 1.87 (1.07, 3.53)* | --- | --- |
| Use of contraception: never | 0.31 (0.17, 0.58)** | 0.11 (0.06, 0.19)** | 0.48 (0.29, 0.79)* |
| Use of OCPs | 1.78 (1.08, 2.93)* | 1.85 (1.18, 2.90)* | --- |
| Use of condoms | --- | --- | 1.99 (1.21, 3.27)* |
| WASO STI score | 1.98 (1.36, 2.86)** | --- | 1.51 (1.12, 2.04)* |
| HIV test within past year | 2.10 (1.29, 3.40)* | --- | --- |
| Sex with HIV+ partner(s) | --- | --- | 0.08 (0.02, 0.29)** |
| US Region: | |||
| South | --- | 0.41 (0.18, 0.90)* | --- |
| Midwest | --- | 0.36 (0.15, 0.83)* | --- |
Results from multivariable analyses; Adjusted odds ratios calculated using multivariable logistic regression with n = 788 (MPTs), n = 760 (contraception), and n = 776 (HIV prophylaxis); Reported behaviors in the past three months unless otherwise stated; aOR = adjusted odds ratio; CI = confidence interval; HIV = human immunodeficiency virus; OCP = oral contraceptive pills; STI = sexually transmitted infection; WASO = worry about sexual outcomes score;
Significant to 0.05;
Significant to 0.001.
4. Discussion
To our knowledge, interest in MPTs has not previously been studied among a U.S. population. A higher proportion of young U.S. women expressed interest in MPTs (83%) compared to the published proportion of African women. From a study population of women, male partners, health professionals, and community stakeholders in Malawi and Zimbabwe, 64% of women were interested in a product that could prevent both pregnancy and HIV infection[11]. It is important to note that while our population is a nationally representative sample, the African women were participants enrolled in microbicide efficacy trials, thereby limiting direct comparison. Notably, we found that interest in a combined method (84%) was higher than interest in single-purpose contraception (76%) or HIV prevention (68%) alone.
Women in our study who reported using contraception were more likely to be interested in MPTs. Our data show that women who “always” used contraception in the past three months were more interested in MPTs. Specifically, this was true for women who used OCPs. Women using non-barrier contraception (such as OCPs) may be less likely to also use condoms, leaving them susceptible to infection[23]. By switching to a dual-purpose product, these women could benefit from added infection prophylaxis. Women who used contraception “some of the time” or “never” were less interested in MPTs, perhaps because contraception is not currently a priority for them in the setting of attempted conception or infertility.
Women who recognized their risks and took action to protect themselves were most likely to be interested in MPTs. Our results show that women who reported undergoing HIV testing in the past year were more interested in MPTs, as was seen in studies for PrEP[24]. Women with higher WASO STI scores, reflecting concern for infection, were also more interested in MPTs. Although higher WASO HIV score was a non-significant predictor, we believe this is related to the smaller number of women concerned specifically about HIV infection. Women who did not evidence concern, for example those women with lower WASO STI scores, expressed less interest in MPTs. These data suggest that infection risk awareness is an important factor in determining MPT interest.
Certain factors known to be associated with HIV acquisition risk, including African American race, were not associated with MPT interest[3]. Although previous research indicates higher interest in PrEP among African American women, we did not find a racial difference for interest in MPTs[14]. Age was not a predictor of MPT interest and we found no link between age and self-perceived risk of HIV despite younger women being at higher risk[3]. In a previous national survey, younger U.S. women demonstrated lower interest in PrEP[25]. Moreover, younger age is a known factor in reduced adherence in PrEP trials in Africa[26, 27]. Finally, among our population, higher – not lower – education was associated with interest in MPTs, contrary to findings from one study noting that lower education was associated with higher potential PrEP uptake[14].
Over half of the women in our study reported at least one HIV risk behavior. There was no significant link between education and women with at least one risk factor; however, women with lower education were more likely to have had anal sex without a condom. Despite their prevalence, HIV risk behaviors were not associated with MPT interest. The WASO scores for HIV were lower than those for STIs, indicating overall less perceived need for protection from HIV, likely explained by the low relative incidence rate in the U.S[2, 3]. Previous PrEP research has shown that low self-perceived risk is a barrier to HIV prophylaxis and could lead to lower MPT uptake[13, 24]. We found that U.S. women demonstrated higher interest in MPTs for STIs other than HIV, suggesting that demand for MPTs aimed at preventing other STIs may be higher than for those to prevent HIV in a population with relatively low rates of HIV infection. Low perceived risk of HIV highlights the benefit of combining contraception and HIV prevention in a single method. Contraception is widely valued due to high actual and perceived rates of unintended pregnancy; therefore, MPTs may have broader appeal due to the contraceptive component. This is supported by our data showing higher interest in MPTs than in single-purpose HIV prophylaxis.
Our study has notable strengths and some limitations. The generalizability of our data is determined by the external validity of our data collection method. The MTurk population has been shown to be more representative of the U.S. population than in-person convenience samples and the racial distribution was found to be similar to a nationally stratified sample survey[15, 28]. However, despite our recruitment strategies, it is possible that our sample does not adequately represent woman at highest risk of HIV infection. Additionally, we did not assess current fertility intentions, which could influence interest in MPTs; however, we believe these behaviors are reflected by assessment of interest in contraception. Similarly, sterilized women were not excluded, potentially leading to underestimation of interest in MPTs. We also recognize that women may have expressed interest in MPTs not for themselves but for the overall public good. Finally, we realize that theoretical interest may not translate to use. Nevertheless, our data emphasize the importance of moving forward with development of MPTs for the U.S. market.
In conclusion, our data show that young, sexually active, U.S. women are interested in MPTs for protection against unintended pregnancy and HIV/STIs. The added benefit of dual protection increased interest in MPTs above that of single-purpose products. Women already using protection, specifically non-barrier contraception in the form of OCPs, or who evidenced concern for infection were most interested in MPTs. Unfortunately, the group of women who reported high-risk sexual behaviors and could most benefit from MPTs did not express higher interest, accentuating the continued need for HIV/STI prevention education.
Implications.
Women in the U.S. are interested in multipurpose prevention technologies, particularly those women who currently use contraception or are concerned about their risk of infection. Our results emphasize the importance of moving forward with MPT development as well as continued HIV/STI prevention education.
Acknowledgments
Supported in part by PHS Grant UL1TR000454 from the Clinical and Translational Science Award Program, National Institutes of Health, National Center for Advancing Translational Sciences. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors would also like to acknowledge the additional funding support provided by the Emory University School of Medicine, Department of Gynecology and Obstetrics via the 2016-2017 Marianne Ruby Award.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Literature Cited
- 1.Finer LB, Zolna MR. Declines in Unintended Pregnancy in the United States, 2008–2011. N Engl JMed. 2016;374:843–52. doi: 10.1056/NEJMsa1506575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2015. Atlanta: Oct, 2016. [accessed: 3.25.17]. https://www.cdc.gov/std/stats15/std-surveillance-2015-print.pdf. [Google Scholar]
- 3.Centers for Disease Control and Prevention. [accessed: 1.9.17];HIV Surveillance Report 2015. 27 http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html Published November 2016. [Google Scholar]
- 4.Romano J, Manning J, Hemmerling A, McGrory E, Holt BY. Prioritizing multipurpose prevention technology development and investments using a target product profile. Antiviral Res. 2013;(100 Suppl):S32–8. doi: 10.1016/j.antiviral.2013.09.016. [DOI] [PubMed] [Google Scholar]
- 5.Beksinska ME, Smit JA, Mantell JE. Progress and challenges to male and female condom use in South Africa. Sexual health. 2012;9:51–8. doi: 10.1071/SH11011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Donta B, Begum S, Naik DD. Acceptability of male condom: an Indian scenario. Indian J Med Res. 2014;(140 Suppl):S152–6. [PMC free article] [PubMed] [Google Scholar]
- 7.Contraception. Centers for Disease Control and Prevention; 2017. [accessed: 2.9.17]. How effective are birth control methods? https://www.cdc.gov/reproductivehealth/contraception. [Google Scholar]
- 8.Malcolm RK, Boyd P, McCoy CF, Murphy D. Beyond HIV microbicides: multipurpose prevention technology products. Br J Obstet Gynaecol. 2014;121:62–9. doi: 10.1111/1471-0528.12852. [DOI] [PubMed] [Google Scholar]
- 9.Friend DR. An update on multipurpose prevention technologies for the prevention of HIV transmission and pregnancy. Expert opinion on drug delivery. 2016;13:533–45. doi: 10.1517/17425247.2016.1134485. [DOI] [PubMed] [Google Scholar]
- 10.Brady M, Tolley E. Aligning product development and user perspectives: social-behavioural dimensions of multipurpose prevention technologies. BJOG. 2014;121(5):70–8. doi: 10.1111/1471-0528.12844. [DOI] [PubMed] [Google Scholar]
- 11.Woodsong C, Musara P, Chandipwisa A, et al. Interest in multipurpose prevention of HIV andpregnancy: perspectives of women, men, health professionals and community stakeholders in two vaginalgel studies in southern Africa. Br J Obstet Gynaecol. 2014;121(5):45–52. doi: 10.1111/1471-0528.12875. [DOI] [PubMed] [Google Scholar]
- 12.Eisingerich AB, Wheelock A, Gomez GB, Garnett GP, Dybul MR, Piot PK. Attitudes and acceptance of oral and parenteral HIV preexposure prophylaxis among potential user groups: a multinational study. PLoS One. 2012;7:e28238. doi: 10.1371/journal.pone.0028238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith DK, Toledo L, Smith DJ, Adams MA, Rothenberg R. Attitudes and program preferences of African-American urban young adults about pre-exposure prophylaxis (PrEP) AIDS Educ Prev. 2012;24:408–21. doi: 10.1521/aeap.2012.24.5.408. [DOI] [PubMed] [Google Scholar]
- 14.Wingood GM, Dunkle K, Camp C, et al. Racial differences and correlates of potential adoption of preexposure prophylaxis: results of a national survey. J Acquir Immune Defic Syndr. 2013;63(1):S95–101. doi: 10.1097/QAI.0b013e3182920126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huff C, Tingley D. Who are these people? Evaluating the demographic characteristics and political.preferences of MTurk survey respondents. Research and Politics 2015. 2015 Jul-Aug;:1–12. [Google Scholar]
- 16.Buhrmester M, Kwang T, Gosling SD. Amazon's Mechanical Turk: A New Source of Inexpensive, Yet High-Quality Data? Perspect Psychol Sci. 2011;6:3–5. doi: 10.1177/1745691610393980. [DOI] [PubMed] [Google Scholar]
- 17.Geography. United States Census Bureau; 2015. Census Regions and Divisions of the United States. [Google Scholar]
- 18.United States Zip Codes. [accessed: 11.8.16];2014 http://www.unitedstateszipcodes.org.
- 19.United States Census Bureau; 2010. [accessed: 11.2.16]. Urban and Rural Universe: Housing units. http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=DEC_10_SF1_H2&prodType=table. [Google Scholar]
- 20.Centers for Disease Control and Prevention; 2016. [accessed: 11.8.16]. HIV Risk Reduction Tool. https://wwwn.cdc.gov/hivrisk. [Google Scholar]
- 21.Sales JM, Spitalnick J, Milhausen RR, et al. Validation of the worry about sexual outcomes scale for use in STI/HIV prevention interventions for adolescent females. Health Educ Res. 2009;24:140–52. doi: 10.1093/her/cyn006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.SPSS for Macintosh, Version 23.0. Armonk, NY: IBM Corporation; 2015. [Google Scholar]
- 23.Kottke M, Whiteman MK, Kraft JM, et al. Use of Dual Methods for Protection from Unintended Pregnancy and Sexually Transmitted Diseases in Adolescent African American Women. J Pediatr Adolesc Gynecol. 2015;28:543–8. doi: 10.1016/j.jpag.2015.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kwakwa HA, Bessias S, Sturgis D, et al. Attitudes Toward HIV Pre-Exposure Prophylaxis in a United States Urban Clinic Population. AIDS Behav. 2016;20:1443–50. doi: 10.1007/s10461-016-1407-9. [DOI] [PubMed] [Google Scholar]
- 25.Rubtsova A, Wingood GM, Dunkle K, Camp C, DiClemente RJ. Young adult women and correlates of potential adoption of pre-exposure prophylaxis (PrEP): results of a national survey. Curr HIV Res. 2013;11:543–8. doi: 10.2174/1570162x12666140129104952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sheth AN, Rolle CP, Gandhi M. HIV pre-exposure prophylaxis for women. Journal of virus eradication. 2016;2:149–55. doi: 10.1016/S2055-6640(20)30458-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baeten JM, Palanee-Phillips T, Brown ER, et al. Use of a Vaginal Ring Containing Dapivirine for HIV-1 Prevention in Women. N Engl J Med. 2016;375:2121–32. doi: 10.1056/NEJMoa1506110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berinsky AJ, Huber GA, Lenz GS. Evaluating Online Labor Markets for Experimental Research: Amazon.com's Mechanical Turk. Political Analysis. 2012;20:351–68. [Google Scholar]